Summary
Treatment of acute promyelocytic leukaemia (APL) with arsenic trioxide (ATO) and all-trans retinoic acid (ATRA) is highly effective first-line therapy, although approximately 5–10% of patients relapse. Tamibarotene is a synthetic retinoid with activity in APL patients who relapse after chemotherapy and ATRA, but has not been studied in relapse after treatment with ATO and ATRA. We report on a phase II study of tamibarotene in adult patients with relapsed or refractory APL after treatment with ATRA and ATO (n = 14). Participants were treated with tamibarotene (6 mg/m2/d) during induction and for up to six cycles of consolidation. The overall response rate was 64% (n = 9), the rate of complete cytogenetic response was 43% (n = 6) and the rate of complete molecular response was 21% (n = 3). Relapse was frequent with 7 of 9 responders relapsing after a median of 4·6 months (range 1·6–26·8 months). The median event-free survival (EFS) was 3·5 months [95% confidence interval (CI) 0–8·6 months] and the median overall survival (OS) was 9·5 months (95% CI 5·9–13·1 months). These results demonstrate that tamibarotene has activity in relapsed APL after treatment with ATO and ATRA and further studies using tamibarotene as initial therapy and in combination with ATO are warranted.
Keywords: Acute promyelocytic leukaemia, tamibarotene, all-trans retinoic acid, arsenic trioxide, clinical trial
The introduction of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO) for treatment of acute promyelocytic leukaemia (APL) has dramatically improved outcomes for patients. Both of these drugs act as differentiating agents while ATO also degrades the PML-RARA transcript and directly induces apoptosis in leukaemia cells (Fang et al, 2002). The efficacy of combination therapy with ATO and ATRA was initially demonstrated in relapsed disease in a small pilot study in patients who had experienced failure to ATRA-based therapy (Aribi et al, 2007). Following this, a phase II trial using this combination in newly diagnosed APL reported a response rate of 92% and overall survival of 85% at 3 years (Estey et al, 2006; Ravandi et al, 2009). Several large randomized trials later confirmed the beneficial role of ATO and ATRA in frontline therapy for APL and reported complete remission (CR) rates in more than 90% of patients, with most patients achieving long-term remission (Powell et al, 2010; Iland et al, 2012; Lo-Coco et al, 2013). Despite this, approximately 5–10% of patients will have resistant disease or relapse after treatment (Powell et al, 2010; Iland et al, 2012; Lo-Coco et al, 2013). Several mechanisms of resistance to ATRA have been proposed, including the development of resistance mutations in the retinoic acid receptor-α (RARA) ligand binding domain, accelerated ATRA catabolism and increased levels of cellular retinoic acid-binding protein (CRABP), which induces retinoic acid metabolism (Adamson et al, 1993; Tomita et al, 2013).
Tamibarotene (previously Am80) is a synthetic retinoid with increased differentiating activity compared to ATRA, based on in-vitro experiments measuring differentiation in APL cell lines (Kagechika et al, 1988; Hashimoto et al, 1995). This agent does not significantly bind to CRABP, suggesting that it may circumvent this mechanism of ATRA resistance (Takeuchi et al, 1998). Tamibarotene has also demonstrated efficacy in APL in untreated patients as well as in those who have relapsed after ATRA and conventional chemotherapy (Tobita et al, 1997; Shinagawa et al, 2014). We report the results of a multi-centre, phase II clinical trial of the synthetic retinoid tamibarotene in APL patients who have relapsed or refractory disease following treatment with both ATRA and ATO.
Materials and methods
Patients
Patients were recruited between November 2007 and October 2011 at eight centres in the United States, Italy and Spain. Patients were eligible for the trial if they were aged 18 years or older, had refractory or relapsed APL and had received prior therapy containing ATRA and ATO, given sequentially or in combination. The diagnosis of APL was made according to World Health Organization (WHO) 2008 criteria based on bone marrow morphology and the presence of t(15;17) by conventional cytogenetics or fluorescence in situ hybridization (FISH) or reverse transcription polymerase chain reaction (RT-PCR) uncovering PML-RARA (Swerdlow et al, 2008). Patients were eligible if they had a morphological or molecular relapse. Refractory disease was defined as having a confirmed diagnosis of APL with a myeloblast and promyelocyte count >10% of bone marrow cells after failing to respond to first- or second-line induction therapy. Relapsed disease was defined as having a myeloblast plus promyelocyte count >10% in the bone marrow or a positive RT-PCR assay for PML-RARA in two consecutive tests separated by at least 1 month following a documented CR. Exclusion criteria for the study included: receipt of chemotherapy within 2 weeks, a history of myelodysplastic syndrome, uncontrolled cardiac disease (such as decompensated heart failure or acute coronary syndrome), uncontrolled renal or liver disease, uncontrolled diabetes or dyslipidemia, active uncontrolled infection, gastrointestinal malabsorption, active second malignancy within 24 months or pregnancy.
Treatment
Patients were treated during induction with tamibarotene (provided by CytRx Corporation, Los Angeles, CA, USA) at a dose of 6 mg/m2/d, taken orally on a twice-daily schedule. Tamibarotene was supplied as 2 mg tablets and calculated doses were rounded up to the nearest even number. The induction period lasted for up to 56 d of continuous treatment or until the achievement of complete remission. After achieving remission, tamibarotene was continued as consolidation therapy at a dose of 6 mg/m2/d, taken orally on a twice-daily schedule in the absence of alternative therapy, such as stem cell transplantation (SCT). Consolidation started within 2–4 weeks of finishing induction therapy and 28-d cycles were repeated every other month for up to six consolidation cycles. Dose reductions to 4·5 and 3 mg/m2/d were allowed for drug-related toxicity.
Follow-up and assessment
Patients had a bone marrow aspiration with conventional cytogenetics and/or FISH and RT-PCR for PML-RARA prior to starting therapy. A bone marrow aspiration was repeated at 29 d after starting therapy and then every 2 weeks until a morphological leukaemia-free state or CR was achieved. After remission was documented, a bone marrow examination was repeated approximately 28 d later to confirm this response. During consolidation, a bone marrow aspirate was performed every 3 months during the first year, every 6 months during the second year and annually after that. Testing for PML-RARA using conventional cytogenetics/FISH and/or RT-PCR for PML-RARA was repeated with each bone marrow aspirate. Pathology, cytogenetic and molecular testing were performed at the individual sites. Adverse events were documented using both patient diaries and at follow-up appointments. Severity of adverse events was graded using version 3.0 of the National Cancer Institute's Common Terminology Criteria for Adverse Events (CTCAE) system (http://ctep.cancer.gov/protocolDevelopment/electronic_applications/docs/ctcaev3.pdf).
Outcomes and statistical analysis
The trial had a two-stage design with an intended total enrollment of 50 patients. The primary endpoint for the trial was the rate of durable response, which was defined as the achievement of CR sustained for at least 28 d. Secondary outcomes included: cytogenetic complete response (CCyR), complete molecular response (CMR), event-free survival (EFS), overall survival (OS) and adverse events. Definitions of endpoints used for the study are described in Appendix S1. Median OS was calculated using the Kaplan–Meier method from the time of starting treatment and data was censored at the time of death or last follow-up. Median EFS was calculated from the time of starting treatment and data was censored at the time of identification of resistant disease, relapse, death or last follow-up, whichever occurred first. A futility analysis was planned after enrolment of 21 patients; at this point, if <3 patients had achieved a durable CR then the response rate would be considered unacceptable and the trial would be terminated. A target CR rate of >25% was predefined by study investigators, and a rate below this value was predetermined to indicate the treatment was ineffective.
Funding and ethics
The trial was sponsored by CytRx Corporation and tamibarotene was provided by the company to the individual sites. The study was registered as a phase II clinical trial through the U.S. National Institute of Health (NCT00520208). The research ethics review boards at each individual enrolling site approved the trial. Informed consent was obtained from all participants enrolled onto the trial. Study investigators had full access to the data and independent evaluation of responses and statistical analysis was performed by the authors.
Results
Study population
Fourteen patients were enrolled between November 2007 and October 2011. The study was stopped because of the slow rate of accrual before the planned interim futility analysis. Baseline characteristics and previous treatments are shown in Table I. A detailed description of prior treatments and responses is available in Appendix S2. Twelve patients had relapsed disease and two had refractory disease. Two patients with relapsed disease (Patients 9 and 12) had a molecular relapse, identified only by RT-PCR, without evidence of morphological relapse. The median duration of the last remission prior to relapse was 278 d (range 28–1176 d) and the duration was greater than 12 months in 10 of 14 patients (Appendix S2). Patients had received a median of 2 (range 2–5) treatment regimens prior to enrolment. Ten patients received at least one cycle of concurrent ATO and ATRA and four received these drugs sequentially. Twelve patients also had previously received conventional chemotherapeutic agents (primarily cytarabine and anthracyclines) and four had previously received gemtuzumab-ozogamicin. Four patients had relapsed after allogeneic SCT prior to enrollment. One of these patients had received an autologous SCT prior to allogeneic SCT. The median duration of treatment with tamibarotene while on trial was 6·7 weeks (range 3–66 weeks).
Table I.
Baseline characteristics and previous treatments.
| Median [range], or n (%) (N = 14) | |
|---|---|
| Characteristics | |
| Age, years | 56 [37–76] |
| Male | 8 (57) |
| Relapsed disease | 12 (86) |
| Molecular relapse only | 2 (14) |
| Morphological relapse | 10 (71) |
| Refractory disease | 2 (14) |
| Performance Status | |
| 0 | 4 (28·6) |
| 1 | 8 (42·9) |
| 2 | 4 (28·6) |
| CR duration (latest remission), d | 278 [28–1176] |
| Achieved CMR with last treatment | 11 (78·6) |
| Previous treatments | |
| Concurrent ATO & ATRA | 10 (71·8) |
| Sequential ATO & ATRA | 4 (28·6) |
| Number of previous treatments | 2 [2–5] |
| Anthracycline | 12 (85·7) |
| Cytarabine | 6 (42·9) |
| Gemtuzumab | 4 (28·6) |
| Allogeneic transplant | 4 (28·6) |
| Autologous transplant | 1 (7·1%) |
CR, complete remission; CMR, complete molecular remission; ATO, arsenic trioxide; ATRA, all-trans retinoic acid.
Response and survival
Individual patient response and survival as well as baseline disease status is shown in Table II. After induction, 5 (36%) patients achieved a CR, 4 (29%) achieved a CR with incomplete recovery of counts (CRi) and 5 (36%) had resistant disease (RD). Six (43%) patients who achieved a CR (n = 3) or CRi (n = 3) achieved a CCyR at a median time of 43 d after starting treatment (range 28–120 d). Two patients with CR (Patient 11) and CRi (Patient 12) were followed by RT-PCR for PML- RARA after induction response and were not re-evaluated with cytogenetics, so their cytogenetic response is unknown; one of these patients (Patient 11) achieved a CMR. One patient with a CR (Patient 6) did not achieve a CCyR but did have a reduction of PML-RARA by FISH from 45% of interphases to 7·5%. Three patients achieved a CMR at a median time of 43 d (range 43–57 d) after starting treatment; a third patient (Patient 6) had a documented complete molecular response by PCR but had a persistent PML-RARA by FISH (7·5%) on the same bone marrow aspirate, thus the PCR result was thought to be a false negative. Patients 9 and 12 were enrolled onto the trial with a molecular-only relapse and neither achieved a CMR during treatment, although both remained in remission (CRi) after induction; the duration of remission after induction until morphological relapse was 8·7 and 4·6 months, respectively. All cases of CR/CRi lasted longer than 28 d, which was predefined as the minimum time period considered to be a durable remission.
Table II.
Treatment response, relapse and survival for individual patients.
| Disease status at enrolment |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | Haematological relapse (Y/N) |
Cytogenetic relapse (Y/N) |
Molecular relapse (Y/N) |
Haematological response |
Cytogenetic response (Y/N) |
Molecular response (Y/N) |
Relapse (Y/N) |
Time to relapse (d) |
Overall survival (d) |
Alive at last follow-up (Y/N) |
| 1 | Y | Y | Y | RD | N | N | – | – | 289 | N |
| 2* | Y | Y | Y | CR | Y | N | N | – | 257 | N |
| 3* | Y | Y | Y | CR | Y | N | N | – | 526 | N |
| 4 | Y | Y | Y | CRi | Y | N | Y | 183 | 213 | N |
| 5 | Y | Y | Y | RD | N | N | – | – | 378 | N |
| 6† | Y | Y | N/A | CR | N | Y | Y | 117 | 183 | Y |
| 7* | Y | Y | Y | CRi | Y | Y | Y | 816 | 1432 | N |
| 8 | Y | Y | N/A | RD | N | N | – | – | 154 | N |
| 9 | N | N | Y | CRi | Y | N | Y | 295 | 320 | N |
| 10 | Y | Y | Y | CR | Y | Y | Y | 49 | 233 | N |
| 11‡ | Y | Y | Y | CR | N/A | Y | Y | 56 | 1769 | Y |
| 12 | N | N | Y | CRi | N/A | N | Y | 141 | 385 | N |
| 13 | Y | Y | Y | RD | – | – | – | – | 64 | N |
| 14 | Y | Y | Y | RD | – | – | – | – | 93 | N |
Time to relapse is calculated from time of first response (CR or CRi).
CR, complete remission; CRi, complete remission with incomplete recovery of counts; RD, resistant disease; N/A, not available; Y, yes; N, no.
Patients 2, 3 and 7 underwent stem cell transplantation after achieving remission.
Patient 6 had a negative molecular test but positive cytogenetics, suggesting that this molecular result was probably not accurate.
Patient 11 had an isolated central nervous system relapse which was successfully treated with IT chemotherapy and craniospinal radiation.
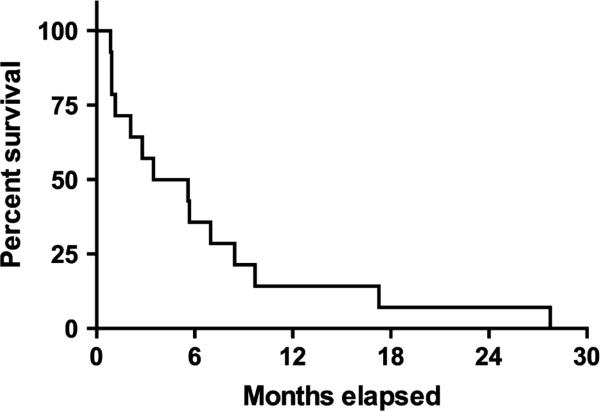
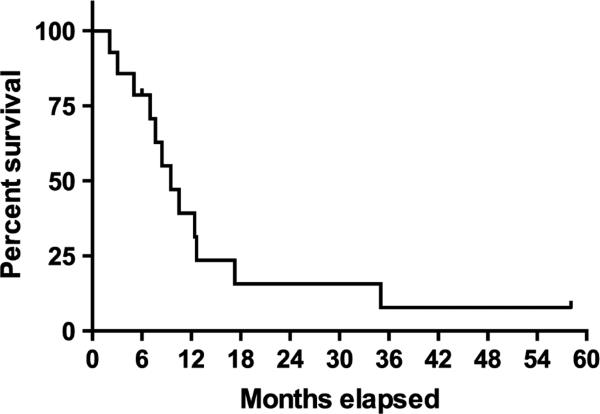
The median EFS for the entire patient population was 3·5 months [95% confidence interval (CI) 0–8·6 months] and the median OS was 9·5 months (95% CI 5·9–13·1 months) (Figs 1 and 2, respectively). The median number of consolidation cycles received by patients achieving CR/CRi was 1 (range, 0–3). Reasons for completing <3 consolidations included: SCT (n = 2), early relapse (n = 2) and unknown reason (n = 1). Two patients (Patients 2, 3) received an allogeneic SCT after achieving a CR; both died of transplant-related complications in CR. Of the other seven patients achieving a response, all eventually relapsed. One patient (Patient 10) had a molecular relapse after receiving one cycle of consolidation and was referred for autologous SCT, but had a morphological relapse prior to this. This patient underwent allogeneic SCT after relapse and died from disease-related causes approximately 2 months later. Another patient (Patient 7) underwent autologous SCT after achieving a CRi and relapsed 816 d after having achieved remission. This patient achieved a complete molecular response prior to transplant. The other five patients achieving a response did not receive SCT; four of them had previously received an allogeneic transplant. The median time to relapse was 4·6 months (range 1·6–26·8 months) (n = 7). One patient (Patient 11) had an isolated central nervous system (CNS) relapse at 56 d, which was successfully treated with intrathecal chemotherapy followed by craniospinal radiation and is currently alive and in remission over 4 years since relapse. This patient did not receive any other systemic therapy. Apart from this patient and the two patients who died of transplant-related complications, all other patients died of complications related to recurrent APL.
Fig 1.
Event-free survival for the entire population of patients with relapsed/refractory acute promyelocytic leukaemia.
Fig 2.
Overall survival for the entire population of patients with relapsed/refractory acute promyelocytic leukaemia.
Adverse events and tolerability
Thirteen patients reported adverse events, with most being non-severe (Grade 1–2). The most frequently reported adverse events (≥3 participants) were: rash (n = 7, grade 1–2), infection (n = 6, grade 1–3), headache (n = 5, grade 1), diarrhoea (n = 3, grade 1–2), neutropenia (n = 3, grade 2–4), insomnia (n = 3, grade 1–2), oropharyngeal pain (n = 3, grade 1), dry skin (n = 3, grade 1) and syncope (n = 3, grade 1–2). Three patients experienced elevated liver transaminases (grade 1–2) and two patients had hypercholesterolaemia/hypertriglyceridaemia (grade 1–2). Adverse events rated grade 3 or higher are shown in Table III. One patient (Patient 4), who had initially achieved a CRi after induction, experienced a fatal CNS hemorrhage when his platelet count was 4 × 109/l, which occurred at the time of disease relapse after 213 d on study. Another patient (Patient 13) with resistant disease died from pneumonia while still on study. This patient had severe neutropenia from the time of enrolment with a neutrophil count consistently less than 0·5 × 109/l. One patient (Patient 7) experienced an episode diagnosed as progressive multifocal leucoencephalopathy (grade 3), although these symptoms resolved and were not identified as related to tamibarotene. Two patients experienced APL differentiation syndrome (grade 2): one patient required a dose reduction of tamibarotene while the other patient continued the tamibarotene at the same dose and the episode was managed with supportive treatment alone.
Table III.
Grade 3–5 adverse events.
| Adverse event | Grade 3 (%) | Grade 4 (%) | Grade 5 (%) | Grade 3–5 (%) |
|---|---|---|---|---|
| Infection | 3 (21) | 0 | 0 | 3 (21) |
| Febrile neutropenia | 2 (14) | 0 | 0 | 2 (14) |
| Neutropenia | 0 | 2 (14) | 0 | 2 (14) |
| Syncope | 2 (14) | 0 | 0 | 2 (14) |
| Hypotension | 2 (14) | 0 | 0 | 2 (14) |
| Hypertension | 1 (7) | 0 | 0 | 1 (7) |
| Angina pectoris | 1 (7) | 0 | 0 | 1 (7) |
| Atrial fibrillation | 1 (7) | 0 | 0 | 1 (7) |
| PML | 1 (7) | 0 | 0 | 1 (7) |
| Haemorrhage | 0 | 0 | 1 (7) | 1 (7) |
| Decreased LOC | 1 (7) | 0 | 0 | 1 (7) |
| Thrombocytosis | 0 | 1 (7) | 0 | 1 (7) |
| Thrombocytopenia | 1 (7) | 0 | 0 | 1 (7) |
| Hypophosphataemia | 1 (7) | 0 | 0 | 1 (7) |
LOC, level of consciousness; PML, progressive multifocal leucoencephalopathy.
Discussion
We report that treatment with single agent tamibarotene was well tolerated and resulted in an overall response rate of 64% in patients with relapsed and refractory APL. Our results suggest that tamibarotene has significant activity in patients with relapsed APL after treatment with ATO and ATRA. Patient responses with tamibarotene were somewhat durable, although median long-term survival was short and relapse occurred in all patients except those who died in remission. Nonetheless, the patient population enrolled in this trial was heavily pretreated with multiple therapies and all patients had >1 relapse prior to enrollment, which suggests the probability of long-term remission was low. Outcomes of patients who relapse or have resistance to both ATRA and ATO have not been described. Tamibarotene appeared to be a safe and tolerable treatment and the adverse effects we observed were comparable to those previously reported (Tobita et al, 1997; Shinagawa et al, 2014). It has been suggested that as tamibarotene has a lower affinity for the dermal retinoic acid receptor-γ, it may have lower rates of dermatological adverse events compared to ATRA (Tobita et al, 1997; Takeuchi et al, 1998). However, in our study, dry skin and rash were among the most frequent adverse events [reported by 10 patients (71%)], although these were mild and manageable. Furthermore, the episodes of APL differentiation syndrome were both non-severe and manageable.
Tobita et al (1997) have also reported on the use of tamibarotene in the relapsed setting. In their trial, 24 patients with APL who relapsed after ATRA-containing treatment were treated with tamibarotene alone (6 mg/m2/d). The majority of patients in the trial had received initial treatment as part of the Japanese Adult Leukaemia Study Group (JASLG) AML-92 trial, which included induction therapy with ATRA as well as daunorubicin and behenoyl cytarabine if considered high risk (peripheral leucocyte count >3 × 109/l) (Asou et al, 1997). Most patients did not receive ATRA as consolidation or maintenance treatment and none had received ATO. Fourteen (58%) patients achieved CR after induction therapy with tamibarotene. Five patients who achieved CR received an allogeneic transplant and none relapsed after a maximum follow-up of 14 months. Eight patients received additional consolidation with conventional chemotherapy and, after a maximum follow-up of 14 months, one patient had relapsed. One patient continued with tamibarotene therapy alone and relapsed after 2 months.
It is unknown if our patients would have had similar results with re-treatment with ATRA and/or ATO. Response rates with ATRA have been reported in a trial of 17 patients with relapsed APL after frontline treatment with chemotherapy alone (Cortes et al, 1994). In this trial, patients with high risk disease also received idarubicin during induction and all patients received idarubicin, mitoxantrone and etoposide during consolidation. Maintenance therapy was given with 6-mercaptopurine and methotrexate for a total of 2 years. Three patients received allogeneic SCT. Of the 14 (82%) patients that achieved CR, 6 (35%) relapsed, 2 (12%) died in CR and 6 (35%) had sustained remissions (Cortes et al, 1994). This CR rate is higher than that reported here with tamibarotene. However, none of the patients in the earlier cohort (Cortes et al, 1994) had previously received ATRA. Outcomes using combination therapy with ATO, ATRA and gemtuzumab in patients with APL relapsing after ATRA-based treatment were reported by Aribi et al (2007). In this pilot trial, 8 patients received induction therapy with ATO, consolidation therapy with ATO, ATRA and gemtuzumab and maintenance therapy with ATRA, idarubicin, 6-mercaptopurine and methotrexate. All patients in this trial achieved CR after induction therapy and all eventually achieved a molecular remission after a median of 4 months (range 1–6 months) on treatment. After a median follow-up of 36 months (range 4–55 months) none of the patients had relapsed, although two deaths occurred in CR (one from lung adenocarcinoma and one from sepsis). We cannot directly compare our results with these trials, but it is reasonable to predict that patients who have resistance to both ATRA and ATO would be less likely to have durable responses after retreatment with ATRA or with ATRA plus ATO.
A recently published randomized trial suggests that tamibarotene may be more effective than ATRA as maintenance therapy in patients with high-risk APL (Shinagawa et al, 2014). In this trial, newly diagnosed patients (n = 344) were treated during induction with ATRA, idarubicin and cytarabine and during consolidation cycles with anthracyclines and cytarabine. Patients in molecular remission after consolidation were randomly assigned to ATRA (n = 135) at a daily dose of 45 mg/m2 or to tamibarotene (n = 134) at a daily dose of 6 mg/m2, for 14 d every 3 months. There was a trend towards a lower number of relapses in the tamibarotene group [20 (15%) vs. 10 (7%)] and improved relapse-free survival (RFS) at 4 years (91% vs. 84%), although neither difference was statistically significant. However, in a subset analysis of 52 patients with high-risk disease (leucocyte count >10 × 109/l) there was improved RFS in the tamibarotene group (87% vs. 52%, P = 0·03; hazard ratio, 0·26; 95% CI, 0·07–0·95). These results suggest the increased potency observed with in vitro differentiation assays using tamibarotene may be clinically relevant and translate to greater differentiation in vivo and decreased development of resistance.
Our results demonstrate the activity of tamibarotene as a single agent in a heavily treated group of patients, which further supports a possible role for the use of this drug in the treatment of APL. Currently, the optimal management for patients relapsing after treatment with ATRA and ATO is unknown. Future clinical trials in the relapsed setting using tamibarotene should consider incorporating other agents, such as anthracyclines, ATO and gemtuzumab, as well as SCT (when available) to improve the possibility of long-term remission. The published results using tamibarotene also suggest a role in the front-line setting and future trials could evaluate concurrent treatment with tamibarotene and ATO in high risk patients.
Acknowledgements
This study received research support from CytRx, CTI (to JC) as well as from the MD Anderson Cancer Center Support Grant CA016672 (to JC).
Footnotes
Author contributions
David Sanford performed the research, analysed the data and wrote the paper. Jorge E. Cortes designed the research study, performed the research, analysed the data and wrote the paper. Francesco Lo-Coco, Miguel A. Sanz, Eros Di Bona, Steven Coutre, Jessica K. Altman, Meir Wetzler, Steven L. Allen, Farhad Ravandi, Hagop Kantarjian performed the research and wrote the paper.
Disclosure
No other authors have a conflict of interest to report.
Supporting Information
Additional Supporting Information may be found in the online version of this article:
Appendix S1. Response criteria used for the study.
Appendix S2. Previous treatments and responses for individual patients.
References
- Adamson PC, Boylan JF, Balis FM, Murphy RF, Godwin KA, Gudas LJ, Poplack DG. Time course of induction of metabolism of all-trans-retinoic acid and the up-regulation of cellular retinoic acid-binding protein. Cancer Research. 1993;53:472–476. [PubMed] [Google Scholar]
- Aribi A, Kantarjian HM, Estey EH, Koller CA, Thomas DA, Kornblau SM, Faderl SH, Laddie NM, Garcia-Manero G, Cortes JE. Combination therapy with arsenic trioxide, all-trans retinoic acid, and gemtuzumab ozogamicin in recurrent acute promyelocytic leukemia. Cancer. 2007;109:1355–1359. doi: 10.1002/cncr.22524. [DOI] [PubMed] [Google Scholar]
- Asou N, Adachi K, Tamura J, Kanamaru A, Kageyama S, Hiraoka A, Omoto E, Sakamaki H, Tsubaki K, Saito K, Ohno R. All-trans retinoic acid therapy for newly diagnosed acute promyelocytic leukemia: comparison with intensive chemotherapy. The Japan Adult Leukemia Study Group (JALSG). Cancer Chemotherapy and Pharmacology. 1997;40(Suppl):S30–S35. doi: 10.1007/s002800051058. [DOI] [PubMed] [Google Scholar]
- Cortes JE, Kantarjian H, O'Brien S, Robertson LE, Koller C, Hirsh-Ginsberg C, Stass S, Keating M, Estey E. All-trans retinoic acid followed by chemotherapy for salvage of refractory or relapsed acute promyelocytic leukemia. Cancer. 1994;73:2946–2952. doi: 10.1002/1097-0142(19940615)73:12<2946::aid-cncr2820731211>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Estey E, Garcia-Manero G, Ferrajoli A, Faderl S, Verstovsek S, Jones D, Kantarjian H. Use of all-trans retinoic acid plus arsenic trioxide as an alternative to chemotherapy in untreated acute promyelocytic leukemia. Blood. 2006;107:3469–3473. doi: 10.1182/blood-2005-10-4006. [DOI] [PubMed] [Google Scholar]
- Fang J, Chen SJ, Tong JH, Wang ZG, Chen GQ, Chen Z. Treatment of acute promyelocytic leukemia with ATRA and As2O3: a model of molecular target-based cancer therapy. Cancer Biology & Therapy. 2002;1:614–620. doi: 10.4161/cbt.308. [DOI] [PubMed] [Google Scholar]
- Hashimoto Y, Kagechika H, Kawachi E, Fukasawa H, Saito G, Shudo K. Correlation of differentiation-inducing activity of retinoids on human leukemia cell lines HL-60 and NB4. Journal of Cancer Research and Clinical Oncology. 1995;121:696–698. doi: 10.1007/BF01218530. [DOI] [PubMed] [Google Scholar]
- Iland HJ, Bradstock K, Supple SG, Catalano A, Collins M, Hertzberg M, Browett P, Grigg A, Firkin F, Hugman A, Reynolds J, Di Iulio J, Tiley C, Taylor K, Filshie R, Seldon M, Taper J, Szer J, Moore J, Bashford J, Seymour JF, Australasian L, Lymphoma G. All-trans-retinoic acid, idarubicin, and IV arsenic trioxide as initial therapy in acute promyelocytic leukemia (APML4). Blood. 2012;120:1570–1580. doi: 10.1182/blood-2012-02-410746. quiz 1752. [DOI] [PubMed] [Google Scholar]
- Kagechika H, Kawachi E, Hashimoto Y, Himi T, Shudo K. Retinobenzoic acids. 1. Structure-activity relationships of aromatic amides with retinoidal activity. Journal of Medicinal Chemistry. 1988;31:2182–2192. doi: 10.1021/jm00119a021. [DOI] [PubMed] [Google Scholar]
- Lo-Coco F, Avvisati G, Vignetti M, Thiede C, Orlando SM, Iacobelli S, Ferrara F, Fazi P, Cicconi L, Di Bona E, Specchia G, Sica S, Divona M, Levis A, Fiedler W, Cerqui E, Breccia M, Fioritoni G, Salih HR, Cazzola M, Melillo L, Carella AM, Brandts CH, Morra E, von Lilienfeld-Toal M, Hertenstein B, Wattad M, Lubbert M, Hanel M, Schmitz N, Link H, Kropp MG, Rambaldi A, La Nasa G, Luppi M, Ciceri F, Finizio O, Venditti A, Fabbiano F, Dohner K, Sauer M, Ganser A, Amadori S, Mandelli F, Dohner H, Ehninger G, Schlenk RF, Platz-becker U, Gruppo Italiano Malattie Ematologiche, d.A., German-Austrian Acute Myeloid Leukemia Study, G. & Study Alliance, L. Retinoic acid and arsenic trioxide for acute promyelocytic leukemia. New England Journal of Medicine. 2013;369:111–121. doi: 10.1056/NEJMoa1300874. [DOI] [PubMed] [Google Scholar]
- Powell BL, Moser B, Stock W, Gallagher RE, Willman CL, Stone RM, Rowe JM, Coutre S, Feusner JH, Gregory J, Couban S, Appelbaum FR, Tallman MS, Larson RA. Arsenic trioxide improves event-free and overall survival for adults with acute promyelocytic leukemia: North American Leukemia Intergroup Study C9710. Blood. 2010;116:3751–3757. doi: 10.1182/blood-2010-02-269621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravandi F, Estey E, Jones D, Faderl S, O'Brien S, Fiorentino J, Pierce S, Blamble D, Estrov Z, Wierda W, Ferrajoli A, Verstovsek S, Garcia-Manero G, Cortes J, Kantarjian H. Effective treatment of acute promyelocytic leukemia with all-trans-retinoic acid, arsenic trioxide, and gemtuzumab ozogamicin. Journal of Clinical Oncology. 2009;27:504–510. doi: 10.1200/JCO.2008.18.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinagawa K, Yanada M, Sakura T, Ueda Y, Sawa M, Miyatake J, Dobashi N, Kojima M, Hatta Y, Emi N, Tamaki S, Gomyo H, Yamazaki E, Fujimaki K, Asou N, Matsuo K, Ohtake S, Miyazaki Y, Ohnishi K, Kobayashi Y, Naoe T. Tamibarotene as maintenance therapy for acute promyelocytic leukemia: results from a randomized controlled trial. Journal of Clinical Oncology. 2014;32:3729–3735. doi: 10.1200/JCO.2013.53.3570. [DOI] [PubMed] [Google Scholar]
- Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. IARC Press; Lyon, France: 2008. [Google Scholar]
- Takeuchi M, Yano T, Omoto E, Takahashi K, Kibata M, Shudo K, Harada M, Ueda R, Ohno R. Relapsed acute promyelocytic leukemia previously treated with all-trans retinoic acid: clinical experience with a new synthetic retinoid, Am-80. Leukaemia & Lymphoma. 1998;31:441–451. doi: 10.3109/10428199809057604. [DOI] [PubMed] [Google Scholar]
- Tobita T, Takeshita A, Kitamura K, Ohnishi K, Yanagi M, Hiraoka A, Karasuno T, Takeuchi M, Miyawaki S, Ueda R, Naoe T, Ohno R. Treatment with a new synthetic retinoid, Am 80, of acute promyelocytic leukemia relapsed from complete remission induced by all-trans retinoic acid. Blood. 1997;90:967–973. [PubMed] [Google Scholar]
- Tomita A, Kiyoi H, Naoe T. Mechanisms of action and resistance to all-trans retinoic acid (ATRA) and arsenic trioxide (As2O 3) in acute promyelocytic leukemia. International Journal of Hematology. 2013;97:717–725. doi: 10.1007/s12185-013-1354-4. [DOI] [PubMed] [Google Scholar]