Abstract
Background
Despite the increasing use of nasoalveolar molding (NAM) in early cleft treatment, questions remain about its effectiveness. This study examines clinician and caregiver appraisals of primary cleft lip and nasal reconstruction with and without NAM in a non-randomized, prospective multicenter study.
Methods
Participants were 110 infants with cleft lip/palate (62 treated with NAM and 48 treated without NAM (NO-NAM)) and their caregivers seeking treatment at one of six high-volume cleft centers. Using the Extent of Difference Scale, standard photos for a randomized subset of 54 infants were rated pre-treatment and post-surgery by an expert clinician blinded to treatment group. Standard blocked and cropped photos included frontal, basal, left and right views of the infants. Using the same scale, caregivers rated their infants’ lip, nose, and facial appearance compared to the general population of infants without clefts pre-treatment and post-surgery. Multilevel modeling was used to model change in ratings of infants’ appearance pre-treatment and post-surgery.
Results
The expert clinician ratings indicated that NAM-treated infants had more severe clefts at pre-treatment; yet both groups were rated equally post-surgery. NAM caregivers reported better post-surgery outcomes compared to NO-NAM caregivers (p<0.05), particularly in relation to the appearance of the nose.
Conclusions
Despite having a more severe cleft before treatment, infants who underwent NAM were found by clinician ratings to have comparable results to those who underwent lip repair alone. Infants who underwent NAM were perceived by caregivers to have better treatment outcomes than those that underwent lip repair without NAM.
INTRODUCTION
The development of nasoalveolar molding (NAM) was inspired by the need for more reproducible and better aesthetic results following primary cleft lip and nasal reconstruction despite cleft severity [1, 2]. Through weekly or biweekly modifications of an alveolar molding plate and nasal stent, NAM is designed to align the alveolar segments, lengthen the columella, increase nasal tip projection, shape the lower lateral cartilages, medially transpose the alar base, and stretch the intranasal lining [3, 4].
A growing number of cleft centers now offer NAM [5] and research has reported on the benefits of NAM or a similar variation of presurgical orthopedics [6, 7]. For example, patients with unilateral cleft lip who undergo NAM reportedly demonstrate greater nasal symmetry through 9 years of age than patients with unilateral cleft lip who do not have NAM [8]. Additionally, compared to children without cleft, patients with bilateral clefts treated with NAM have near normal nasal morphology through 12.5 years of age [9]. Despite the increasing volume of NAM research, use of NAM remains an area of active debate [3, 10]. The transition from small, retrospective, single-center reports, to larger, prospective, multi-center studies is necessary to provide more robust scientific outcomes regarding treatment effectiveness. To date, virtually all reports on the effects of NAM on facial appearance have been of the former design.
The evaluation of facial appearance is an important outcome variable in the study of health-related quality of life and the impact of cleft treatment [11–13]. Given the importance of facial attractiveness, much research has been devoted to understanding subjective evaluations or ratings of facial difference. However, the selection and composition of raters may have a significant impact on study findings [11]. For example, even though laypersons and professionals can reliably differentiate between varying levels of facial attractiveness [14], professionals reportedly rate facial difference more severely than laypersons [15, 16]. This rating discrepancy may be attributed to medical training that teaches professionals to be more aware and critical of minute differences in facial appearance. The relevance of patient-reported outcomes is now recognized as a crucial endpoint in treatment success [17], yet relatively little is known about how caregiver evaluations of appearance compare to evaluations by healthcare professionals. This non-randomized, prospective, multicenter study investigates the subjective assessment of the surgical outcomes of primary cleft lip and nasal repair with and without NAM by both caregivers and an experienced clinician, blinded to treatment group, time and site. The research questions are: 1) What is the expert clinician’s assessment of facial appearance before and after cleft lip and nasal repair in infants undergoing NAM compared to infants undergoing traditional care without NAM (NO-NAM), and 2) What are the caregivers’ assessment of their infants’ facial appearance before and after cleft lip and nasal repair in infants undergoing NAM compared to NO-NAM?
PATIENTS AND METHODS
Sample/Procedures
This non-randomized, prospective multicenter study includes patients undergoing cleft lip reconstruction at six cleft/craniofacial centers: University of North Carolina-Chapel Hill, Oregon Health and Science University, New York University Langone Medical Center, Children's Healthcare of Atlanta, Mercy Children’s Hospital (St. Louis, MO), and Riley Hospital for Children (Indianapolis, IN). All study sites are approved by the Commission on Approval of Teams (CAT) of the American Cleft Palate Craniofacial Association (ACPA) and Cleft Palate Foundation (CPF) and are high volume, nationally recognized, and geographically diverse cleft centers. The caregivers of infants with non-syndromic complete unilateral or bilateral cleft lip with or without a cleft palate and no other major medical issues were recruited for the study. Caregivers with a major psychiatric disorder (e.g., schizophrenia) that might interfere with their ability to adhere to the study protocol or who could not speak or understand English or Spanish were excluded. Spanish interpreters were available on-site, as needed.
In all instances, reconstructive surgeons at the study sites delivered the study’s outlined standardized treatment presentation to eligible caregivers, regardless of cleft severity. This presentation included viewing pre- and post-surgery photographs, explaining treatment protocol(s), and answering questions. Once the caregivers made a treatment decision for their infants as either NAM (early intervention with NAM followed by cleft lip surgery) or NO-NAM (cleft lip surgery only), patient care coordinators were then responsible for recruiting and obtaining the caregivers’ written informed consent. The caregivers’ treatment decision alone determined group assignment. Caregivers consented to complete questionnaires and to have photographs taken of their infant for viewing by a clinician rater. The project was approved by the Institutional Review Board at each institution.
One hundred and ten patients were recruited to this study: 62 infants had NAM and 48 underwent surgical repair alone (NO-NAM). Forty-nine (79%) of the children treated with NAM and 35 (73%) of the children treated without NAM had unilateral clefts. NAM caregivers completed the Extent of Difference (EOD) questionnaire prior to NAM treatment (infant ~6 weeks old), at the end of NAM treatment and prior to lip surgery, and following secondary palate surgery (infant ~13 months old). NO-NAM caregivers completed the EOD questionnaire prior to lip surgery and following secondary palate surgery (~13 months old).
Measure
Extent of Difference (EOD) Scale
The EOD includes a four-point rating of the appearance of the infant’s overall face, nose, and lips as compared to children without cleft in the general population: 0 - same as other children (not different); 1 - a little different (mildly different), 2 - more than a little different (moderately different), and 3 - very different. The EOD is an adaptation of the severity scale developed by Kuijpers-Jagtman, et al. [18], which is also similar to the scale used in a recent Americleft study [19]. The interrater reliability of the instrument is .80 which was attained at the calibration meeting for our multicenter study on Quality of Life in Children with Cleft. The EOD has been referenced in several publications [20, 21] and has demonstrated excellent discriminative validity. Using the EOD rating scale, the clinician rated standardized photographs of the infants. The caregivers used the same EOD scale to directly rate the appearance of their infants’ face.
Photographs
Standardized facial photographs were taken in four poses (frontal, right and left profile, and basal) pre-treatment and post-surgery (~13 months of age). An electronic manual was created to standardize photographs across sites. The full-face frontal photograph was taken at repose (not smiling) with the head oriented in a neutral position. Profile photographs were taken from both the left and right sides, again with the infant’s head in a neutral position. For basal photographs, infants were seated with their backs straight and their heads positioned at a 45-degree angle so that they were looking at the ceiling. Each photograph was cropped, blocked, and numerically coded by a research coordinator at each site and uploaded to a secure website. After cropping and blocking, a quality assurance review was carried out by the principal investigator at each site. A sample of the standardized poses is presented in Figure 1.
Figure 1.
Sample post-surgery photographs illustrating the four poses rated by the expert clinician.
Figure 1 A is frontal pose;
Figure 1 B is left pose;
Figure 1 C is right pose;
Figure 1 D is basal pose
Thirty-seven sets of photographs of infants treated with NAM and 17 sets of infants treated without NAM were randomly selected for rating by an experienced cleft surgeon. A total of 125 sets of photographs (54 Subjects x 2 time points + 17 randomly selected duplicate sets) were randomly ordered for rating. The clinician rater, blinded to treatment group, time point, and site, evaluated each set of photographs for each child at each of the two time points. This clinician was not responsible for providing any treatment to these infants. After viewing each photographic pose, the clinician rated the appearance of the infant’s face, nose, and lip using the EOD standard four-point scale.
Statistical Analysis/Modeling
Clinician and caregiver ratings were analyzed separately. The clinician rated each photographic pose (i.e., front, basal, left and right) of the infants (patients) separately (before and after treatment), whereas caregivers were asked to compare the overall appearance of their child’s nose, lips, and face to a child without a cleft in the general population. To compare the two ratings, we provide correlation coefficients. For the clinician’s rating of appearance, intra-rater reliability was assessed by weighted kappa for concordance. Bivariate comparisons report p-values derived from t-tests. Because data contain repeated measures of cleft severity, multilevel modeling was used to allow us to account for attrition and for regression to the mean. Laterality of cleft was associated with clinician-rated severity, so we accounted for whether clefts were right unilateral, left unilateral, or bilateral. We examined non-linearity in sensitivity analyses and examined distributional assumptions. Since clinician ratings were not normal, generalized linear modeling was used. We report results from the EOD comparing NAM-treated and NO-NAM treated children. Results from all models provide beta-coefficients, standard errors, and exact p-values. To assess the explanatory power of each model, we calculated Pseudo-R2. Statistical analyses were done using Stata 13.1 IC [22].
RESULTS
Clinician Ratings
The concordance of the clinician ratings for the face, nose, and lips was excellent for the basal and frontal poses (Kappa > 0.83). The kappa values for the profile poses indicated good to excellent agreement (0.58 to 1.0). For the basal and frontal poses, 94% of the ratings for the face, nose, and lip were rated as severe before surgery. One-third to one-half of the infants in both treatment groups were rated as no different or only mildly different from normal post-surgery. Across the nose, lip, and face, the clinician rated infants as very different at baseline and mildly-moderately different post-surgery. The clinician was consistent across facial areas. The clinician found that overall, most photos indicated moderate to severe differences (Table 1) at baseline.
Table 1.
Characteristics of caregiver (n=118) and clinician (n=54) ratings
| Caregiver rater
|
Clinician rater
|
|||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Caregiver ratings | Lip | Baseline | 2.03 | 0.92 | 2.65 | 0.79 |
| Post-surgery | 1.20 | 0.76 | 1.51 | 0.62 | ||
| Nose | Baseline | 1.70 | 0.91 | 2.55 | 0.88 | |
| Post-surgery | 0.97 | 0.62 | 1.40 | 0.77 | ||
| Face | Baseline | 1.43 | 0.89 | 2.66 | 0.79 | |
| Post-surgery | 0.74 | 0.53 | 1.62 | 0.68 | ||
| Caregiver age | Baseline | 30.29 | 6.24 | |||
|
| ||||||
| Percent | Percent | |||||
|
| ||||||
| Bilateral cleft | Baseline | 22.41% | 28.30% | |||
| Caregiver male | Baseline | 9.57% | ||||
| Cleft lip/palate | Baseline | 74.14% | 84.54% | |||
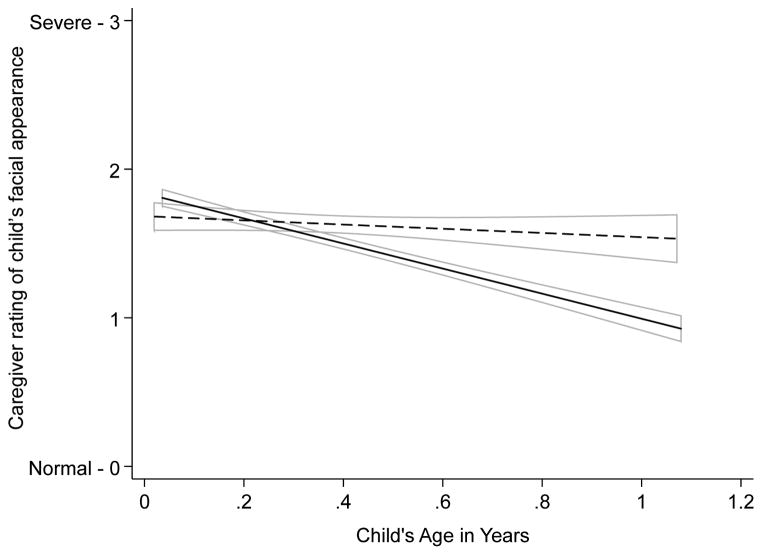
Examining clinician-rated appearance severity by treatment status (Table 2), we find that the NO-NAM group began with, on average, less severely rated clefts. The risk of more severe categorizations decreased between pre-treatment and post-surgery visits for NO-NAM patients. However, those with NAM treatment showed a decline in severity compared to those with traditional treatment. While this pattern was evident across lip, nose, and face, results were strongest when examining the nose (B=−0.52 (p=0.025), versus −0.37 on Table 2). To visually clarify the pattern found in Table 3, we provide trajectories in clinician-rated appearance associated with treatment (Figure 2). Trajectories show that those treated with NAM therapy were, on average, more severely rated at baseline and then experienced larger declines in clinician-rated severity that were sufficient to eradicate pre-surgical differences in cleft-related severity.
Table 2.
Beta coefficients, standard errors, and exact p-values examining the association between treatment and clinician-rated cleft severity derived from random coefficients multilevel modeling adjusting for cleft type in relation to direction and area of photograph.
| B | SE | P | |
|---|---|---|---|
| NO NAM Treatment | Reference | ||
| NAM Treatment | 0.37 | 0.13 | 0.004 |
| Post-surgical visit | −1.11 | 0.11 | <0.001 |
| NO NAM Treatment | Reference | ||
| NAM x Post-surgical visit | −0.37 | 0.14 | 0.010 |
| Constant | 0.89 | 0.13 | |
|
| |||
| Pseudo-R2 | 0.29 | <0.001 | |
Note: Models account for pose, side of the face, cleft-type (right or left unilateral or bilateral).
Table 3.
Beta-coefficients, standard errors, and exact p-values derived from mixed effects longitudinal models examining the association between treatment track and change in caregivers’ overall ratings of the appearance of their children with clefts.
| Model 1
|
Model 2
|
Model 3
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| B | SE | P | B | SE | P | B | SE | P | |
| NO NAM Treatment | Reference | Reference | Reference | ||||||
| NAM Treatment | -0.026 | 0.112 | 0.819 | −0.018 | 0.111 | 0.872 | −0.080 | 0.115 | 0.484 |
| Child's Age | −0.424 | 0.106 | <0.001 | −0.421 | 0.106 | <0.001 | −0.440 | 0.106 | <0.001 |
| Traditional Treatment | Reference | Reference | Reference | ||||||
| NAM Treatment x Child's Age | −0.375 | 0.129 | 0.004 | −0.377 | 0.129 | 0.003 | −0.364 | 0.128 | 0.005 |
| Caregiver Age | 0.007 | 0.005 | 0.208 | 0.008 | 0.005 | 0.121 | |||
| Female Caregiver | Reference | Reference | |||||||
| Male Caregiver | 0.093 | 0.109 | 0.393 | 0.054 | 0.110 | 0.625 | |||
| Unilateral Cleft | Reference | ||||||||
| Bilateral Cleft | 0.125 | 0.079 | 0.117 | ||||||
| Cleft Lip Only | Reference | ||||||||
| Cleft Lip/Palate | 0.133 | 0.082 | 0.105 | ||||||
| Constant | 1.844 | 0.152 | 1.630 | 0.217 | 1.508 | 0.223 | |||
|
| |||||||||
| Pseudo−R2 | 0.11 | 0.031 | 0.11 | <0.001 | 0.11 | <0.001 | |||
| Change in R2 | 0.00 | 0.844 | 0.00 | 0.761 | |||||
Note: Models examining the association between covariates and change in cleft severity over time yield similar results.
Figure 2.
Treatment-related differences in clinician severity ratings of photographs by treatment type and pre/post-operative status among those who were NO-NAM treated (dark gray) and those who were NAM-treated (light gray box). 95% confidence intervals are provided (error bars).
Caregivers’ ratings
Caregivers rated the appearance difference of their children’s clefts as moderately different at baseline and mildly different post-surgery (Table 1). Caregiver ratings were moderately correlated with clinician ratings of frontal or basal, but not profile, views (ranging from 0.37 to 0.55 overall). For example, the caregiver rating of the nose was associated with the clinician’s ratings of basal and frontal poses (r=0.55 and 0.44 respectively). Notably, there was no treatment group difference at baseline in caregiver ratings for the nose, lip, or face (P=0.492, 0.518, and 0.216 respectively).
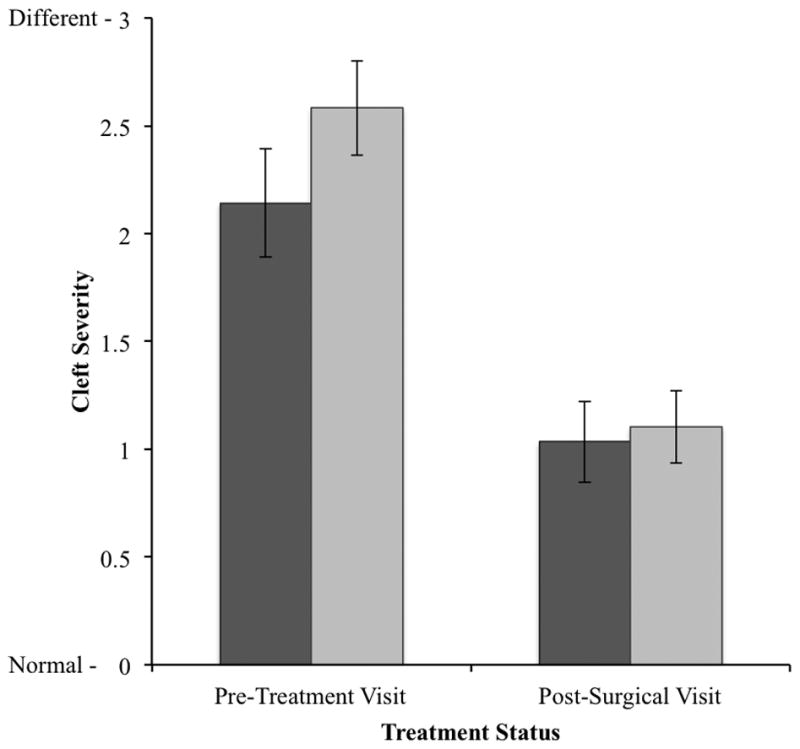
Examining the association between NAM treatment and changes in caregiver-rated severity over time, NAM treatment was associated with improved caregiver ratings over the treatment period after surgery (Table 3, Model 1). Adjusting for caregiver age and sex (Model 2) and child’s cleft type (Model 3) did not change results. Subscale results suggested that the pattern of results was consistent for lip, nose, and face. However, the NAM treatment group showed larger benefits to the appearance of the nose: the NO-NAM group showed no significant improvement in the nose over time (B=−0.19, P=0.299) while the NAM group showed a three-fold greater improvement over time (B=−0.58, P=0.007).
To visually explain these results, we provide trajectories of caregivers’ ratings of child’s appearance over child’s age in years by treatment status (Figure 3). Coefficients provided in Table 3 show that at post-surgery (at around 13 months of age), caregivers whose children underwent NAM reported seeing a greater improvement in their child’s overall appearance as compared to the caregivers of children who underwent traditional treatment.
Figure 3.
Expected longitudinal trajectories of change in caregivers’ ratings of children’s appearance as children age among those whose children are undergoing NO-NAM treatment (black dashed lines) and NAM treatment (solid black lines). 95% Confidence Intervals are provided (gray outlines).
DISCUSSION
This pilot project is the first non-randomized, prospective multicenter study comparing a cleft clinician’s and caregivers’ perceptions of infants’ appearance outcomes following primary cleft lip and nasal reconstruction with and without nasoalveolar molding (NAM). The blinded clinician/rater reported a more severe presurgical cleft difference in the NAM group compared to the NO-NAM group, and a greater improvement in facial appearance in the NAM group post-surgery. After surgical intervention, both the NAM and NO-NAM groups were found to have equivalent facial difference ratings, despite the greater pre-treatment severity in facial difference in the NAM group. Longitudinal analyses of perception of change showed a statistically significant improvement in cleft lip and nasal repair for NAM caregivers compared to NO-NAM caregivers. NAM caregivers also rated their children as experiencing greater improvement in appearance differences over time than did their NO-NAM counterparts. The benefits of NAM were, in the caregivers’ ratings, strongest in relation to the appearance of the nose.
Examining caregiver perceptions of treatment outcomes is relevant and congruent with new initiatives in patient-oriented research and care [23]. While previous research has used professional ratings of treatment photographs [24], this study is novel because it includes the caregivers, who are important stakeholders in their infants’ cleft treatment. Knowledge gained from this report and other patient-oriented outcomes studies has implications for: 1) informing treatment decision-making for both cleft teams and caregivers; 2) determining cost effectiveness of early cleft treatment options; and 3) providing baseline information on long-term cost effectiveness. To date, this report is the first to indicate that both professional and caregiver subjective evaluations exhibited greater appearance improvement among the NAM-treated children in comparison to traditional treatment without NAM.
Although this report represents the strongest scientific evidence to date on the effectiveness of NAM, the study is not without limitations. Patients were assigned to treatment group largely by institutional protocol and patient preference, not by randomization. Such may account for pre-treatment differences in clinician-rated severity in the NAM group. Although the surgeons at each of the study sites are experienced cleft surgeons, variations may exist in individual surgical skills, techniques, and outcomes. While randomization is the best way to control for unobserved surgical experience [26], ethical and logistical difficulties often limit the utility of such methods. In our results, there is no definitive reason to believe that NAM treatment would unduly influence caregivers’ views of their own infants over time. Because the study is observing caregivers as they proceed through their agreed-upon scheduled treatments, and not through an intervention provided by the study itself, it is unlikely that NAM and NO-NAM caregivers would be differently influenced by study participation. Furthermore, the clinician rater was blinded and photos were both duplicated and randomized, thereby removing the possibility of an association between treatment and the outcome. Moreover, the clinician and caregiver ratings were associated suggesting that both were similarly rating severity of the child’s cleft, and results from both find larger improvements in cleft severity associated with NAM treatment. Relying on one clinician provides useful clarity and reduces unnecessary variability in clinician ratings and the excellent intrarater reliability found in this study is noteworthy. However, results may be more or less severe because of the clinician’s specific characteristics. Future studies should use a panel of expert clinicians to provide more generalizable estimates of cleft severity. Finally, while the EOD is a four-point scale that has been used in multiple studies and has demonstrated positive psychometric worthiness [27, 28].
The fact that the results from this pilot study reference a small sample highlights the need for replication. Additionally, the treatment outcomes assessed are short-term, which underscores that follow-up and reassessing the effects of initial cleft treatment on facial growth and aesthetic form are crucial. Furthermore, the potential additional stress that NAM places on caregivers is just beginning to be understood and should be the focus of continued research [25]. Long-term follow-up in the NAM patient population should also address potential risks of this therapy to maxillary growth [10]. Finally, given that this study was underpowered to do so, future research should examine the bilateral cleft nasal deformity using long-term multicenter outcomes.
CONCLUSIONS
In this non-randomized, prospective multicenter study, the expert clinician rated the NAM group to have a more severe cleft pre-treatment. Caregivers reported significantly greater results in facial appearance after primary cleft lip and nasal repair in their infants who underwent NAM compared to caregivers whose infants underwent traditional care. Therefore, even if no significant differences were noted after primary lip and nasal surgery between the two treatment groups, the NAM patients had a greater level of improvement as they started with a more severe condition. Yet no group difference was observed in facial appearance post-surgery.
Acknowledgments
The authors acknowledge the financial support of NIDCR grant #DE021853, Caregivers Responses to Nasoalveolar Molding and Early Cleft Care (Broder, PI). We thank the research PIs (Drs. John Riski, Barry Grayson, Jeffrey Marsh, Sunil Tholpady) and the sites’ clinical teams for their dedication to research and provision of care. We appreciate the time and effort of the caregivers.
Footnotes
Statement of Author Role/Participation:
Hillary L. Broder participated in concept formation and manuscript preparation. Sean Clouston and Ceib Phillips participated in data analysis and manuscript preparation. Roberto Flores, Judah Garfinkle, and Lacey Sischo participated in manuscript preparation. Richard Kirschner completed the photograph ratings and manuscript revisions.
Financial Disclosure:
This research was supported by NIH/NIDCR grant #DE021853 (H. Broder, PI).
References
- 1.Grayson BH, Maull D. Nasoalveolar molding for infants born with clefts of the lip, alveolus, and palate. Clinics in Plastic Surgery. 2004;31(2):149–158. doi: 10.1016/S0094-1298(03)00140-8. [DOI] [PubMed] [Google Scholar]
- 2.Grayson BH, Santiago PE, Brecht LE, Cutting CB. Presurgical nasoalveolar molding in infants with cleft lip and palate. Cleft Palate−Craniofacial Journal. 1999;36(6):486–498. doi: 10.1597/1545-1569_1999_036_0486_pnmiiw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 3.Grayson BH, Garfinkle JS. Early cleft management: the case for nasoalveolar molding. Am J Orthod Dentofacial Orthop. 2014;145(2):134–42. doi: 10.1016/j.ajodo.2013.11.011. [DOI] [PubMed] [Google Scholar]
- 4.Lee CT, Garfinkle JS, Warren SM, Brecht LE, Cutting CB, Grayson BH. Nasoalveolar molding improves appearance of children with bilateral cleft lip-cleft palate. Plastic and Reconstructive Surgery. 2008;122(4):1131–7. doi: 10.1097/PRS.0b013e318184590c. [DOI] [PubMed] [Google Scholar]
- 5.Sischo L, Chan JW, Stein M, Smith C, van Aalst J, Broder HL. Nasoalveolar Molding: Prevalence of Cleft Centers Offering NAM and Who Seeks It. Cleft Palate Craniofac J. 2012;49(3):270–5. doi: 10.1597/11-053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gomez DF, Donohue ST, Figueroa AA, Polley JW. Nasal Changes After Presurgical Nasoalveolar Molding (PNAM) in the Unilateral Cleft Lip Nose. Cleft Palate-Craniofacial Journal. 2012;49(6):689–700. doi: 10.1597/11-007. [DOI] [PubMed] [Google Scholar]
- 7.Chang CS, Por YC, Liou EJ, Chang CJ, Chen PK, Noordhoff MS. Long-term comparison of four techniques for obtaining nasal symmetry in unilateral complete cleft lip patients: a single surgeon's experience. Plastic and Reconstructive Surgery. 2010;126(4):1276–84. doi: 10.1097/PRS.0b013e3181ec21e4. [DOI] [PubMed] [Google Scholar]
- 8.Barillas I, Dec W, Warren SM, Cutting CB, Grayson BH. Nasoalveolar Molding Improves Long-Term Nasal Symmetry in Complete Unilateral Cleft Lip-Cleft Palate Patients. Plastic and Reconstructive Surgery. 2009;123(3):1002–1006. doi: 10.1097/PRS.0b013e318199f46e. [DOI] [PubMed] [Google Scholar]
- 9.Garfinkle JS, King TW, Grayson BH, Brecht LE, Cutting CB. A 12-Year Anthropometric Evaluation of the Nose in Bilateral Cleft Lip-Cleft Palate Patients following Nasoalveolar Molding and Cutting Bilateral Cleft Lip and Nose Reconstruction. Plastic and Reconstructive Surgery. 2011;127(4):1659–1667. doi: 10.1097/PRS.0b013e31820a64d7. [DOI] [PubMed] [Google Scholar]
- 10.Hathaway RR, Long RE., Jr Early cleft management: in search of evidence. Am J Orthod Dentofacial Orthop. 2014;145(2):135–41. doi: 10.1016/j.ajodo.2013.11.012. [DOI] [PubMed] [Google Scholar]
- 11.Al-Omari I, Millett DT, Ayoub AF. Methods of assessment of cleft-related facial deformity: a review. Cleft Palate Craniofac J. 2005;42(2):145–56. doi: 10.1597/02-149.1. [DOI] [PubMed] [Google Scholar]
- 12.Sarwer DB, Bartlett SP, Whitaker LA, Paige KT, Pertschuk MJ, Wadden TA. Adult psychological functioning of individuals born with craniofacial anomalies. Plastic and Reconstructive Surgery. 1999;103(2):412–418. doi: 10.1097/00006534-199902000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child's version) Community Dentistry and Oral Epidemiology. 2007;35(Suppl 1):20–31. doi: 10.1111/j.1600-0528.2007.0002.x. [DOI] [PubMed] [Google Scholar]
- 14.Tobiasen JM. Scaling facial impairment. Cleft Palate J. 1989;26(3):249–54. discussion 254. [PubMed] [Google Scholar]
- 15.Ritter K, Trotman CA, Phillips C. Validity of subjective evaluations for the assessment of lip scarring and impairment. Cleft Palate Craniofac J. 2002;39(6):587–96. doi: 10.1597/1545-1569_2002_039_0587_voseft_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 16.Al-Omari I, Millett DT, Ayoub A, Bock M, Ray A, Dunaway D, et al. An appraisal of three methods of rating facial deformity in patients with repaired complete unilateral cleft lip and palate. Cleft Palate Craniofac J. 2003;40(5):530–7. doi: 10.1597/1545-1569_2003_040_0530_aaotmo_2.0.co_2. [DOI] [PubMed] [Google Scholar]
- 17.Rozier RG, Pahel BT. Patient- and Population-Reported Outcomes in Public Health Dentistry: Oral Health-Related Quality of Life. Dental Clinics of North America. 2008;52(2):345–365. doi: 10.1016/j.cden.2007.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Kuijpers-Jagtman AM, Nollet PJ, Semb G, Bronkhorst EM, Shaw WC, Katsaros C. Reference photographs for nasolabial appearance rating in unilateral cleft lip and palate. Journal of Craniofacial Surgery. 2009;20(Suppl 2):1683–6. doi: 10.1097/SCS.0b013e3181b3ed9c. [DOI] [PubMed] [Google Scholar]
- 19.Mercado A, Russell K, Hathaway R, Daskalogiannakis J, Sadek H, Long RE, et al. The americleft study: an inter-center study of treatment outcomes for patients with unilateral cleft lip and palate part 4. Nasolabial aesthetics. Cleft Palate Craniofac J. 2011;48(3):259–64. doi: 10.1597/09-186.1. [DOI] [PubMed] [Google Scholar]
- 20.Broder HL, Wilson-Genderson M, Sischo L. Reliability and validity testing for the Child Oral Health Impact Profile-Reduced (COHIP-SF 19) Journal of Public Health Dentistry. 2012;72(4):302–12. doi: 10.1111/j.1752-7325.2012.00338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Broder HL, Wilson-Genderson M, Sischo L, Norman RG. Examining factors associated with oral health-related quality of life for youth with cleft. Plast Reconstr Surg. 2014;133(6):828e–834e. doi: 10.1097/PRS.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.StataCorp. Stata Statistical Software: Release 13. StataCorp LP; College Station, TX: 2013. [Google Scholar]
- 23.Selby JV, Beal AC, Frank L. The Patient-Centered Outcomes Research Institute (PCORI) national priorities for research and initial research agenda. JAMA. 2012;307(15):1583–4. doi: 10.1001/jama.2012.500. [DOI] [PubMed] [Google Scholar]
- 24.Rubin MS, Clouston S, Ahmed MM, Lowe KM, Shetye PR, Broder HL, et al. Assessment of Presurgical Clefts and Predicted Surgical Outcome in Patients Treated With and Without Nasoalveolar Molding. Journal of Craniofacial Surgery. 2015;26(1):75–79. doi: 10.1097/SCS.0000000000001233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sischo L, Broder HL, Phillips C. Coping With Cleft: A Conceptual Framework of Caregiver Responses to Nasoalveolar Molding. Cleft Palate Craniofac J. 2014 doi: 10.1597/14-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roberts CT, Semb G, Shaw WC. Strategies for the Advancement of Surgical Methods in Cleft-Lip and Palate. Cleft Palate-Craniofacial Journal. 1991;28(2):141–149. doi: 10.1597/1545-1569_1991_028_0141_sftaos_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 27.Osman MM, Cohade C, Nakamoto Y, Wahl RL. Respiratory motion artifacts on PET emission images obtained using CT attenuation correction on PET-CT. European Journal of Nuclear Medicine and Molecular Imaging. 2003;30(4):603–606. doi: 10.1007/s00259-002-1024-x. [DOI] [PubMed] [Google Scholar]
- 28.Affleck G, Tennen H, Pfeiffer C, Fifield J. Appraisals of Control and Predictability in Adapting to a Chronic Disease. Journal of Personality and Social Psychology. 1987;53(2):273–279. doi: 10.1037//0022-3514.53.2.273. [DOI] [PubMed] [Google Scholar]