Abstract
Little is known about how to integrate primary care with mental/behavioral services outside of clinical trials. The authors implemented a collaborative care model (CCM) for depression in a safety net patient-centered medical home. The model focused on universal screening for symptoms, risk stratification based on symptom severity, care management for intensive follow-up, and psychiatry consultation. CCM increased rates of primary care physician encounters, timely follow-up for monitoring symptoms of depression, and documentation of treatment response. Contextual factors that facilitated or hindered practice redesign included clinic leadership, quality improvement culture, staffing, technology infrastructure, and external incentives/disincentives for organizational change. (Population Health Management 2016;19:46–55)
Background
Depression is one of the most common chronic conditions encountered in primary care. Given the prevalence of and complex interactions between comorbid mental and physical health conditions, successful management of depression in primary care settings is a major public health priority. A number of studies have demonstrated that the collaborative care model (CCM) is effective for improving management of depression in primary care.1,2 The Community Preventive Services Task Force defines collaborative care for depressive disorders as “a multicomponent, healthcare system-level intervention using case managers to link primary care providers, patients, and mental health specialists.”3 Core components of effective CCM depression care programs include population health management, measurement-based care (eg, using standardized tools to monitor symptoms), and “stepped care” in which treatment plans are systematically adjusted until treatment goals are achieved.4 CCM for depressive disorders improves physical and mental health outcomes, quality of life/functional status, satisfaction with care, and provides good economic value in terms of lower cost of care.1,2,5
Integration of primary care with mental/behavioral health services is now being promoted as a preferred model of care. However, there are multiple clinical, administrative, and financial factors that contribute to operational success.6 Health service delivery redesign, practice culture change, consolidation of information systems, care team expansion as well as cross-disciplinary training, accountability, and coordination of care among primary care providers and mental health specialists is required. In a recent study examining collaborative care for depression in community health centers, participating organizations displayed significant variability in their ability to enact system-level practice changes, as evidenced by differences in quality indicators and outcomes, despite receiving similar training and resources to do so.7
Little is known about how to implement such changes outside of well-controlled clinical trials. This article describes the practice transformation and quality improvement context of a community health center that offers colocated primary care and mental/behavioral health services. The research team implemented CCM for depression care that focused on universal screening for symptoms of depression, risk stratification of patients based on symptom severity, care management for intensive follow-up, and psychiatry consultation. The team examines process of care for patients who received care in this setting. The team also examines whether there were differences in improvement of symptoms of depression among patients who received collaborative care versus those who received care from their primary care provider only. Finally, the research team describes facilitators and barriers to implementing CCM for depression care under typical practice conditions.
Methods
Study design, setting, and population
This is a retrospective observational study of depression care management implemented in a community health center in New Orleans, Louisiana. The research team conducted a chart review of adult patients (≥18 years of age) seen between July 2012 and April 2014. The center, which has maintained level 3 patient-centered medical home recognition by the National Committee for Quality Assurance since 2008, serves a population of mostly African Americans, publicly insured patients, and low-income working adults. The center is also a major teaching site for residency training in internal medicine and psychiatry. Tulane University's Institutional Review Board approved this study.
Historic context for practice transformation
Between 2007 and 2010, the health center participated in the Primary Care Access and Stabilization Grant (PCASG) along with 24 provider organizations to increase access to primary care and mental/behavioral health services for a mostly uninsured adult population in post-Katrina New Orleans. The health center continued integrating primary care and mental health through the Greater New Orleans Community Health Connection Medicaid 1115 Waiver program (2010–2014), which provided insurance coverage for adults who did not qualify for Louisiana Medicaid, and the New Orleans Charitable Fund (NOCHF, 2012 to 2015), which provided funding for mental health providers. In 2013, the health center became a Federally Qualified Health Center (FQHC), which enhanced reimbursement for services provided by primary care and mental health providers (including a licensed clinical social worker [LCSW]).
Depression care quality improvement
Between 2008 and 2010, the health center's administrative leaders, primary care providers (PCPs) and mental/behavioral health providers (MHPs) participated in the Mental Health Infrastructure and Training (MHIT) Program.8 The center's team also participated in collaborative learning sessions sponsored by PCASG and NOCHF to support integration of primary care, mental health, and social services. While participating in these initiatives, the center formed a quality improvement (QI) team, comprising the medical director (EPH), medicine-psychiatrist (DD), a LCSW, a community health worker, and a health coach, to perform rapid-cycle QI on depression care management using the Plan-Do-Study-Act model. The QI team met on a monthly basis to identify and define processes to support systematic depression screening, processing of referrals, scheduling, and billing procedures. The QI team monitored protocol adherence and clinical performance on a quarterly basis and collaborated with operations management for process improvement.
Collaborative care model
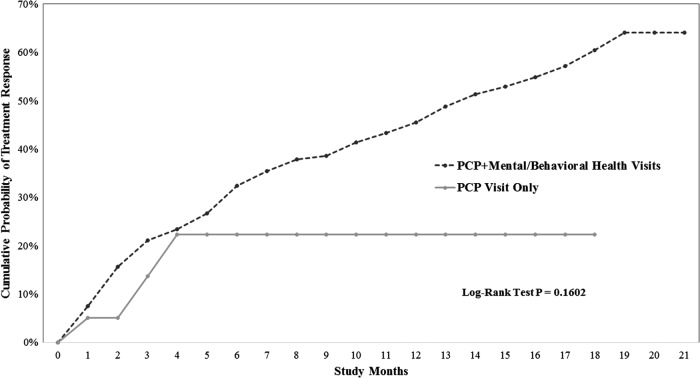
Figure 1 summarizes the health center's CCM for depression. In study year 1, medical assistants (MAs) used a 2-question depression screen at every visit as part of the intake process: “In the past 2 weeks have you been bothered by little interest or pleasure in doing things? In the past 2 weeks have you been bothered by feeling down depressed or hopeless?” If patients answered “yes” to at least 1 question, the MAs were to give patients the Patient Health Questionnaire (PHQ)-9,9 which was self-administered. The MAs then entered the PHQ-9 as a lab result in the electronic medical record (EMR). An adaptation of the PHQ-210 was used initially for the purpose of simplifying the workflow for MAs at triage. Because results of the 2-question screener were not entered into the EMR, it was difficult to assess protocol fidelity. The QI team then implemented the PHQ-210 as a universal screener in study year 2 and emphasized documentation in the EMR as a lab result. A PHQ-2 score of 3 or higher (range 0–6) has 83% sensitivity and 92% specificity for major depression.10 All patients who scored 3 or higher were then administered the PHQ-9. A PHQ-9 score of 10 or greater (range 0–27) has 88% sensitivity and specificity for major depression.9
FIG. 1.
Flowchart of collaborative care model for depression care. CHW, community health worker; LCSW, licensed clinical social worker; PCP, primary care provider; PHQ, Patient Health Questionnaire.
The lead psychiatrist (DD) reviewed guidelines with PCPs including assessment and diagnosis of depression; use of the PHQ-9 to screen for symptoms and monitor response to treatment; therapeutic options (medications, psychotherapy); and indications for referring to the LCSW, community health worker (CHW), or psychiatrist. If PCPs elected not to refer patients to care management, they were advised that patients with elevated PHQ-9 scores and a diagnosis of depression should be reevaluated in 4-week intervals for monitoring and treatment adjustment while symptoms are acute. PCPs were instructed to review patient responses to PHQ-9 items to verify accuracy and address concerns during the visit. Treatment plans were tailored to individual patients. Options included watchful waiting (1–2 months) with reassessment, antidepressant medication, psychotherapy, or a combination of these approaches. For depression care treatment goals, a decrease of 5 points in PHQ-9 score was considered clinically significant improvement, a decrease in score by 50% was responsive to therapy, and a decrease in score to less than 5 for 3 months was considered remission.1 If PHQ-9 scores indicated nonresponsiveness or partial response, then providers were to reassess the diagnosis and contributing factors, modify treatment plans, and/or refer to psychiatry and/or the LCSW. For patients with PHQ-9 scores ≥10, providers were encouraged to refer patients to depression care management with the mental health CHW and/or LCSW.
The mental health CHW, under LCSW and psychiatrist supervision, provided depression care management that involved patient education and assistance with self-care skills. The CHW conducted follow-up assessments to readminister the PHQ-9 every 4 weeks, monitor symptom progress, and review adherence to treatment and self-management goals. Follow-up assessments also included updating assets and barriers to recovery and self-management (supports, motivation, perceived stigma, comorbid medical conditions, cognitive problems, side effects, problems with the therapeutic relationship, logistical/economic/cultural factors). The CHW encouraged behavioral goal setting, facilitated connections with social resources, problem solved if goals were not met, and consulted regularly with psychiatry and the LCSW.
The LCSW depression care management caseload focused mostly on patients identified as high risk (PHQ-9 score ≥20). The LCSW followed up with patients in person or by phone to assess adherence to treatment plans, review symptom progress with PHQ-9 tracking, inquire about no-shows for recent appointments, review personal goals and help patients problem solve if goals were not met, and update assets/barriers/supports to recovery. The LCSW also offered counseling services as indicated (behavioral activation, psychotherapy, crisis planning, facilitating connection to substance abuse counseling, and treatment). Repeat PHQ-9 scores and updated care plans were flagged for PCP review. The LCSW also notified PCPs if patients' symptoms were not adequately improved within 10 weeks of starting or changing treatment. These notifications included reminders to consider medication change.
The lead psychiatrist (who is also a general internist) conducted weekly multidisciplinary team meetings with the LCSW, mental health CHW, and a health coach to review complex patient cases. The health coach's duties included counseling patients on an individual basis, developing the center's health and wellness programming (eg, walking groups, community-oriented patient education library), and connecting patients to community-based resources to achieve health goals. Health coaching activities covered weight loss management and physical activity; nutrition (reading food labels, healthy cooking); smoking cessation; hypertension, and diabetes and depression self-care tools. The health center had parallel QI initiatives whereby the clinical pharmacist provided care management for chronic medical conditions. The psychiatrists referred patients to the health coach and clinical pharmacist as part of their treatment plans for behavioral activation around healthy lifestyle choices and management of comorbid conditions.
The health center's PCPs and psychiatrists shared the same administrative and exam room work space, which facilitated curbside consultation and shared treatment planning. Patients who were nonresponsive to treatment plans (eg, no improvement in symptoms 8–10 weeks after being on optimal doses of medication) were eligible for “stepped care” with a psychiatrist and/or LCSW. If a “warm handoff” was requested and staff was available, MAs facilitated the handoff. Otherwise patients were scheduled for the next available appointment upon discharge from their PCP visits. The LCSW was scheduled for 50-minute assessments. Psychiatry conducted 60-minute new evaluations, 30-minute follow-up visits, and 15-minute visits for medication review. The psychiatrists provided consultation regarding psychotropic medication and suspected complicating diagnoses (eg, bipolar, psychotic, substance abuse, personality disorders). The LCSW provided psychotherapy, options for which included individual supportive therapy, group supportive therapy, individual cognitive behavioral therapy (CBT), family therapy, relaxation training, grief counseling, crisis counseling, and brief counseling on behavior change. CBT was the core approach to managing depression, and the LCSW employed strategies learned through the aforementioned MHIT Program.8 CBT was used to help patients break the connection between personal thoughts, individual actions, and interactions with people, which patients identified as negative and affecting symptoms of depression. The number of CBT sessions was tailored to individual patient needs and preferences.
Electronic medical records
The EMR system, SuccessEHS (Greenway Health LLC, Carrollton, Georgia), was fully integrated into the health center's CCM. PCPs used computerized order entry to refer patients for consultation with a psychiatrist, LCSW, CHW, health coach, or clinical pharmacist. PHQ-2 and PHQ-9 scores were entered as lab results to facilitate creation of patient registries for depression care management. Care management results were flagged for PCPs for review when an action response was required. MHP evaluations and progress notes are visible to PCPs and vice versa. A security protocol was created for “psychotherapy notes” to satisfy HIPAA (Health Insurance Portability and Accountability Act) regulations for release of medical records to outside entities. As a standard, the vast majority of mental health notes were at the same security level as primary care notes. In some instances, psychotherapy notes may have contained very sensitive information that patients did not want to share with all providers. When this situation occurred, notes were coded at a higher security level.
Data collection
Data were abstracted from the EMR for patients age ≥18 years who had PCP encounters between July 2012 and April 2014. The main outcome variable was PHQ-9 total score for patients with ≥2 encounters with at least 2 PHQ-9 scores documented during the study period. Patients with a baseline PHQ-9 ≥10 were coded as eligible for care management. Patients with a follow-up PHQ-9 score 50% or less than their baseline score were coded as responsive to therapy. Time to treatment response was coded as the number of months to reach a 50% decrease in PHQ-9 scores. Other variables abstracted from the EMR included age, sex, insurance type, diagnosis codes, encounter types (PCP vs. MHP), and process of care variables (presence/absence of documented PHQ-2 and PHQ-9 scores, referrals to and encounters with LCSW/psychiatrists). The QI team's monthly meetings were audio recorded and summarized into meeting minutes.
Data analysis
The research team compared baseline characteristics of patients who only had encounters with their PCP to patients who had additional encounters with MHPs using the Student t test for continuous variables and chi-square analysis for categorical variables. Survival analysis methods that adjust for censored observations were used to estimate the probability of a PHQ-9 score dropping to 50% of a baseline score. Survival times were defined for each patient as time to reach a 50% drop. Here the term survival time is used in the broad sense to mean time until the occurrence of an event. For this study's purpose, the event is reaching a 50% drop in baseline PHQ-9 score. Some patients had not experienced this event by the end of the study period and the last time observed without reaching a 50% drop was recorded for each. In survival analysis methodology, these are referred to as censored observations. Kaplan-Meier product limit estimates were used to estimate cumulative probability curves for both those patients who only saw their PCP and those patients who had additional visits with MHPs. Median time to reaching a 50% drop was reported when available. The log rank test was used to test for significant differences in the 2 cumulative probability curves. Cox proportional hazards regression models were used to adjust for patient characteristics when comparing those patients who only see their PCP and those patients who have additional visits with MHPs. Variables considered were age of the patient at the first visit, sex, race, baseline PHQ-9, insurance type, body mass index ≥25, self-reported tobacco use and diagnosis codes for anxiety (International Classification of Diseases, Ninth Revision: 300.0x, 300.2x, 300.3, 308.3, 309.81), depression (296.xx, 311.xx), diabetes (250.xx, 648.0x, 775.1x), and hypertension (401.xx-405.xx).
QI team meeting minutes were examined to identify facilitators/barriers to protocol adherence. The CCM, as previously described by Wagner et al,11 was used to classify facilitators/barriers within the essential elements of chronic disease management: patient self-management support, delivery system design, decision support, clinical information systems, health care organization support, and linkages to community resources. The Model for Understanding Success in Quality was used to subclassify facilitators/barriers within the context of QI activities.12 This framework identifies contextual factors at multiple levels of health care systems likely to influence the perception of success of QI efforts: external environment, organization, “micro-systems” (clinic/department/office), QI teams, data infrastructure, and resource availability.
Results
Patient characteristics
Table 1 summarizes patient characteristics. A total of 5044 adult patients were seen, 1044 of whom also saw an MHP. Most patients served were middle age, black non-Hispanic women. Compared to patients who only saw their PCP, a significantly higher proportion of patients who saw an MHP had insurance; saw their PCP almost twice as often; were diagnosed with anxiety disorders, depression, and/or active tobacco use; had PHQ-9 scores documented in the EMR; and had appropriate short-term follow-up.
Table 1.
Characteristics of Adult Patients Seen Between July 2012 and April 2014
| All Patients Seen N=5044 | PCP encounters only N=4040 | PCP+mental health encounters N=1004 | |
|---|---|---|---|
| Age (mean, SD) | 47 (14.4) | 47 (14.4) | 48.0 (14.0) |
| Black, non-Hispanic (n, %) | 3564 (70.7) | 2873 (71.1) | 691 (68.8) |
| Female (n, %)* | 3100 (61.5) | 2454 (60.7) | 646 (64.5) |
| Insurance (n, %)* | |||
| Medicaid (Regular/1115 Waiver) | 2231(44.2) | 1718 (42.5) | 513 (51.1) |
| Medicare | 554 (11.0) | 424 (10.5) | 130 (12.9) |
| Commercial | 683 (13.5) | 569 (14.1) | 114 (11.4) |
| Self-Pay | 1576 (31.3) | 1329 (32.9) | 247 (24.6) |
| Clinic encounter types (mean, SD) | |||
| PCP* | 3.1 (2.6) | 2.7 (2.2) | 4.7 (3.6) |
| LCSW (N=319) | 3.9 (6.0) | . | 3.9 (6.0) |
| Psychiatry (N=888) | 3.1 (3.0) | . | 3.1 (3.0) |
| Chronic conditions (n, %) | |||
| Anxiety disorder* | 426 (8.4) | 167 (4.1) | 259 (25.8) |
| Depression* | 781 (15.5) | 330 (8.2) | 451 (44.9) |
| Diabetes | 900 (17.8) | 719 (17.8) | 181 (18.0) |
| Hypertension | 2241 (44.4) | 1786 (44.2) | 455 (45.3) |
| Overweight/Obese | 3880 (76.9) | 3112 (77.0) | 768 (76.5) |
| Tobacco use (Current)* | 1510 (29.9) | 1151 (28.4) | 359 (35.8) |
| PHQ-9 documented at least once* | 787 (15.6) | 271 (6.7) | 516 (51.4) |
| Baseline documented PHQ-9≥10 | N=266 | N=23 | N=243 |
| Time to first follow-up PHQ-9 among patients with baseline score≥10 | |||
| ≤1 month | 104 (39.1) | 5 (21.7) | 99 (40.7) |
| ≤3 months | 191 (71.8) | 14 (60.9) | 177 (72.8) |
P<0.05 comparing the PCP-only group versus the PCP+Mental health provider group.
LCSW, licensed clinical social worker; PCP, primary care physician; PHQ, Patient Health Questionnaire; SD, standard deviation.
Trends in process of care and protocol adherence
Table 2 summarizes trends in screening for symptoms of depression or monitoring response to treatment. The rates of overall depression screening with the PHQ-2 was 54% by the end of the study. The rate of documenting the PHQ-9 fluctuated and ranged from 5% to 16%. Most of these patients scored in the moderate to severe range of symptoms and were seen by an MHP. Referral rates from the PCPs to the MHPs varied (0%–42%).
Table 2.
Trends in PHQ-9 Administration for Assessing Symptoms of Depression or Monitoring Response to Treatment Before and After Implementing PHQ-2 Screening for Primary Care Visits
| Reporting Period (n%) | |||||||
|---|---|---|---|---|---|---|---|
| Before PHQ-2 implemented | After PHQ-2 implemented | ||||||
| Process Measures | Mo. 1–3 N=1606 | Mo. 4–6 N=1666 | Mo. 7–9 N=1802 | Mo. 10–12 N=1760 | Mo. 13–15 N=1740 | Mo. 16–18 N=1835 | Mo. 19–21 N=1631 |
| PHQ-9 for screening/monitoring treatment response | |||||||
| Of total patients seen, how many have a PHQ-9 documented? | 255 (15.8) | 178 (10.7) | 98 (5.4) | 95 (5.4) | 199 (11.4) | 194 (10.6) | 165 (10.1) |
| Of those with a PHQ-9 documented, how many have moderate-to-severe depression symptoms (PHQ-9≥10)? | 203 (79.6) | 127 (71.3) | 65 (66.3) | 69 (72.6) | 141 (70.9) | 130 (67.0) | 117 (70.9) |
| Of those with a PHQ-9≥10, how many were referred to an LCSW/Psychiatrist? | 0 (0) | 20 (15.7) | 16 (24.6) | 29 (42.0) | 47 (33.3) | 26 (20.0) | 29 (24.8) |
| Of those with a PHQ-9≥10, how many have an encounter with an LCSW and/or Psychiatrist? | 120 (59.1) | 81 (63.8) | 56 (86.2) | 48 (69.6) | 95 (66.3) | 100 (77.3) | 71 (61.8) |
LCSW, licensed clinical social worker; Mo, month; PHQ, Patient Health Questionnaire.
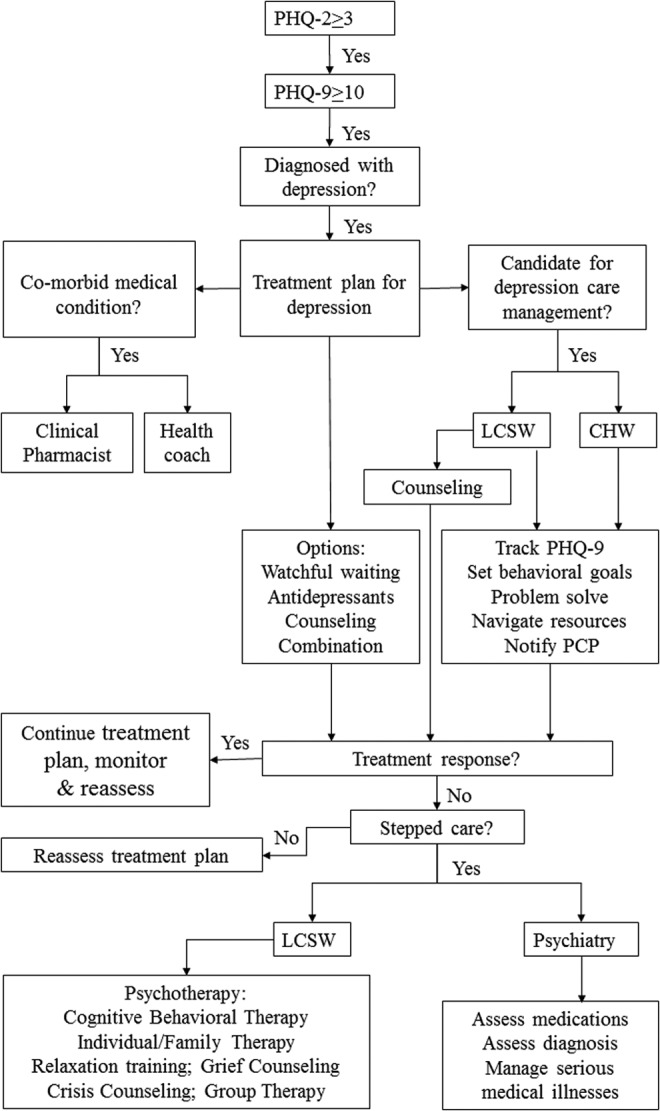
Comparison of cumulative probability of treatment response
A higher proportion of patients who saw an MHP achieved treatment response compared to those who only saw their PCP (36% vs. 13%, P=.03 by chi-square analysis). To describe time to recovery, the plots in Figure 2 show the probability of a patient reaching a 50% drop in baseline PHQ-9 score before time t, where t is study months. The median time to patient recovery for the PCP+MHP group was 14 months whereas the median time to recovery was not observed in the PCP-only group after 18 months. The log rank test, comparing these probability distributions of time to recovery between the 2 groups resulted in no significant difference (P=.16); however, the heavy censoring because of few patients in the PCP group with treatment response (3 out of 23) would be expected to result in low power to detect significant differences. None of the potential predictors of reaching a 50% decrease in PHQ-9 were statistically significant. Adjusting for these factors resulted in 1.7-fold increase in hazard ratio for PCP+MHP visits vs. PCP-only visits; however, this increase also was not statistically significant (P=0.37).
FIG. 2.
Time until PHQ-9 score improves to 50% of baseline. PCP, primary care provider.
Quality improvement context of collaborative depression care
Table 3 describes the center's protocol for collaborative depression care and describes facilitators/barriers to implementing each component. Major facilitators included clinic-level promotion of general wellness, colocation of services, use of a shared EMR, physician champions, and financial incentives for practice change. Noteworthy barriers included limitations in EMR functional capabilities and related workflows that made it difficult to consistently adhere to screening and care management protocols. Although the EMR facilitated generating lists of patients with elevated PHQ-9 scores, the LCSW and CHW were unable to track care management activities for a caseload of patients in a centralized location within the EMR. Although the care manager had access to a Web-based registry tool introduced through the MHIT program, using 2 different systems for tracking and documenting care increased workloads, decreased efficiency, and as expected, decreased adherence to protocol. Staff/provider/management turnover made protocol adherence difficult to maintain. Lack of full-time, on-site psychiatry led to service capacity limitations and extended wait times for evaluations. Mixed messaging about whether or not billing for primary care and mental health on the same day at the same location was permissible led to scheduling practices that were not necessarily convenient or patient-centered. The CHW's essential care coordination activities were not reimbursable under any health plan and were only supported by philanthropic funds.
Table 3.
Quality Improvement Context, Facilitators, and Barriers to Implementing Collaborative Depression Care
| Chronic Care Model Elements | Depression Care Protocol Components | Facilitators | Barriers |
|---|---|---|---|
| Patient self-management support | Colocation of LCSW to provide individual and group psychotherapy; written care plan provided; CHW serving as both care manager and case manager to support setting goals and accountability, facilitating peer support group |
QI culture: The clinic's promotion of general wellness through health education initiatives emphasized equal importance of physical and mental wellness. Resource availability: The clinic had dedicated clinic space for group activities, encouraging peer support. |
QI culture: Restructuring of clinic discharge process under different management eliminated self-management goals from discharge paperwork Resource availability: The CHW/LCSW had limited availability for “warm handoffs” with PCPs. |
| Delivery system redesign | MAs administer depression screen during intake like a vital sign; on-site staff dedicated to scheduling mental health visits | QI culture: Colocation of primary care and mental health decreased stigma of psychiatric diagnoses |
QI culture and motivation: Lack of organizational incentives for MAs to administer depression screening to all patients led to inconsistencies in protocol adherence Data infrastructure: PHQ documentation as a lab result required navigating to a different part of the EMR, adding steps to workflows |
| Clinical information systems | Depression screening questions and scores documented as quantitative lab results; protocol recommends considering care management referral for PHQ-9≥10; mental/behavioral health specialists document consult results and care plan in EMR | Data infrastructure: All providers shared the same EMR and coordinated care plans; lab results, consult orders, and encounter rates were retrievable for performance reports, allowing data-driven modifications to protocol | Data infrastructure: Difficulty in tracking CHW/LCSW caseload without functional EMR-based registry resulted in inefficient workflows for tracking measures and treatment plans and made it difficult to determine in a timely manner when stepped care was indicated; maintaining a registry in a different system increased staff workload and contributed to nonadherence to protocol |
| Provider decision support | Provider education about assessment and treatment of depression and collaborative care model. Psychiatry consultation for medication review, diagnostic clarification of complex cases, management of patients with severe mental illnesses | QI leadership: The lead psychiatrist and medical director championed protocol adherence |
Data infrastructure: Transitioning to a new EMR database under new management led to elimination of site-specific clinical decision-support alerts reminding providers of care plan algorithms Resource availability: There were a limited number of psychiatry sessions (equivalent to 2 days), which increased wait time for new evaluations |
| Community resource linkage | Social services case management assigned to CHW under supervision of LCSW | Resource availability: CHW conducted home visits and on-site peer support groups. |
Data infrastructure: Tracking community referrals within the EMR was difficult Resource availability: There are limited case management resources for uninsured patients |
| Health care organization support | Provider/staff training in collaborative model for depression | Resource availability: Staff turnover among MAs and providers required constant retraining in depression screening, treatment, documentation, and workflow | |
| Federal, state, private sector policies | Grants supported care team expansion for clinics providing care to the underserved | External motivation: Financial incentives from grants supported medical home transformation; LCSW billing under FQHC model enhanced revenue; requirement for depression screening by select health plans and funding agencies motivated top management to enforce depression screening | External motivation: Low reimbursement rates and limitations on billing for primary care and mental health on the same day were deterrents to providing care; CHW care coordination and case management activities were not reimbursed despite their importance to treatment plans, providing little incentive on the organizational level to support the full collaborative care model. |
CHW, community health worker; EMR, electronic medical record; FQHC, Federally Qualified Health Center; LCSW, licensed clinical social worker; MA, medical assistant; PCP, primary care physician; PHQ, Patient Health Questionnaire; QI, quality improvement.
Discussion
This article describes a 6-year practice transformation process for integrating primary care and mental/behavioral health services in a safety net medical home. The medical home model employed in this study includes a multidisciplinary care team (PCPs, psychiatrists, LCSW, mental health CHW, health coach, clinical pharmacist) colocated in the same facility to provide a comprehensive, holistic approach to patient care. The practice design addresses the need to manage comorbid physical and mental health conditions. Mental/behavioral health providers were colocated with PCPs to have a greater reach in the community to address unmet mental health needs, to decrease the stigma of mental health conditions, and to convey the equal importance of and connection between physical and mental wellness. The research team also aimed to minimize logistical challenges of coordinating high-quality mental health care.
This study's findings are consistent with results from a larger study that demonstrated that community-based organizations that successfully implement collaborative care can achieve meaningful improvements in process and outcomes of care.7 Practice transformation was facilitated by disaster recovery activities that included training programs to promote implementation of CCMs as well as community-wide demonstration projects to support capacity building and to finance care coordination for an underserved population. The need for integrated services and proactive screening of patients for depression was clearly substantiated by the prevalence of moderate-to-severe depression symptoms and mental health disorders diagnosed. Most patients with at least moderate depressive symptoms had referrals ordered or they sought behavioral health services. Patients who experienced mental health collaborative care saw their PCP twice as often, had timelier follow-up for monitoring symptoms of depression, and had documented treatment response.
The facilitators/barriers to practice integration of primary care and mental/behavioral health services were related to clinic QI leadership and culture, availability of resources within the organization and in the surrounding community, organization-level data infrastructure, and external motivators of or deterrents to care integration. Although having on-site program champions was important, sustainability of programming was threatened once these champions left the organization. Engraining aspects of collaborative care into the organizational culture through job descriptions, operational policy and procedures, and ongoing staff training was imperative. As described in a previous study,13 using both an EMR for routine care documentation and an external care management registry tool was not sustainable. The registry tool could not be customized to meet the research team's needs. However, not using a registry led to missed opportunities to proactively identify patients who may need stepped care, which in turn may have prolonged time to improvement of symptoms. Disparate reimbursement practices have previously been identified as major barriers to integrated service delivery.6,14 Although the research team successfully built capacity for integrated care using funding from demonstration grants, programming sustainability relied heavily on funding from the Medicaid Waiver and transitioning the clinic under an FQHC. Behavioral health billing for the LCSW under the FQHC model enhanced revenues, making it possible to finance this position independent of grants. Sustainable funding for care management services provided by non-licensed personnel (eg, CHW) who might increase a practice's capacity for providing such services is still lacking under current models of reimbursement.
This study has several limitations. This study reflects the experience of only 1 organization and has limited external generalizability. Patients were not randomized into study groups; instead, patients were referred to MHPs at their PCP's discretion. Consequently, there may be unmeasured confounders that explain group differences (albeit not statistically significant) in patients achieving 50% reduction in PHQ-9 scores. As a retrospective study, data interpretation is limited by missing or incomplete data. PHQ-9s could have been recorded within the text of provider notes instead of entered as structured data. Therefore, the trends reported for protocol adherence may be inaccurate. The research team could not definitively determine all indications for referring (or not referring) patients with elevated PHQ-9 scores to MHPs. For example, patients could have had elevated scores but, at the discretion of their PCPs, were not formally diagnosed with depression. Patients' symptoms may have been attributed to other mental health diagnoses or causes not readily captured by visit diagnosis codes. Patients also could have already been established with other MHPs outside of the study institution. Finally, the research team did not have consistent access to information on urgent care use, emergency department visits, or inpatient hospitalizations (eg, claims data, notices via health information exchanges) and therefore cannot determine whether the programming generated cost savings for the population served.
Notwithstanding these limitations, this study's purpose was to describe the implementation process for integrating primary care and mental/behavioral health services in a safety net medical home, the QI context, and program outcomes. The research team was able to create a well-functioning, colocated collaborative team under restricted resources. Organizations striving to implement collaborative care should focus their program design on addressing operational successes and challenges related to organization and clinic culture, QI leadership, staffing, health information technology, and financing. Sustainability of such programming will depend on health policy makers eliminating roadblocks to practice redesign through innovative reimbursement strategies that place value on population health management, care management, and care coordination.
Author Disclosure Statement
Drs. Price-Haywood, Dunn-Lombard, and Lefante and Ms. Harden-Barrios declared no conflicts of interest with respect to the research, authorship, and/or publication of this article. At the time this study was conducted, Dr. Price-Haywood was the Chief Medical Officer for Tulane University's Office of Community Affairs and Health Policy and Medical Director of the Tulane University Community Health Center. Dr. Donisha Dunn-Lombard was Director of Mental Health Services at Tulane University Community Health Center.
The authors received the following financial support for the research, authorship, and/or publication of this article: This study was supported by the New Orleans Charitable Health Fund (administered by the Louisiana Public Health Institute) and in part by 1 U54 GM104940 from the National Institute of General Medical Sciences of the National Institutes of Health, which funds the Louisiana Clinical and Translational Science Center. The ideas expressed in this manuscript are the sole responsibility of the authors and do not necessarily represent the official views of the Louisiana Public Health Institute or the National Institutes of Health.
Acknowledgment
The authors would like to thank Access Health Louisiana Federally Qualified Health Center Network for their collaboration on this project.
References
- 1.Thota AB, Sipe TA, Byard GJ, et al. . Collaborative care to improve the management of depressive disorders: a community guide systematic review and meta-analysis. Am J Prev Med. 2012;42:525–538 [DOI] [PubMed] [Google Scholar]
- 2.Woltmann E, Grogan-Kaylor A, Perron B, Georges H, Kilbourne AM, Bauer MS. Comparative effectiveness of collaborative chronic care models for mental health conditions across primary, specialty, and behavioral health care settings: systematic review and meta-analysis. Am J Psychiatry. 2012;169:790–804 [DOI] [PubMed] [Google Scholar]
- 3.Community Preventive Services Task Force. Recommendation from the community preventive services task force for use of collaborative care for the management of depressive disorders. Am J Prev Med. 2012;42:521–52422516494 [Google Scholar]
- 4.Unützer J, Park M. Strategies to improve the management of depression in primary care. Prim Care. 2012;39:415–431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jacob V, Chattopadhyay SK, Sipe TA, Thota AB, Byard GJ, Chapman DP; Community Preventive Services Task Force. Economics of collaborative care for management of depressive disorders: a community guide systematic review. Am J Prev Med. 2012;42:539–549 [DOI] [PubMed] [Google Scholar]
- 6.Kathol RG, Butler M, McAlpine DD, Kane RL. Barriers to physical and mental condition integrated service delivery. Psychosom Med. 2010;72:511–518 [DOI] [PubMed] [Google Scholar]
- 7.Bauer AM, Azzone V, Goldman HH, et al. . Implementation of collaborative depression management at community-based primary care clinics: an evaluation. Psychiatr Serv. 2011;62:1047–1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Springgate BF, Wennerstrom A, Meyers D, et al. . Building community resilience through mental health infrastructure and training in post-Katrina New Orleans. Ethn Dis. 2011;21(3 suppl 1):S1–20-9 [PMC free article] [PubMed] [Google Scholar]
- 9.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284–1292 [DOI] [PubMed] [Google Scholar]
- 11.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779 [DOI] [PubMed] [Google Scholar]
- 12.Kaplan HC, Froehle CM, Cassedy A, Provost LP, Margolis PA. An exploratory analysis of the model for understanding success in quality. Health Care Manage Rev. 2013;38:325–338 [DOI] [PubMed] [Google Scholar]
- 13.Bentham W, Vannoy SD, Badger K, Wennerstrom A, Springgate BF. Opportunities and challenges of implementing collaborative mental health care in post-Katrina New Orleans. Ethn Dis. 2011;21(3 suppl 1):S1-30–7 [PMC free article] [PubMed] [Google Scholar]
- 14.O'Donnell AN, Williams M, Kilbourne AM. Overcoming roadblocks: current and emerging reimbursement strategies for integrated mental health services in primary care. J Gen Intern Med. 2013;28:1667–1672 [DOI] [PMC free article] [PubMed] [Google Scholar]