Abstract
The objective of this review was to summarize the evidence concerning the benefit of varicocele treatment to improve natural fertility in subfertile males. We also analyzed the effect of varicocele treatment on conventional semen parameters and sperm functional tests. An electronic search to collect the data was performed using the PubMed/MEDLINE databases until July 2015. Data pooled from a variety of study designs indicate that varicocelectomy improves semen parameters in the majority of the treated men with clinical varicocele and abnormal semen parameters regardless of the chosen surgical method. Surgical varicocele repair was beneficial not only for alleviating oxidative stress-associated infertility but also to improve sperm nuclear DNA integrity. However, given the low magnitude of the effect size in sperm DNA integrity, further research is needed to elucidate its clinical significance. Conflicting results on the effect of varicocele treatment on natural fertility seem to be due to heterogeneous study designs and, more importantly, patient selection criteria. When these issues are controlled, current evidence indicates that treatment of subclinical varicocele is not warranted, as it does not seem to improve fertility. On the contrary, fair evidence indicates that varicocele treatment should be offered to infertile patients with palpable varicocele and abnormal semen parameters. This evidence supports the current guidelines issued by the American Urological Association and European Association of Urology, which state that varicocele treatment should be offered to male partners of infertile couples presenting for evaluation with clinical varicocele and semen parameters alterations.
Keywords: male infertility, review, treatment outcome varicocele, varicocelectomy
INTRODUCTION
Varicocele is the major reversible cause of male infertility. It is observed in 35%–40% of all men with primary infertility and in up to 80% of those with secondary infertility.1 The higher incidence of varicocele in men with secondary infertility suggests its progressive nature, which might be explained by a progressive testicular dysfunction involving both spermatogenesis and steroidogenesis. The negative impact of varicocele on spermatogenesis has been documented by a progressive reduction in the size of testicle ipsilateral to the varicocele.2 Since the classic work of Macleod, who described an association between infertility, abnormal semen parameters and varicocele, a multitude of studies have examined varicocele by various angles.3 Nonetheless, the exact mechanisms implicated in the pathophysiology of varicocele on male fertility are not fully understood.
Several theories have been formulated to explain the testicular impairment caused by varicocele, including hypoxia, autoimmunity, elevated testicular temperature, reflux of catecholamine, and increased oxidative stress. However, none of them can completely explain the variable modulating effect of varicocele on male fertility. Recently, the oxidative stress theory has emerged as an important contributory factor due to findings of an association between elevated reactive oxygen species and impaired sperm function in men with varicocele. Additionally, reduction of oxidative stress markers has been noted after varicocele repair. Notwithstanding, varicocele continues to be a topic of heated debate in andrology and related areas; with supporters as well as opponents of its association with subfertility.
In this review, we present historical as well as the most recent evidence of an association between varicocele treatment and natural pregnancy outcome. First, we provide data about the effect of varicocele treatment on semen characteristics, both in conventional parameters as well as in oxidative stress markers and sperm DNA damage. Then, we focus on the studies and meta-analyses evaluating the association between varicocele treatment and natural pregnancy outcome. The aim was to critically evaluate the studies’ strengths and drawbacks and therefore shed light onto the ongoing debate. Hence, we conducted an electronic search using PubMed/MEDLINE databases until July 2015. We also searched among the references of the identified articles. There were no limits placed on the year of publication, but we restricted the search to articles published in English. The search combined terms and descriptors related to natural fertility outcome (natural pregnancy OR unassisted pregnancy) after varicocelectomy OR varicocele repair OR varicocele treatment. The study was exempted from Institutional Review Board approval given that it did not involve any human intervention. Although our study was structured as a classic review rather than a systematic review, we followed the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) statement as much as possible.4
VARICOCELE TREATMENT AND POSTTREATMENT SEMEN PARAMETERS
Historical evidence
Semen parameters improvement after varicocele treatment were first reported by Tulloch in the mid-20th century, who performed high surgical ligation of varicose veins in 30 patients with infertility. The author showed a marked improvement in postoperative seminal parameters in 66% of the treated subjects.5 Thereafter, several independent studies have corroborated Tulloch's initial findings. In a case-control study, Okuyama et al. evaluated 224 subfertile men with clinical varicocele subjected to either varicocele repair by Palomo technique or expectant management. Improvements in sperm density from 11.6 × 106 ml−1 to 25.3 × 106 ml−1 (P < 0.01) and percentage of progressive motile sperm from 21.3% to 30.2% (P < 0.05) were observed in the group of treated men followed up for 12 months. The investigators also reported pregnancy rates to be higher in the group of treated men (30.6% vs 18.1% in the control group, P < 0.01).6
Recently, Shamsa et al. retrospectively evaluated 1711 patients who underwent varicocele treatment mainly by microsurgical subinguinal repair. Not only sperm concentration (by 11.9%, P < 0.001), but also sperm motility and morphology (38.3% to 41.1% and 54.5% to 56.5%, respectively, both P < 0.01) were increased postoperatively. Interestingly, the aforementioned series included seven patients who were initially azoospermic but ejaculated sperm on their postoperative ejaculates.7 Bakri et al. also reported significant improvement in sperm count in 100 men treated for subfertility who had palpable varicocele confirmed by ultrasound examination. Sperm count improved from 18.2 × 106 ml−1 to 25.1 × 106 ml−1 6 months after varicocele treatment (P = 0.01).8
Evidence from randomized controlled trials
A few randomized controlled trials (RCTs) have examined the role of varicocele treatment on postoperative semen analysis. In a study evaluating 136 infertile couples, the male partners with clinical varicocele were randomly assigned to varicocelectomy or observation. The groups were matched according to female and male age, personal background, varicocele grade, and serum hormones values. The intervention group achieved significant improvements in semen parameters. Sperm concentration increased by 75%, whereas motility and morphology by 5.2% and 8%, respectively. In contrast, there were no obvious changes in semen parameters of control subjects within the same follow-up period of 12 months.9 Abdel-Meguid et al. analyzed 145 men randomly assigned for varicocele treatment or observation from a total of 150 men intended to treat. Patient characteristics were evenly distributed among groups, including varicocele grading. There was a significant improvement in sperm concentration (18.1 × 106 ml−1 to 32.2 × 106 ml−1, P < 0.01), motility (25.3% to 41.0%, P < 0.01) and normal morphology (31.2% to 39.1%, P < 0.01) in the treatment group on a follow-up period of 12 months. No change was found on semen parameters during the follow-up period in the observation group.10
Evidence from meta-analyses
The encouraging benefits of varicocele repair to the semen parameters of subfertile men were ratified by three recent meta-analyses. Agarwal et al. pooled 17 studies that included only infertile men with clinical varicocele and with at least one abnormal semen parameter. The intervention was either high ligation of the veins or subinguinal microsurgical varicocelectomy. There was a consistent improvement in sperm concentration by 9.71 × 106 ml−1 when the microsurgical repair was used and by 12.03 × 106 ml−1 when high ligation had been performed. There were also increments in motility after high ligation (by 9.92%) and microsurgical repair (by 11.72%). Sperm morphology change was not stratified according to the type of intervention; nevertheless, there was an increment of 3.16% on the average of normal forms.11 Baazeem et al. have also evaluated the role of varicocele repair on semen analysis. They pooled 22 studies of various designs, including meta-analyses as well as randomized and nonrandomized prospective controlled studies, and analyzed sperm concentration before and after repair of clinical varicoceles in men with infertility and abnormal semen parameters. The authors found an overall increase in sperm concentration of 12.32 × 106 ml−1 from before to after interventions. In their study, sperm motility data were available from 17 prospective studies. Using the random-effects model a combined increment of 10.86% in motility was demonstrated. They also evaluated five prospective studies reporting the percentage of progressive motile sperm and confirmed that a significant improvement has occurred as well. The pooled improvement in progressive sperm motility was 9.69% using the random-effects model.12
Finally, Schauer et al. published a meta-analysis aiming to determine the impact of each type of intervention; namely, high ligation, inguinal varicocelectomy, and subinguinal varicocelectomy on the semen parameters of subfertile men. The aforementioned study pooled 14 articles including randomized controlled trials, interventional trials, and cohort studies, which accounted for 1476 subjects. Inclusion criteria comprised subfertility and/or at least one abnormal semen parameter, clinical varicocele, and 19 years of age or older. All the studied techniques led to a significant improvement in sperm count (by 10.85 × 106 ml−1 on average; P = 0.006) and motility (by 6.80% on average; P < 0.001). Only minimal differences were observed between intervention groups. The higher increment in sperm count and sperm motility was achieved by inguinal approaches, albeit of no clinical significance when compared to other techniques. The results of this meta-analysis indicated that varicocelectomy leads to significant improvements in sperm count and motility regardless of the chosen surgical technique.13
Collectively, data from these studies indicate that varicocele treatment improves semen parameters of infertile men with clinical varicocele.
VARICOCELE, OXIDATIVE STRESS, AND SPERM DNA DAMAGE
Oxidative stress and varicocele
Low and controlled concentrations of reactive oxygen species (ROS) play important roles in sperm physiological processes such as capacitation, acrosome reaction, and signaling for fertilization. However, increased ROS activity significantly impairs sperm function that can ultimately lead to infertility.14
Current evidence suggests that oxidative stress is the central element contributing to infertility in men with varicocele, to which the testis responds by way of heat stress, ischemia or production of vasodilators, such as nitric oxide.15 In one study, Sharma et al. evaluated ROS and total antioxidant capacity (TAC) scores in relation to fertility according to different male infertility diagnosis. A total of 127 patients attending an infertility clinic was enrolled, 56 varicocele patients among them, and outcome measures were compared to a group of 24 healthy and with proven fertility. Patients from the varicocele group had a higher ROS activity (2.10 log against 1.39 log in control group, P = 0.02), a decreased TAC score (1100 trolox against 1650 trolox in control group, P < 0.001) and a lower ROS-TAC score (34.87 against 50.00 in control group, P < 0.001).16 In another study, Hendin et al. evaluated ROS activity and TAC in 21 infertile men with varicocele and 17 healthy controls. The authors found an increased ROS activity (2.18 log in varicocele group against 1.30 log in control group, P = 0.02), and decreased TAC (1186 trolox equivalent against 1443 trolox equivalent, P = 0.05) in patients with varicocele. The aforementioned oxidative stress markers were also associated with decreased normal sperm morphology (r2 = −0.35, P = 0.046).17 In a meta-analysis by Agarwal et al. including four papers evaluating total seminal antioxidants by the enhanced chemiluminescence technique confirmed that elevated ROS activity and diminished TAC scores are found in patients with varicocele. The authors compared subjects with varicocele to fertile males totalizing 118 patients and 76 normal healthy controls. The mean differences in ROS and TAC concentrations were 0.73 log (P < 0.001) and −368 trolox equivalents (P < 0.001), respectively.18 In summary, infertile men with and without varicocele have elevated levels of reproductive tract ROS; however, such levels are higher in the former, thus indicating that varicocele exacerbates ROS generation and, consequently, oxidative damage to sperm.
Do ROS levels decrease after varicocelectomy?
A number of studies have investigated the effect of varicocele treatment for alleviating oxidative stress-associated infertility. In a recent review, Hamada et al. summarized the evidence and concluded that varicocelectomy was an effective treatment to decrease oxidative stress.19 Also Chen et al. examined a total of 30 patients with varicocele and evaluated the effect of varicocelectomy 6 months postoperatively. The authors reported improvements in sperm concentration, motility, and morphology; nonetheless, they noted that antioxidant levels increased even in the patients with no improvements in semen parameters. Antioxidants levels measured included seminal protein thiols and ascorbic acid. Protein thiols increased from 0.77 mg dl−1 to 3.0 mg dl−1 (P < 0.01) and ascorbic acid increased from 1.87 mg dl−1 to 3.12 mg dl−1 (P < 0.01).20 Conversely, Mancini et al. evaluating 33 men subjected to varicocelectomy did not find improvements on seminal and intracellular antioxidants, but only Coenzyme Q10 was evaluated.21 Mostafa et al. studied a larger cohort totalizing 68 infertile men. The authors examined the impact of varicocele repair on semen parameters and ROS levels. There were significant improvements in semen parameters both at 3 and 6 months postoperatively. The ROS levels followed the same trend with a progressive decrease up to 6 months in association with an increase in superoxide dismutase, catalase, glutathione peroxidase and vitamin C levels (P < 0.001). The mean improvement in superoxide dismutase seminal levels was 9.0 U ml−1 (P < 0.001) 6 months after the procedure.22
Collectively, surgical varicocele repair has been shown to be beneficial not only for alleviating oxidative stress-associated infertility but also for preventing and protecting against the progressive character of varicocele and its consequent upregulations of systemic oxidative stress.
Sperm DNA fragmentation and varicocele
Besides affecting sperm membrane sperm-oocyte fusion, ROS have been associated with sperm DNA damage.23 ROS can inflict damage to both nuclear and mitochondrial DNA, thus resulting in the base modification, strand breaks, and chromatin cross-link.24 As a consequence, poor embryo development, miscarriage, and infertility may occur.
Zini and Dohle conducted a systematic review of the literature to gather the evidence about the relationship between varicocele and sperm DNA fragmentation. The authors included seven case–control studies involving both fertile and infertile men with clinical varicocele and fertile controls, accounting for 279 subjects. In six studies, patients with varicocele had higher sperm DNA fragmentation than controls, indicating that varicocele was associated with DNA damage even when fertility had not been impaired.25 In a recent study involving a large cohort of 593 men with various etiology conditions attending infertility clinics, including 98 men with varicocele and 80 fertile controls, Esteves et al. examined the percentage of spermatozoa with fragmented DNA (SDF) using the sperm chromatin dispersion test (SCD). The highest SDF were observed in men with varicocele (35.7% ± 18.3%) and in those with leukocytospermia (41.7% ± 17.6%) compared with fertile men as well as individuals with testicular cancer and repeated ART failure (P < 0.05). Interestingly, a specific subpopulation with massive nuclear DNA damage, so-called degraded sperm, could be distinguished from the whole population of fragmented sperm. This class was not exclusive of varicocele patients, but was over-represented in this group (P < 0.001). Using receiver operating characteristics (ROC) analysis, DDSi, defined as the proportion of degraded sperm in the whole population of spermatozoa with fragmented DNA, was able to identify patients with varicocele with 94% accuracy.26
Do sperm DNA damage decrease after varicocelectomy?
In 2011, Zini et al. evaluated sperm DNA damage before and after subinguinal microsurgical varicocelectomy in 25 patients with palpable varicocele. The DNA fragmentation index (DFI) was significantly decreased from 18% to 11% (P < 0.001) after treatment.27 Recently, Li et al. evaluated 19 men with varicocele and infertility and 19 healthy controls with normal semen analysis. The authors found higher DFI in the varicocele group, but a marked improvement in sperm concentration, motility, and morphology that was accompanied by a decrease in DFI from 28.4% to 22.4% (P = 0.018) occurred after varicocele repair.28
In a larger cohort study, Smit et al. evaluated 49 men with palpable varicocele and infertility. Semen parameters improved while DFI decreased from 35.2% to 30.2% (P = 0.019) 3 months postoperatively. The aforementioned authors also reported that 37% of the couples conceived naturally after an average of 7.2 months after varicocele repair.29 Recently, Telli et al. evaluated 72 men with varicocele and infertility subjected to varicocelectomy. The authors noted that semen parameters and DFI were improved 3 months after varicocelectomy.30 A meta-analysis of 6 studies, including 177 patients with varicocele, evaluated the effect size of varicocelectomy on sperm DNA damage. The authors reported that varicocelectomy improve sperm DNA integrity with a mean difference of −3.37% (95% CI: −4.09–−2.65).31
A summary of the studies examining sperm DNA damage and pre- and post-varicocele surgery indicates that treatment is associated with improvements in sperm nuclear DNA integrity. Due to the low magnitude of the effect size, further research is needed to elucidate the clinical significance of varicocelectomy on sperm DNA damage.
VARICOCELE AND NATURAL PREGNANCY RATES
The debate about the role of varicocelectomy in male infertility lay on the actual benefit of intervention to improve natural fertility. Several studies attempting to investigate this issue, including randomized controlled trials (RCT) and meta-analyses, have yielded equivocal results. Given the multitude of variables that influence fertility, it is important to discuss critically the outcome of each study taking into consideration the inclusion of patients with subclinical varicocele, varicocele grade, duration of follow-up, surgical technique and cohort size.
Subclinical and low-grade varicocele and pregnancy rates
Yamamoto et al. specifically studied the effect of varicocelectomy in men with either subclinical or grade 1 varicocele. The authors enrolled 85 patients with infertility who were randomized into high ligation or observation. Despite noting improvements in the semen parameters of treated men, similar pregnancy rates (10% in varicocelectomy group and 6.7% in control group, P = 0.758) were observed after 1 year follow-up. The authors concluded that varicocelectomy might improve spermatogenesis; however, pregnancy was not affected.32 Unal et al. also evaluated patients with subclinical varicocele. The authors randomized 42 patients to varicocelectomy or medical therapy with clomiphene citrate, a selective estrogen receptor modulator, and evaluated the impact of varicocele repair in this specific subset of patients. In a median follow-up of 15 months, only 1 and 2 pregnancies were achieved in the medical therapy and varicocelectomy groups, respectively. Despite the small cohort analyzed, the authors concluded that varicocelectomy was not superior to medical therapy in patients with subclinical varicocele.33
As far as low-grade varicocele is concerned, Grasso et al. conducted an RCT with 68 infertile couples in whom the male partners had grade 1 varicocele associated with semen abnormalities. Patients were allocated to observation or varicocele repair using either the Palomo technique or ligation of dilated veins through the inguinal approach. The follow-up period was 12 months, and natural pregnancies were recorded. There were no differences in semen parameters and pregnancy rates of treated compared with untreated men. Overall, the pregnancy rate was 4.4%; the authors concluded that there was no substantial evidence to recommend treatment to men with grade 1 varicocele.34
Clinical varicocele and natural pregnancy rates
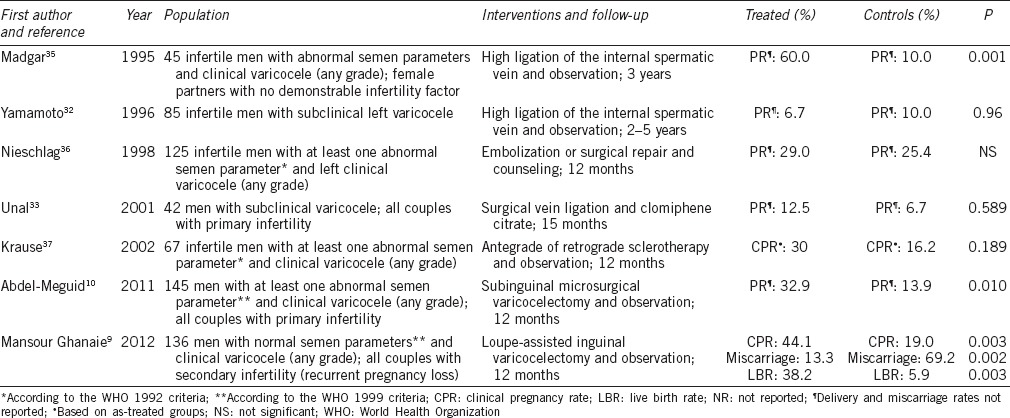
The effect of varicocele treatment to improve natural fertility in men with clinical varicocele has been debated since the classic work of Madgar et al. in 1995. The authors enrolled 45 couples in whom varicocele had been the only factor implicated in the couple's inability to conceive. All subjects had a clinical varicocele and semen abnormalities. Patients were randomized to high ligation of dilated veins at the beginning of the study or after 1 year if the pregnancy had not occurred. In the observation and treatment groups, respectively, 10% and 60% of couples achieved a natural pregnancy. Then, patients in the observation group were submitted to varicocele repair, and the pregnancy rate in the subsequent year was 44.4%. Both groups were observed for two additional years, and the authors observed that most of the pregnancies occurred 12 months after the procedure.35 The results of this study provided strong evidence that varicocelectomy was able to increase natural pregnancy rates.
On the contrary, other RCTs could not corroborate Madgar et al. observations. In one study, Nieschlag et al. studied 125 couples with no demonstrable infertility factor other than varicocele. The male partners were subjected to treatment (surgical ligation or embolization) or counseling. There was a significant improvement in sperm concentration in the intervention group, but pregnancy rates were not different between treated (29%) and untreated (25.4%) couples.36 In another RCT, Krause et al. studied a cohort of 67 patients assigned to sclerotherapy or no treatment. However, some patients initially assigned to observation group were actually treated during the study. An analysis based on the intention to treat did not yield differences in pregnancy rates. When further analysis “per treatment” was conducted, a 30% pregnancy rate was recorded in the treated group compared to 16.2% in the observation group, albeit of no statistical significance. The authors commented that the study was initially designed to include 460 patients to have enough power, but instead, only 67 patients were included.37
Giagulli and Carbone in a nonrandomized study including 137 patients subjected to varicocele treatment and 185 patients to expectant management did not find a difference in the overall pregnancy rates between treated and untreated groups. Both groups were followed for 12 months. Notably, a subgroup analysis showed that individuals with infertility duration of more than 2 years and who had their varicoceles treated achieved higher pregnancy rate than the untreated counterparts (26% vs 13.4%, P = 0.02). The authors concluded that couples with infertility longer than 2 years could benefit from varicocele repair to restore natural fertility.38
In a well-designed, prospective, randomized controlled trial by Abdel-Meguid et al. 145 participants underwent varicocele treatment (subinguinal microsurgical varicocelectomy) or observation. During a 12-month period, pregnancies were registered. The natural pregnancy rate was 32.9% in the varicocelectomy group and 13.9% in the observation group. The odds for natural pregnancy favored the treated group (OR: 3.04; 95% CI: 1.33–6.95).10 Mansour Ghanaie et al. conducted an RCT to evaluate the effects of varicocele treatment in couples with first-term recurrent miscarriage. The main outcome was live birth rate. All included patients had clinically palpable varicocele, and the couples were randomly assigned to varicocele repair or observation. During a follow-up period of 12 months, 30 pregnancies (44.1%) were registered in the treated group and 13 (19%) in the expectant group (P < 0.05).9 A summary of the studies examining the role of varicocele repair on natural pregnancy rates is provided in Table 1.
Table 1.
Randomized controlled trials of varicocelectomy and its effect on natural pregnancy rates
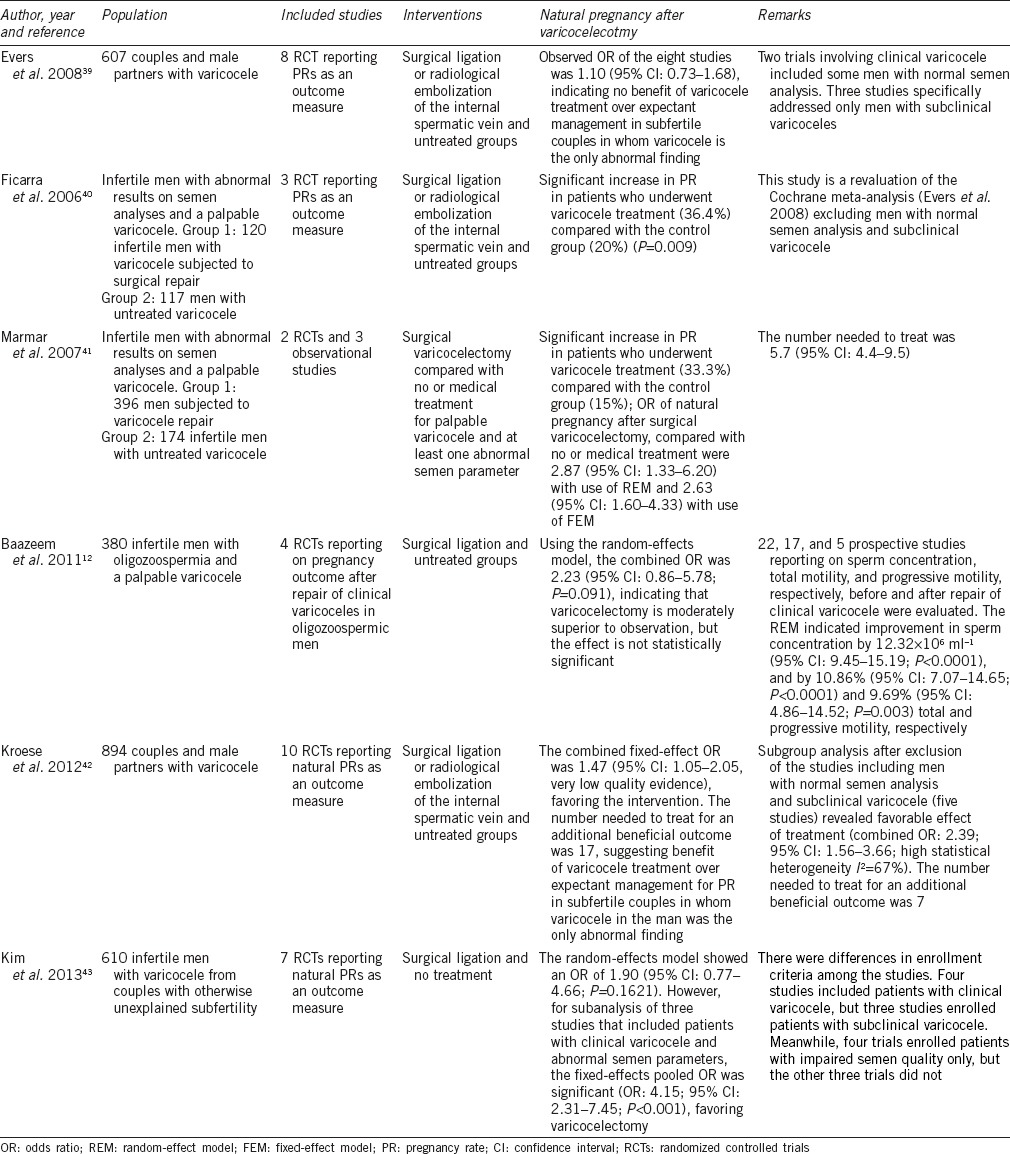
Several meta-analyses have also evaluated the effect of varicocelectomy on natural pregnancy rates. In an early study by the Cochrane Institute involving eight studies, no benefit from varicocele treatment compared to counseling was verified regarding the odds of pregnancy (OR: 1.10; 95% CI: 0.73–1.68).39 A major critique to this study was the inclusion of patients with subclinical varicocele and/or normal semen characteristics. Hence, Ficarra et al. reviewed the randomized clinical trials for varicocele repair taking into consideration only patients with clinical varicocele and abnormal semen analyses. The authors included three RCT and found that pregnancy rates were higher in the group of treated patients (36.4%) compared with untreated counterparts (20%; P = 0.009).40 In a subsequent meta-analysis by Marmar et al. involving five studies and 570 patients, the authors reported significantly higher chances for pregnancy after varicocelectomy than either no treatment or medication in patients with clinical varicoceles and at least one abnormal semen parameter (OR: 2.87; 95% CI: 1.33–6.20; P < 0.001).41 However unlike previous meta-analyses, the study of Marmar et al. included RCT as well as observational studies scored for bias.
Later in 2011, Baazeem et al. assessed both randomized and nonrandomized trials involving varicocelectomy in men with clinical varicocele and oligozoospermia. Considering only the four RCTs reporting natural pregnancy the combined odds ratio using the random-effect model was 2.23 (95% CI: 0.86–5.78; P = 0.091). The authors identified a number of studies reporting sperm concentration, total motility, and progressive motility before and after varicocelectomy. The random-effects model indicated that sperm concentration was increased by 12.32 × 106 ml−1 (95% CI: 9.45–15.19; P < 0.0001). There were marked increases in total motility (10.86%, 95% CI: 7.07–14.65%; P < 0.0001) and progressive motility as well (9.69%, 95% CI: 4.86–14.52; P = 0.003). The authors concluded that varicocelectomy was moderately superior to observation, but the effect was not statistically significant. And added that varicocelectomy was associated with a significant increase in sperm concentration as well as total and progressive motility.12
Recently in 2012, the Cochrane Institute published a revised meta-analysis on the effects of varicocele treatment (surgery or embolization) in subfertility. The meta-analysis included ten RCTs involving 894 men. None of the studies reported live birth. The combined fixed-effect odds ratio of the 10 studies for the outcome of pregnancy was 1.47 (95% CI: 1.05–2.05) favoring the intervention. The number needed to treat for an additional pregnancy was 17, suggesting a benefit of varicocele treatment over expectant management in subfertile couples in whom varicocele was the only abnormal finding. The omission of studies that included men with normal semen analysis and subclinical varicocele was the subject of a planned subgroup analysis. The outcome of the subgroup analysis (five studies) also favored treatment, with a combined OR of 2.39 (95% CI: 1.56–3.66). The number needed to treat for an additional beneficial outcome was 7. The evidence was suggestive rather than conclusive, as the main analysis was subject to fairly high statistical heterogeneity (I2 = 67%), and findings were no longer significant when the random-effects model was used or when the analysis was restricted to higher quality studies. The authors concluded that there is evidence suggesting that treatment of varicocele in men from couples with otherwise unexplained subfertility may improve a couple's chance of pregnancy. However, the authors commented about the quality of the available evidence being very low, and that more research is needed with live birth or pregnancy rate as the primary outcome.42 Finally in 2013, Kim et al. pooled 610 patients from seven RCTs reporting pregnancy outcome after surgical repair of varicocele in men from couples with otherwise unexplained infertility. Due to the significant heterogeneity among the included studies, the random-effects model was applied. A combined OR of 1.90 (95% CI: 0.77–4.66) was obtained, thus suggesting that varicocelectomy was not superior to observation. To analyze the potential causes of heterogeneity, the authors performed a subgroup analysis pooling only the three studies (312 patients) that included patients with clinical varicocele. Of note, heterogeneity was markedly decreased and the fixed-effect model indicated a combined OR of 4.15 (95% CI: 2.31–7.45) favoring varicocele treatment.43 A summary of the meta-analyses examining the role of varicocele repair on natural pregnancy rates is provided in Table 2.
Table 2.
Meta-analyzes of varicocelectomy and its effect on natural pregnancy rates
Collectively, data from the aforementioned studies suggest that treatment of subclinical varicocele is not warranted, as it does not seem to improve fertility. On the contrary, fair evidence indicates that varicocele treatment should be offered to infertile patients with palpable varicocele and abnormal semen parameters. This evidence supports the current guidelines issued by the American Urological Association and European Association of Urology, which state that varicocele treatment should be offered to patients from infertile couples presenting for evaluation with semen parameters alterations.
CONCLUSIONS
Varicocelectomy is believed to improve one or more semen parameters in the majority of the treated subjects. A significant attenuation of oxidative stress markers occurs after varicocelectomy, and significant improvements in sperm DNA integrity has been demonstrated in infertile men after varicocele repair. Conflicting results obtained from different studies attempting to answer to the question of whether or not varicocelectomy improves natural fertility seems to be due to heterogeneous study designs and, more importantly, patient selection criteria. No definitive randomized prospective clinical trial of sufficient size exists at this time due to the inherent difficulties of establishing such a trial and enrolling infertility patients. In the absence of such a trial, critical assessment of the best quality data available leads to the conclusion that varicocelectomy can benefit properly selected infertile men.
AUTHOR CONTRIBUTIONS
BCT participated in the acquisition of data, summarized the collected evidence and helped to draft the manuscript. SCE participated in data analysis and helped to draft the manuscript. MSC designed the study, participated in the acquisition of data and helped to draft the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
The authors declare no competing interests.
REFERENCES
- 1.Gorelick JI, Goldstein M. Loss of fertility in men with varicocele. Fertil Steril. 1993;59:613–6. [PubMed] [Google Scholar]
- 2.Lipshultz LI, Corriere JN., Jr Progressive testicular atrophy in the varicocele patient. J Urol. 1977;117:175–6. doi: 10.1016/s0022-5347(17)58387-1. [DOI] [PubMed] [Google Scholar]
- 3.MacLeod J. Seminal cytology in the presence of varicocele. Fertil Steril. 1965;16:735–57. doi: 10.1016/s0015-0282(16)35765-x. [DOI] [PubMed] [Google Scholar]
- 4.Stewart LA, Clarke M, Rovers M, Riley RD, Simmonds M, et al. Preferred reporting items for systematic review and meta-analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–65. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 5.Tulloch WS. Varicocele in subfertility; results of treatment. Br Med J. 1955;2:356–8. doi: 10.1136/bmj.2.4935.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Okuyama A, Fujisue H, Matsui T, Doi Y, Takeyama M, et al. Surgical repair of varicocele: effective treatment for subfertile men in a controlled study. Eur Urol. 1988;14:298–300. doi: 10.1159/000472964. [DOI] [PubMed] [Google Scholar]
- 7.Shamsa A, Nademi M, Aqaee M, Fard AN, Molaei M. Complications and the effect of varicocelectomy on semen analysis, fertility, early ejaculation and spontaneous abortion. Saudi J Kidney Dis Transpl. 2010;21:1100–5. [PubMed] [Google Scholar]
- 8.Al Bakri A, Lo K, Grober E, Cassidy D, Cardoso JP, et al. Time for improvement in semen parameters after varicocelectomy. J Urol. 2012;187:227–31. doi: 10.1016/j.juro.2011.09.041. [DOI] [PubMed] [Google Scholar]
- 9.Mansour Ghanaie M, Asgari SA, Dadrass N, Allahkhah A, Iran-Pour E, et al. Effects of varicocele repair on spontaneous first trimester miscarriage: a randomized clinical trial. Urol J. 2012;9:505–13. [PubMed] [Google Scholar]
- 10.Abdel-Meguid TA, Al-Sayyad A, Tayib A, Farsi HM. Does varicocele repair improve male infertility?. An evidence-based perspective from a randomized, controlled trial. Eur Urol. 2011;59:455–61. doi: 10.1016/j.eururo.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532–8. doi: 10.1016/j.urology.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 12.Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, et al. Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol. 2011;60:796–808. doi: 10.1016/j.eururo.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Schauer I, Madersbacher S, Jost R, Hubner WA, Imhof M. The impact of varicocelectomy on sperm parameters: a meta-analysis. J Urol. 2012;187:1540–7. doi: 10.1016/j.juro.2011.12.084. [DOI] [PubMed] [Google Scholar]
- 14.Saleh RA, Agarwal A. Oxidative stress and male infertility: from research bench to clinical practice. J Androl. 2002;23:737–52. [PubMed] [Google Scholar]
- 15.Agarwal A, Hamada A, Esteves SC. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol. 2012;9:678–90. doi: 10.1038/nrurol.2012.197. [DOI] [PubMed] [Google Scholar]
- 16.Sharma RK, Pasqualotto FF, Nelson DR, Thomas AJ, Jr, Agarwal A. The reactive oxygen species-total antioxidant capacity score is a new measure of oxidative stress to predict male infertility. Hum Reprod. 1999;14:2801–7. doi: 10.1093/humrep/14.11.2801. [DOI] [PubMed] [Google Scholar]
- 17.Hendin BN, Kolettis PN, Sharma RK, Thomas AJ, Jr, Agarwal A. Varicocele is associated with elevated spermatozoal reactive oxygen species production and diminished seminal plasma antioxidant capacity. J Urol. 1999;161:1831–4. [PubMed] [Google Scholar]
- 18.Agarwal A, Prabakaran S, Allamaneni SS. Relationship between oxidative stress, varicocele and infertility: a meta-analysis. Reprod Biomed Online. 2006;12:630–3. doi: 10.1016/s1472-6483(10)61190-x. [DOI] [PubMed] [Google Scholar]
- 19.Hamada A, Esteves SC, Agarwal A. Insight into oxidative stress in varicocele-associated male infertility: part 2. Nat Rev Urol. 2013;10:26–37. doi: 10.1038/nrurol.2012.198. [DOI] [PubMed] [Google Scholar]
- 20.Chen SS, Huang WJ, Chang LS, Wei YH. Attenuation of oxidative stress after varicocelectomy in subfertile patients with varicocele. J Urol. 2008;179:639–42. doi: 10.1016/j.juro.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 21.Mancini A, Milardi D, Conte G, Festa R, De Marinis L, et al. Seminal antioxidants in humans: preoperative and postoperative evaluation of coenzyme Q10 in varicocele patients. Horm Metab Res. 2005;37:428–32. doi: 10.1055/s-2005-870232. [DOI] [PubMed] [Google Scholar]
- 22.Mostafa T, Anis TH, El-Nashar A, Imam H, Othman IA. Varicocelectomy reduces reactive oxygen species levels and increases antioxidant activity of seminal plasma from infertile men with varicocele. Int J Androl. 2001;24:261–5. doi: 10.1046/j.1365-2605.2001.00296.x. [DOI] [PubMed] [Google Scholar]
- 23.Aitken RJ. The role of free oxygen radicals and sperm function. Int J Androl. 1989;12:95–7. doi: 10.1111/j.1365-2605.1989.tb01290.x. [DOI] [PubMed] [Google Scholar]
- 24.Ozmen B, Koutlaki N, Youssry M, Diedrich K, Al-Hasani S. DNA damage of human spermatozoa in assisted reproduction: origins, diagnosis, impacts and safety. Reprod Biomed Online. 2007;14:384–95. doi: 10.1016/s1472-6483(10)60883-8. [DOI] [PubMed] [Google Scholar]
- 25.Zini A, Dohle G. Are varicoceles associated with increased deoxyribonucleic acid fragmentation? Fertil Steril. 2011;96:1283–7. doi: 10.1016/j.fertnstert.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Esteves SC, Gosalvez J, Lopez-Fernandez C, Nunez-Calonge R, Caballero P, et al. Diagnostic accuracy of sperm DNA degradation index (DDSi) as a potential noninvasive biomarker to identify men with varicocele-associated infertility. Int Urol Nephrol. 2015;47:1471–7. doi: 10.1007/s11255-015-1053-6. [DOI] [PubMed] [Google Scholar]
- 27.Zini A, Azhar R, Baazeem A, Gabriel MS. Effect of microsurgical varicocelectomy on human sperm chromatin and DNA integrity: a prospective trial. Int J Androl. 2011;34:14–9. doi: 10.1111/j.1365-2605.2009.01048.x. [DOI] [PubMed] [Google Scholar]
- 28.Li F, Yamaguchi K, Okada K, Matsushita K, Ando M, et al. Significant improvement of sperm DNA quality after microsurgical repair of varicocele. Syst Biol Reprod Med. 2012;58:274–7. doi: 10.3109/19396368.2012.692431. [DOI] [PubMed] [Google Scholar]
- 29.Smit M, Romijn JC, Wildhagen MF, Veldhoven JL, Weber RF, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2013;189:S146–50. doi: 10.1016/j.juro.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 30.Telli O, Sarici H, Kabar M, Ozgur BC, Resorlu B, et al. Does varicocelectomy affect DNA fragmentation in infertile patients? Indian J Urol. 2015;31:116–9. doi: 10.4103/0970-1591.152811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang YJ, Zhang RQ, Lin YJ, Zhang RG, Zhang WL. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online. 2012;25:307–14. doi: 10.1016/j.rbmo.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 32.Yamamoto M, Hibi H, Hirata Y, Miyake K, Ishigaki T. Effect of varicocelectomy on sperm parameters and pregnancy rate in patients with subclinical varicocele: a randomized prospective controlled study. J Urol. 1996;155:1636–8. [PubMed] [Google Scholar]
- 33.Unal D, Yeni E, Verit A, Karatas OF. Clomiphene citrate versus varicocelectomy in treatment of subclinical varicocele: a prospective randomized study. Int J Urol. 2001;8:227–30. doi: 10.1046/j.1442-2042.2001.00289.x. [DOI] [PubMed] [Google Scholar]
- 34.Grasso M, Lania C, Castelli M, Galli L, Franzoso F, et al. Low-grade left varicocele in patients over 30 years old: the effect of spermatic vein ligation on fertility. BJU Int. 2000;85:305–7. doi: 10.1046/j.1464-410x.2000.00437.x. [DOI] [PubMed] [Google Scholar]
- 35.Madgar I, Weissenberg R, Lunenfeld B, Karasik A, Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil Steril. 1995;63:120–4. doi: 10.1016/s0015-0282(16)57306-3. [DOI] [PubMed] [Google Scholar]
- 36.Nieschlag E, Hertle L, Fischedick A, Abshagen K, Behre HM. Update on treatment of varicocele: counselling as effective as occlusion of the vena spermatica. Hum Reprod. 1998;13:2147–50. doi: 10.1093/humrep/13.8.2147. [DOI] [PubMed] [Google Scholar]
- 37.Krause W, Muller HH, Schafer H, Weidner W. Does treatment of varicocele improve male fertility? results of the ‘Deutsche Varikozelenstudie’, a multicentre study of 14 collaborating centres. Andrologia. 2002;34:164–71. doi: 10.1046/j.1439-0272.2002.00494.x. [DOI] [PubMed] [Google Scholar]
- 38.Giagulli VA, Carbone MD. Varicocele correction for infertility: which patients to treat? Int J Androl. 2011;34:236–41. doi: 10.1111/j.1365-2605.2010.01081.x. [DOI] [PubMed] [Google Scholar]
- 39.Evers JH, Collins J, Clarke J. Surgery or embolisation for varicoceles in subfertile men. Cochrane Database Syst Rev. 2008;16:CD000479. doi: 10.1002/14651858.CD000479.pub3. [DOI] [PubMed] [Google Scholar]
- 40.Ficarra V, Cerruto MA, Liguori G, Mazzoni G, Minucci S, et al. Treatment of varicocele in subfertile men: the Cochrane review – A contrary opinion. Eur Urol. 2006;49:258–63. doi: 10.1016/j.eururo.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 41.Marmar JL, Agarwal A, Prabakaran S, Agarwal R, Short RA, et al. Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysis. Fertil Steril. 2007;88:639–48. doi: 10.1016/j.fertnstert.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 42.Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012;10:CD000479. doi: 10.1002/14651858.CD000479.pub5. [DOI] [PubMed] [Google Scholar]
- 43.Kim KH, Lee JY, Kang DH, Lee H, Seo JT, et al. Impact of surgical varicocele repair on pregnancy rate in subfertile men with clinical varicocele and impaired semen quality: a meta-analysis of randomized clinical trials. Korean J Urol. 2013;54:703–9. doi: 10.4111/kju.2013.54.10.703. [DOI] [PMC free article] [PubMed] [Google Scholar]


