Abstract
There are several options for the treatment of varicocele, including surgical repair either by open or microsurgical approach, laparoscopy, or through percutaneous embolization of the internal spermatic vein. The ultimate goal of varicocele treatment relies on the occlusion of the dilated veins that drain the testis. Percutaneous embolization offers a rapid recovery and can be successfully accomplished in approximately 90% of attempts. However, the technique demands interventional radiologic expertise and has potential serious complications, including vascular perforation, coil migration, and thrombosis of pampiniform plexus. This review discusses the common indications, relative contraindications, technical details, and risks associated with percutaneous embolization of varicocele.
Keywords: interventional radiology, male infertility, therapeutic embolization, varicocele
INTRODUCTION
A varicocele consists of abnormally dilated and tortuous veins within the pampiniform plexus of the spermatic cord.1 Varicocele is prevalent, occurring in approximately 15% of all men, 35% of men with primary infertility, and up to 80% of men with secondary infertility.1 While the majority of men with varicocele are asymptomatic, there is clear evidence that varicocele is associated with a progressive decline in testicular function resulting in impaired semen parameters and possibly decreased serum testosterone.2 Accordingly, treatment of varicocele has been shown to arrest continued decline in testicular function, improve semen parameters and, in some reports, serum testosterone.3 Thus, in some men with primary or secondary infertility, treatment of varicocele may obviate the need for assisted reproduction, thereby sparing additional interventions, cost, and psychological stress. Varicocele can also lead to scrotal pain, and correction of varicocele can benefit men with scrotal pain who have failed conservative measures.4
Both surgical and nonsurgical approaches to the treatment of varicocele have been described. The conventional inguinal or subinguinal operative approach involves an inguinal incision with surgical ligation of all visibly dilated spermatic veins and careful avoidance of the testicular artery.5 Laparoscopic varicocelectomy utilizes a minimally invasive operative technique to ligate the internal spermatic veins proximally.6 Radiographic approaches involve venography to identify the internal spermatic and collateral veins with subsequent venous occlusion via a variety of occlusion and embolization techniques. The rate of varicocele recurrence is highly variable ranging from 0.6% to 45% depending upon treatment approach.1 Efficacy of varicocelectomy for the treatment of infertility is determined based upon improvement in serum testosterone levels, semen parameters, and, ultimately, pregnancy rates following treatment. In patients with scrotal pain, the primary objective is alleviation of pain.
Percutaneous embolization is the least invasive of all treatment approaches. In contrast to traditional surgical therapies, percutaneous interventional approaches do not require surgical incisions and thus can be performed under local anesthesia, whereas surgical approaches require more extensive anesthetic preparations. The use of venography enables the precise identification of the internal spermatic veins, in addition to any collateral venous vascular supply that may contribute to the clinical pathology. In addition, the transvenous method virtually eliminates the potential for damage to the testicular artery, which results in theoretically reduced complications related to testicular pain and atrophy.
The current article reviews the use of percutaneous varicocele embolization. We will provide a brief overview of the history of the procedure and review several approaches and materials used in contemporary embolization, success and complications of embolization, and an evaluation of percutaneous embolization in the adolescent population.
HISTORY OF PERCUTANEOUS EMBOLIZATION OF VARICOCELE
Spermatic venography was first introduced in the 1970s as a diagnostic tool for the identification of incompetent spermatic veins and the need for surgical intervention.7 In 1978, Lima et al. made the first attempt at a percutaneous therapeutic intervention for the management of varicocele. Percutaneous occlusion of the left spermatic vein was achieved by injecting a combination of glucose and a sclerosing agent through a transvenous catheter.8 Over the ensuing years, subsequent attempts used a variety of obliterative methods including sclerosing agents, balloon occlusion, and coil embolization.
The early attempts at percutaneous embolization employed a transfemoral approach to the left spermatic vein. While successful, the femoral approach limited access to the right spermatic vein, thereby limiting the scope of the procedure to patients with a unilateral varicocele. In 1981, Formanek et al. pioneered the transjugular approach, which enabled bilateral percutaneous embolization.9,10 Currently, both transfemoral and transjugular approaches are used.
RELEVANT VASCULAR ANATOMY OF VARICOCELE
Knowledge of venous drainage patterns of the internal spermatic vein is critical for vascular access techniques. The internal spermatic vein begins at the confluence of the pampiniform, or spermatic venous, plexus near the femoral head. Typically, the left spermatic vein drains into the left renal vein whereas the right drains directly into the inferior vena cava on the anterolateral wall below the right renal vein. The greater prevalence of left-sided varicocele is believed to be secondary to the unique angle at the confluence of the left spermatic and renal veins, which leads to increased hydrostatic pressure. Significant variations in this typical pattern have been described with anomalous communications noted among retroperitoneal, peritoneal, adrenal, and portal veins, as well as communication between left and right spermatic veins.11,12
OVERVIEW OF THE EMBOLIZATION TECHNIQUE
Anesthesia
The procedure is typically performed on an outpatient basis. The use of anesthesia is limited to the use of local anesthesia and intravenous sedation. Shielding with limited fluoroscopy is used to minimize radiation exposure to patients, especially in young males.13
Vascular access
For a left-sided varicocele, the most common access is the right common femoral vein (Figure 1). Right-sided access is routinely preferred as it is technically easier and provides an optimal angle for catheter access into the left renal and internal spermatic vein. For a right-sided varicocele, the internal jugular or basilica vein approach is more commonly utilized. The right internal spermatic vein is typically located at an acute angle on the right anterolateral inferior vena cava just below the right renal vein, which results in a straight line approach from the internal jugular vein access point.
Figure 1.
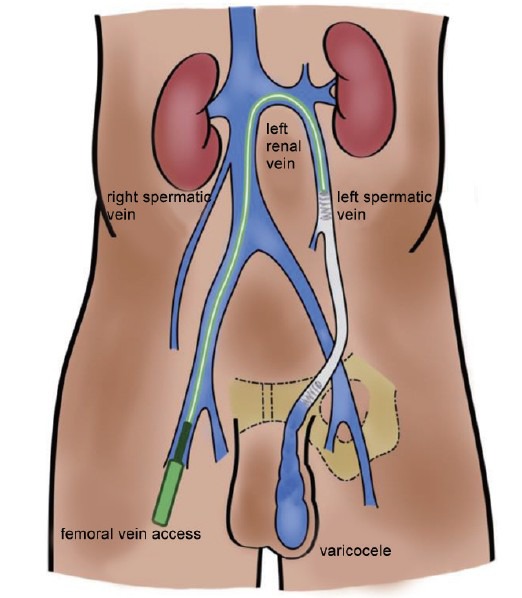
Illustration of left spermatic vein access from the right femoral vein.
Venography
The catheter tip is placed at the junction of the distal internal spermatic vein and the pampiniform plexus. A venogram is performed by placing the patient in reverse Trendelenburg position or with the patient performing the Valsalva maneuver. This is useful in confirmation of the diagnosis and mapping of the venous collaterals.13 The typical venous collateral pattern is the branching of the internal spermatic vein into the medial and lateral divisions at the L4 level. The medial division drains into the left renal vein or inferior vena cava while the lateral division drains into the renal capsular and/or colonic veins. Cross-communications between the left and right spermatic veins are often seen. Recognizing the presence of collaterals is crucial as an unsuccessful interruption of these collateral pathways may contribute to the persistence or recurrence of varicocele.14,15,16
Choice of embolic agent
Embolic agents commonly utilized for varicocele embolization include mechanically occlusive solid and liquid embolic agents. Figure 2 demonstrates a case of left varicocele embolization which employs both types of agents. The choice of embolic agent depends on operator preference. Solid embolics include coils and vascular plugs. In addition to mechanical occlusion, the presence of thrombogenic “fibers” within the coils induces thrombotic occlusion. Disadvantages of solid embolics include risk of coil migration and venous perforation. Liquid embolics include the popularly used sclerosant sodium tetradecyl sulfate (STS) and adhesive polymers like nBCA (glue). Liquid embolics induce an inflammatory reaction, resulting in endothelial necrosis and thrombosis. Disadvantages of liquid embolics include risk of catheter entrapment, nontarget embolization, glue migration, and pampiniform plexus phlebitis.14,17
Figure 2.
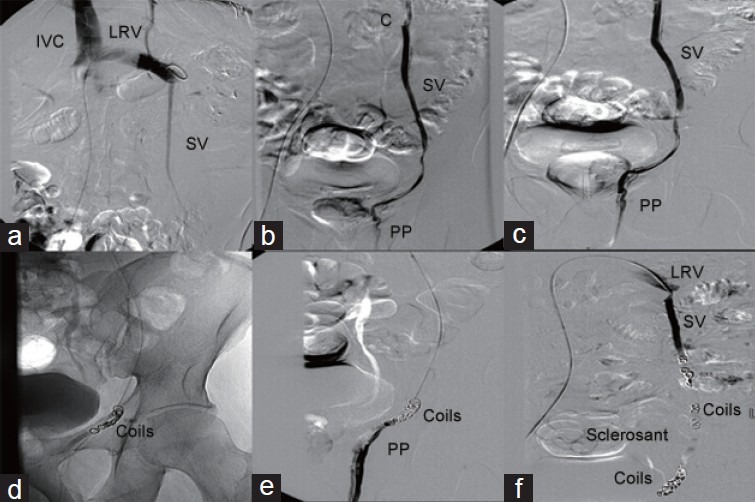
43-year-old male with recurrent varicocele following remote varicocelectomy who presented for embolization with access via the right common femoral vein. (a) Selective catheterization of the left renal vein showed reflux into the left SV. Selective venogram of the left SV in its mid aspect; (b) and later at the level of inguinal ligament. (c) Confirmed the reflux into multiple branches of SV distally and into the PP. (d) Coil embolization of distal branches of the SV and (e) proximal embolization of the SV was performed using the sandwich technique. (f) Postcoiling venogram demonstrated no residual reflux distally into the left gonadal vein.
Postprocedure care
Patients should be observed for approximately 2–3 h postprocedure before being discharged home. Although patients can return to routine activities within 24–48 h, they are advised to avoid heavy lifting and contact sports for 5–7 days and consume a soft solid diet for 3 days to prevent constipation. A follow-up Doppler ultrasound is performed at 3 months and semen analysis at 4–6 months in patients undergoing therapy due to infertility. At follow-up, even though veins can be evident on exam, success of the procedure is determined by lack of retrograde flow.
OUTCOMES OF PERCUTANEOUS VARICOCELE EMBOLIZATION
Technical success
Technical success with percutaneous embolization is defined as cessation of flow as demonstrated by intra-operative imaging. Successful embolization depends upon several factors such as patient anatomy, vascular access, and intra-operative factors such as embolization material and vasospasm. Anatomical considerations are particularly important, especially with regard to laterality of the varicocele. Since inception, percutaneous embolization for right-sided varicoceles has proven technically challenging.9 Whereas left-sided technical failures are rare, multiple studies have shown technical failure rates as high as 49% for right-sided varicocele.18,19 A meta-analysis by Cayan et al. found an overall technical failure rate of 13.05% among 314 patients, irrespective of laterality, but the authors did not report follow-up duration for this cohort.20
Careful patient selection can ensure greater technical success. For example, in the setting of recurrent varicocele following surgical therapy, excellent success has been shown ranging from 93% to 100%.4,15,21
Recurrence
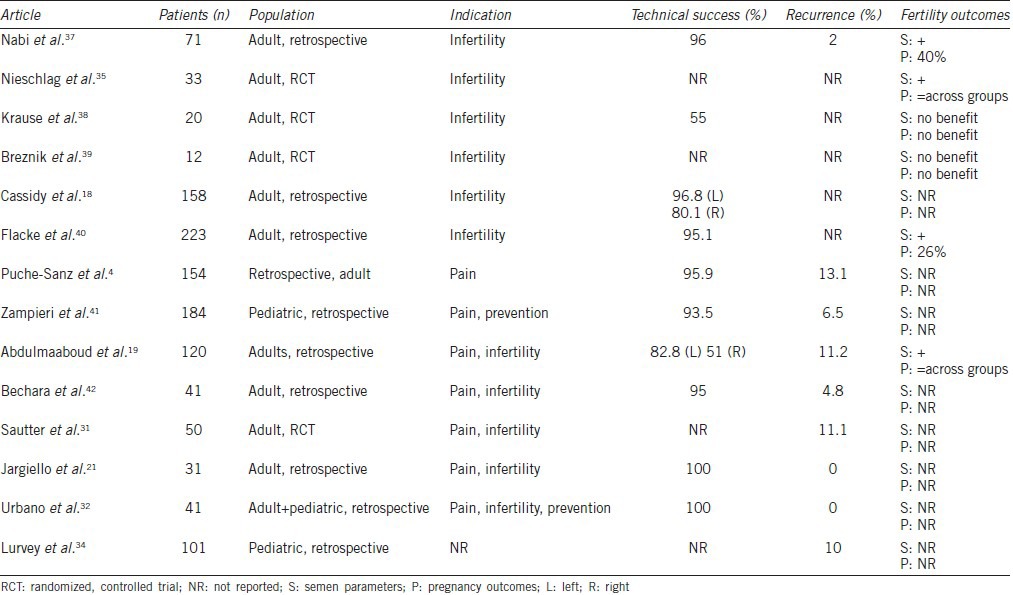
One advantage of embolization over surgery is the ability to perform intra-operative venography that can identify venous anatomic variants. Theoretically, this can help to prevent recurrence, as the majority of surgical failures result from undiagnosed gonadal vein duplications.21 However, the literature revealed a wide range of postembolization recurrence from 0% to 24% as compared to 0%–3% for microsurgical varicocelectomy (Table 1).20 While contemporary series show lower recurrence rates likely resulting from improved embolization technique and operator experience, embolization remains inferior to the microsurgical technique.
Table 1.
Outcomes of percutaneous embolization
Fertility
The effect of percutaneous embolization on fertility remains controversial due to the sparsity of data correlating intervention with pregnancy outcomes. Multiple studies have demonstrated improvement in semen parameters following embolization. For example, Prasivoravong et al. performed retrospective analysis on 47 infertile male patients with left varicocele and at least one abnormal semen parameter who underwent embolization. Following embolization, median sperm concentration improved from 5.78 to 38.75 × 106 per ejaculate, and there were corresponding significant increases in sperm motility, vitality, percentage of normal sperm, and sperm head morphology. However, there was no improvement in postoperative serum testosterone, FSH or inhibin B levels. Correlation of postoperative semen parameters with successful pregnancy was not assessed.22 Other studies have confirmed similar results.23,24
Despite improvement of semen parameters, pregnancy outcomes following embolization in infertile couples with otherwise unexplained infertility are equivocal. An initial meta-analysis by Cayan et al. demonstrated that embolization was inferior to microsurgical varicocelectomy with regard to natural pregnancy rates.20 A later Cochrane review confirmed that there was weak evidence showing improved pregnancy rates following intervention, however, this was not well-correlated to live birth as an endpoint, nor was there a distinction made between surgical versus endoscopic treatment.25 Based on these findings, we recommend against utilizing percutaneous embolization as a first-line treatment for varicocele in men with infertility.
Embolization for scrotal pain
Percutaneous embolization is a viable treatment option for men suffering from orchalgia secondary to varicocele. Postoperative inflammation and scarring may prevent resolution or even exacerbate pain following surgical treatment, which may be avoided with the percutaneous approach.26 Puche-Sanz et al. performed a retrospective review of 154 patients who underwent embolization of varicocele for pain. Using visual analog scale pain questionnaires (range 1–10), median preoperative pain was 7 and postoperative pain was 0. At 39 months follow-up, 86.9% of patients had complete resolution of pain.4 Thus, embolization may be an appropriate option for patients with a painful varicocele.
Embolization for recurrence of varicocele following surgery
Percutaneous embolization may be an ideal treatment option for recurrences after surgery. Patients who have undergone primary surgical repair may not want to undergo a second operation, and surgeons may not feel comfortable with artery and lymphatic sparing techniques in the postsurgical patient due to the likelihood of distorted anatomy.26 Furthermore, studies have demonstrated that recurrent varicocele is often associated with increased inguinal collateral vasculature, which may be difficult to ligate surgically but can be well-targeted with endoscopic therapy.16 Jargiello et al. reported on 33 patients who had recurrence of a left varicocele following surgical management. Patients underwent retrograde venography to evaluate the anatomic architecture responsible for failure, following which they underwent embolization for definitive management. Anatomic studies revealed that 93% of patients had incompetence of the gonadal vein (most commonly secondary to gonadal vein duplication, 66%). Subsequent embolization was technically successful in 100% of patients.21 Other series have demonstrated similar technical success and improvement in semen parameters following embolization for recurrence.27 Percutaneous embolization remains an excellent choice for patients with recurrence following surgical treatment.
POSTOPERATIVE COMPLICATIONS
Major complications of embolization are rare. While venous vascular perforation is relatively common during the procedure, it rarely results in major hemorrhage. Even occasional inadvertent arterial perforation, for example, injury to the femoral artery, rarely results in major sequelae.28 Coil migration is a known risk of embolization procedures but is quite rare. Coil migration during left varicocelectomy can cause renal vein thrombosis; theoretically, further migration is possible to the level of the vena cava and even the pulmonary venous system, as reported in one instance.29 This can be prevented by accurately oversizing coils and using detachable coils or vascular plugs. Vicini et al. reported a case of large bowel infarction due to embolization of a venous anastomosis between the spermatic and mesenteric veins, which could not be detected on preembolization angiography.30
Patients who undergo embolization may experience peri-procedural pain for up to 10 days. While a few studies have reported a 3%–3.7% incidence of epididymitis with embolization and one group reported a 10% risk of hematoma, multiple studies have demonstrated 0% risk of developing chronic scrotal pain.19,31,32 The incidence of postembolization hydrocele is quite low, ranging from 0% to 12%, likely resulting from sparing of lymphatic channels via the intravascular approach.33,34,35
COST EFFECTIVENESS
In the current healthcare economic landscape, cost effectiveness is a crucial component in the evaluation of any diagnostic or therapeutic intervention. Kovac et al. performed a Markov decision-analysis model to evaluate cost effectiveness of microsurgical varicocelectomy, nonmicrosurgical varicocelectomy, and percutaneous embolization. The model included contingency scenarios for recurrence following each of the above primary interventions. The authors found that microsurgical varicocelectomy was the most cost effective method of treatment based on pregnancy outcomes, costing approximately $5402 (Canadian) per pregnancy. Percutaneous embolization was the least cost effective method, costing approximately $7300 (Canadian) per pregnancy.36
RELATIVE CONTRAINDICATIONS
We recommend against percutaneous embolization in a number of specific scenarios based on the above data (Table 2). Patients with bilateral grade 3 varicocele should not be considered for embolization given the significantly higher technical failure rates for right-sided varicocele, deeming these patients likely to require further surgical therapy. Patients who present for treatment of varicocele due to infertility should be recommended for surgery rather than embolization, due to evidence-based data that suggests pregnancy rates are improved following surgery but not with embolization.
Table 2.
Indications for percutaneous embolization in treatment of symptomatic varicocele
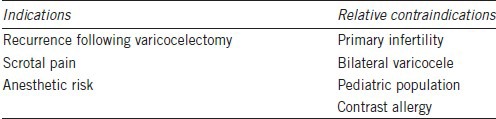
In the pediatric and adolescent populations, radiation exposure during embolization is a concern. Radiation to the gonads is associated with an increased risk of infertility or future malignancy, and pediatric patients may be at highest risk given their long life expectancy.
Embolization is an ideal choice for patients with a varicocele recurrence following initial surgical management as technical and clinical success in this scenario is excellent. Furthermore, embolization may be considered in patients with scrotal pain secondary to varicocele who are reluctant to undergo surgical intervention. Embolization is also an excellent alternative for patients with high anesthetic risk due to medical comorbidities as it can be performed easily under local anesthesia.
CONCLUSION
Overwhelming data suggests that percutaneous embolization for varicocele is a safe procedure in both adult and pediatric patients. Embolization offers certain advantages over surgery such as the ability to perform venography and the use of local anesthesia in lieu of more invasive anesthetic technique. However, embolization carries the risk, albeit small, of technical failure and, therefore, the need for further surgical management. Furthermore, recurrence rates following embolization are higher than those following surgical approaches. With careful patient selection and pretreatment counseling, embolization can be appropriately employed as a safe and effective treatment option for symptomatic varicocele.
AUTHOR CONTRIBUTIONS
JH, SM, and KP performed the literature review and drafted the manuscript. RR conceived of the topic, structured the discussion, and provided the urologic perspective for the manuscript. SB provided the radiologic perspective and images. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Wein AJ, Kavoussi LR, Campbell MF. Philadelphia, PA: Elsevier Saunders; 2012. Campbell-Walsh Urology. [Google Scholar]
- 2.Pastuszak AW, Wang R. Varicocele and testicular function. Asian J Androl. 2015;17:659–67. doi: 10.4103/1008-682X.153539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanrikut C, McQuaid JW, Goldstein M. The impact of varicocele and varicocele repair on serum testosterone. Curr Opin Obstet Gynecol. 2011;23:227–31. doi: 10.1097/GCO.0b013e328348a3e2. [DOI] [PubMed] [Google Scholar]
- 4.Puche-Sanz I, Flores-Martin JF, Vazquez-Alonso F, Pardo-Moreno PL, Cozar-Olmo JM. Primary treatment of painful varicocoele through percutaneous retrograde embolization with fibred coils. Andrology. 2014;2:716–20. doi: 10.1111/j.2047-2927.2014.00253.x. [DOI] [PubMed] [Google Scholar]
- 5.Nadelson EJ, Cohen M, Warner R, Leiter E. Update: varicocelectomy – A safe outpatient procedure. Urology. 1984;24:259–61. doi: 10.1016/0090-4295(84)90355-8. [DOI] [PubMed] [Google Scholar]
- 6.Hagood PG, Mehan DJ, Worischeck JH, Andrus CH, Parra RO. Laparoscopic varicocelectomy: preliminary report of a new technique. J Urol. 1992;147:73–6. doi: 10.1016/s0022-5347(17)37137-9. [DOI] [PubMed] [Google Scholar]
- 7.Sabatier JC, Bruneton JN, Drouillard J, Tavernier J, Ducos M, et al. [Spermatic phlebography: techniques and indications. A study on 37 cases (author's transl)] Ann Radiol (Paris) 1977;20:539–44. [PubMed] [Google Scholar]
- 8.Lima SS, Castro MP, Costa OF. A new method for the treatment of varicocele. Andrologia. 1978;10:103–6. doi: 10.1111/j.1439-0272.1978.tb01324.x. [DOI] [PubMed] [Google Scholar]
- 9.Formanek A, Rusnak B, Zollikofer C, Castaneda-Zuniga WR, Narayan P, et al. Embolization of the spermatic vein for treatment of infertility: a new approach. Radiology. 1981;139:315–21. doi: 10.1148/radiology.139.2.7220874. [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez R, Narayan P, Formanek A, Amplatz K. Transvenous embolization of internal spermatic veins: nonoperative approach to treatment of varicocele. Urology. 1981;17:246–8. doi: 10.1016/0090-4295(81)90040-6. [DOI] [PubMed] [Google Scholar]
- 11.Bass JE, Redwine MD, Kramer LA, Huynh PT, Harris JH., Jr Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics. 2000;20:639–52. doi: 10.1148/radiographics.20.3.g00ma09639. [DOI] [PubMed] [Google Scholar]
- 12.Bahren W, Lenz M, Porst H, Wierschin W. [Side effects, complications and contraindications for percutaneous sclerotherapy of the internal spermatic vein in the treatment of idiopathic varicocele] Rofo. 1983;138:172–9. doi: 10.1055/s-2008-1055705. [DOI] [PubMed] [Google Scholar]
- 13.D Beecroft JR. Percutaneous varicocele embolization. Can Urol Assoc J. 2007;1:278–80. [PMC free article] [PubMed] [Google Scholar]
- 14.Sze DY, Kao JS, Frisoli JK, McCallum SW, Kennedy WA, 2nd, et al. Persistent and recurrent postsurgical varicoceles: venographic anatomy and treatment with N-butyl cyanoacrylate embolization. J Vasc Interv Radiol. 2008;19:539–45. doi: 10.1016/j.jvir.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 15.Kim J, Shin JH, Yoon HK, Ko GY, Gwon DI, et al. Persistent or recurrent varicocoele after failed varicocoelectomy: outcome in patients treated using percutaneous transcatheter embolization. Clin Radiol. 2012;67:359–65. doi: 10.1016/j.crad.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 16.Rais-Bahrami S, Montag S, George AK, Rastinehad AR, Palmer LS, et al. Angiographic findings of primary versus salvage varicoceles treated with selective gonadal vein embolization: an explanation for surgical treatment failure. J Endourol. 2012;26:556–60. doi: 10.1089/end.2011.0387. [DOI] [PubMed] [Google Scholar]
- 17.Iaccarino V, Venetucci P. Interventional radiology of male varicocele: current status. Cardiovasc Intervent Radiol. 2012;35:1263–80. doi: 10.1007/s00270-012-0350-z. [DOI] [PubMed] [Google Scholar]
- 18.Cassidy D, Jarvi K, Grober E, Lo K. Varicocele surgery or embolization: which is better? Can Urol Assoc J. 2012;6:266–8. doi: 10.5489/cuaj.11064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdulmaaboud MR, Shokeir AA, Farage Y, Abd El-Rahman A, El-Rakhawy MM, et al. Treatment of varicocele: a comparative study of conventional open surgery, percutaneous retrograde sclerotherapy, and laparoscopy. Urology. 1998;52:294–300. doi: 10.1016/s0090-4295(98)00178-2. [DOI] [PubMed] [Google Scholar]
- 20.Cayan S, Shavakhabov S, Kadioglu A. Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl. 2009;30:33–40. doi: 10.2164/jandrol.108.005967. [DOI] [PubMed] [Google Scholar]
- 21.Jargiello T, Drelich-Zbroja A, Falkowski A, Sojka M, Pyra K, et al. Endovascular transcatheter embolization of recurrent postsurgical varicocele: anatomic reasons for surgical failure. Acta Radiol. 2015;56:63–9. doi: 10.1177/0284185113519624. [DOI] [PubMed] [Google Scholar]
- 22.Prasivoravong J, Marcelli F, Lemaitre L, Pigny P, Ramdane N, et al. Beneficial effects of varicocele embolization on semen parameters. Basic Clin Androl. 2014;24:9. doi: 10.1186/2051-4190-24-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tanahatoe SJ, Maas WM, Hompes PG, Lambalk CB. Influence of varicocele embolization on the choice of infertility treatment. Fertil Steril. 2004;81:1679–83. doi: 10.1016/j.fertnstert.2003.10.044. [DOI] [PubMed] [Google Scholar]
- 24.Di Bisceglie C, Fornengo R, Grosso M, Gazzera C, Mancini A, et al. Follow-up of varicocele treated with percutaneous retrograde sclerotherapy: technical, clinical and seminal aspects. J Endocrinol Invest. 2003;26:1059–64. doi: 10.1007/BF03345250. [DOI] [PubMed] [Google Scholar]
- 25.Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012;10:Cd000479. doi: 10.1002/14651858.CD000479.pub5. [DOI] [PubMed] [Google Scholar]
- 26.Ramasamy R. Percutaneous embolization: a viable treatment option for varicocele. Basic Clin Androl. 2014;24:10. doi: 10.1186/2051-4190-24-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Punekar SV, Prem AR, Ridhorkar VR, Deshmukh HL, Kelkar AR. Post-surgical recurrent varicocele: efficacy of internal spermatic venography and steel-coil embolization. Br J Urol. 1996;77:124–8. doi: 10.1046/j.1464-410x.1996.82321.x. [DOI] [PubMed] [Google Scholar]
- 28.Lenz M, Hof N, Kersting-Sommerhoff B, Bautz W. Anatomic variants of the spermatic vein: importance for percutaneous sclerotherapy of idiopathic varicocele. Radiology. 1996;198:425–31. doi: 10.1148/radiology.198.2.8596844. [DOI] [PubMed] [Google Scholar]
- 29.Chomyn JJ, Craven WM, Groves BM, Durham JD. Percutaneous removal of a Gianturco coil from the pulmonary artery with use of flexible intravascular forceps. J Vasc Interv Radiol. 1991;2:105–6. doi: 10.1016/s1051-0443(91)72481-0. [DOI] [PubMed] [Google Scholar]
- 30.Vicini P, Di Pierro GB, Grande P, Voria G, Antonini G, et al. Large bowel infarct following antegrade scrotal sclerotherapy for varicocele: a case report. Can Urol Assoc J. 2014;8:E641–3. doi: 10.5489/cuaj.1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sautter T, Sulser T, Suter S, Gretener H, Hauri D. Treatment of varicocele: a prospective randomized comparison of laparoscopy versus antegrade sclerotherapy. Eur Urol. 2002;41:398–400. doi: 10.1016/s0302-2838(02)00022-2. [DOI] [PubMed] [Google Scholar]
- 32.Urbano J, Cabrera M, Alonso-Burgos A. Sclerosis and varicocele embolization with N-butyl cyanoacrylate: experience in 41 patients. Acta Radiol. 2014;55:179–85. doi: 10.1177/0284185113493774. [DOI] [PubMed] [Google Scholar]
- 33.Storm DW, Hogan MJ, Jayanthi VR. Initial experience with percutaneous selective embolization: a truly minimally invasive treatment of the adolescent varicocele with no risk of hydrocele development. J Pediatr Urol. 2010;6:567–71. doi: 10.1016/j.jpurol.2010.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Lurvey R, Durbin-Johnson B, Kurzrock EA. Adolescent varicocele: a large multicenter analysis of complications and recurrence in academic programs. J Pediatr Urol. 2015;11:186.e1–6. doi: 10.1016/j.jpurol.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nieschlag E, Behre HM, Schlingheider A, Nashan D, Pohl J, et al. Surgical ligation vs. angiographic embolization of the vena spermatica: a prospective randomized study for the treatment of varicocele-related infertility. Andrologia. 1993;25:233–7. doi: 10.1111/j.1439-0272.1993.tb02716.x. [DOI] [PubMed] [Google Scholar]
- 36.Kovac JR, Fantus J, Lipshultz LI, Fischer MA, Klinghoffer Z. Cost-effectiveness analysis reveals microsurgical varicocele repair is superior to percutaneous embolization in the treatment of male infertility. Can Urol Assoc J. 2014;8:E619–25. doi: 10.5489/cuaj.1873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nabi G, Asterlings S, Greene DR, Marsh RL. Percutaneous embolization of varicoceles: outcomes and correlation of semen improvement with pregnancy. Urology. 2004;63:359–63. doi: 10.1016/j.urology.2003.09.026. [DOI] [PubMed] [Google Scholar]
- 38.Krause W, Muller HH, Schafer H, Weidner W. Does treatment of varicocele improve male fertility? results of the ‘Deutsche Varikozelenstudie’, a multicentre study of 14 collaborating centres. Andrologia. 2002;34:164–71. doi: 10.1046/j.1439-0272.2002.00494.x. [DOI] [PubMed] [Google Scholar]
- 39.Breznik R, Vlaisavljevic V, Borko E. Treatment of varicocele and male fertility. Arch Androl. 1993;30:157–60. doi: 10.3109/01485019308987750. [DOI] [PubMed] [Google Scholar]
- 40.Flacke S, Schuster M, Kovacs A, von Falkenhausen M, Strunk HM, et al. Embolization of varicocles: pretreatment sperm motility predicts later pregnancy in partners of infertile men. Radiology. 2008;248:540–9. doi: 10.1148/radiol.2482071675. [DOI] [PubMed] [Google Scholar]
- 41.Zampieri N, Chironi C, Sulpasso M. Treatment of varicocele with transfemoral retrograde sclero-embolization in pediatric patients under local anesthesia. Minerva Pediatr. 2015;67:227–9. [PubMed] [Google Scholar]
- 42.Bechara CF, Weakley SM, Kougias P, Athamneh H, Duffy P, et al. Percutaneous treatment of varicocele with microcoil embolization: comparison of treatment outcome with laparoscopic varicocelectomy. Vascular. 2009;17(Suppl 3):S129–36. doi: 10.2310/6670.2009.00062. [DOI] [PubMed] [Google Scholar]


