Abstract
We present an unusual case of a 13-year-old child who following minor head injury presented with what appeared to be a thin chronic subdural hematoma on plain computed tomography imaging. The child was found to have an underlying arachnoid cyst. Intra- and extra-cystic bleeding had occurred simultaneously causing an isodense cyst with an accompanying subdural collection. This radiographically occult pathology should be excluded using magnetic resonance imaging in any child presenting with a subdural collection.
Keywords: Arachnoid cyst, pediatric, subdural hematoma
Introduction
This is an interesting case of a child who, following a minor head injury a few weeks earlier, was initially found to have a thin chronic subdural haematoma on plain computed tomography (CT) imaging. Following burr hole surgery for evacuation of the subdural haematoma his post-operative scan revealed an underlying arachnoid cyst. It is established that intra-cystic bleeding can ensue following minor head injury in patients with this benign developmental malformation. Often the haemorrhage is obvious on initial imaging but this is not always the case.
Clinical Background
A 13-year-old boy presented with a 1-month history of worsening global headache with associated nausea and vomiting. The symptoms developed following an injury sustained by falling and hitting his head on a chair. He did not lose consciousness but had no memory of the event. He had no significant past medical history, met all his developmental milestones and had no significant family history.
On examination he had normal higher mental and cranial nerve function and no focal motor deficits. His only sign was mild right papilledema. All blood tests were normal.
A plain CT head [Figure 1] revealed a thin isodense subdural collection overlying the left cerebral convexity with 4 mm of midline shift. Sulcal effacement and distortion of the frontal horn of the left lateral ventricle could also be seen. There was no acute hemorrhage or fracture.
Figure 1.
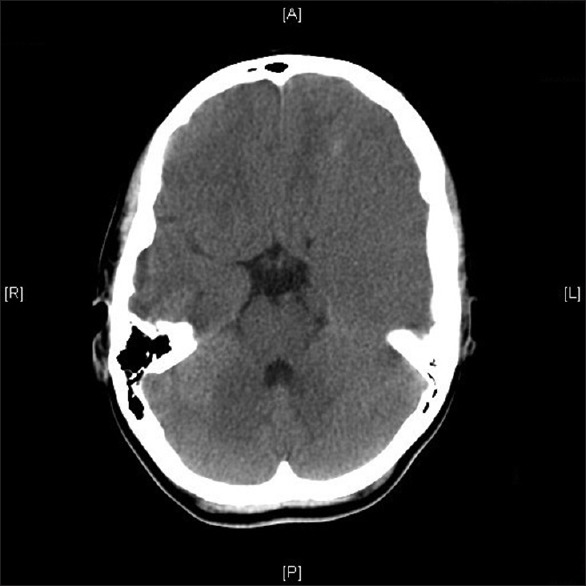
Axial computed tomography head: Thin left hemispheric subdural collection
Discussion
Arachnoid cysts are benign developmental malformations arising in the arachnoid membrane. Minor head trauma often precedes complications causing rupture of small bridging vessels between the dura and outer membrane of the cyst.[1] It can cause intracystic or extracystic hemorrhage.[2] In this case, intra- and extra-cystic bleeding had occurred simultaneously causing an isodense arachnoid cyst with an accompanying subdural collection. The degree of midline shift was a clue to this radiographically occult pathology.
The child was managed surgically first with a left-sided burr hole evacuation of the chronic subdural hematoma. However, he continued to have persistent headache for 3 days after surgery. A second CT head scan was, therefore, performed [Figure 2], revealing the left middle cranial fossa arachnoid cyst causing the residual midline shift. This was also managed surgically with a temporal craniotomy and marsupialization of the high-pressure cyst [Figures 3 and 4].
Figure 2.

Axial computed tomography brain: Postburr hole drainage: Left temporal arachnoid cyst revealed
Figure 3.
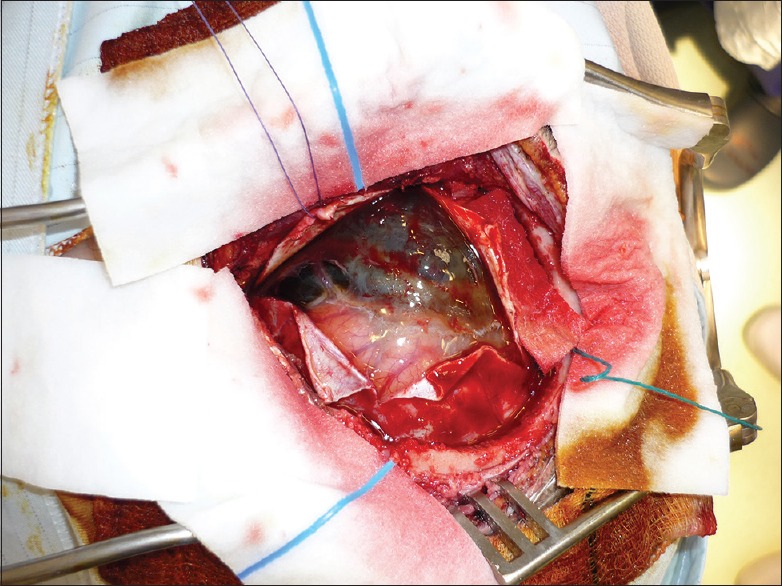
Photograph: Craniotomy to reveal membrane of arachnoid cyst
Figure 4.
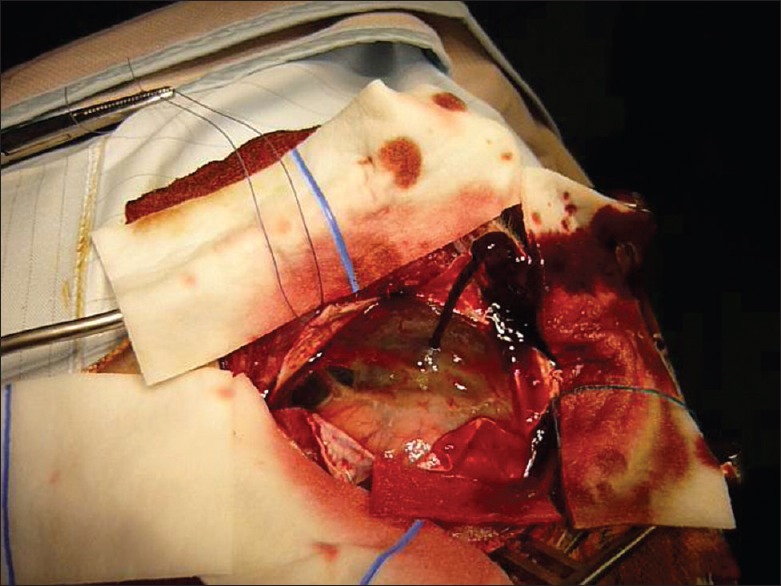
Photograph: Evacuation of high-pressure cystic hematoma
The majority of arachnoid cysts are incidental findings on brain imaging and do not require treatment. However, surgical intervention is widely accepted in symptomatic patients. Treatment options vary and include microscopic or endoscopic cystocisternostomy, cyst wall resection, and shunt insertion.
In this case, the cyst was located in the cerebral convexity and had displaced deeper brain structures; therefore, craniotomy for cyst wall resection/marsupialization was indicated.[3] There is increasing evidence to suggest that fenestrations made endoscopically are as safe and effective as open surgical techniques.[4]
Conclusion
Arachnoid cysts can be isodense on CT as has been demonstrated here. Magnetic resonance imaging should show the cyst as a well-defined nonenhancing mass that is isointense to cerebrospinal fluid and should, therefore, be considered in any child presenting with a subdural collection.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- 1.Kwak YS, Hwang SK, Park SH, Park JY. Chronic subdural hematoma associated with the middle fossa arachnoid cyst: Pathogenesis and review of its management. Childs Nerv Syst. 2013;29:77–82. doi: 10.1007/s00381-012-1896-4. [DOI] [PubMed] [Google Scholar]
- 2.Cress M, Kestle JR, Holubkov R, Riva-Cambrin J. Risk factors for pediatric arachnoid cyst rupture/hemorrhage: A case-control study. Neurosurgery. 2013;72:716–22. doi: 10.1227/NEU.0b013e318285b3a4. [DOI] [PubMed] [Google Scholar]
- 3.Duz B, Kaya S, Daneyemez M, Gonul E. Surgical management strategies of intracranial arachnoid cysts: A single institution experience of 75 cases. Turk Neurosurg. 2012;22:591–8. doi: 10.5137/1019-5149.JTN.5616-11.0. [DOI] [PubMed] [Google Scholar]
- 4.Johnson RD, Chapman S, Bojanic S. Endoscopic fenestration of middle cranial fossa arachnoid cysts: Does size matter? J Clin Neurosci. 2011;18:607–12. doi: 10.1016/j.jocn.2010.10.006. [DOI] [PubMed] [Google Scholar]


