Abstract
Background:
The exact role of vitamin D in the development and severity of preeclampsia is still unclear. The aim of the present study was to investigate the association between vitamin D supplement and preeclampsia in pregnant women.
Materials and Methods:
In this randomized controlled trial, in 2012, 140 nulliparous pregnant women in two groups received supplementation with 600 IU/day of vitamin D or supplementation free of vitamin D at 16 week gestation until the delivery. The main outcomes included the frequency of preeclampsia and subtypes by clinical severity and infant birth weight.
Results:
Mean of maternal age and gestational age at the delivery in all studied subjects were 25 ± 4.1 years and 37.4 ± 3 weeks, respectively, which were not statistically significant between the groups. Preeclampsia was observed in two subjects in case group compared to seven subjects in control group, which was not significant (P-value = 0.09). In case group, subjects with preeclampsia diagnosed as mild preeclampsia and in control group four subjects were mild, and three were severe. No significant differences were noted between the case and control groups in the frequency of preeclampsia subtypes by clinical severity. Infant birth weight in case group who was significantly higher than control group, which was statistically significant between groups (P-value = 0.09).
Conclusion:
In summary, our results demonstrated that vitamin D supplementation during the third trimester of pregnancy; despite the non-significant association between vitamin D supplementation and preeclampsia, reduce the risk of preeclampsia. However, further studies needs to be done.
Key Words: Nulliparous women, preeclampsia, pregnancy, vitamin d supplementation
INTRODUCTION
Preeclampsia is a thoughtful condition of pregnancy, which is associated with proteinuria, hypertension and end-organ disease. The condition is associated with a poor pregnancy outcome and can affect multiple organs. Worldwide, one of the leading causes of maternal death is preeclampsia, which, estimated to influence between 2-8% of all pregnancies.[1,2,3] Data from some studies supports associations of vitamin D deficiency and preterm birth, decreased birth weight, and hypertensive disease in pregnancy.[4,5,6,7,8] Another data suggesting an association between vitamin D deficiency and preeclampsia is now developing.[5] And an association between low maternal vitamin D and early-onset, severe preeclampsia is recently reported.[9] Whereas, an increased risk for preeclampsia is reported in an investigation when serum vitamin D levels decreased around 20 ng/mL after adjusting for confounders.[5] Another data suggested with only a 10ng/mL increase in maternal vitamin D a possible reduction of the risk of preeclampsia.[9] Also, association between vitamin D deficiency and preeclampsia is reported in a population based study on 23,423 women, which authors found that a 27 percent reduction in the risk for preeclampsia was associated with vitamin D intake of 15-20 micrograms per day relative to less than 5 micrograms per day.[8]
A widespread public health problem is maternal vitamin D deficiency.[5] Deficiency of vitamin D is diagnosed at level of <32 ng/mL and using the secriteria,[10] vitamin D deficiency is very common in pregnancy with up to 50% of individuals,[11,12,13] though, depending on the country of residence and local clothing customs, a prevalence ranges from 18-84% is reported by previous studies.[14,15,16,17] Lack of adequate sunlight exposure needed to synthesize vitamin D3 in the skin, and oral intakes that are too low to meet the increased demands of pregnancy are reasons of epidemic deficiency of vitamin D during pregnancy.[5,18]
Based on the role of maternal vitamin D deficiency, as a potential in dependent risk factor for preeclampsia, vitamin D supplementation in early pregnancy remains a possible intervention and possible improved pregnancy outcomes through prevention or delay of preeclampsia. Furthermore, because vitamin D supplementation is simple and cost-effective with a low likelihood of toxicity, increased supplementation in pregnant women is recommend previously. And further prospective longitudinal studies or randomized controlled trials to assess the potential effect of vitamin D supplementation on adverse pregnancy outcomes are suggested. Thus, this study was aimed to examine the impact of vitamin D supplementation in reduction of risk of preeclampsia in nulliparous women in a randomized controlled trial.
MATERIALS AND METHODS
Present study was a double-blind randomized controlled trial, which was conducted, between May, 2012 and January, 2012, on 140 nulliparous pregnant women who had been referred to “Shahid Beheshti” hospital in Isfahan, Iran. Pregnant women at less than 16 week gestation from outpatient clinics at “Shahid Beheshti” hospital were eligible if they did not have any sign of vitamin D deficiency, did not using aspirin and had no diagnosis of chronic hypertension, gestational diabetes, renal disease or systemic lupus erythematus. Immigration, abruption, and unwilling to continue the study protocol were the main exclusion criteria, Also, subjects with familial history of PTL, infection and other risk factor of PTL were excluded from the study. After the participating patients were explained about and informed of the purposes of the study, written informed consent was obtained from them all; also, ethical review of the protocol was obtained from the institutional ethics committee at the Isfahan University of Medical Sciences.
Subjects meeting the inclusion criteria, using random-maker software “Random Allocation”, were randomly divided into two groups of case and control. Case group included 70 pregnant women who received supplementation with 600 IU daily of vitamin D at 16 week gestation until labor, also, in control group, 70 pregnant women received daily supplementation free of vitamin D and followed through pregnancy to labor process. Duration of treatment patients were unaware of the treatment allocation and were followed up monthly by a doctor who was blinded to the study groups.
Maternal age, gestational age at delivery, infant birth weight, and frequency of preeclampsia sub types by clinical severity, delivery and preterm labor were variables to be observed in studied subjects by a blinded doctor.
All statistical analyses were done using “SPSS-20”. Variables are reported as mean ± SD and number (percent) as appropriate. Maternal age, gestational age at delivery, infant birth weight were compare between case and control groups using Independent sample t-test. Frequency of preeclampsia sub types by clinical severity, delivery and preterm labor in studied groups were assessed applying Chi-square test and exact test. The level of significance is considered to be less than 0.05.
RESULTS
Figure 1 shows the algorithm of study. Of 147 reviewed subjects seven did not meet eligible criteria and did not enter to the study. Either, in case group, during the follow-up period two subjects did not desire to continue and were excluded, finally, 138 subjects (68 cases and 70 controls) completed the study and analyzed.
Figure 1.
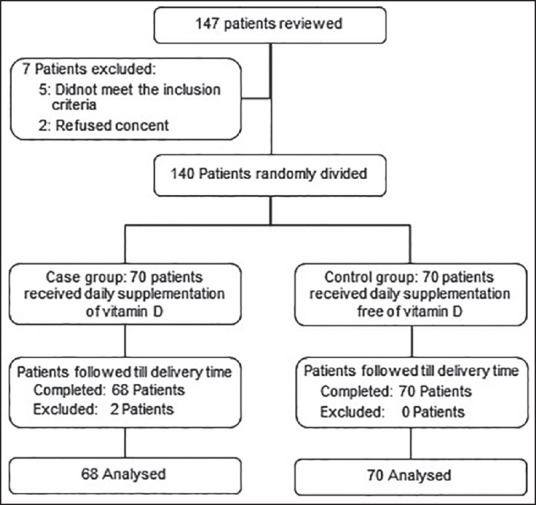
Patients who entered to the study, divided into the study groups and analyzed
Mean of maternal age and gestational age at delivery in all studied subjects were 25 ± 4.1 years and 37.4 ± 3 weeks, respectively. Comparison of maternal age, gestational age at delivery, infant birth weight, preeclampsia, delivery and preterm labor reported in Table 1. As shown, maternal age and gestational age at delivery in both the groups were similar and differences between groups were not statistically significant. Infant birth weight in case group who received vitamin D supplementation was higher than control group, result of Independent sample t-test shows that this difference in the mean of infant birth weight between groups was statistically significant. Preeclampsia was observed in 9 (6.5 percent) subjects of 138 studied subjects. Of these subjects, two subjects were in case group and seven subjects were in control group, but no significant differences in the frequency of preeclampsia were noted between case and control groups. Based on diagnostic criteria of preeclampsia subtypes by clinical severity in case group, two subjects with preeclampsia diagnosed as mild preeclampsia and of seven subjects with preeclampsia in control group four subjects diagnosed as mild, and three subjects diagnosed as severe preeclampsia. As expected, all subjects of severe preeclampsia were delivered preterm due to their disease with gestational age at delivery of 26, 28 and 34 weeks. No significant differences were noted between case and control groups in the frequency of preeclampsia sub types by clinical severity. The frequency of cesarean was done in 70 studied subjects that in both groups was the same and was not statistically significant (49 percent in case group versus 51 percent in control group P-value = 0.09).
Table 1.
Comparison of characteristics and outcomes between study groups
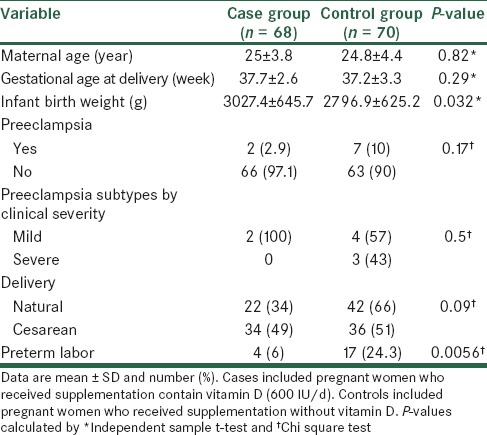
As shown in Table 1 preterm labor was occurred in 21 of all studied subjects. Between case and control groups in the frequency of preterm labor significant differences was noted whereas in controls preterm labor more occurred than cases (4 subjects in case group versus 17 subjects in control group P-value = 0.0056). Labor pain, bleeding and fetal distress were known as reasons of preterm labor in case group and in controls labor pain, bleeding, fetal distress, breech and severe preeclampsia were known as reasons of preterm labor. Results showed that differences in frequency of preterm labor reasons between both groups were not statistically significant [Figure 2].
Figure 2.
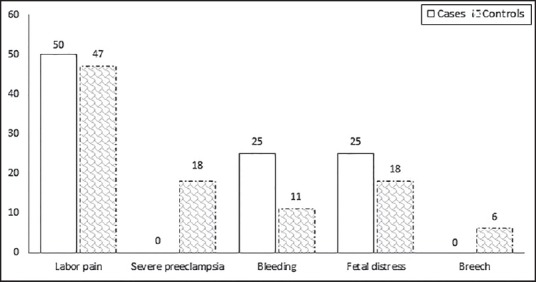
Comparison of the percent of reasons for preterm labor in studied groups. Cases included 68 pregnant women who received supplementation contain vitamin D (600 IU/d) and control group included 70 pregnant women who received supplementation without vitamin D. Differences between both groups were not statistically significant (P-value = 0.84)
DISCUSSION
Evidence to evaluate the effectiveness of vitamin D in pregnancy is no enough and much of what we know comes from observational rather than experimental design, therefore, at present vitamin D supplementation is not routinely offered to all pregnant women.[19] In the present study, we assessed the effect of vitamin D supplementation in reduction of risk of preeclampsia in nulliparous women. Our results showed that the frequency of preeclampsia in case group, who received vitamin D supplementation, was lower than control group but this difference between case and control groups was not statistically significant. Subjects with preeclampsia in case group diagnosed as mild preeclampsia whereas, in control group, nearly half of subjects with preeclampsia diagnosed as severe preeclampsia, however, difference was not significant between groups. Additionally, we observed that in case group infant birth weight was significantly higher than control group and also, preterm labor in controls significantly more occurred than cases (6% in case group versus 24% in control group).
Preeclampsia is one of the leading causes of maternal and perinatal morbidity and mortality which, vitamin D has been hypothesized to influence preeclampsia risk.[3] In the Norwegian mother and child cohort study, the association between intake of vitamin D during pregnancy and the risk of preeclampsia in 23,423 nulliparous pregnant women was estimated and authors observed 27% reduction in risk of preeclampsia after vitamin D supplementation in these women.[8] Investigators in another cohort study reported that the risk of preeclampsia in the female offspring's first pregnancy reduced after regular supplementation with vitamin D in the first year of life.[20] Also, role of vitamin D in the prevention of preeclampsia is supported by two clinical trials, however, in one of these studies as an uncontrolled trial, supplementation with a multivitamin/mineral supplement and halibut liver oil provided at 20 week gestation reduced the odds of preeclampsia.[21] In other study,400 women at 20-24 week gestation randomized to vitamin D and calcium supplements or no treatment, results of this study shows that in the treated group reduction occurred in the incidence of preeclampsia compared with the untreated group though this was not statistically significant.[22] Results of the present study in similar to these studies shows the reduction in the incidence of preeclampsia compared with controls however, this decrease was not statistically significant.
Indirectly, during the gestation vitamin D consumption may affect infant birth weight.[23] In the present study infant birth weight in women who received vitamin D supplementation, was significantly more than control group. This result is in similar with other findings which reported that intake of milk, and therefore vitamin D and calcium, during pregnancy is associated with increased infant birth weight. Authors in this study showed that the birth weights of infants born to women with low milk consumption, observed as those least likely to consume a daily vitamin D intake of 200 IU, was lower compared with those born to women who did not limit their consumption of milk.[24] In another study Asian woman with vitamin D-deficient received 1,000 IU/day of vitamin D during the third trimester and result shows a lower proportion of neonates with low birthweight compared to the placebo group.[25] Also, Marya et al., reported the highest birth weight of infants in mothers who received 600,000 IU of vitamin D during the seventh and eighth months, of pregnancy.[22] In contrast with our results other study showed that low birth weight is noted in infants of mothers supplemented with vitamin D.
We thinks that some possible limitations of the present study that should be addressed and noted in future studies are included; unmeasured sun exposure, maternal baseline 25-OH-D and preconception, physical activity, local area and early pregnancy dietary intake to help realize the effect of these factors. Level of calcium in studied women was an important unmeasured covariate in our study, whereas, low calcium intake may be associated with vitamin D deficiency and may be a risk factor for preeclampsia. Therefore, calcium intake may confound an association between maternal vitamin D deficiency and preeclampsia risk. Therefore, additional well-designed, prospective, randomized trials of supplementation with good sample size that control for dietary exposure will be necessary to determine a potential role for vitamin D in the prevention of preeclampsia.
In conclusion, results of the present study demonstrated that vitamin D supplementation during the third trimester of pregnancy; reduce the risk of preeclampsia however, this was not statistically significant. And further trials are needed to further clarify the effect of calcium supplementation, vitamin D supplementation, or both on reduce the incidence of preeclampsia.
ACKNOWLEDGMENTS
Financial support was provided by the Isfahan University of Medical Sciences (Grant 392004); Isfahan, Iran.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
REFERENCES
- 1.Lise Brantsæter A, Myhre R, Haugen M, Myking S, Sengpiel V, Magnus P, et al. Intake of Probiotic Food and Risk of Preeclampsia in Primiparous Women The Norwegian Mother and Child Cohort Study. Am J Epidemiol. 2011;174:807–15. doi: 10.1093/aje/kwr168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Geographic variation in the incidence of hypertension in pregnancy. World Health Organization International Collaborative Study of Hypertensive Disorders of Pregnancy. Am J Obstet Gynecol. 1988;158:80–3. [PubMed] [Google Scholar]
- 3.Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005;365:785–99. doi: 10.1016/S0140-6736(05)17987-2. [DOI] [PubMed] [Google Scholar]
- 4.Fischer D, Schroer A, Lüdders D, Cordes T, Bücker B, Reichrath J, et al. Metabolism of vitamin D3 in the placental tissue of normaland preeclampsia complicated pregnancies and premature births. Clin Exp Obstet Gynecol. 2007;34:80–4. [PubMed] [Google Scholar]
- 5.Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92:3517–22. doi: 10.1210/jc.2007-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.August P, Marcaccio B, Gertner JM, Druzin ML, Resnick LM, Laragh JH. Abnormal 1,25-dihydroxyvitamin D metabolism in preeclampsia. Am J Obstet Gynecol. 1992;166:1295–9. doi: 10.1016/s0002-9378(11)90625-5. [DOI] [PubMed] [Google Scholar]
- 7.Frolich A, Rudnicki M, Storm T, Rasmussen N, Hegedus L. Impaired 1,25-dihydroxy vitamin D production in pregnancy-induced hypertension. Eur J Obstet Gynecol Reprod Biol. 1992;47:25–9. doi: 10.1016/0028-2243(92)90210-p. [DOI] [PubMed] [Google Scholar]
- 8.Haugen M, Brantsaeter AL, Trogstad L, Alexander J, Roth C, Magnus P, et al. Vitamin D supplementation and reduced risk of preeclampsia in nulliparous women. Epidemiology. 2009;20:720–6. doi: 10.1097/EDE.0b013e3181a70f08. [DOI] [PubMed] [Google Scholar]
- 9.Robinson CJ, Alanis MC, Wagner CL, Hollis BW, Johnson DD. Plasma 25-hydroxy vitamin D levels in early-onset severe preeclampsia. Am J Obstet Gynecol. 2010;203:361–6. doi: 10.1016/j.ajog.2010.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357:266–81. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 11.Mulligan ML, Felton SK, Riek AE, Bernal-Mizrachi C. Implications of vitamin D deficiency in pregnancy and lactation. Am J Obstet Gynecol. 2009;202:429. doi: 10.1016/j.ajog.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Davis LM, Chang SC, Mancini J, Nathanson MS, Witter FR, O’Brien KO. Vitamin D insufficiency is prevalent among pregnant African American adolescents. J Pediatr Adolesc Gynecol. 2010;23:45–52. doi: 10.1016/j.jpag.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 13.Nesby-O’Dell S, Scanlon KS, Cogswell ME, Gillespie C, Hollis BW, Looker AC, et al. Hypovitaminosis D prevalence and determinants among African American and white women of reproductive age: Third National Health and Nutrition Examination Survey, 1988-1994. Am J Clin Nutr. 2002;76:187–92. doi: 10.1093/ajcn/76.1.187. [DOI] [PubMed] [Google Scholar]
- 14.Dawodu A, Wagner CL. Mother-child vitamin D deficiency: An international perspective. Arch Dis Child. 2007;92:737–40. doi: 10.1136/adc.2007.122689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Meer IM, Karamali NS, Boeke AJ, Lips P, Middelkoop BJ, Verhoeven I, et al. High prevalence of vitamin D deficiency in pregnant non-Western women in The Hague, Netherlands. Am J Clin Nutr. 2006;84:350–9. doi: 10.1093/ajcn/84.1.350. [DOI] [PubMed] [Google Scholar]
- 16.Bassir M, Laborie S, Lapillonne A, Claris O, Chappuis MC, Salle BL. Vitamin D deficiency in Iranian mothers and their neonates: A pilot study. Acta Paediatr. 2001;90:577–9. [PubMed] [Google Scholar]
- 17.Sachan A, Gupta R, Das V, Agarwal A, Awasthi PK, Bhatia V. High prevalence of vitamin D deficiency among pregnant women and their newborns in northern India. Am J Clin Nutr. 2005;81:1060–4. doi: 10.1093/ajcn/81.5.1060. [DOI] [PubMed] [Google Scholar]
- 18.Lee JM, Smith JR, Philipp BL, Chen TC, Mathieu J, Holick MF. Vitamin D deficiency in a healthy group of mothers and newborn infants. Clin Pediatr. 2007;46:42–4. doi: 10.1177/0009922806289311. [DOI] [PubMed] [Google Scholar]
- 19.Mahomed K, Gülmezoglu AM. Vitamin D supplementation in pregnancy. Cochrane Database Syst Rev. 2011;2:CD000228. doi: 10.1002/14651858.CD000228.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hypponen E, Hartikainen AL, Sovio U, Jarvelin MR, Pouta A. Does vitamin D supplementation in infancy reduce the risk of pre-eclampsia? Eur J Clin Nutr. 2007;61:1136–9. doi: 10.1038/sj.ejcn.1602625. [DOI] [PubMed] [Google Scholar]
- 21.Olsen SF, Secher NJ. A possible preventive effect of low-dose fish oil onearly delivery and pre-eclampsia: Indications from a 50-year-old controlled trial. Br J Nutr. 1990;64:599–609. doi: 10.1079/bjn19900063. [DOI] [PubMed] [Google Scholar]
- 22.Marya RK, Rathee S, Manrow M. Effect of calcium and vitamin Dsupplementation on toxaemia of pregnancy. Gynecol Obstet Invest. 1987;24:38–42. doi: 10.1159/000298772. [DOI] [PubMed] [Google Scholar]
- 23.Kimball S, El-Hajj Fuleihan G, Vieth R. VITAMIN D: A Growing Perspective. Crit Rev Clin Lab Sci. 2008;45:339–415. doi: 10.1080/10408360802165295. [DOI] [PubMed] [Google Scholar]
- 24.Mannion CA, Gray-Donald K, Koski KG. Association of low intake of milk and vitamin D during pregnancy with decreased birth weight. CMAJ. 2006;174:1273–7. doi: 10.1503/cmaj.1041388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maxwell JD, Ang L, Brooke OG, Brown IR. Vitamin D supplements enhance weight gain and nutritional status in pregnant Asians. Br J Obstet Gynaecol. 1981;88:987–91. doi: 10.1111/j.1471-0528.1981.tb01686.x. [DOI] [PubMed] [Google Scholar]


