Abstract
Objectives
To describe both conditions of a two-group randomized trial, one that promotes physical activity and one that promotes cancer screening, among churchgoing Latinas. The trial involves promotoras (community health workers) targeting multiple levels of the Ecological Model. This trial builds on formative and pilot research findings.
Design
Sixteen churches were randomly assigned to either the physical activity intervention or cancer screening comparison condition (approximately 27 women per church). In both conditions, promotoras from each church intervened at the individual- (e.g., beliefs), interpersonal- (e.g., social support), and environmental- (e.g., park features and access to health care) levels to affect change on target behaviors.
Measurements
The study’s primary outcome is min/wk of moderate-to-vigorous physical activity (MVPA) at baseline and 12 and 24 months following implementation of intervention activities. We enrolled 436 Latinas (aged 18–65 years) who engaged in less than 250 min/wk of MVPA at baseline as assessed by accelerometer, attended church at least four times per month, lived near their church, and did not have a health condition that could prevent them from participating in physical activity. Participants were asked to complete measures assessing physical activity and cancer screening as well as their correlates at 12- and 24-months.
Summary
Findings from the current study will address gaps in research by showing the long term effectiveness of multi-level faith-based interventions promoting physical activity and cancer screening among Latino communities.
Keywords: Faith-based intervention, Health promotion, Minority health, Physical activity, Cancer screening, Hispanics/Latinos
Many chronic diseases impact Latinas at disproportionate rates. Latinos have a higher prevalence of diabetes and obesity than non-Hispanic whites, which puts Latinos at greater risk for developing other health conditions (e.g., cardiovascular health problems and depression). Latina women are twice as likely to be diagnosed with cervical cancer, and 1.5 times more likely to die from cervical cancer compared to non-Hispanic white women. The low engagement in moderate-to-vigorous leisure-time physical activity (MVPA) [1] and screening rates for many cancers like cervical and colorectal [2] contributes to high disease rates and mortality in Latinas. The large size and rapid growth of the Latino population is a compelling rationale to focus on chronic disease prevention, as Latinos will account for most of the U.S. population growth through 2050 [3].
Emerging research suggests that disparities in health behaviors and outcomes are the result of a range of proximal, intermediate, and distal determinants [4]. Proximal determinants involve biologic factors, behaviors, and psychological factors such as mental health status and cognitions. Intermediate determinants consist of social norms and social support, while distal determinants include the social and physical or built environment (e.g., density of grocery stores or parks in a neighborhood). A key tenet of ecological models is that interventions that target multiple levels of influence (e.g., individual, social, and environmental) should be more effective in changing behavior than those that target only one level [4]. There have been a limited number of multi-level interventions focusing on the promotion of physical activity among adults [5–7] and, to our knowledge, only one study used a randomized controlled design [6]. When considering interventions for cancer prevention, a fewer programs have used the ecological approach to inform program development. The relative popularity of multi-level interventions recognizes the importance of creating socially and physically supportive environments to achieve sustained behavior change.
Numerous health promotion researchers [8–13] and national surveys suggest that churches are ideal settings for Latino-focused health promotion programs because they can have substantial reach into Latino communities. Sixty-eight percent of Latinos identify as Catholic (15% Evangelical Protestant), and close to 42% of Latino Catholics indicate attending church at least weekly [14]. Churches are attractive settings for promoting health because they have infrastructural resources (e.g., meeting spaces) and a system of volunteers that can provide social support for adopting and maintaining new health behavior changes [15]. Health promotion programs that partner closely with churches and increase the capacity of church members to provide mutual support are likely to be sustainable after the research is completed. A systematic literature review of faith-based physical activity interventions underscored the need for implementing faith-based multi-level physical activity programs [16]. This review found that the majority of church-based physical activity interventions increased physical activity. However, almost all of the studies were limited because they assessed physical activity by self-report, were short in duration (intervention of 12 weeks or less), and targeted primarily African American women.
This manuscript describes a two-group randomized controlled trial to assess the effectiveness of a physical activity intervention targeting multiple levels of influence for behaviors among Latinas, Fe en Acción (Faith in Action). Sixteen churches were recruited and randomly assigned to either the physical activity intervention or cancer screening comparison condition. Trained bilingual/bicultural (Spanish/English and Mexican-origin) promotoras (community health workers) intervened at the individual (e.g., motivational interviewing), social (e.g., informational support), and environmental (e.g., park features and access to health care) levels. Evaluation protocols assessed changes at these levels, including implementation fidelity. The physical activity intervention is innovative in its focus on promoting physical activity in Latino faith-based organizations and its modification of the built environment (e.g., increasing access to safe parks and neighborhoods) [12,17–19]. Churches provide valuable settings in which to promote chronic disease prevention, as they are established institutions that mobilize Latino communities [16,12, 18]. Undertaking two interventions simultaneously recognizes the multiple health needs in this community, provides useful services to all participants, and is an efficient method of evaluating multiple interventions.
1. Methods
1.1. Overview of study design and research aims
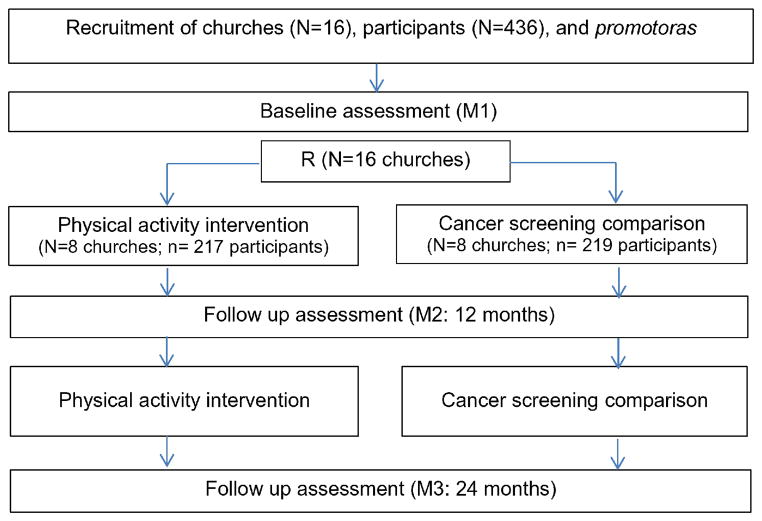
This two-group randomized controlled trial combines innovative and traditional methods for promoting MVPA and cancer screening (breast, cervical, colorectal, and skin) among Latinas, and is tested simultaneously in a two-group design. Both interventions lasted two years. The study’s primary outcome was min/week of accelerometer-assessed MVPA at baseline (M1) and 12 months (M2) and 24 months (M3) following the start of the intervention. We selected cancer screening as a comparison condition given the relevance of this topic to our target community (i.e., low cervical and colorectal cancer screening rates and follow-up). It was hypothesized that over time, participants in the physical activity condition would engage in significantly higher levels of MVPA, compared to participants in the cancer screening condition. We also expected greater changes in individual-, interpersonal-, and environmental-level correlates of physical activity among participants in the physical activity condition compared to those in the cancer screening condition. Conversely, we expected that participants in the cancer screening condition would engage in higher screening rates compared to those in the physical activity intervention. We anticipated greater changes in individual, interpersonal, and environmental correlates of cancer screening in this condition compared to the physical activity condition (Fig. 1).
Fig. 1.
Study design.
While recruitment, randomization, promotora training, and baseline and 12-month follow-up assessments are all completed, the intervention and final measures remain active through the end of 2015. All study protocols were approved by the Institutional Review Board of San Diego State University. The current trial is registered under NCT01776632.
1.2. Recruitment and eligibility criteria
1.2.1. Recruitment of churches
The Principal Investigator and Project Coordinator discussed the study with the Chancellor of the Roman Catholic Diocese of San Diego, who provided a list of 53 churches offering services in Spanish. A staggered recruitment strategy was used and began for the first wave in January 2011 and was completed for the final wave in March 2013. Project staff approached churches with a minimum of 200 Latino families and at least one Spanish-language mass. Inclusion criteria included agreeing to be randomly assigned to either condition (physical activity or cancer screening) and commitment of space for program activities and participant measurements. The original goal was to only include churches that were at least 3 miles apart. As recruitment progressed it was necessary to include a few churches that were about 1 mile apart. However, the participant criterion that they attend only their nearby church reduced concerns about potential contamination. During enrollment, the pastor from each participating church signed a memorandum of understanding that outlined the pastor’s commitment of space for measurement and intervention activities, announcements at mass and other meetings, promotion of the project on church grounds, and assistance in identifying potential candidates for the promotora roles. The study recruited 16 Catholic churches in San Diego County and 436 Latinas who attended these churches, an average of 27 participants per church.
1.2.2. Recruitment of participants
Participant recruitment for the first wave began in April 2011 and continued through August 2013 for the final wave of churches. Participants were blinded to condition during recruitment. Women were recruited via fliers, word of mouth, printed announcements in church bulletins, and verbal announcements during Spanish-language masses and other ministry group meetings targeting Latinas (e.g., Bible study, choir, and marriage classes). Recruitment efforts were conducted in Spanish or English. Inclusion criteria were women who self-identified as Latina, were between the ages of 18 and 65, attended the church at least four times a month for any reason, lived within 15 minutes driving distance from the church, had access to reliable transportation to get to the church, identified no barriers to attend activities at the church during the week, planned on attending the church for the next 24 months, did not attend other churches enrolled in the study, and had relatively low levels of physical activity (details described below). Recruitment was limited to those living near and attending only a participating church to enhance exposure to both the classes and the local environmental change components of the intervention. Churchgoers and community members not enrolled in the study could participate in intervention activities as all activities were offered free at the church or local parks and community centers.
Potential participants were excluded if they had a health condition that limited their ability to be physically active (e.g., being pregnant or having a disability). Women were screened and completed the Physical Activity Readiness Questionnaire (PAR-Q) to assess risks for complications resulting from physical activity [20]. The PAR-Q assesses potential heart problems, joint or bone problems, pregnancy, diabetes, and current medication use. Individuals who reported one or more positive responses to the PAR-Q were required to have their physician approve their participation in the program by completing the PARmedX. Table 1 provides the sociodemographic characteristics of our sample.
Table 1.
Descriptive characteristics of Latina participants at baseline, overall and stratified by condition. Fe en Acción, San Diego, CA (2011–2013).
| Overall (N = 436)
|
Physical activity (n = 217)
|
Attention-control (n = 219)
|
|
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Demographics | |||
| Born in Mexico | 394 (90.8)a | 193 (88.9)b | 201 (92.6)c |
| Married/living as married | 334 (77.3) | 168 (78.1) | 166 (76.5) |
| Employedd | 285 (65.8) | 147 (68.7) | 138 (63.0) |
| Monthly household income <$2000 | 236 (58.3)e | 115 (56.1)f | 121 (60.5)g |
| <High school completed | 238 (54.8) | 116 (53.7) | 122 (56.0) |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Mean age (years) | 44.4 (9.6) | 44.5 (9.8) | 44.4 (9.4) |
| Residence in the US (years) | 21.0 (10.3) | 22.1 (11.2) | 19.8 (9.2) |
| Accelerometer-assessed PA | |||
| MVPA (min/week)h | 103.2 (63.8) | 98.8 (61.5) | 107.6 (65.8) |
| Moderate PA (min/week) | 102.2 (62.9) | 98.1 (61.0) | 106.2 (64.7) |
| Vigorous PA (min/week) | 1.1 (5.0) | 0.7 (3.6) | 1.4 (6.1) |
| Light PA (min/week) | 2305.9 (587.5) | 2308.2 (570.9) | 2303.7 (604.8) |
| Sedentary time (min/week) | 7558.0 (644.8) | 7550.4 (611.5) | 7565.7 (677.5) |
| % Sedentary timei | 75.8 (6.1) | 75.8 (5.9) | 75.8 (6.3) |
| Reported PA | |||
| Leisure vigorous PA (min/week) | 17.5 (58.3) | 19.7 (62.5) | 15.2 (53.8) |
| Leisure moderate PA (min/week) | 50.1 (88.9) | 51.4 (97.3) | 48.8 (79.9) |
| Leisure MVPA (min/week) | 67.6 (112.8) | 71.2 (121.1) | 64.0 (104.1) |
| Occupational MVPA (min/week) | 481.7 (886.9) | 493.5 (798.7) | 469.9 (968.1) |
| Total transport PA (min/week) | 57.9 (160.2) | 66.1 (198.3) | 49.7 (109.6) |
| Household light PA (min/week) | 1236.7 (870.8) | 1171.4 (816.8) | 1301.4 (918.5) |
| Household MVPA (min/week) | 431.8 (473.7) | 399.3 (451.6) | 463.9 (493.5) |
| Total household LMVPA (min/week) | 1668.5 (1104.1) | 1570.7 (1005.0) | 1765.3 (1188.7) |
| Total sedentary time (min/day) | 240.2 (159.2) | 246.5 (165.0) | 233.9 (153.3) |
| Anthropometrics | |||
| Height (cm) | 155.3 (6.1) | 155.6 (6.4) | 155.0 (5.9) |
| Weight (kg) | 73.2 (16.3) | 74.6 (16.9) | 71.9 (15.5) |
| Waist circumference (cm) | 94.9 (14.7) | 95.8 (15.0) | 94.1 (14.3) |
| Body mass index (kg/m2) | 30.3 (6.2) | 30.8 (6.6) | 29.9 (5.8) |
LMVPA = light, moderate, and vigorous physical activity; MVPA = moderate-to-vigorous physical activity; PA = physical activity; SD = standard deviation.
Remainder include those born in the US (n = 33) or another foreign country (n = 7). Missing n = 2.
Remainder include those born in the US (n = 20) or another foreign country (n = 4).
Remainder include those born in the US (n = 13) or another foreign country (n = 3). Missing n = 2.
Includes full-time, part-time, self-employed, and seasonal work.
Missing n = 31.
Missing n = 12.
Missing n = 19.
Primary aim.
Out of total wear time.
1.3. Screening for women who are least active
1.3.1. Self-report screener
We used a two-stage screening process. The first stage involved the administration of two self-report screeners that classified individuals as active or low-active. Trained research assistants screened women for their physical activity using two screeners: the Stanford Brief Activity Survey (SBAS) [21] and a 3-question assessment [22]. The SBAS involved 2 items assessing on-the-job and leisure-time activity [21]. Each item had 5 response choices, and respondents selected the option that best described their activity during work and leisure time (frequency, intensity, time, and type of activity). Each response option was graded as inactive, light, moderate (3.0–4.9 METs), hard (5.0–6.9 METs), and very hard (≥7.0 METs) [23]. The screeners’ scoring table was used to combine the responses from the 2 items and determine the respondents’ current activity level [21]. Women were eligible if they met the SBAS criteria for ‘inactive’ or ‘light-intensity activity’ as determined by the screener’s scoring table.
The 3-question assessment assessed frequency of engaging in at least 20 min/week of vigorous leisure-time physical activity, at least 30 min/week of moderate leisure-time physical activity, and at least 30 min/week of walking (for leisure or transportation) [22]. The response options for the item on vigorous physical activity ranged from 0 (none) to 2 (3 or more times/week; equivalent to 60 min/week); for moderate physical activity, response options ranged from 0 (none) to 3 (5 or more times/week; equivalent to 150 min/week); and for walking, response options ranged from 0 (none) to 3 (5 or more times/week; equivalent to 150 min/week). Women were eligible if they reported insufficient physical activity as defined as engaging in less than 60 min/week of vigorous physical activity, or less than 150 min/week of walking and moderate physical activity combined, or less than 150 min/week of the combination of reported vigorous and moderate physical activity and walking. Those who were classified as “low-active” by both screeners were invited to participate in the second stage of the screening criteria which involved wearing an accelerometer for 7 days.
Those who met accelerometer wear time criteria (i.e., a minimum of 5 valid days, including at least 3 weekdays and 1 weekend day, with at least 10 valid hours/day) and engaged in less than 250 minutes/week of MVPA as assessed by the accelerometer were eligible to participate. While the Centers for Disease Control and Prevention recommend that adults engage in at least 150 minutes/week of aerobic moderate-intensity physical activity or 75 minutes/week of vigorous-intensity activity or a combination of both, early in recruitment it became evident that over 50% of Latinas exceeded 150 min/week of accelerometer-assessed MVPA [24]. Due to the high percentage of Latinas engaging in at least 150 min/week of MVPA, likely due to more activity in the transportation (i.e., walking to/from places), work-related and household domains, the accelerometer-based MVPA threshold for inclusion was modified to include those who engaged in less than 250 min/week of accelerometer-assessed MVPA. Another consideration was that the 150 min/week guideline is based mainly on self-reports of leisure physical activity and because accelerometers pick up all domains of physical activity, there is not a good match between guidelines and accelerometer data.
1.4. Intervention description
1.4.1. Recruitment and selection of promotoras in both conditions
Two to three promotoras were recruited from each church based on their experience promoting health, bilingual fluency (English/Spanish), and commitment to teaching others to engage in the targeted preventive behaviors. Candidates were identified by pastors and church leaders of enrolled churches, who provided names of individuals who might be interested in becoming a paid promotora. Recruitment flyers were also posted throughout the church. Candidate promotoras completed an application asking about their access to transportation, their availability during the week, ability to work in the US, involvement in the church and community, and health practices (e.g., healthy eating and physical activity). The Intervention Coordinator screened applicants by phone to assess eligibility. Eligible candidates were interviewed in person at the church and assessed for their ability to lead groups, commitment to the two-year project, knowledge of the church and community, and leadership skills. Promising candidates for the physical activity condition had experience attending group exercise classes and were involved in their church. For the cancer screening condition, promising candidates had experience teaching small groups, were involved in their church communities, and preferably had a background in health education, nursing, or other healthcare field. Selected promotoras were hired at $10 per hour and worked between 5 and 10 hours per week.
1.4.2. Training of promotoras in the physical activity condition
Promotoras in the physical activity condition received 6 weeks of training, totaling more than 24 hours of small group training. All promotoras were required to complete the training and were compensated for their time at $10 per hour. The Intervention Coordinator and a Physical Activity Specialist led the training, which consisted of twice weekly meetings for 6 weeks conducted in Spanish. Behavioral scientists, an exercise physiologist, specialists in exercise, physical activity and kinesiology, and graduate students helped develop the curriculum (Table 2). The training was culturally tailored for a Latino (largely Mexican-origin) audience using methods similar to Resnicow’s surface and deep levels [25]. Examples of cultural tailoring included images of Latina women in the training manual, foods common in Latino diets, music selections for cardio dance, the use of Catholic prayer cards, and conducting all training sessions in Spanish. Prior to implementation, sessions were pilot-tested with Catholic Latina women who provided feedback not only on session content, but also on the faith components, and cultural relevance. Images, training activities, and language were adjusted based on this formative research. Using recommendations from the Aerobics and Fitness Association of America (www.afaa.com) and the American Council on Exercise (www.acefitness.org), both national fitness instructor training programs, the curriculum focused on safe exercises for people who had been largely inactive during leisure time. The faith-based components of the curriculum were developed by the Intervention Coordinator, who had experience working in Latino churches and knowledge of Catholic faith traditions. Bible verses encouraging health, leadership, teamwork, and service to others were included in the sessions. Training sessions began with group prayer and Bible verses focusing on physical health, serving others, and leadership. During training, promotoras were assigned homework exercises, including designing strength training classes, developing cardio dance choreography, and practicing stretching exercises. The promotoras’ final training session focused on Motivational Interviewing, giving them the tools to use a modified version of a script developed by Resnicow [26,27]. Finally, all physical activity promotoras were certified in CPR and First Aid. Following completion of training, promotoras demonstrated a 30-minute class to the Intervention Coordinator and Physical Activity Specialist that included a 10-minute warm-up, 10 minutes of cardio dance or strength training exercises, and a 10-minute cool-down. Those who reached a level of competence adequate to begin teaching classes received a certificate of completion, a project pin, two project exercise shirts to wear while teaching, an exercise mat, towel, water bottle, backpack, sun visor, and class instructional materials.
Table 2.
Promotora training curriculum.
| Level | Physical activity | Cancer screening |
|---|---|---|
| Individual | Importance of physical activity; warm-up and class instruction; cool-down and Injury prevention; walking groups; strategies for healthy eating; cardio dance 1; cardio dance II; strength training I; strength training II; maintaining a healthy weight | The importance of prevention; breast cancer I; breast cancer II; cervical cancer I; cervical cancer II; colorectal cancer I; colorectal cancer II; skin cancer |
| Interpersonal | How to enhance group cohesion; increase group participation; implement Motivational Interviewing | How to enhance group cohesion; increase group participation; implement Motivational Interviewing |
| Environmental | What is advocacy; conducting a walk audit; identifying priorities for change; understanding local government; how to write an action plan; advocacy tools and tips | Accessing health care services; patient rights and responsibilities |
Six months after the start of intervention activities, Circulate San Diego (www.circulatesd.org), a local non-profit organization that advocates for healthy built environments, conducted a 2-day, 8-hour training with promotoras on the impact of the built environment on physical activity and on advocacy and community organizing. Promotoras were trained to identify built environmental targets of change using walk audits and develop solutions to improve the church and surrounding neighborhood for walking and other forms of physical activity. These targets included the removal of pedestrian barriers, aesthetic improvements, and other environmental changes. Circulate San Diego’s promotora training was enhanced with hands-on experiences and skill-building opportunities. During and following the environmental training, promotoras were encouraged to attend and participate in community meetings, legislative meetings, and parish council meetings to learn about community resources, organize community action, and facilitate built environmental changes.
1.4.3. Training of promotoras in the cancer screening condition
Promotoras in the cancer screening condition received 6 weeks of training, totaling more than 24 hours. The training was required and promotoras received $10 per hour for attending training sessions and completing assignments. The Intervention Coordinator led the training, which consisted of twice weekly meetings conducted in Spanish (see Table 2). Project staff (including behavioral scientists and graduate students) developed the curriculum with input from representatives from the American Cancer Society and the University of California, San Diego (UCSD) Moores Cancer Center. Training sessions began with a prayer and Bible verses for reflection, a group icebreaker activity, a review of learning objectives and key terms, and session materials. Promotoras were assigned homework to enhance their learning, increase their knowledge of cancer screening services in their communities, review current cancer screening recommendations, and develop skills as health educators. Throughout the training, promotoras prepared short presentations of learned session information to present to the group for feedback (e.g., risk factors for cervical cancer). Promotoras received feedback on content presentation, public speaking skills, and use of interactive activities to explain concepts. Those who completed the promotora training received a certificate of completion, project pin, project polo shirt, and class instructional materials. Promotoras were provided with Spanish-language health education handouts to use in their workshops from the local chapter of the American Cancer Society or created by project staff. In addition, promotoras attended workshops about the Affordable Care Act aimed to help inform the Latino community about the new healthcare law to help study participants access needed healthcare resources.
1.4.4. Fe en Acción physical activity intervention components
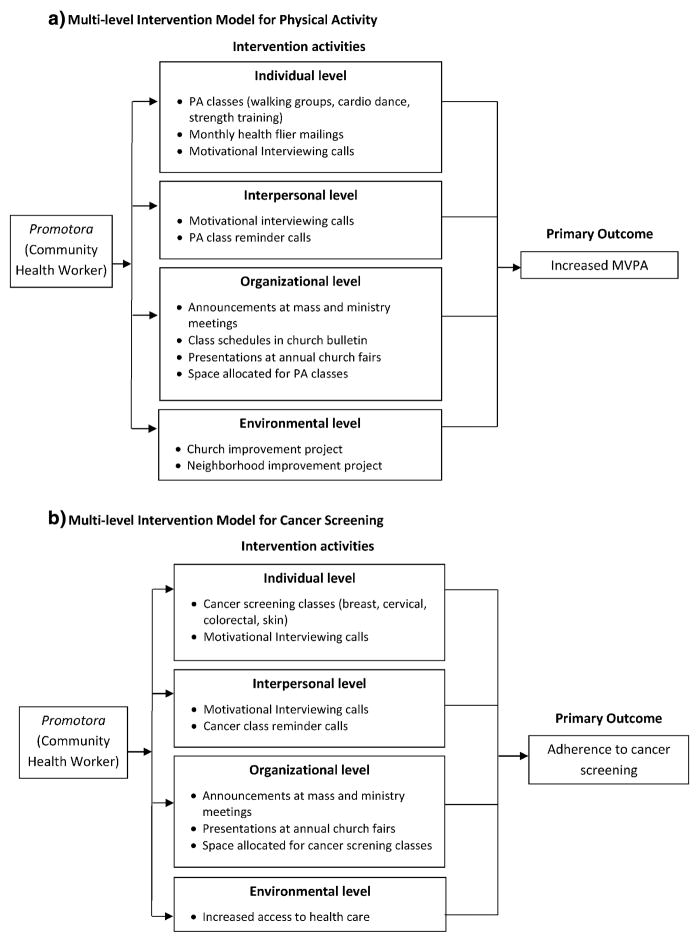
The study methods and intervention were informed by a pilot study in San Diego, CA that assessed the short-term efficacy of a church-based multi-level intervention promoting physical activity among Latinas [28]. The study involved 97 churchgoing Latinas, and physical activity was assessed via accelerometer. Because the current study included components (cancer screening and group fitness training) that were not included in the pilot study, we conducted further formative research including input of churchgoing Latinas before implementing the program. Churchgoing Latinas from a church not enrolled in the main study were invited to participate in trial sessions of the proposed promotora training and provided feedback on three physical activity sessions. They were recruited through relationships developed during the pilot study. This feedback was essential in the development of the final version of the promotora training curriculum, the participant materials (e.g., monthly handouts), and the church materials (See Fig 2 for intervention components).
Fig. 2.
(a). Multi-level intervention model for physical activity. (b). Multi-level intervention model for cancer screening.
1.4.5. Individual level
The intervention offered three types of free physical activity activities at or near the church site: 2 walking groups, 2 cardio dance classes, and 2 strength training classes each week. Within each church, the variety of classes offered served to reach individuals with various fitness levels and different activity preferences. In each church, six classes were offered weekly at different days and times to accommodate various schedules. The exercise classes were structured such that the first 10 minutes consisted of warm-up followed by 30–40 minutes of MVPA, and concluded with a 10-minute cool-down. The classes began with a scripted introduction, where the promotora introduced herself, provided a brief description of the class, discussed safety precautions, identified new attendees, and confirmed that all participants signed in and completed the liability waiver. Before starting the warm-up, promotoras led the group in prayer or elicited volunteers from their classes to lead an opening prayer. At the end of class, promotoras reviewed one of the monthly health handouts (handed out in person as well) with participants and engaged the group in a 5-minute interactive discussion.
Over 24 months, project staff mailed participants in the physical activity intervention monthly evidence-based educational handouts addressing the following 14 topics: benefits of physical activity, setting healthy goals, physical activity guidelines, overcoming barriers to physical activity, myths about physical activity, proper hydration, healthy eating, physical activity resources for families, promoting physical activity in your neighborhood, making time for physical activity, portion control, ways to burn more calories, injury prevention, and the benefits of strength training. The handouts were developed by the Intervention Coordinator and topics came from the following sources: Centers for Disease Control and Prevention’s Division of Nutrition, Physical Activity and Obesity; US Department of Agriculture’s MyPlate; and Centers for Disease Control and Prevention’s Physical Activity Resources for Health Professionals. Included in the mailing was a current physical activity class schedule for the participant’s church site.
1.4.5.1. Participant engagement in physical activity classes
We used two incentive programs to motivate attendance to exercise classes. The first was a monthly raffle based on class attendance that was open to all who attended physical activity classes, not limited to study participants. The second was a point system rewarding study participants for class attendance during the first 3 months of intervention. Raffle and point system prizes included project shirts, towels, water bottles, visors, backpacks, and exercise mats. The study also encouraged attendance at physical activity classes through a Noche Familiar (Family Night) event held at churches in the physical activity condition as a “kick-off” event at the start of intervention activities. Study participants and their families were invited to attend the evening event that included a healthy dinner, presentations by experts in nutrition and mental health, and an introduction to the promotoras, who promoted their physical activity classes. The purpose of these events was to present the program to participants in an inviting way without the pressure of having to immediately engage in physical activity. Some participants could have been hesitant to engage in physical activity and this event provided them with an introduction to other participants and program staff. The inclusion of spouses and children was intended to elicit greater social support for behavioral changes.
1.5. Interpersonal level
To target interpersonal factors, promotoras conducted Motivational Interviewing (MI) calls to address barriers to physical activity and reinforce efforts to engage in physical activity. MI is a counseling approach that allows individuals to develop their own arguments for change, does not prematurely push an individual to change, and encourages participants to find meaning in their decisions [29]. Although these components may be considered individual level factors, we included MI in the interpersonal level because the promotoras supported the individual change. Thus, MI could target factors at the individual level as well as the interpesonal level. We modeled the MI approach after Resnicow’s MI [26]. During the MI phone calls, promotoras asked participants about their physical activity frequency, duration, barriers, and solutions to increasing activity or intensity, benefits of increasing physical activity, and to articulate the link between their values and benefits of engaging in physical activity. Each MI call lasted approximately 30 minutes, and participants received MI calls every 3 to 4 months over the two-year intervention, for a total of five calls. The Intervention Coordinator trained the promotoras on how to address factors like time management, setting realistic physical activity goals, eliciting support from family and friends to engage in physical activity, and monitoring physical activity. Based on participants’ responses, the promotoras were able to help each participant set realistic physical activity goals.
1.5.1. Organizational level
At the organizational level, churches provided physical space for cardio dance and strength training classes. In addition, physical activity class schedules were printed in the church bulletins, and churches allowed promotoras to hang promotional banners and posters advertising the classes. Churches provided time at the end of mass for the promotoras or the priests themselves to remind church members of the physical activity classes and encourage them to attend. Finally, churches provided booths at ministry fairs and annual church fairs for promotoras to promote the physical activity classes.
1.5.2. Environmental level
Circulate San Diego trained the promotoras on how to conduct walk audits to evaluate the quality of the church grounds and surrounding neighborhood, with a primary focus on pedestrian environmental features (e.g., sidewalks, trees, and lighting). Promotoras in the physical activity intervention completed a walkability audit around their church to highlight areas of improvement including aesthetics (e.g., trash and/or overgrown plants on sidewalks, high speed traffic, unguarded dogs, and odors) and physical structures (e.g., missing or broken sidewalks and lack of planting strips and street trees). Training the promotoras to address the built environment and physical activity issues served two purposes. First, increasing awareness of the built environment prepared the promotoras to identify environmental change likely to enhance the physical activity environment and then present these recommendations to the community. Second, the promotoras prepared for a community leadership role that was consistent with the promotora model [30, 31], including community organizing amongst church members and advocating for improvements to the built environment. The hierarchy of built environmental targets of change was established based upon three factors: a) the timeframe in which change could realistically occur in proximity to the church (e.g., on church premises); b) the proximity of the environmental target to the church, defined as being within one block or near enough to the church so that traveling there by foot would not pose an undue barrier; and c) the level of interest of the church in a given target for change. Following training with Circulate San Diego, promotoras gathered church members who were interested in improving their communities to identify potential targets for change and used collaborative processes to select two projects, one at the church site and another in the community surrounding the church. Both targets were required to result in improving opportunities for and reducing environmental barriers to physical activity. Because churches were located throughout San Diego County, environmental targets varied by church site. Some churches were in more rural communities while others were in more urban areas; therefore church members identified different kinds of projects. With a commitment to the collaborative process, environmental projects were not dictated by project staff but were identified by church members themselves. As a result, evaluation of the projects consisted of completion of both the church- and community-level projects within the two-year intervention period and submission of a final report. Examples of church-level projects included repainting of basketball court lines and replacement of basketball nets, beautification of church grounds to promote outdoor activities, and increased lighting to enhance safety and security. Community-level projects included traffic calming solutions, park beautification projects, trail restoration, improved street lighting, and sidewalk improvements. For community-level projects, promotoras sought advice from Circulate San Diego and project staff on how and where to advocate for changes in their communities. In addition, promotoras were encouraged to collaborate with other community organizations (e.g., civic groups, Health and Human Services Agency, San Diego Organizing Project, and advocacy groups) and government agencies (e.g., schools, recreation centers, public works, engineering, planning, and redevelopment/development agencies) to facilitate these environmental level changes. For projects requiring supplies (e.g., installation of a church garden and re-painting of basketball courts) supplies were either donated by church members or promotoras conducted fundraisers to collect funds for purchasing supplies. No money was provided by the project to facilitate the environmental projects. Once environmental projects were completed, promotoras submitted final reports to the Intervention Coordinator which included meeting agendas and minutes, action plans, community contact information, before and after photographs, and a final summary of the project.
1.5.3. Fe en Acción cancer screening comparison condition
The cancer screening intervention, developed by the Principal Investigator, Intervention Coordinator, and project staff, was based on current cancer screening recommendations from the National Cancer Institute (NCI) and the American Cancer Society (ACS). The intervention was pilot-tested with Latina women from a local church and modified according to their feedback. In addition, advisory committee members from the UCSD Moores Cancer Center and the American Cancer Society reviewed materials and provided feedback. Finally, two church leaders reviewed the intervention materials to assess appropriateness of language for the church context. To enhance the intervention, handouts from NCI and ACS were provided to participants in either Spanish or English.
1.5.4. Individual level
Participants in the cancer screening condition were invited to attend a 6-week group discussion series led by promotoras in which they received information about cancer screening and prevention. Each class consisted of a prayer, overview of objectives, icebreaker activity, didactic lesson, interactive activity, question and answer, and closing prayer. The four classes devoted to specific cancers reviewed the screening recommendations based on guidelines from ACS and NCI, risk factors for cancer, prevention tips, and a review of anatomy of the selected area. The first class provided an introduction and information on the burden of cancer among Latinos. The second class reviewed breast cancer risk factors, screening recommendations, types of breast cancer, and treatment options. The third class covered cervical cancer, including risk factors, human papilloma virus, prevention, and treatment. The fourth class taught participants about colorectal cancer, the risk factors, screening recommendations and types, and included a video. The fifth class covered skin cancer, risk factors, prevention, screening, and treatment. During the final class, participants discussed their rights and responsibilities as patients and learned how to advocate for themselves in the healthcare system. Each class was 1.5–2 hours in duration and structured to allow for discussion and interactive learning activities. At the final class, participants received a graduation certificate and Fe en Acción bracelet. Although the intervention covered the topics of breast, cervical, colorectal, and skin cancers, only the first three cancers were in the evaluation and analyses components. Promotoras in the cancer screening condition recruited and led a minimum of six series of 6-week cancer screening workshops each year of the two-year intervention. Following the completion of each 6-week series, promotoras spent 1–2 weeks recruiting a new group of church members for the next series.
1.5.4.1. Participant engagement in cancer screening classes
Participants were invited to attend classes and to complete all classes in the 6-week series. Promotoras maintained a list of participant attendance and called those participants who had not completed the classes to motivate them to attend. Participants were encouraged to ask questions and share experiences openly with the group. For topics that were too personal to share or for participants who preferred anonymity, promotoras used a box or basket in which participants could leave anonymous questions. Following the session, the promotora either located the answer in the promotora manual or contacted the Intervention Coordinator for assistance. In the following class, the promotora provided answers to the anonymous questions. If participants missed one or more classes during a series, they were encouraged to make up those classes during the next series. The project provided small incentives (pens, bags, prayer cards, etc.) that the promotoras gave out to during interactive learning games and as prizes for attendance.
1.5.5. Interpersonal level
Participants received four MI calls over the course of the two-year intervention. Promotoras used a guide, adapted from Resnicow’s [26], to evaluate barriers to cancer screening, fears about cancer, values related to health and spirituality, and solutions to overcome barriers to screening. Participants reported on their most recent cancer screenings and made goals for age-appropriate screening appointments. In some cases, promotoras accompanied participants to cancer screening appointments, providing social support and comfort. At the end of each MI call, promotoras worked with the participant to establish goals related to cancer screening, which could include calling their doctor to schedule a screening appointment, researching what screening tests are covered by their health insurance, or talking with family members about medical histories. These goals were recorded and the promotora referred to them in subsequent MI calls as a form of accountability.
1.5.6. Organizational level
At the organizational level, churches provided classrooms at the church for cancer screening workshops. In addition, churches allowed promotoras to insert flyers advertising their classes in the weekly church bulletin and to make announcements at mass inviting church members to attend the cancer screening workshops. Church leaders (i.e. priests) were invited to attend the final cancer screening class in the 6-week series to pray for the graduates and support the efforts of the promotora. Finally, churches provided booths at ministry fairs and annual church fairs, where the promotoras invited church members to the cancer screening workshops.
1.5.7. Environmental level
During training, cancer screening promotoras gathered information about local clinics and their services. Lists of these clinics were provided to church members in the cancer screening classes. The promotoras gathered this information to help them network with local healthcare providers and to become knowledgeable about resources in their immediate communities. The curriculum included information about state-funded screening and treatments programs including the Breast and Cervical Cancer Treatment Program (http://www.dhcs.ca.gov/services/medical/Pages/BCCTP.aspx), FamilyPACT (http://www.familypact.org/), and Every Woman Counts (http://www.dhcs.ca.gov/services/Cancer/ewc). Following the implementation of the Affordable Care Act (ACA) legislation, promotoras were referred to workshops on how to enroll in the ACA and to review common questions and concerns. The promotoras then provided this information to study participants at the cancer screening workshops verbally and in the form of handouts.
1.6. Evaluation component
Participants in both the physical activity and cancer screening conditions were measured at each of the following time-points during the study: 1) at baseline (M1), 2) 12 months after the start of physical activity or cancer screening activities (M2), and 3) 24 months after the start of physical activity or cancer screening activities (M3). At each time-point, participants’ MVPA was assessed objectively using an accelerometer, anthropometric measures were recorded, a fitness test was conducted, and a survey was administered (Table 3). All data collectors were blinded to condition for baseline, M2, and M3 measures. Participants received $25 for completion of measures at each data collection point.
Table 3.
Survey measures completed by participants and objective data collected by staff.
| Measures | |
|---|---|
| Primary outcome | Moderate to vigorous physical activity (accelerometer) |
| Secondary outcomes | Leisure time physical activity (Global Physical Activity Questionnaire); anthropometry (height, weight, waist circumference); heart rate/fitness |
| Individual level factors | Diet; self-efficacy for group exercise; behavioral strategies for physical activity; depressive symptoms; stress; sleep; cancer screening knowledge; cancer screening adherence (breast, cervical, colorectal); perceived barriers to cancer screening (breast, cervical, and colorectal). |
| Interpersonal level factors | Social support; neighborhood and church social cohesion |
| Organizational level factors | Church promoting healthy behaviors |
| Environmental level factors | Neighborhood walkability; social environment; presence of features that facilitate physical activity; park use; place attachment; advocacy for community projects; access to health servcies |
| Moderators or covariates | |
| Demographic, socioeconomic, and health insurance | Age, household income, education, marital status, number of children in the home, employment status, occupation, ethnicity, and health insurance status |
| Acculturation | Acculturation scale; country of birth, years living in the US |
| Religiosity | God locus of health control; perceived religious influence of health behavior and illness as a punishment |
1.6.1. Sample size estimation
Sample size was based on a comparison between the two groups across the two post-intervention measurements at M2 and M3 (12 and 24 months following the start of intervention activities) as a vector of repeated measures on the primary outcome of number of minutes per day of MVPA. The intended effect size was based on a review of studies, the 2008 Physical Activity Guidelines for Americans (150 min/week of MVPA) [32] as well as staying within the guidelines standardized effect sizes of 0.3 to 0.5 (small-medium to medium) suggested by Cohen [33].
Although the outcomes will be measured on individuals, randomization to condition occurred at the church level; therefore, some clustering among the observations at the church level was expected. Prior to randomization, churches were stratified by size, as previous studies showed that participants who attended larger churches differed in socio-demographic factors compared to those who attended smaller churches [34]. Based on this evidence, we assumed an intraclass correlation of 0.05. With an alpha level of 0.05, the power achievable with 16 churches and 20 subjects per church was estimated at 85%.
Based on previous intervention studies carried out by this research team on Latino populations in San Diego, we anticipated a dropout rate of 25% over two years. This rate was based on census data on the birthrate of Latinos and account for the assumption that about 5% of our sample might become pregnant over the two-year period. Therefore, instead of 20 participants per church, the target sample for recruitment was 20[1/(1−.25)] = 27 per church. The total sample size proposed was 432 participants across 16 churches. Subsequent evaluation of baseline data found the ICC estimate for MVPA was 0.028, thus affirming our assumption.
1.7. Primary outcome: MVPA
1.7.1. Objective measure of MVPA
The primary dependent variable was assessed using the ActiGraph GT3-X or GT3-X+ activity monitor (Actigraph, Pensacola, FL). ActiGraph monitors are electronic 3-dimensional motion sensors that detect intensity, frequency, and duration of movement on three axes. Participants were asked to wear the ActiGraph at the hip on an elastic belt. Data output has been calibrated [35] to intensity of physical activity for adults, which makes it possible to determine moderate and vigorous intensity physical activity (outcome variable). Valid data were defined as ≥ 10 hours per day of data with non-wear time defined as ≥60 consecutive minutes of zero count values. At each measurement point, participants were asked to wear the ActiGraph for 7 consecutive days to obtain a minimum of 5 valid days of wear (must include at least 1 weekend day). Participants not meeting the minimum wear time criteria were asked to re-wear the device for the number of days needed plus an extra day to ensure sufficient days of data were obtained. Data were processed with each minute counted using the Troiano 2008 cut-points to define MVPA as >2020 counts per minute [36].
1.8. Secondary outcomes
1.8.1. Self-report of physical activity
1.8.1.1. Global Physical Activity Questionnaire (GPAQ)
Developed by the World Health Organization (WHO), the GPAQ was a comprehensive assessment of domain-specific physical activity and sedentary behavior in adults. The 16-item GPAQ evaluates physical activity in three domains (occupational, transport-related [walking/bicycling], and leisure-time) as well as sedentary time. Questions about household activity (cleaning, laundry, home repairs, etc.) were added to capture time spent doing physical activity in the home. The original GPAQ’s occupation activity section was adapted to exclude household activity. A Spanish-language version of the GPAQ has been cross-validated with Actigraph data among Latinas [37].
1.8.2. Body mass index (BMI)
Weight was measured using a digital scale (Health-o-Meter Professional, McCook, IL) set to kilograms. Participants were asked to remove their shoes and bulky clothing. The research assistant recorded the weight of the participant two times and calculated the average. Height was measured twice using a Shorr board™ (Weigh and Measure, LLC, Olney, MD) and an average was calculated from the two measurements. BMI was calculated as the ratio of weight in kilograms divided by the square of the height in meters.
1.8.3. Waist circumference
Measuring 1 inch above the umbilicus and marking the spot with a sticker, the research assistant instructed the participant to cross her arms and place her hands on opposite shoulders. A Gulick measuring tape was extended around the waist and at the end of normal expiration, measurement was taken to the nearest 0.1 centimeters. Waist circumference was measured twice and averaged. Other studies have used similar protocols measuring waist circumference 1 inch above the umbilicus [38,39].
1.8.4. Step test for fitness
To assess heart rate/fitness, participants were asked to complete a 3-minute submaximal step test [40]. To determine if a participant could perform the step-test, trained RA’s measured the participants’ blood pressure using a standardized protocol with an automated blood pressure monitor (Omron Healthcare, Inc, Bannockburn, IL). If a participant had a reading of ≥140 for systolic or ≥90 for diastolic, a second measurement was taken a few minutes following the first measurement. If the second reading was below these cut-points, the participant was asked to perform the step test, otherwise, it was deferred. To start the step test, a digital metronome (SEIKO UK Limited, Berkshire, UK) was set at one of two levels (i.e., 68 or 104 beats per minute) depending on the participants’ reported level of physical activity and age [41]. Once the step test began, heart rate was measured at 2:00, 2:30, and 3:00 minutes with a wearable heart rate monitor (Polar T31-Coded, New York, US). At the end of the test, the participant was asked to immediately sit down. Heart rate was then measured at 30-seconds and 60-seconds post-test. Heart rate recovery was estimated by taking the difference between the peak heart rate (at 3 minutes) and heart rate at 30 and 60 seconds post-test.
1.9. Individual, interpersonal, organizational, and environmental factors (secondary aims)
1.9.1. Individual level
Survey measures examined the following individual-level variables, food/beverage consumption, self-efficacy for participating in group exercise classes, behavioral strategies for physical activity, depressive symptoms, advocacy, health conditions, religiosity, perceived stress, sleep, cancer screening knowledge and screening behaviors, and perceived barriers to screening. An adapted version of the NCI Food Attitudes and Behaviors (FAB) Survey assessed fruit and vegetable consumption [42] and the full version of the NCI Quick Food Scan [43] assessed eating habits. We assessed beverage consumption, particularly soda and sugary drinks, using items developed in house. Self-efficacy for participating in group exercise classes was assessed using items developed in house including perceived efficacy for group exercise and participants’ behavioral strategies for engaging in physical activity. Physician-diagnosed chronic health conditions (diabetes, heart disease, cancer, etc.) were assessed using items adapted from CDC’s Behavioral Risk Factors Surveillance System (BRFSS) [44]. A participant’s belief that God controls her health status was assessed with the God Locus of Health Control (GLHC) [45] scale. To assess emotional health, we used the Center for Epidemiologic Studies Depression scale (10 items) (CES-D-10) [46] and Perceived Stress Scale (PSS) 4-item version [47]. Questions from the Hispanic Community Health Study/Study of Latinos assessed sleep duration and quality [48]. The 2010 BRFSS survey assessed cancer screening behaviors for breast, cervical, and colorectal cancers. The “don’t know” and “refused” options were removed from the response options [44]. To assess participants’ knowledge of cancer, the Esperanza y Vida Cancer Knowledge Questionnaire [49] and Health Information National Trends Survey [50] were used. In addition to the original response options of “true” and “false”, a “don’t know” option was added. We used four scales to assess perceived barriers to screening for breast, cervical, and colorectal cancers: the 1990 Tampa survey [51], Perceived Barriers to Getting Screened [52], Perceived Benefits of CRC Screening and Barriers to Undergoing CRC Screening [53], and Colon Cancer Knowledge and Attitudes [54]. Scales were shortened and responses changed to a 5-point Likert scale.
1.9.2. Interpersonal level
Factors at the interpersonal level deemed related to physical activity included social support for exercise, and social cohesion (in the neighborhood and church). We adapted a previously developed social support measure [55] to specifically assess social support for exercise. The measure allowed respondents to list up to six individuals who provided them with support for exercise, his/her gender and relationship to the respondent, the type and amount of support provided, and the respondent’s satisfaction with this type/level of support. Neighborhood and church social cohesion were assessed using items adapted from validated instruments for neighborhood social cohesion [56].
1.9.3. Organizational level
We adapted items from the Faith and Community Health Assessment survey that assesses health-related activities offered by one’s faith organization to evaluate whether or not a respondent’s church promoted and encouraged activities for physical activity, healthy eating, and cancer screenings [57].
1.9.4. Environmental level
Built and social environmental characteristics of respondents’ residential neighborhoods were assessed subjectively through the survey. Each participant’s residential location was within 15-minutes of the church. Subjective assessment of residential neighborhood walkability (e.g., aesthetics and land use mix) and the social environment (e.g., safety from crime and traffic) were measured using validated scales that assessed participants’ perceptions of neighborhood features related to physical activity [58,59]. In addition, project staff conducted objective assessments of the church neighborhood. The church neighborhood was defined as the block surrounding the church, where the walking groups took place. Two environmental audits objectively assessed the neighborhoods of participating churches: the Pedestrian Environment Data Scan (PEDS) [60], which assessed environmental features that could influence walking in the church neighborhood (e.g., pedestrian paths and road conditions within a mile of the church); and the Physical Activity Resource Assessment (PARA) [61], which evaluated the church environment for recreation facilities (e.g., presence of features for physical activity such as basketball courts; amenities such as trash containers; and incivilities such as graffiti and litter in the church premises). In addition, items were developed to evaluate frequency of use of parks in the participants’ residential neighborhoods and parks near their church. We evaluated attachment to the park near the participants’ church with an adapted version of an instrument that assessed two key dimensions of place attachment, place identity and place dependence [62]. Access to health care was assessed using one item developed by project staff.
1.10. Moderators and covariates
1.10.1. Demographic characteristics
The survey collected age, household income, education, marital status, number of children in the home, employment status, occupation, ethnicity, and health insurance status.
1.10.2. Acculturation
The Bidimensional Acculturation Scale (BAS) for Hispanics assessed acculturation levels in two key domains, Hispanic and non-Hispanic [63]. We also collected reports of country of birth and years living in the US.
1.10.3. Religiosity
We assessed mechanisms of the religion-health connection with two scales previously tested among African Americans: (1) the Perceived Religious Influence of Health Behavior scale (e.g. tobacco use); and (2) the Illness as Punishment for Sin scale, based on the notion that illness is a punishment from God, thereby pointing to the potentially negative effect that religious involvement may have on health [64].
1.10.4. Process evaluation
Process evaluation will help determine whether the promotoras’ efforts to promote physical activity, cancer screening, and to advocate for changes in the physical environment influenced individuals as well as the environment. This type of evaluation will help identify (1) for whom the intervention is effective, (2) what components of the intervention are effective, and (3) under what circumstances the intervention is effective. Process evaluation will also help determine whether the intervention was delivered with fidelity, adhering to the overall planned dose. In the physical activity condition, participants could potentially attend up to 6 one-hour classes each week of the two-year intervention and receive as many as 5 MI calls over the two years. In the cancer screening condition, participants could attend up to 6 cancer screening workshops (1.5–2 hours each) and receive as many as 4 MI calls over the two years. In this multi-level intervention, promotoras completed weekly activity logs indicating activities attempted or completed, which provides information on intervention dose (e.g., number of sessions held; number of participants; number of letters sent to city council). We also collected attendance sheets, call logs, and MI logs. We asked participants about their experience with the promotoras (e.g., leadership ability and encouragement) in the surveys. The Intervention Coordinator conducted quality control checks with the promotoras to ensure they accurately gave information and followed project protocols.
To assess the intensity and quality of promotora-led physical classes, we used SOFIT-X, an observational tool to evaluate group exercise classes [65]. Promotoras were given feedback on the intensity level of classes, quality of instruction, and areas in need of improvement. For the cancer screening classes, intervention staff members observed a selected number of promotora-led classes and provided written and verbal feedback.
1.11. Planned analyses
The proposed statistical analyses take into account the potential church clustering effects. In addition, there are two post-intervention measures. As such, statistical modeling is planned using mixed-effects models. The distribution of MVPA will be examined to determine the appropriate error distribution for the models. The analyses will treat the post-intervention M2 (12 months after the start of intervention) and M3 (24 months after the start of intervention) data as a vector of repeated measures, adjusting for socio-demographic co-variates. Terms in the initial model would include an indicator variable to represent the two conditions, and indicator variable to represent the two time periods, a condition by time interaction, baseline accelerometer-assessed MVPA levels, a random effect for churches and a random effect for participants nested within churches. In the proposed mixed-effects model, we will compare the rates of change over time between the two conditions to determine if the intervention effects are maintained over the follow-up period by evaluating the condition by time interaction. Because the environmental component of the intervention may take longer to show some effect, this would be reflected in the M3 measurement and with a significant interaction. If the interaction is not significant, the interaction will be dropped and a second model will be fitted to assess the overall condition main effect. Secondary outcome measures such as BMI will be analyzed in a similar manner as the primary outcome. Furthermore, we will examine the impact of the intervention on individual, interpersonal, and environmental correlates of physical activity. In the event that some individual, interpersonal, and environmental correlates may be viewed as dichotomous, a generalized linear models approach will be applied using the GLIMMIX procedure in SAS to fit a mixed-effects logistic regression. Their moderating influences can be measured and tested by constructing an interaction between the specific correclate and the intervention condition. These interaction terms would augment models described above for the primary aim.
2. Discussion
To our knowledge, this is the first two-group randomized controlled trial evaluating the impact of multi-level interventions promoting physical activity and cancer screening among low-active Latinas. The group activities as well as the Motivational Interviewing were designed to deliver physical activity and cancer screening educational information, facilitate physical activity and cancer screening social support, identify and address environmental barriers, and provide positive reinforcement for physical activity and cancer screening. These factors are likely to influence individual motivations and attitudes and ultimately impact behaviors. Studies examining the impact of the environment on behavior suggest a positive association between favorable neighborhood environment characteristics (e.g., mixed land use, street connectivity, availability of sidewalks, and access to recreational facilities) and physical activity for transportation and leisure [66]. Previous research involving Latino communities has found that aspects of the environment such as the lack of sidewalks, parks not close to home, lack of safety (e.g., being afraid to walk in the neighborhood) and other environmental barriers discouraged Latinas from being physically active outside in their neighborhood [67,68]. Therefore, targeting the environment is likely to be an important facilitator of Latinas’ physical activity.
The current study differs from previous randomized controlled trials promoting physical activity in faith-based settings in a number of ways. Wilcox et al. randomized Methodist Episcopal churches to an intervention promoting physical activity and healthy eating or delayed intervention condition [69]. A selected group of members from the intervention churches attended cooking trainings where church kitchen staff received information on how to provide healthy meals and snacks within the church context. These churches were given a stipend, monthly mailings (15 months), and technical assistance during program implementation. Study findings showed significant effects favoring the intervention group in self-reported leisure-time MVPA levels. The current study builds on prior research by targeting the built environment and evaluating the impact of a two-year multi-level intervention using the accelerometer. Most research examining the impact of faith-based physical activity interventions have been conducted between 6 and 12 months. The current study aims to examine the long term effects (24 months) of the faith-based physical activity intervention on participants’ physical activity as well as secondary outcomes and psychosocial correlates of physical activity. Thus, the study will add long-term physical activity outcome data for faith-based interventions in the US.
Research examining the impact of faith-based programs on the cancer screening practices of Latinos has shown promise. In the present study, the intervention was delivered by bilingual/bicultural promotoras who were members of the participating churches. Our study augmented previous research by addressing multiple cancers and increasing access to health care services. More randomized community trials using ecological approaches are needed to help build evidence on the types of multi-level programs that are recommended for addressing chronic diseases, including cancer among Latinos.
Faith-based organizations are an important and promising setting in promoting preventive behaviors among Latinos. We focused on Catholic churches because the majority of Latinos identify as Catholic. According to a Pew Research Center report, 68% of Latinos identify as Catholic, 55% of Latino Catholics are Spanish-language dominant, and 69% are from Mexico. Close to 42% of Latino Catholics indicate attending church at least weekly [14]. Given the central role of the church within the Latino community and commitment to the well-being of its members, the church serves as an ideal setting for the current study. Churches support family celebrations such as baptisms and quinceañeras (sweet 15’s). Churches have many advantages as settings for implementing health promotion programs, as they are organizations that have space and facilities to implement such programs that can be sustained. The current study integrates faith-based messages which improves the likelihood that the church will adopt and support the program. For these reasons, faith-based interventions have the potential to address health disparities in physical activity and cancer screening behaviors among Latinas.
Acknowledgments
Preparation of this paper was supported by funding from the National Cancer Institute (R01CA138894; R01CA138894-04S1).
Footnotes
The authors report no competing interests.
References
- 1.Neighbors CJ, Marquez DX, Marcus BH. Leisure-time physical activity disparities among Hispanic subgroups in the United States. Am J Public Health. 2008;98(8):1460–1464. doi: 10.2105/AJPH.2006.096982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, et al. Design and implementation of the hispanic community health study/study of latinos. Ann Epidemiol. 2010;20(8):629–641. doi: 10.1016/j.annepidem.2010.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.LATINOS IN THE UNITED STATES. Popul Bull. 2010;65(3):1–6. [Google Scholar]
- 4.Warnecke RB, Oh A, Breen N, et al. Approaching health disparities from a population perspective: the national institutes of health centers for population health and health disparities. Am J Public Health. 2008;98(9):1608–1615. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. J R Soc Promot Health. 2008;128(1):31–40. doi: 10.1177/1466424007085223. [DOI] [PubMed] [Google Scholar]
- 6.Kerr J, Rosenberg DE, Nathan A, et al. Applying the ecological model of behavior change to a physical activity trial in retirement communities: description of the study protocol. Contemp Clin Trials. 2012;33(6):1180–1188. doi: 10.1016/j.cct.2012.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warren BS, Maley M, Sugarwala LJ, Wells MT, Devine CM. Small steps are easier together: a goal-based ecological intervention to increase walking by women in rural worksites. Prev Med. 2010;50(5–6):230–234. doi: 10.1016/j.ypmed.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Sauaia A, Min SJ, Lack D, et al. Church-based breast cancer screening education: impact of two approaches on Latinas enrolled in public and private health insurance plans. Prev Chronic Dis. 2007;4(4):A99. [PMC free article] [PubMed] [Google Scholar]
- 9.Duan N, Fox SA, Derose KP, Carson S. Maintaining mammography adherence through telephone counseling in a church-based trial. Am J Public Health. 2000;90(9):1468. doi: 10.2105/ajph.90.9.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lopez VA, Castro FG. Participation and program outcomes in a church-based cancer prevention program for Hispanic women. J Community Health. 2006;31(4):343. doi: 10.1007/s10900-006-9016-6. [DOI] [PubMed] [Google Scholar]
- 11.Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Prev Chronic Dis. 2005;2(4):A07. [PMC free article] [PubMed] [Google Scholar]
- 12.Lasater TM, Wells BL, Carleton RA, Elder JP. The role of churches in disease prevention research studies. Public Health Rep. 1986;101(2):125–131. [PMC free article] [PubMed] [Google Scholar]
- 13.Derose KP, Duan N, Fox SA. Women’s receptivity to church-based mobile mammography. J Health Care Poor Underserved. 2002;13(2):199. doi: 10.1353/hpu.2010.0648. [DOI] [PubMed] [Google Scholar]
- 14.Pew Research Center. Changing Faiths: Latinos and the transformation of American faith. http://www.pewhispanic.org/2007/04/25/changing-faiths-latinos-and-the-transformation-of-american-religion/ Published April 25, 2007.
- 15.Kong BW. Community-based hypertension control programs that work. J Health Care Poor Underserved. 1997 Nov;8(4):409–415. doi: 10.1353/hpu.2010.0031. [DOI] [PubMed] [Google Scholar]
- 16.Bopp M, Peterson J, Webb B. A comprehensive review of faith-based physical activity interventions. Am J Lifestyle Med. 2012;6:460–478. [Google Scholar]
- 17.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annu Rev Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 18.Peterson J, Atwood JR, Yates B. Key elements for church-based health promotion programs: outcome-based literature review. Public Health Nurs. 2002;19(6):401–411. doi: 10.1046/j.1525-1446.2002.19602.x. [DOI] [PubMed] [Google Scholar]
- 19.Ellison CG, Levin JS. The religion-health connection: evidence, theory, and future directions. Health Educ Behav. 1998;25(6):700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- 20.Canadian Society for Exercise Physiology. [Accessed February 8, 2010];Physical Activity Readiness Questionnaire -PAR-Q. http://www.csep.ca/cmfiles/publications/parq/par-q.pdf.
- 21.Taylor-Piliae RE, Norton LC, Haskell WL, et al. Validation of a new brief physical activity survey among men and women aged 60–69 years. Am J Epidemiol. 2006;164(6):598–606. doi: 10.1093/aje/kwj248. [DOI] [PubMed] [Google Scholar]
- 22.Smith BJ, Marshall AL, Huang N. Screening for physical activity in family practice: evaluation of two brief assessment tools. Am J Prev Med. 2005;29(4):256–264. doi: 10.1016/j.amepre.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 23.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 24.Arredondo EM, Sotres-Alvarez D, Stoutenberg M, et al. Physical activity levels in US Latino/Hispanic adults: Results from the HCHS/SOL. Am J Prev Med. 2015 doi: 10.1016/j.amepre.2015.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 26.Resnicow K, Jackson A, Braithwaite R, et al. Healthy body/healthy spirit: a church-based nutrition and physical activity intervention. Health Educ Res. 2002;17(5):562–573. doi: 10.1093/her/17.5.562. [DOI] [PubMed] [Google Scholar]
- 27.Resnicow K, Jackson A, Wang T, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the eat for life trial. Am J Public Health. 2001;91(10):1686–1693. doi: 10.2105/ajph.91.10.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arredondo E, Mueller K, Mejia E, Rovira-Oswalder T, Richardson D, Hoos T. Advocating for environmental changes to increase access to parks: engaging promotoras and youth leaders. Health Promot Pract. 2013;14(5):759–766. doi: 10.1177/1524839912473303. [DOI] [PubMed] [Google Scholar]
- 29.Rollnick S, Miller WR. What is motivational interviewing? Behav Cogn Psychother. 1995;23(4):325–334. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- 30.Ayala GX, Vaz L, Earp JA, Elder JP, Cherrington A. Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res. 2010;25(5):815–840. doi: 10.1093/her/cyq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cherrington A, Ayala GX, Elder JP, Arredondo EM, Fouad M, Scarinci I. Recognizing the diverse roles of community health workers in the elimination of health disparities: from paid staff to volunteers. Ethn Dis. 2010;20(2):189–194. [PMC free article] [PubMed] [Google Scholar]
- 32.United States Department of Health and Human Services. 2008 Physical activity guidelines for Americans. USDHHS; Washington, DC: 2008. [Google Scholar]
- 33.Cohen J. Statistical power analysis for the behavioral sciences. Lawrence Erlbaum Associates, Publishers; Hillsdale, NJ: 1988. [Google Scholar]
- 34.Arredondo EM, Elder JP, Ayala GX, Campbell NR. Is church attendance associated with Latinas’ health practices and self-reported health? Am J Health Behav. 2005;29(6):502–511. doi: 10.5555/ajhb.2005.29.6.502. [DOI] [PubMed] [Google Scholar]
- 35.Nichols JF, Morgan Cg, Chabot LE, Sallis JF, Calfas KJ. Assessment of physical activity with the computer science and applications, inc. accelerometer: laboratory versus field validation. Res Q Exerc Sport. 2000;71:36–43. doi: 10.1080/02701367.2000.10608878. [DOI] [PubMed] [Google Scholar]
- 36.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 37.Hoos T, Espinoza N, Marshall S, Arredondo EM. Validity of the Global Physical Activity Questionnaire (GPAQ) in adult Latinas. J Phys Act Health. 2012;9(5):698–705. doi: 10.1123/jpah.9.5.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Folsom AR, Kushi LH, Anderson KE, et al. Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women’s Health Study. Arch Intern Med. 2000;160(14):2117–2128. doi: 10.1001/archinte.160.14.2117. [DOI] [PubMed] [Google Scholar]
- 39.Zhang X, Shu XO, Yang G, et al. Abdominal adiposity and mortality in Chinese women. Arch Intern Med. 2007;167(9):886–892. doi: 10.1001/archinte.167.9.886. [DOI] [PubMed] [Google Scholar]
- 40.Siconolfi SF, Garber CE, Lasater TM, Carleton RA. A simple, valid step test for estimating maximal oxygen uptake in epidemiologic studies. Am J Epidemiol. 1985;121(3):382–390. doi: 10.1093/oxfordjournals.aje.a114010. [DOI] [PubMed] [Google Scholar]
- 41.Butland RJ, Pang J, Gross ER, Woodcock AA, Geddes DM. Two-, six-, and 12-minute walking tests in respiratory disease. Br Med J (Clin Res Ed) 1982;284(6329):1607–1608. doi: 10.1136/bmj.284.6329.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Yaroch AL, Tooze J, Thompson FE, et al. Evaluation of three short dietary instruments to assess fruit and vegetable intake: the National Cancer Institute’s food attitudes and behaviors survey. J Acad Nutr Diet. 2012;112(10):1570–1577. doi: 10.1016/j.jand.2012.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Thompson FE, Midthune D, Subar AF, Kipnis V, Kahle LL, Schatzkin A. Development and evaluation of a short instrument to estimate usual dietary intake of percentage energy from fat. J Am Diet Assoc. 2007;107(5):760–767. doi: 10.1016/j.jada.2007.02.006. [DOI] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey questionnaire. U.S. Department of Health and Human Services; Atlanta, Georgia: 2010. [Google Scholar]
- 45.Wallston KA, Malcarne VL, Flores L, et al. Does god determine your health? the god locus of health control scale. Cogn Ther Res. 1999;23(2):131–142. [Google Scholar]
- 46.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 47.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 48.Hispanic Community Health Study/Study of Latinos. [Accessed May 23, 2010];HCHS/SOL Questionnaire. https://www2.cscc.unc.edu/hchs/system/files/forms/UNLICOMMSleepSLE02182008.pdf.
- 49.Saad-Harfouche FG, Jandorf L, Gage E, et al. Esperanza y vida: training lay health advisors and cancer survivors to promote breast and cervical cancer screening in Latinas. J Community Health. 2011;36(2):219–227. doi: 10.1007/s10900-010-9300-3. [DOI] [PubMed] [Google Scholar]
- 50.National Cancer Institute. [Accessed July 15, 2010];HINTS database. http://hints.cancer.gov/
- 51.Fuller SM, McDermott RJ, Roetzheim RG, Marty PJ. Breast cancer beliefs of women participating in a television-promoted mammography screening project. Public Health Rep. 1992;107(6):682–690. [PMC free article] [PubMed] [Google Scholar]
- 52.Byrd TL, Peterson SK, Chavez R, Heckert A. Cervical cancer screening beliefs among young Hispanic women. Prev Med. 2004;38(2):192–197. doi: 10.1016/j.ypmed.2003.09.017. [DOI] [PubMed] [Google Scholar]
- 53.Hay JL, Ford JS, Klein D, et al. Adherence to colorectal cancer screening in mammography-adherent older women. J Behav Med. 2003;26(6):553–576. doi: 10.1023/a:1026253802962. [DOI] [PubMed] [Google Scholar]
- 54.Walsh JME, Kaplan CP, Nguyen B, Gildengorin G, McPhee SJ, Pérez-Stable EJ. Barriers to colorectal cancer screening in Latino and Vietnamese Americans. Compared with non-Latino white Americans. J Gen Intern Med. 2004;19(2):156–166. doi: 10.1111/j.1525-1497.2004.30263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Marquez B, Elder JP, Arredondo EM, Madanat H, Ji M, Ayala GX. Social network characteristics associated with health promoting behaviors among Latinos. Health Psychol. 2014;33(6):544–553. doi: 10.1037/hea0000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Seidman E, Allen L, Aber JL, et al. Development and validation of adolescent-perceived microsystem scales: social support, daily hassles, and involvement. Am J Community Psychol. 1995;23(3):355–388. doi: 10.1007/BF02506949. [DOI] [PubMed] [Google Scholar]
- 57.Eat Smart. Move More North Carolina. [Accessed February 1, 2010];Eating Smart and Moving More: Planning Guide for Faith Communities. http://ncfamilieseatingbetter.org/faithfulfamilies/_links/ESMMPlanningGuideFaith.pdf.
- 58.Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93(9):1552–1558. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Evenson KR, Sotres-Alvarez D, Deng Y, et al. Accelerometer adherence and performance in a cohort study of US hispanic adults. Med Sci Sports Exerc. 2014;47(4):725–734. doi: 10.1249/MSS.0000000000000478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Clifton KJ, Livi Smith A, Rodriguez D. The development and testing of an audit for the pedestrian environment. Landsc Urban Plan. 2007;80(1–2):95–110. [Google Scholar]
- 61.Lee RE, Booth KM, Reese-Smith JY, Regan G, Howard HH. The Physical Activity Resource Assessment (PARA) instrument: evaluating features, amenities and incivilities of physical activity resources in urban neighborhoods. Int J Behav Nutr Phys Act. 2005;2:13. doi: 10.1186/1479-5868-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williams DR, Vasek JJ. The measurement of place attachment: validity and generalizability of a psychometric approach. Forest Sci. 2002;49(6):830–840. [Google Scholar]
- 63.Marin G, Gamba RJ. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS) Hisp J Behav Sci. 1996;18(3):297–316. [Google Scholar]
- 64.Holt CL, Clark EM, Roth D, et al. Development and validation of instruments to assess potential religion-health mechanisms in an African American population. J Black Psychol. 2009;35(2):271–288. doi: 10.1177/0095798409333593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Duesterhaus M. A system for observing fitness instruction time in group-exercise classes – SOFIT X. San Diego Graduate School of Public Health., San Diego State University; 2011. [Google Scholar]
- 66.Cerin E, Leslie E, du Toit L, Owen N, Frank LD. Destinations that matter: associations with walking for transport. Health Place. 2007;13(3):713–724. doi: 10.1016/j.healthplace.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 67.Evenson KR, Sarmiento OL, Macon ML, Tawney KW, Ammerman AS. Environmental, policy, and cultural factors related to physical activity among Latina immigrants. Women Health. 2002;36(2):43–57. doi: 10.1300/J013v36n02_04. [DOI] [PubMed] [Google Scholar]
- 68.Martinez SM, Arredondo EM, Perez G, Baquero B. Individual, social, and environmental barriers to and facilitators of physical activity among Latinas living in San Diego County: focus group results. Fam Community Health. 2009;32(1):22–33. doi: 10.1097/01.FCH.0000342814.42025.6d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wilcox S, Parrot A, Baruth M, et al. The faith, activity, and nutritio program: a randomized controlled trial in African-American churches. Am J Prev Med. 2013;44(2):122–131. doi: 10.1016/j.amepre.2012.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]