Abstract
Varicocele affects approximately 35%–40% of men presenting for an infertility evaluation. There is fair evidence indicating that surgical repair of clinical varicocele improves semen parameters, decreases seminal oxidative stress and sperm DNA fragmentation, and increases the chances of natural conception. However, it is unclear whether performing varicocelectomy in men with clinical varicocele prior to assisted reproductive technology (ART) improve treatment outcomes. The objective of this study was to evaluate the role of varicocelectomy on ART pregnancy outcomes in nonazoospermic infertile men with clinical varicocele. An electronic search was performed to collect all evidence that fitted our eligibility criteria using the MEDLINE and EMBASE databases until April 2015. Four retrospective studies were included, all of which involved intracytoplasmic sperm injection (ICSI), and accounted for 870 cycles (438 subjected to ICSI with prior varicocelectomy, and 432 without prior varicocelectomy). There was a significant increase in the clinical pregnancy rates (OR = 1.59, 95% CI: 1.19–2.12, I2 = 25%) and live birth rates (OR = 2.17, 95% CI: 1.55–3.06, I2 = 0%) in the varicocelectomy group compared to the group subjected to ICSI without previous varicocelectomy. Our results indicate that performing varicocelectomy in patients with clinical varicocele prior to ICSI is associated with improved pregnancy outcomes.
Keywords: assisted reproductive techniques, meta-analysis, pregnancy outcome, systematic review, varicocele, varicocelectomy
INTRODUCTION
Varicocele is defined as a dilatation of the pampiniform plexus veins. It is the most common cause of male infertility affecting about 15%–20% of the general population and 35%–40% of men presenting for an infertility evaluation.1,2,3 Until now, the exact mechanisms that ultimately lead to infertility are not fully understood despite the fact that varicocele pathophysiology has been discussed for close to five decades. The main theories postulate that venous reflux leading to elevated testicular temperature and oxidative stress are the key elements.4,5 Equally debatable is the actual benefit of interventions although recent evidence indicates that treatment may improve the chance of pregnancy in subfertile couples in whom varicocele is the only abnormal finding.6,7
Oxidative stress and elevated sperm DNA fragmentation have been associated with varicocele-mediated infertility.4,6,7,8,9,10,11 Although sperm with fragmented DNA can fertilize oocytes with apparently similar efficiency to sperm without DNA fragmentation, it has been found that high DNA fragmentation negatively impacts embryo development and may jeopardize pregnancy outcomes in assisted reproductive technology (ART).12,13 There is fair evidence indicating that surgical repair of clinical varicocele improves sperm parameters, decreases seminal oxidative stress and sperm DNA fragmentation, and increases seminal antioxidants.6,7,14,15 However, it is unclear whether performing varicocelectomy in infertile males with clinical varicocele prior to ART improves treatment outcomes.16
The objective of this study was to collect and summarize all evidence that evaluated the benefit of varicocelectomy on ART outcomes in nonazoospermic infertile men with clinical varicocele.
MATERIALS AND METHODS
We followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement to report the results of this review.17 The study was exempted from Institutional Review Board approval as it did not involve any interventions in humans.
Search strategy
An exhaustive electronic search was performed using the MEDLINE and EMBASE databases up to April 2015. There were no limits placed on the year of publication, but we restricted the search to articles published in English. We also searched among the references of the identified articles. The search combined relevant terms and descriptors related to varicocele, varicocelectomy, varicocele repair, IVF, ICSI, and ART.
Eligibility criteria and data extraction
This systematic review and meta-analysis included studies comparing ART outcomes of nonazoospermic patients with clinical varicocele who underwent varicocelectomy prior to ART to those without prior varicocele repair. Clinical varicoceles were considered as those diagnosed based on the finding of varicose veins in the spermatic cord either by visual inspection or palpation with or without the aid of the Valsalva maneuver during physical examination with the patient standing.18 ART was defined as all treatments or procedures that include the in vitro handling of both human oocytes and sperm or of embryos for the purpose of establishing a pregnancy. This included in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) and embryo transfer.19 For the purpose of this review, ART did not include assisted insemination (artificial insemination) using sperm from either a woman's partner or a donor.
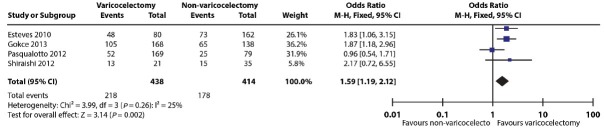
The selection criteria are described in Table 1. In the first screening, two independent authors (M.R. and S.C.E.) assessed all of the abstracts retrieved from the search and then obtained the full manuscripts of the citations that met the inclusion criteria. These authors evaluated the studies’ eligibility and quality, and they subsequently extracted the data. Any discrepancies were solved by agreement and, if needed, they reached a consensus with the third author (A.A.).
Table 1.
Selection criteria of included studies (PICOS)
Outcome measures
The pregnancy rates, both clinical pregnancy and live birth, were the primary outcomes of interest. Secondary outcomes included fertilization rate, implantation rate, and miscarriage rate. Clinical pregnancy was defined as a pregnancy observed sonographically by the visualization of a fetal heartbeat by 7 weeks of gestation. The clinical pregnancy rate was the number of clinical pregnancies expressed per 100 embryo transfers. The live birth rate was defined as the ratio between the number of deliveries resulting in at least one live birth and the number of embryo transfers. Miscarriage was defined as a nonviable clinical pregnancy on ultrasound follow-up until gestational week 20. The implantation rate was defined as the number of gestational sacs observed sonographically divided by the number of transferred embryos. The fertilization rate was defined by the number of two pronuclei zygotes divided by the number of metaphase II oocytes subjected to sperm injections.
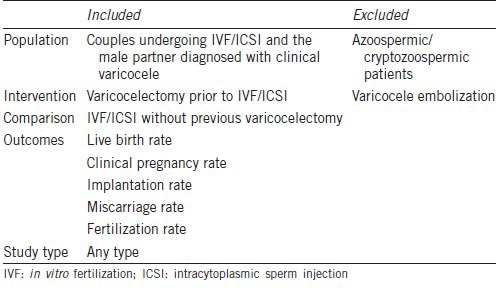
Risk of bias assessment
We followed the guidance recommended by the Cochrane Collaboration to assess the risk of bias from the included studies.20 We evaluated sequence generation, allocation concealment, blinding, and incomplete outcome data for each trial included in the review. A low risk of bias was considered when a judgment of “yes” for all domains was obtained, whereas a high risk of bias was considered when a judgment of “no” for one or more domains was obtained. An unclear risk of bias was defined when an “unclear” judgment in any domain was considered. The quality assessment of the included trials is shown in Table 2.
Table 2.
Quality assessment of included trials
Analysis
We pooled the data of the dichotomous outcomes from the original studies to obtain the odds ratio (OR) for the occurrence of an outcome event and presented their corresponding 95% confidence intervals (CIs). Statistical significance was set at P < 0.05. To quantify statistical heterogeneity, we used the I2 statistic in order to describe the variations across trials that were due to heterogeneity and not to sampling error. We pooled the outcome data from each study using a Mantel-Haenszel model and applied the fixed-effects model. When the heterogeneity was >50% (I2 > 50%), we applied the random-effects model.21 We used the Review Manager 5 software (Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) to conduct the meta-analysis. It was not possible to perform a meta-analysis for implantation, miscarriage, and fertilization rates due the nature of the studies evaluating these outcomes.
RESULTS
Our electronic search retrieved 114 articles. After screening the titles and abstracts, we determined that six articles were eligible for inclusion. Among these, two articles were excluded. One of them was a review article,22 and the other study did not fulfill the inclusion criteria23 as the primary comparison was between patients submitted to varicocelectomy and observation. Although the authors of this aforementioned study evaluated ART outcomes in patients who did not achieve natural pregnancy after varicocele repair, they have included intrauterine insemination as an ART treatment modality. As stated in the eligibility criteria, the objective of our study was to compare only patients submitted to ART as per the ICMART definition. The complete selection process is depicted in Figure 1.
Figure 1.
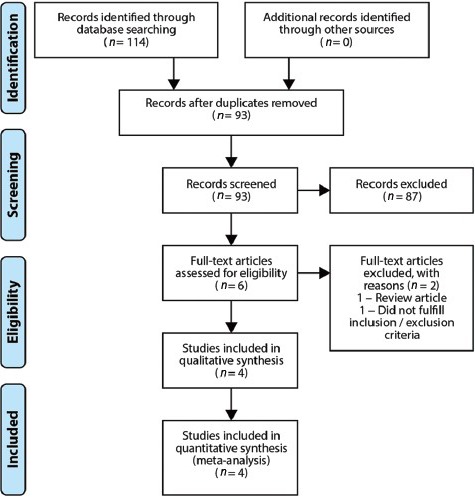
Flowchart showing the identification and selection process of studies included in the meta-analysis.
Description of the included studies
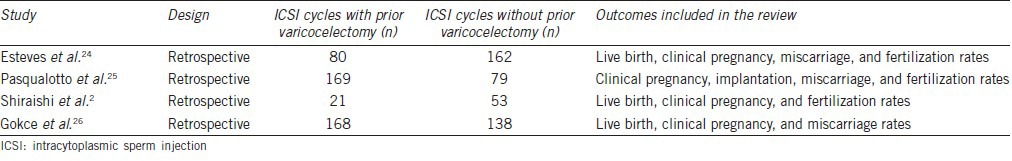
Four retrospective studies were included, all of which involved ICSI as the ART method.2,24,25,26 The four included studies accounted for 870 ICSI cycles (438 with prior varicocelectomy, and 432 without prior varicocelectomy). In three of the included studies, the patients subjected to varicocelectomy had undergone microsurgical subinguinal varicocele repair.24,25,26 The characteristics of the studies included in this review are presented in Table 3. Only two of the studies provided information about the interval between varicocelectomy and ICSI.24,26 In the study by Esteves et al., the mean interval between the operation and ART was 6.2 months (range 4 to 13) while it was 7.2 ± 2.8 months in the study by Gokce et al.24,26 Two of the studies stated that only patients without varicocele recurrence were enrolled in the analysis.24,25 As far as the varicocele grade is concerned, none of the included studies analyzed the association between varicocele grade and ART outcomes.
Table 3.
Characteristics of the included studies
Outcomes
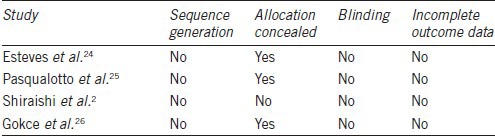
Clinical pregnancy rate
All four included studies reported data on clinical pregnancy (Table 4).2,24,25,26 There was a statistically significant increase in the pregnancy rate in three of the studies, favoring the group with prior varicocelectomy.2,24,26 In one of the studies, the authors did not find a statistically significant difference between the groups with and without previous varicocele repair.25 Overall, there was a significant increase in the clinical pregnancy rate by ICSI with prior varicocelectomy compared with nonvaricocelectomy (OR = 1.59, 95% CI: 1.19–2.12,I2 = 25%) (Figure 2).
Table 4.
ICSI outcome in infertile men with treated and untreated clinical varicocele
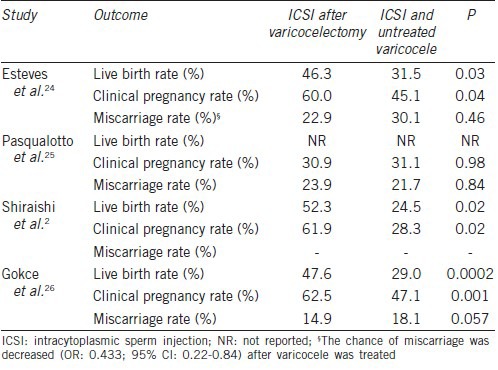
Figure 2.
Forest plot of comparison: 1 Varicocelectomy + ICSI versus ICSI without varicocelectomy, outcome: Clinical pregnancy.
Live birth rate
Three of the included studies reported data on live birth.2,24,26 All of them reported statistically increased live birth rates in the group of patients that have undergone varicocelectomy prior to the ICSI procedure (Table 4). A significant benefit on live birth rates was found for varicocelectomy plus ICSI compared to ICSI without previous varicocelectomy (OR = 2.17, 95% CI: 1.55–3.06, I2 = 0%) (Figure 3).
Figure 3.
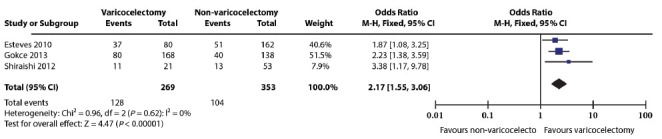
Forest plot of comparison: Varicocelectomy + ICSI versus ICSI without varicocelectomy, outcome: Live birth.
Implantation rate
Only one of the included studies evaluated implantation.25 It was observed that the implantation rate was not statistically different in the group subjected to varicocelectomy (17.3%) compared to the one without varicocelectomy (22.1%) (Table 4).
Miscarriage rate
There were three studies evaluating miscarriage.24,25,26 One of them found that the chance of miscarriage was decreased (OR: 0.433; 95% CI: 0.22-0.84) after varicocele was treated.24 Two of them did not find statistically significant differences between the two groups (Table 4).25,26
Fertilization rate
Three of the included studies evaluated fertilization after sperm injections. Esteves et al. found statistically significant differences between the two groups (78% vs 66%, P = 0.04), favoring the group with prior varicocelectomy.24 In contrast, Pasqualotto et al.25 found statistically significant differences between the two groups (64.9% vs 73.2%, P = 0.03), favoring the group without varicocele repair. Finally, Shiraishi et al.2 did not find statistically significant differences between the two groups (70.3% vs 68.6%).
DISCUSSION
To our knowledge, this is the first systematic review and meta-analysis addressing the potential benefits of varicocelectomy on ART outcomes in nonazoospermic infertile men with clinical varicocele. Our study included only nonazoospermic patients with clinical varicocele who either underwent or did not undergo varicocelectomy prior to ICSI. Our electronic search did not retrieve any study that evaluated conventional IVF as the ART treatment method. Our findings, which included 870 ICSI cycles, indicated that varicocelectomy prior to ICSI resulted in significantly higher pregnancy rates compared to ICSI without varicocele repair. All included studies reported data on clinical pregnancy, and there was a significant increase in the clinical pregnancy rate with varicocelectomy compared with nonvaricocelectomy (OR = 1.59, 95% CI: 1.19–2.12, I2 = 25%). Three of the four included studies evaluated live birth rates, and a statistically significant increase in live birth rates was also observed in patients with clinical varicocele subjected to microsurgical varicocelectomy prior to ICSI (OR = 2.17, 95% CI: 1.55–3.06, I2 = 0%).
Although ICSI is an efficient treatment modality for severe male factor infertility, including varicocele as the underlying cause, the procedure does not take into account for the possibility that the selected spermatozoa have damaged DNA.12 Sperm DNA fragmentation has been associated with poorer results in ART treatment27,28,29,30,31,32 though this association is not conclusive.33,34,35 The results of a recent meta-analysis showed a significant decrease in pregnancy using sperm with high DNA damage in IVF cycles, whereas there was no difference in pregnancy rates in ICSI cycles.36 These differences might be explained by inherent distinction in the population treated and sperm handling techniques used by IVF and ICSI methods,37 and reinforce the importance of performing further investigation to evaluate the correlation between sperm DNA damage and IVF/ICSI outcomes.
Despite the fact that none of the included studies had evaluated sperm functional factors, an improvement in sperm function would be a plausible explanation for the observed beneficial effect of prior varicocelectomy on ICSI outcomes. Of note, three of the included studies reported semen analysis results, and in two of them, a significant improvement in sperm count and motility was observed after varicocelectomy.24,26 It has been shown that patients with a postoperatively improved semen quality are more likely to achieve natural conception after varicocelectomy.6 In addition, varicocele repair may allow a couple with severely impaired semen parameters to improve and eventually pursue less invasive treatment modalities.5 Finally, the surgical repair is associated with improvements in functional factors, such as seminal oxidative stress and sperm DNA integrity, which are not routinely assessed in the standard semen analysis.38,39
There is increasing evidence suggesting that sperm DNA fragmentation is associated with miscarriage in ART.13,36,40 In a meta-analysis involving 2969 couples, the risk of miscarriage was increased by 2.16-fold when semen specimens with an abnormally high proportion of DNA damage were used for ICSI (95% CI: 1.54–3.03, P < 0.00001).13 This increased risk of miscarriage would be related to a “late paternal effect” during the activation of male gene expression.41 This means that despite nonapparent peri-fertilization, the influence of a damaged paternal chromatin could be observed after zygotic transcriptional activation.42 In our study, three of the four included series had evaluated miscarriage rates. One of them had found lower chance of miscarriage in the group with prior varicocelectomy when compared to the group without varicocelectomy.24 Two of the studies did not find statistically significant differences between the two groups. However, one of these studies26 had included young female patients in whom the negative effect of sperm DNA damage on embryo development might have been modulated by the ability of the oocyte to repair sperm DNA damage before the first cleavage.42,43,44 In the other, a group of patients with large palpable varicoceles was studied, but surprisingly enough, semen parameters in these patients were very well preserved before varicocele repair, which might have limited the beneficial effect of varicocelectomy.25
There are some limitations in our study as there are no randomized clinical trials concerning the research question. All of the included studies were retrospective. Therefore, the quality of this evidence is considered low to moderate. In addition, there is limited objective evidence related to the potential benefits of performing prior varicocelectomy as none of the included studies evaluated functional semen analysis, such as sperm DNA fragmentation. Despite that, a postoperative improvement in conventional semen parameters was noted in two of the included24,26 In addition, the literature is scarce in studies evaluating the cost-effectiveness of performing microsurgical varicocelectomy prior to ART in nonazoospermic infertile men with clinical varicocele.45 Thus, it is not possible to conclude whether the increased cost of performing varicocelectomy would be cost-effective for achieving a live birth in this category of infertile men requiring ART.
CONCLUSION
The findings of this systematic review and meta-analysis indicate that performing varicocelectomy in patients with clinical varicocele prior to ICSI is associated with improved pregnancy outcomes. The results of our study provide a rationale for conducting further prospective research to evaluate varicocelectomy in infertile men with clinical varicocele before performing ART treatment.
AUTHOR CONTRIBUTIONS
SCE designed the study, participated in the acquisition of data, and helped to draft and revise the manuscript. MR participated in the acquisition of data, performed data analysis and prepared the manuscript. AA revised the manuscript and helped in coordination. All authors read and approved the final manuscript.
COMPETING INTERESTS
The authors declared no competing interests.
ACKNOWLEDGMENTS
The authors are grateful to Dr. Harlev Avraham for his critical reading of the manuscript.
REFERENCES
- 1.Esteves SC, Miyaoka R, Agarwal A. An update on the clinical assessment of the infertile male. [Corrected] Clinics (Sao Paulo) 2011;66:691–700. doi: 10.1590/S1807-59322011000400026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shiraishi K, Matsuyama H, Takihara H. Pathophysiology of varicocele in male infertility in the era of assisted reproductive technology. Int J Urol. 2012;19:538–50. doi: 10.1111/j.1442-2042.2012.02982.x. [DOI] [PubMed] [Google Scholar]
- 3.Masson P, Brannigan RE. The varicocele. Urol Clin North Am. 2014;41:129–44. doi: 10.1016/j.ucl.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 4.Agarwal A, Hamada A, Esteves SC. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol. 2012;9:678–90. doi: 10.1038/nrurol.2012.197. [DOI] [PubMed] [Google Scholar]
- 5.Practice Committee of the American Society for Reproductive Medicine; Society for Male Reproduction and Urology. Report on varicocele and infertility: a committee opinion. Fertil Steril. 2014;102:1556–60. doi: 10.1016/j.fertnstert.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 6.Marmar JL, Agarwal A, Prabaskan S, Agarwal R, Short RA, et al. Reassessing the value of varicocelectomy as a treatment for male subfertility with a new meta-analysis. Fertil Steril. 2007;88:639–48. doi: 10.1016/j.fertnstert.2006.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Kroese AC, de Lange NM, Collins J, Evers JL. Surgery or embolization for varicoceles in subfertile men. Cochrane Database Syst Rev. 2012;10:CD000479. doi: 10.1002/14651858.CD000479.pub5. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal A, Prabakaran S, Allamaneni SS. Relationship between oxidative stress, varicocele and infertility: a meta-analysis. Reprod Biomed Online. 2006;12:630–3. doi: 10.1016/s1472-6483(10)61190-x. [DOI] [PubMed] [Google Scholar]
- 9.Blumer CG, Restelli AE, Giudice PT, Soler TB, Fraietta R, et al. Effect of varicocele on sperm function and semen oxidative stress. BJU Int. 2012;109:259–65. doi: 10.1111/j.1464-410X.2011.10240.x. [DOI] [PubMed] [Google Scholar]
- 10.Wright C, Milne S, Leeson H. Sperm DNA damage caused by oxidative stress: modifiable clinical, lifestyle and nutritional factors in male infertility. Reprod Biomed Online. 2012;28:684–703. doi: 10.1016/j.rbmo.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Esteves SC, Gosálvez J, López-Fernández C, Núñez-Calonge R, Caballero P, et al. Diagnostic accuracy of sperm DNA degradation index (DDSi) as a potential noninvasive biomarker to identify men with varicocele-associated infertility. Int Urol Nephrol. 2015;47:1471–7. doi: 10.1007/s11255-015-1053-6. [DOI] [PubMed] [Google Scholar]
- 12.Avendaño C, Franchi A, Duran H, Oehninger S. DNA fragmentation of normal spermatozoa negatively impacts embryo quality and intracytoplasmic sperm injection outcome. Fertil Steril. 2010;94:549–57. doi: 10.1016/j.fertnstert.2009.02.050. [DOI] [PubMed] [Google Scholar]
- 13.Robinson L, Gallos ID, Conner SJ, Rajkhowa M, Miller D, et al. The effect of sperm DNA fragmentation on miscarriage rates: a systematic review and meta-analysis. Hum Reprod. 2012;27:2908–17. doi: 10.1093/humrep/des261. [DOI] [PubMed] [Google Scholar]
- 14.Zini A, Blumenfeld A, Libman J, Willis J. Beneficial effect of microsurgical subinguinal varicocelectomy on human sperm DNA integrity. Hum Reprod. 2005;20:1018–21. doi: 10.1093/humrep/deh701. [DOI] [PubMed] [Google Scholar]
- 15.Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, et al. Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology. 2007;70:532–8. doi: 10.1016/j.urology.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 16.McIntyre M, Hsieh TC, Lipshultz L. Varicocele repair in the era of modern assisted reproductive techniques. Curr Opin Urol. 2012;22:517–20. doi: 10.1097/MOU.0b013e328358e191. [DOI] [PubMed] [Google Scholar]
- 17.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:332–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Miyaoka R, Esteves SC. A critical appraisal on the role of varicocele in male infertility. Adv Urol 2012. 2012:597495. doi: 10.1155/2012/597495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zegers-Hochschild F, Adamson GD, de Mouzon J, Ishihara O, Mansour R, et al. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92:1520–4. doi: 10.1016/j.fertnstert.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Higgins JP, Green S. London: The Cochrane Colaboration; 2011. Cochrane Handbook for Systematic Reviews of Interventions. Ver. 5.1.0. [Google Scholar]
- 21.Higgins JP, Thompson SG, Spiegelhalter DJ. A re-evaluation of random-effects meta-analysis. J R Stat Soc Ser A Stat Soc. 2009;172:137–59. doi: 10.1111/j.1467-985X.2008.00552.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cocuzza M, Cocuzza MA, Bragais FM, Agarwal A. The role of varicocele repair in the new era of assisted reproductive technology. Clinics. 2008;63:395–404. doi: 10.1590/S1807-59322008000300018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zini A, Boman J, Baazeem A, Jarvi K, Libman J. Natural history of varicocele management in the era of intracytoplasmic sperm injection. Fertil Steril. 2008;90:2251–6. doi: 10.1016/j.fertnstert.2007.10.071. [DOI] [PubMed] [Google Scholar]
- 24.Esteves SC, Oliveira FV, Bertolla RP. Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicocele. J Urol. 2010;184:1442–6. doi: 10.1016/j.juro.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 25.Pasqualotto FF, Braga DP, Figueira RC, Setti AS, Iaconelli A, Jr, et al. Varicocelectomy does not impact pregnancy outcomes following intracytoplasmic sperm injection procedures. J Androl. 2012;33:239–43. doi: 10.2164/jandrol.110.011932. [DOI] [PubMed] [Google Scholar]
- 26.Gokce MI, Gülpinar O, Süer E, Mermerkaya M, Aydos K, et al. Effect of performing varicocelectomy before intracytoplasmic sperm injection on clinical outcomes in non-azoospermic males. Int Urol Nephrol. 2013;45:367–72. doi: 10.1007/s11255-013-0394-2. [DOI] [PubMed] [Google Scholar]
- 27.Duran EH, Morshedi M, Taylor S, Oehninger S. Sperm DNA quality predicts intrauterine insemination outcome: a prospective cohort study. Hum Reprod. 2002;17:3122–8. doi: 10.1093/humrep/17.12.3122. [DOI] [PubMed] [Google Scholar]
- 28.Benchaib M, Braun V, Lornage J, Hadj S, Salle B, et al. Sperm DNA fragmentation decreases the pregnancy rate in an assisted reproductive technique. Hum Reprod. 2003;18:1023–8. doi: 10.1093/humrep/deg228. [DOI] [PubMed] [Google Scholar]
- 29.Henkel R, Hajimohammad M, Stalf T, Hoogendijk C, Mehnert C, et al. Influence of deoxyribonucleic acid damage on fertilization and pregnancy. Fertil Steril. 2004;81:965–72. doi: 10.1016/j.fertnstert.2003.09.044. [DOI] [PubMed] [Google Scholar]
- 30.Virro MR, Larson-Cook KL, Evenson DP. Sperm chromatin structure assay (SCSA) parameters are related to fertilization, blastocyst development, and ongoing pregnancy in in vitro fertilization and intracytoplasmic sperm injection cycles. Fertil Steril. 2004;81:1289–95. doi: 10.1016/j.fertnstert.2003.09.063. [DOI] [PubMed] [Google Scholar]
- 31.Muriel L, Garrido N, Fernandez JL, Remohi J, Pellicer A, et al. Value of the sperm deoxyribonucleic acid fragmentation level, as measured by the sperm chromatin dispersion test, in the outcome of in vitro fertilization and intracytoplasmic sperm injection. Fertil Steril. 2006;85:371–83. doi: 10.1016/j.fertnstert.2005.07.1327. [DOI] [PubMed] [Google Scholar]
- 32.Bungum M, Humaidan P, Axmon A, Spano M, Bungum L, et al. Sperm DNA integrity assessment in prediction of assisted reproduction technology outcome. Hum Reprod. 2007;22:174–9. doi: 10.1093/humrep/del326. [DOI] [PubMed] [Google Scholar]
- 33.Caglar GS, Koster F, Schopper B, Asimakopoulos B, Nehls B, et al. Semen DNA fragmentation index, evaluated with both TUNEL and Comet assay, and the ICI outcome. In Vivo. 2007;21:1075–80. [PubMed] [Google Scholar]
- 34.Lin M, Lee RK, Li S, Lu C, Sun F, et al. Sperm chromatin structure assay parameters are not related to fertilization rates, embryo quality, and pregnancy rates in in vitro fertilization and intracytoplasmic sperm injection, but might be related to spontaneous abortion rates. Fertil Steril. 2008;90:352–9. doi: 10.1016/j.fertnstert.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 35.Nicopoullos JD, Gilling-Smith C, Almeida PA, Homa S, Norman-Taylor JQ, et al. Sperm DNA fragmentation in subfertile men: the effect on the outcome of intracytoplasmic sperm injection and correlation with sperm variables. BJU Int. 2008;101:1553–60. doi: 10.1111/j.1464-410X.2008.07518.x. [DOI] [PubMed] [Google Scholar]
- 36.Zhao J, Zhang Q, Wang Y, Li Y. Whether sperm deoxyribonucleic acid fragmentation has an effect on pregnancy and miscarriage after in vitro fertilization/intracytoplasmic sperm injection: a systematic review and meta-analysis. Fertil Steril. 2014;102:998–1005. doi: 10.1016/j.fertnstert.2014.06.033. [DOI] [PubMed] [Google Scholar]
- 37.Lewis SE. Should sperm DNA fragmentation testing be included in the male infertility work-up? Reprod Biomed Online. 2015;31:134–7. doi: 10.1016/j.rbmo.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 38.Smit M, Romijn JC, Wildhagen MF, Veldhoven JL, Weber RF, et al. Decreased sperm DNA fragmentation after surgical varicocelectomy is associated with increased pregnancy rate. J Urol. 2010;183:270–4. doi: 10.1016/j.juro.2009.08.161. [DOI] [PubMed] [Google Scholar]
- 39.Wang YJ, Zhang RQ, Lin YJ, Zhang RG, Zhang WL. Relationship between varicocele and sperm DNA damage and the effect of varicocele repair: a meta-analysis. Reprod Biomed Online. 2012;25:307–14. doi: 10.1016/j.rbmo.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 40.Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damage is associated with an increase risk of pregnancy loss after IVF and ICSI: systematic review and meta-analysis. Hum Reprod. 2008;23:2663–8. doi: 10.1093/humrep/den321. [DOI] [PubMed] [Google Scholar]
- 41.Tesarik J, Greco E, Mendoza C. Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum Reprod. 2004;19:611–5. doi: 10.1093/humrep/deh127. [DOI] [PubMed] [Google Scholar]
- 42.Simon L, Murphy K, Shamsi MB, Liu L, Emery B, et al. Paternal influence of sperm DNA integrity on early embryonic development. Hum Reprod. 2014;29:2402–12. doi: 10.1093/humrep/deu228. [DOI] [PubMed] [Google Scholar]
- 43.Evenson D, Wixon R. Meta-analysis of sperm DNA fragmentation using the sperm chromatin structure assay. Reprod Biomed Online. 2006;12:466–72. doi: 10.1016/s1472-6483(10)62000-7. [DOI] [PubMed] [Google Scholar]
- 44.Meseguer M, Martinez-Conejero JA, O’Connor JE, Pellicer A, Remohi J, et al. The significance of sperm DNA oxidation in embryo development and reproductive outcome in an oocyte donation program: a new model to study a male infertility prognostic factor. Fertil Steril. 2008;89:1191–9. doi: 10.1016/j.fertnstert.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 45.Penson DF, Paltiel AD, Krumholz HM, Palter S. The cost-effectiveness of treatment for varicocele related infertility. J Urol. 2002;168:2490–4. doi: 10.1016/S0022-5347(05)64175-4. [DOI] [PubMed] [Google Scholar]