Abstract
Background:
Cholecystectomy is considered as the most important and relatively common postoperative pain control often begins in recovery room by using systemic narcotics that may have some side effects. The aim of this study is to evaluate the effect of premedication with oral tizanidine on pain relief after elective laparoscopic cholecystectomy.
Materials and Methods:
In this double-blinded clinical trial, 70 adults of American Society of Anesthesiologist physiologic state 1 and 2 scheduled for elective laparoscopic cholecystectomy under general anesthesia were studied and randomly divided in two study and control groups. Ninety minutes before the induction of anesthesia, patients received either 4 mg tizanidine (study group) orally in 50cc or the same volume of plain water as a placebo (control group). Then, the vital signs, pain intensity, duration of stay in recovery, and the analgesic consumption were measured and then compared in both groups during 24 h postoperatively.
Results:
There was no significant difference in patient characteristics, with respect to age, weight, gender, and duration of anesthesia and surgery between the groups (P > 0.05). The pain intensity, need for analgesic drugs (34.57 ± 8.88 mg vs. 101.86 ± 5.08 mg), and the duration of stay in recovery room (67.43 ± 1.59 min vs. 79.57 ± 5.48 min) were significantly lower in tizanidine group than that of the control group.
Conclusion:
Oral administration of 4 mg tizanidine before laparoscopic cholecystectomy reduces postoperative pain, opioid consumption, and consequence of the duration of stay in recovery room without any complication.
Key Words: Analgesia, laparoscopic cholecystectomy, postoperative pain, tizanidine
INTRODUCTION
Acute pain control after surgery is one of the important aims of caring patients postoperatively. In spite of the scientific progresses in the knowledge of pathophysiology and pharmacology of the analgesics and development in much effective pain control procedures, most patients are still experiencing crucial difficulties concerning this problem. Therefore, it seems that the progresses done in this field are not sufficient enough[1] to control pain. Some harmful consequences such as hemodynamic and metabolic instability, failure to achieve the desired result of surgery, negative nitrogen balance, lack of patients’ satisfaction, and increase in the duration of recovery stay and patients’ costs will occur when pain persist.[2]
The postoperative pain causes the entrance of neural massages flood to spinal cord and the release of excitatory amino acids and neuropeptide from thin afferent nerve C-fibers. The increase of excitability status of spinal dorsal horn neurons will result in prolonged postoperative pain sensation. This central nervous system's (CNS’s) responsiveness as a kind of pain memory is called central sensitization (CS), which results in prolonged pain sensation.[3] The stimulation of the receptor N-methyl-D-aspartic acid (NMDA) plays an important role in CS process and the excitatory amino acids such as glutamate and aspartate activate this receptor.[4] Thus, in case of inhibition of the NMDA receptors, neuropathic pain resulting from inflammation and surgery could be possibly reduced.[4]
Cholecystectomy is considered as an important and relatively common operation. Although there is no precise statistic of people suffering from gallstone disease in Iran, it is 10% of the population in USA. Thereby, designing some strategies to reduce postoperative pain after cholecystectomy seems to be necessary. Nowadays, because of the advantages of laparoscopic surgeries, which are limited abdominal incision, shorter stay in hospital, the possibility of doing daily activities after 2 weeks, and less postoperative complications, 90% of the cholecystectomy operations in USA are done under this procedure.[5]
Controlling the postoperative pain often begins in recovery room by using opioids, especially morphine. However, systemic opioids may develop many complications such as nausea and vomiting, apnea, respiratory depression, and urinary retention. To reduce the complications and consumption of the opioids, other procedures are recommended. One of these procedures is preemptive analgesia.[6]
Tizanidine is a 2α-adrenoreceptor agonist and also a derivative of clonidine which has the same effects of clonidine such as creating tranquility, reducing anxiety and analgesia, but the side effects such as low arterial blood pressure and bradycardia are lower with tizanidine than those of clonidine. As the spinal cord is the primary site of tizanidine effect and it prevents the release of excitatory amino acids (aspartic and glutamic acids) by stimulating the 2α presynaptic receptors, this drug can be useful to reduce postoperative pain and the need for tranquilizers through inhibition of CS.[3,7] As far as tizanidine can be administered orally, this procedure is much preferable than injection procedures.
The side effects of tizanidine include drowsiness, xerostomia, fatigue, asthenia, anxiety, headache, bradycardia and low arterial blood pressure, gastrointestinal and liver disorders, which are principally dose-dependent.[8] This drug is absorbed easily by gastrointestinal system and after the oral administration, the peak plasma concentration will occur in one or 2 h. The eliminative half-life of this drug is between 2 and 4 h.[9]
Some researches have been carried out about the analgesic effect of this drug:
In one trial, the consumption of 3 mg tizanidine orally before entering to operating room considerably reduced the pain resulting from local anesthetic infiltration while using epidural catheter[7]
Other trial showed that tizanidine reduces the need for midazolam to prevent consciousness before induction of general anesthesia[10]
In other trial, the prescription of 4 mg tizanidine before the plaque removal surgery from lower limb caused the reduction of pain and also the need for opioid[3]
In an experimental research on the rats, the consumption of tizanidine before the spinal cord surgery has resulted in relative analgesia[11]
The effect of tizanidine on the phantom limb pain syndrome was studied in another research and it was observed that tizanidine is effective in reducing all kinds of phantom limb pains[12]
In another study, the effects of two 2α adrenergic agonist's drugs, tizanidine and clonidine, as the premedication on tetracaine spinal analgesia was compared with the control group. In both groups of receiving tizanidine and clonidine, the 1st time of pain appearance and the duration of analgesia after the operation were longer than those of the control group. However, the heart rate and systolic blood pressure reduced considerably in clonidine group.[13]
By considering the researches done about the effects of oral tizanidine on relieving pain in the above studies and the fact that the analgesic effect of this drug has not been yet studied after the major operations, we decided to carry out our research on the effect of this drug on postoperative pain of laparoscopic cholecystectomy under general anesthesia.
MATERIALS AND METHODS
After our Institutional Ethics Committee approval and taking the patients’ informed consent, 70 adults of American Society of Anesthesiologist class of 1 and 2 scheduled for elective laparoscopic cholecystectomy under general anesthesia were studied. Patients aged between 18 and 60, with no history of drug and alcohol consumption, lack of beta-blocker, digoxin, anticonvulsants and antihypertensive drugs consumption, lack of allergy to tizanidine, lack of history of CNS, liver and gastrointestinal disorders, and chronic pains were included in our study. Patients should not use analgesic drugs within 6 h before surgery and have no bradycardia (pulse rate <60). If the operation lasted under 30 min or over 120 min or any changes in surgery program from laparoscopy to laparotomy was made, the patients were taken out of this study.
In this controlled, prospective clinical trial, all patients were divided into two groups by a convenient random double-blinded method. Sealed envelopes were prepared by an anesthesia research nurse who was not involved in data collection. She prepared one labeled envelope for each patient and used the same labels for similar glasses of water (50cc) containing either 4 mg tizanidine (study group) or the plain water as a placebo (control group). These envelopes were stored in research nurse box in the operating room. Ninety minutes before the operation, the first anesthesiologist who did not participate in data collection pulls out one of the envelops for patient and also selects the similar labeled glass of water (50cc) (containing either 4 mg tizanidine tablet or placebo). Patients in both groups were received similar volumes (50cc) of liquids at the same time by the first anesthesiologist.
Before the operation, the patients were trained in handling the visual analog scales (VASs), the patients’ characteristics such as age, gender, and weight were recorded, and patients’ vital signs (heart rate and blood pressure) were measured and recorded as baseline values. All patients were monitored by pulse oximeter, capnograph, electrocardiogram, noninvasive blood pressure device, and thermometer. Anesthesia was induced by thiopental sodium 5 mg/kg/intravenous (IV), atracurium 0.5 mg/kg/IV, and fentanyl 3 µ/kg/IV, the patients were intubated and the anesthesia was maintained by isoflurane 1–1.25% and oxygen. The laparoscopic surgery was done by gas pressure under 15 mm Hg. During the first 15 min, the vital signs (pulse and blood pressure) were measured and recorded every 5 min and then were measured and recorded every 15 min until the discharge from the recovery room. If any complication such as bradycardia (pulse under 60) and/or hypotension (blood pressure <20% of basic blood pressure) occurred, they were recorded and the blowing of CO2 was stopped, and to treat bradycardia, atropine 0.01 mg/kg, and in case of hypotension, ephedrine 5 mg, were injected with 500cc crystalloid. If the treatment was not achieved, the other dose of the medications was repeated until the treatment was achieved.
For all the patients, the duration of anesthesia, operation, stay in recovery room, and the extubation time were measured and recorded.
At recovery room and after transferring patients to the ward at 1, 2, 3, 6, 12, and 24 h postoperatively, the vital signs and pain intensity (pain score) were evaluated by an investigator who was blinded to the treatment assignment.
If the pain score was more than 4, 2 mg morphine (IV) would be prescribed and if after 15 min if the pain score still stayed more than 4, another 2 mg IV morphine would be prescribed again until the pain score reduces to 3 or lower. The total amount of narcotics consumed within 24 h after the operation was recorded.
In addition, the amount of narcotic that was used after surgery in the recovery room and the total amount during 24 h postoperatively were separately measured and recorded. Moreover, in the recovery room and ward, the time of first request for analgesics was recorded.
The patient's monitoring and pain score recordings were done by an anesthesia assistant who had no information about the kind of the received medications.
In the study group, the complications of tizanidine such as xerostomia, nausea and vomiting, drowsiness, headache, and bradycardia were monitored and the patients’ satisfaction as poor (1), average (2), good, (3) and excellent (4), was asked and recorded 24 h after surgery for both groups.
Data were collected and then analyzed by repeating the observations using SPSS software version 20 (SPSS, Inc., Chicago IL), Chi-square statistic tests, t-test, and variance analysis test. P values lower than 0.05 were assumed significant.
RESULTS
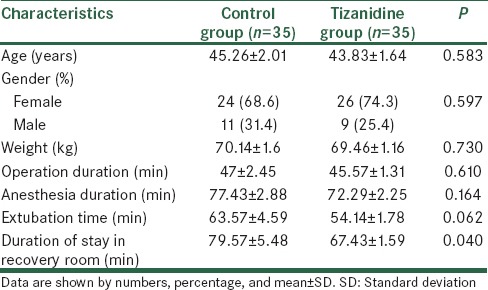
A total of 70 patients met the inclusion criteria. These patients were randomly assigned to the tizanidine group (n = 35) or the placebo group (n = 35). The groups were similar with respect to age, weight, gender, and the duration of anesthesia and surgery (P > 0.05). The extubation time was similar in both groups but the duration of stay in recovery room was significantly shorter in the tizanidine group than the placebo group (P < 0.05) [Table 1].
Table 1.
The comparison of age, weight, gender, duration of anesthesia and operation, extubation time, and the duration of stay in the recovery room
There was no significant difference in the heart rates between two groups at any times. The mean arterial blood pressure (MAP) at 30 min after beginning of anesthesia was significantly lower in the tizanidine group. However, in other times, there was no significant difference in MAP between the groups [Figure 1].
Figure 1.
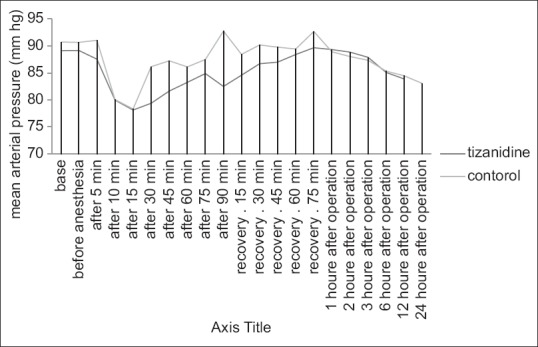
The comparison of mean arterial pressure during the operation, recovery room, and ward with the base
In recovery room and at 1, 2, 3, 6, 12, and 24 h after operation, the VAS in the tizanidine group was significantly lower than in the control group [Figure 2], and the average opioid consumption was also significantly lower in the tizanidine group (P < 0.05) [Table 2].
Figure 2.
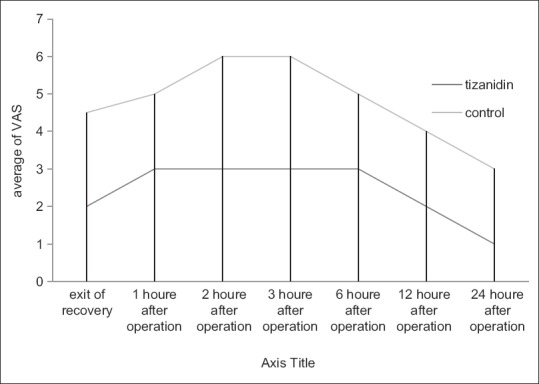
The average of visual analog scale after the operation in the tizanidine and control groups
Table 2.
The comparison of the mean of the time of first request for the opioid after the operation and the consumed narcotic dose
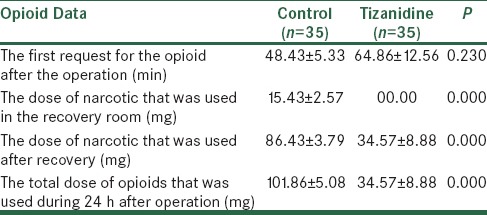
Although the first request for opioid was sooner in the control group in comparison with the tizanidine group, this difference was not significant (P > 0.05) [Table 2].
Complications of tizanidine such as xerostomia, nausea and vomiting, drowsiness, headache, and bradycardia (PR < 60) were also compared. Among them, drowsiness was seen in four patients in the tizanidine group, which was statistically significant, but bradycardia was more in the control group, however, this difference was not significant. The satisfaction level was also higher in the tizanidine group in comparison with the control group.
DISCUSSION
In this study, we have demonstrated that the administration of tizanidine before operation in patients scheduled for elective laparoscopic cholecystectomy under general anesthesia improves postoperative analgesia, provides less pain intensity, and decreases the amount of analgesic consumption.
Tizanidine, which is an alpha-adrenergic agonist, acts by increasing the presynaptic inhibition of motor neurons at the alpha 2-adrenergic receptor sites, possibly by reducing the release of excitatory amino acids (aspartic and glutamic acids) and inhibiting facilitatory caeruleospinal pathways, resulting in a reduction in spasticity. It is mainly used as a muscle relaxant to treat the spasms, cramping, and tightness of muscles caused by medical problems such as multiple sclerosis, amyotrophic lateral sclerosis, spastic diplegia, back pain, or certain other injuries to the spine or CNS. It is also prescribed off-label for migraine headaches, as a sleep aid, and as an anticonvulsant.[3,7,9]
Tizanidine produces antihypertensive effects, possibly by binding to the imidazoline receptors. Pharmacologic studies found tizanidine to have one fifth to one-tenth of the potency of clonidine in lowering blood pressure. These antihypertensive effects are mild and transitory in relation to its activity as a muscle relaxant. This medicine also has antinociceptive effects. However, these effects may be mediated through an alpha 2-adrenergic receptor mechanism rather than a narcotic or endorphin mechanism. Thereby, it could be useful to reduce the postoperative pain and the need for tranquilizers. The antinociceptive action has been confirmed at doses lower than those producing a muscle relaxant action. The exact mechanism of the action of tizanidine is unknown.[3,9,13]
Some researches have been done about the effects of oral tizanidine in relieving pain.
Nouroozi et al.[3] reported that administration of 4 mg tizanidine before the plaque removal surgery from the lower limb lessens pain and postoperative opioid consumption.
In Takenaka's study,[10] the effect of tizanidine given as a premedication on perioperative hemodynamics, sedation, hypnosis, and midazolam requirements for induction of anesthesia was assessed in patients scheduled for elective surgery under general anesthesia. They found that the increase in mean arterial blood pressure after the induction of anesthesia and the amount of midazolam necessary for loss of consciousness were significantly less in patients who had received tizanidine 4 mg. In this study, authors were interested more in hemodynamic and sedative effects of tizanidine, but in our survey we pertained more to the analgesic effect of this drug.
Imanaga et al.[7] also found that oral administration of 3 mg tizanidine as premedication reduces the infiltration pain of local anesthetic during epidural catheterization. Blood pressure and rate-pressure product in the operating room were also attenuated by receiving tizanidine. In this study, the analgesic effect of tizanidine was studied during epidural infiltration of local anesthetic, but we studied postoperative pain in patients receiving general anesthesia.
Moreover, Wajima et al.[9] reported that premedication with 4 mg oral tizanidine, 90 min before surgical skin incision significantly shortens the time to loss of consciousness in the study group than in the control group (P = 0.03) and it successfully reduces the minimum alveolar concentration of sevoflurane by 18% in human adults. In this study, the authors concerned on the sedative effect of tizanidine during anesthesia rather than its postoperative analgesic effect which was our major concern. Considering these surveys and other studies, it can be suggested that low dose (4 mg) of tizanidine can establish hemodynamic stability. In addition, it does not have side effects such as a severe decrease in blood pressure seen with clonidine.
In our study, the effect of premedication with oral tizanidine on postoperative pain in patients undergoing laparoscopic cholecystectomy was studied. There was no significant difference in the heart rates between two groups at any times. Thirty minutes after the induction of anesthesia, mean arterial blood pressure was significantly lower in the tizanidine group when compared with control group (P < 0.05). The difference may be attributed to the peak plasma concentration of tizanidine and its peak effect [Figure 1].
We also found that in the recovery room and at 1, 2, 3, 6, 12, and 24 h after operation, the VAS in the tizanidine group was significantly lower than in the control group [Figure 2]. The average opioid consumption was also significantly lower in the tizanidine group (P < 0.05). Although the first request for opioid was sooner in the control group in comparison with the tizanidine group, this difference was not significant (P > 0.05) [Table 2].
In our study, we found that the administration of tizanidine before operation improves postoperative analgesia, provides less pain intensity, and decreases the amount of analgesic consumption, which is comparable with the previous study of the effect of oral tizanidine on pain after plaque removal surgery from the lower limb.[3]
The staying time in the recovery room was shorter in the tizanidine group and this difference was significant (P < 0.05) [Table 1]. This difference could be attributed to the tizanidine group's lower pain feeling and their lack of need for opioid in the recovery room.
The sedative effect may be due to the fact that as far as the stimulation of the NMDA receptor plays an important role in CS process, the excitatory amino acids such as glutamate and aspartate activate this receptor. Thus, in case of inhibition of the NMDA receptors, neuropathic pain resulting from inflammation and surgery could be possibly reduced. Therefore, tizanidine may have a preemptive analgesic effect and may be effective as a premedication.
Eventually, the patients’ level of satisfaction in the tizanidine group (3.17) was significantly higher in comparison with the control group's level of satisfaction (1.91).
None of the patients complained about xerostomia, nausea, and headache. Bradycardia (PR < 60) was unexpectedly more in the control group, however, this difference was not significant. Vomiting was also reported in one case of the control group, and four patients in the tizanidine group complained about drowsiness, but not in the control group, and this difference was significant.
According to the present study, we concluded that premedication with oral tizanidine 90 min before the operation can reduce the pain scores, analgesic consumption, analgesic related side effects, and thereby providing early return to normal daily activity after laparoscopic cholecystectomy. Regarding tizanidine's short duration of action, administration of this drug is recommended for sedating, stabilizing hemodynamic responses during the operations, and for reducing the required dose of anesthetic.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to sincerely thank the support of all the colleagues in the operating room and wards of Alzahra University Hospital affiliated to Isfahan University of Medical Sciences, Isfahan, Iran. Furthermore, our special thanks to the patients who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. This prospective, randomized, observational study was approved by the Ethics Committee of our university, (Anesthesiology and Critical Care Research Center, Isfahan University of Medical Sciences, Isfahan, Iran) and all patients gave written, informed consent.
REFERENCES
- 1.Pazuki SH. Evaluation of the effect of metoclopramide infusion on postoperative pain in candidates of cholecystectomy in Tehran Emam Khomeini hospital. Rahavard Danesh. 2000;3:6–10. [Google Scholar]
- 2.Elyasi H, Abdolmohammadi S, Mosaffa F, Madadi F, Dabbagh A. The effect of intra-articular magnesium sulfate on postoperative acute pain in knee arthroscopy. Pajoohandeh J. 2009;14:1–4. [Google Scholar]
- 3.Nouroozi M, Douroodian M, Nashibi M, Ahmadinejad M. Effect of Tizanidine on postoperative pain. J Iran Soc Anaesthesiol Intensive Care. 1388;31:24–32. [Persian] [Google Scholar]
- 4.Christopher L. Acute postoperative pain. In: Miller RD, editor. Anesthesia. 6th ed. Philadelphia: Churchill Livingstone; 2005. pp. 2729–62. [Google Scholar]
- 5.Safarpoor F, Koohsari M. Laparoscopic cholecystectomy: Preferential procedure. Gilan Univ Med J. 2002;11:50–5. [Google Scholar]
- 6.Tverskoy M, Oren M, Vaskovich M, Dashkovsky I, Kissin I. Ketamine enhances local anesthetic and analgesic effects of bupivacaine by peripheral mechanism: A study in postoperative patients. Neurosci Lett. 1996;215:5–8. doi: 10.1016/s0304-3940(96)12922-0. [DOI] [PubMed] [Google Scholar]
- 7.Imanaga K, Wajima Z, Inoue T, Ogawa R. Effect of oral tizanidine on local-anesthetic infiltration pain during epidural catheterization. J Nippon Med Sch. 2004;71:105–10. doi: 10.1272/jnms.71.105. [DOI] [PubMed] [Google Scholar]
- 8.Henney HR, Chez M. Pediatric safety of tizanidine: Clinical adverse event database and retrospective chart assessment. Paediatr Drugs. 2009;11:397–406. doi: 10.2165/11316090-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 9.Wajima Z, Yoshikawa T, Ogura A, Imanaga K, Shiga T, Inoue T, et al. Oral tizanidine, an alpha2-adrenoceptor agonist, reduces the minimum alveolar concentration of sevoflurane in human adults. Anesth Analg. 2002;95:393–6. doi: 10.1097/00000539-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 10.Takenaka M, Iida H, Kasamatsu M, Katoh H, Tashiro T, Dohi S. Tizanidine for preanesthetic medication. Masui. 1996;45:971–5. [PubMed] [Google Scholar]
- 11.Turan A, Karamanlioglu B, Memis D, Hamamcioglu MK, Tükenmez B, Pamukçu Z, et al. Analgesic effects of gabapentin after spinal surgery. Anesthesiology. 2004;100:935–8. doi: 10.1097/00000542-200404000-00025. [DOI] [PubMed] [Google Scholar]
- 12.Vorobeichik IaM, Kukushkin ML, Reshetniak VK, Ovechkin AM, Gnezdilov AV. The treatment of the phantom pain syndrome with tizanidine. Zh Nevrol Psikhiatr Im S S Korsakova. 1997;97:36–9. [PubMed] [Google Scholar]
- 13.Omote K, Satoh O, Sonoda H, Kumeta Y, Yamaya K, Namiki A. Effects of oral alpha 2 adrenergic agonists, clonidine and tizanidine, on tetracaine spinal anesthesia. Masui. 1995;44:816–23. [PubMed] [Google Scholar]


