Endoscopic ultrasound (EUS) is a useful tool in the management of both gastrointestinal (GI) and non-GI disease states. It has been employed around the world since the 1990s. However, many centers in Canada have only recently started to use EUS routinely for patient management. There are currently no Canadian credentialing guidelines for EUS.
Proficiency requires adequate experience and training. Supervised “hands-on” training likely allows endosonographers to achieve proficiency more quickly than self-training.[1] The Forum on Canadian Endoscopic Ultrasound (FOCUS) proposes these guidelines as an objective framework to help institutions assess the training and competency of endosonographers for credentialing purposes.
SELF-TRAINING
A large proportion of ultrasonographers are self-taught. A 2004 international survey of clinical EUS practice found that only 18.8% of responders had greater than 6 months of training, 9.4% of respondents had 3-6 months of supervised training, and 7.3% of responders had less than 3 months of supervised training.[2] The remaining respondents were self-taught or learned by observation only.
Wang et al. evaluated EUS trainees’ evolution prospectively. Compared with pretraining, the proportion of trainees who succeeded in locating each structure after the training were, respectively, celiac axis (36% vs. 80.5%), pancreatic body and tail (51.5% vs. 80.5%), splenic vein and artery (48.5% vs. 84%), left kidney (60% vs. 83%), and spleen (47% vs. 83%). They concluded that a structured training program significantly improved the successful localization of structures.[3]
A survey of practicing endosonographers in various parts of the Asia-Pacific region outside Japan was conducted in 2006. Seventy one of 87 physicians surveyed responded. They had performed a median of 500 procedures in their career; 49.3% were self-taught and only 22.5% had undergone a formal EUS fellowship of at least 6 months. Ninety percent believed that a formal EUS fellowship was needed to acquiring competence, with a minimum number of supervised procedures performed over a minimum amount of time (median 6 months).[4]
A survey of Latin American endosonographers demonstrated that 48.6% of respondents had more than 6 months of training. Thirty-seven percent of respondents thought at least 6 months of formal training was necessary to acquire competence. Additionally, the majority of respondents (64%) felt that more than 50 procedures for pancreatic-biliary lesions were necessary.[5]
CURRENT GUIDELINES
There are currently no Canadian guidelines for EUS credentialing. Current Canadian guidelines require 150 gastroscopies [100 unassisted, 20 nonvariceal bleeding, 20 variceal bleeding, 20 esophageal dilatation, and 20 percutaneous endoscopic gastrostomy (PEG) tube placement],[6] 150 colonoscopies, (100 unassisted),[7] 30 flexible sigmoidoscopies for competency,[8] and 200 endoscopic retrograde cholangiopancreatographies (including 80 sphincterotomies and 60 stent placements).[9]
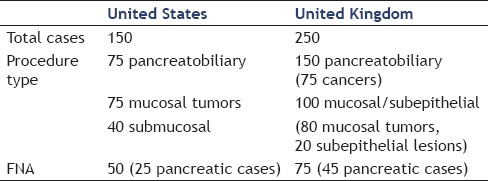
EUS training guidelines have been adopted in the United States (US) by the American Society for Gastrointestinal Endoscopy (ASGE) and in the United Kingdom (UK) by the British Society of Gastroenterology (BSJ) [Table 1]. In the US, 150 cases are required, including 75 pancreato-biliary cases, 75 mucosal tumors, and 40 submucosal abnormalities. The US guidelines also recommend 50 EUS fine needle aspiration (FNA) cases (25 pancreatic).[10] The UK guidelines recommend that EUS trainees perform 250 supervised procedures, including 80 luminal cancers, 20 submucosal lesions, and 150 pancreatobiliary cases (at least half of which are likely pancreatic adenocarcinomas). A total of 75 EUS-FNA procedures should be performed, of which 45 likely should be pancreatic adenocarcinomas.[11]
Table 1.
USA and United Kingdom EUS guidelines for credentialing
A thorough review on training in EUS-FNA was published by Paquin in 2013. It concluded that formal training in EUS-FNA is recommended in order to maximize proficiency, “hands-on” training in humans should produce the best results, and that current EUS-FNA guidelines be tested to determine whether current minimal training thresholds need upgrading.[12]
EVALUATION OF CURRENT GUIDELINES
As stated previously, ASGE recommendations for EUS include 150 supervised cases. However, recent studies have demonstrated that the learning curve for mastery may be much more than previously thought. A study by Wani et al. evaluated the performance of five advanced endoscopic trainees (who had between 175 and 402 EUS procedures during training). The study observed substantial variability in the numbers needed to achieve competency, with only two trainees showing acceptable performance after 225 and 196 cases. None of the trainees achieved training guideline goals after the recommended minimal 150 procedures.[13] Thus, some experts question the numbers required to obtain competency.[14]
A study by Eloubeidi and Tamhane showed that after 1 year of formal EUS training (300 supervised cases and 45 EUS-FNA) the median number of EUS-FNA passes needed to achieve a diagnosis decreased significantly after 100 additional FNA procedures and that complication rates decreased after 200 additional cases.[15] A study of 25 US gastroenterology training programs offering advanced EUS training showed that the average number of supervised procedures per trainee varied considerably (median 200; range 50-1,100), with only 48% of fellows meeting the minimum number of procedures as recommended by ASGE. This lead to a conclusion that some training centers may not offer minimal training requirements during a 1-year curriculum.[16] Azad et al. conducted a study to evaluate the viability of US gastrointestinal training programs to meet ASGE guidelines in EUS. In a 3-year program, the median number of EUS procedure trainees were exposed to was 50 (0-350), in an advanced 1-year fellowship was 200 (50-1,100). Dedicated “hands-on” training was significant greater in an advanced 1-year fellowship than a 3-year GI fellowship training (81% vs. 57%).[16]
The available data from Wani et al. and Eloubiedi suggest that the proposed number of cases may not be enough for competency in EUS.[13,15] An editorial from Sedarat and Kochman suggest that the available volume of procedures at training centers likely limits the exposure of trainees to adequate number of procedures. The volume required to obtain competency is greater than one had previously postulated.[16] The 2001 ASGE guidelines have not been updated. Over the last decade, a shift toward more interventional procedures has occurred. It is unclear if this shift should influence training guidelines.
TRAINING ADJUNCTS
Proficiency cannot be strictly defined by “the number” of procedures achieved. Other independent factors are required. Bloom et al. called these the cognitive, psychomotor, and affective domains.[17] The cognitive aspects of the procedure are as important as the technical aspects of the procedures. The indications/contraindications, the risks, and benefits of performing the technique and the application of the information gleaned from the procedure are aspects usually not evaluated objectively in training centers. Most experts recommend a 6-24 month “hands-on” EUS fellowship.[18] This may provide adequate time for trainees to fully comprehend the nontechnical aspects of the procedure and thus be able to achieve mastery of a given procedure.
Several training adjuncts are available to possibly assist trainees achieve competency. Direct observation of experts, videos, and simulators may help prepare for true hands-on training.[19] Nonhuman “hands-on” training models exist; including inert phantoms and animal models using live or ex vivo porcine organs. Unfortunately, porcine biliopancreatic anatomy is very different from that of humans.[19,20,21,22,23]
Studies have reported significant variations in the competency of advanced endoscopy trainees. Competency has typically been subjective based on trainer's evaluations during training. A study by Wani et al. evaluated a standardized data collection form to grade EUS examinations. Using a five-point scoring system they objectively defined competency with EUS, with acceptable and unacceptable failure rates of 10% and 20%, respectively.[24] One can propose that competency should be based not only on serial subjective (e.g. every 50 EUS performed) evaluation of trainee, but on validated standardized, objective evaluations.
PROPOSED CANADIAN GUIDELINES
The Forum on Canadian Endoscopic Ultrasound (FOCUS) is a national Canadian meeting held every year since 2013. It brings together Canadian endosonographers to review best practices in EUS, with a focus on challenges related to Canadian healthcare systems. The lack of credentialing guidelines for training and credentialing Canadian physicians in EUS has been a major issue at all meetings.
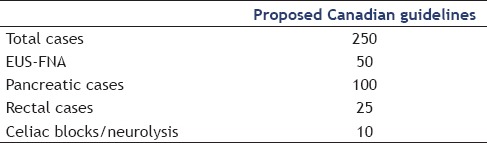
After reviewing the data in the first meeting, guidelines were proposed to the group in September 2014. The proposal acknowledged that ASGE guidelines may not require enough cases for competency in EUS. The FOCUS proposed that trainees undergo “hands-on” training in at least 250 supervised cases. Included in these procedures, the trainee should perform at least 50 FNA independently — 100 pancreatic cases, 25 rectal cases, at least 10 celiac blocks/neurolysis [Table 2]. Other therapeutic cases, such as pseudocyst drainage, should be dependent on the training center availability and expertise.
Table 2.
Proposed Canadian EUS guidelines for credentialing and privileging
The proposed guidelines had 90% approval from the 75 attendees present at the FOCUS 2014. The maintenance of competency was not discussed at this meeting. However, it was agreed that future subjects for discussion should include CME programs and monitoring of quality measures.
CONCLUSION
In conclusion, we believe that the establishment of Canadian guidelines for EUS is warranted. The proposed guidelines should provide a framework for the institutions to assess the training of physicians seeking credentials to perform EUS.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Nayar M, Joy D, Wadehra V, et al. Effect of dedicated and supervised training on achieving competence in EUS-FNA of solid pancreatic lesions. Scand J Gastroenterol. 2011:46;997–1003. doi: 10.3109/00365521.2011.579158. [DOI] [PubMed] [Google Scholar]
- 2.Das A, Mourad W, Lightdale CJ, et al. An international survey of the clinical practice of EUS. Gastrointest Endosc. 2004;60:765–70. doi: 10.1016/s0016-5107(04)02168-6. [DOI] [PubMed] [Google Scholar]
- 3.Wang MH, Dy F, Khien VV, et al. Structured endoscopic ultrasonography (EUS) training program improved knowledge and skills of trainees: Results from the Asian EUS Group. Dig Endosc. 2015;27:687–91. doi: 10.1111/den.12458. [DOI] [PubMed] [Google Scholar]
- 4.Ho KY. Survey of endoscopic ultrasonographic practice and training in the Asia-Pacific region. J Gastroenterol Hepatol. 2006;21:1231–5. doi: 10.1111/j.1440-1746.2006.04254.x. [DOI] [PubMed] [Google Scholar]
- 5.Drigo JM, Castillo C, Weyer W, et al. Endoscopic ultrasound practice survey in Latin America. Endosc Ultrasound. 2013;2:208–18. doi: 10.4103/2303-9027.121251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponich T, Enns R, Romagnuolo J, et al. Canadian credentialing guidelines for esophagogastroduodenoscopy. Can J Gastroenterol. 2008;22:349–54. doi: 10.1155/2008/987012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Romagnuolo J, Enns R, Ponich T, et al. Canadian credentialing guidelines for colonoscopy. Can J Gastroenterol. 2008;22:17–22. doi: 10.1155/2008/837347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enns R, Romagnuolo J, Ponich T, et al. Canadian credentialing guidelines for flexible sigmoidoscopy. Can J Gastroenterol. 2008;22:115–9. doi: 10.1155/2008/874796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Springer J, Enns R, Romagnuolo J, et al. Canadian credentialing guidelines for endoscopic retrograde cholangiopancreatography. Can J Gastroenterol. 2008;22:547–51. doi: 10.1155/2008/582787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Eisen GM, Dominitz JA, Faigel DO, et al. American Society for Gastrointestinal Endoscopy. Guidelines for credentialing and granting privileges for endoscopic ultrasound. Gastrointest Endosc. 2001;54:811–4. doi: 10.1016/s0016-5107(01)70082-x. [DOI] [PubMed] [Google Scholar]
- 11.Meenan J, Harris K, Oppong K, et al. Service provision and training for endoscopic ultrasound in the UK. Frontline Gastroenterol. 2011;2:188–94. doi: 10.1136/fg.2010.004101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paquin SC. Training in endoscopic ultrasound-guided fine needle aspiration. Endsoc Ultrasound. 2014;3:12–6. doi: 10.4103/2303-9027.127123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wani S, Coté GA, Keswani R, et al. Learning curves for EUS by using cumulative sum analysis: Implications for American Society for Gastrointestinal Endoscopy recommendations for training. Gastrointest Endosc. 2013;77:558–65. doi: 10.1016/j.gie.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 14.Sedarat A, Kochman ML. Competency in EUS: Is it the curriculum, test, trainer, or trainee? Gatrointest Endosc. 2013;77:566–7. doi: 10.1016/j.gie.2012.11.043. [DOI] [PubMed] [Google Scholar]
- 15.Eloubiedi MA, Tamhane A. EUS-guided FNA of solid pancreatic masses: A learning curve with 300 consecutive procedures. Gastrointest Endosc. 2005;61:700–8. doi: 10.1016/s0016-5107(05)00363-9. [DOI] [PubMed] [Google Scholar]
- 16.Azad JS, Verma D, Kapadia AS, et al. Can U.S. GI fellowship programs meet American Society for Gastrointestinal Endoscopy recommendations for training in EUS? A survey of U.S. GI fellowship program directors. Gastrointest Endosc. 2006;64:235–41. doi: 10.1016/j.gie.2006.04.041. [DOI] [PubMed] [Google Scholar]
- 17.Bloom BS, Englehart MD, Furst EJ, et al. Boston: Allyn & Bacon; 1956. Taxonomy of Educational Objectives: The Classification of Educational Goals. Handbook: Cognitive Domain. [Google Scholar]
- 18.Polkowski M, Larghi A, Weynand B, et al. European Society of Gastrointestinal Endoscopy (ESGE). Learning, techniques and complications of endoscopic ultrasound (EUS)-guided sampling in gastroenterology: European Society of Gastrointestinal Endoscopy (ESGE) Technical Guideline. Endoscopy. 2012;44:190–206. doi: 10.1055/s-0031-1291543. [DOI] [PubMed] [Google Scholar]
- 19.Barthet M. Endoscopic ultrasound teaching and learning. Minerva Med. 2007;98:247–51. [PubMed] [Google Scholar]
- 20.Sorbi D, Vazquez-Sequeiros E, Wiersema MJ. A simple phantom for learning EUS-guided FNA. Gastrointest Endosc. 2003;57:580–3. doi: 10.1067/mge.2003.141. [DOI] [PubMed] [Google Scholar]
- 21.Matsuda K, Tajiri H, Hawes RH. How shall we experience EUS and EUS-FNA before the first procedure?. The development of learning tools. Dig Endosc. 2004;16:S236–9. [Google Scholar]
- 22.Bussen D, Sailer M, Fuchs KH, et al. A teaching model for endorectal ultrasound-guided biopsy and drainage of pararectal tumors. Endoscopy. 2004;36:217–9. doi: 10.1055/s-2004-814251. [DOI] [PubMed] [Google Scholar]
- 23.Fritscher-Ravens A, Cuming T, Dhar S, et al. Endoscopic ultrasound-guided fine needle aspiration training: Evaluation of a new porcine lymphadenopathy model for in vivo hands-on teaching and training, and review of the literature. Endoscopy. 2013;45:114–20. doi: 10.1055/s-0032-1325931. [DOI] [PubMed] [Google Scholar]
- 24.Wani S, Hall M, Keswani RN, et al. Variation in aptitude of trainees in endoscopic ultrasonography, based on cumulative sum analysis. Clin Gastroenterol Hepatol. 2015;13:1318–25. doi: 10.1016/j.cgh.2014.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]


