Abstract
It is well known that obesity has a multifactorial etiology, including biological, environmental, and psychological causes. For this reason, obesity treatment requires a more integrated approach than the standard behavioral treatment based on dietary and physical activity only. To test the long-term efficacy of an enhanced cognitive–behavioral therapy (CBT) of obesity, including a virtual reality (VR) module aimed at both unlocking the negative memory of the body and to modify its behavioral and emotional correlates, 163 female morbidly obese inpatients (body mass index >40) were randomly assigned to three conditions: a standard behavioral inpatient program (SBP), SBP plus standard CBT, and SBP plus VR-enhanced CBT. Patients' weight, eating behavior, and body dissatisfaction were measured at the start and upon completion of the inpatient program. Weight was assessed also at 1 year follow-up. All measures improved significantly at discharge from the inpatient program, and no significant difference was found among the conditions. However, odds ratios showed that patients in the VR condition had a greater probability of maintaining or improving weight loss at 1 year follow-up than SBP patients had (48% vs. 11%, p = 0.004) and, to a lesser extent, than CBT patients had (48% vs. 29%, p = 0.08). Indeed, only the VR-enhanced CBT was effective in further improving weight loss at 1 year follow-up. On the contrary, participants who received only the inpatient program regained back, on average, most of the weight they had lost. Findings support the hypothesis that a VR module addressing the locked negative memory of the body may enhance the long-term efficacy of standard CBT.
Introduction
The diffusion of obesity is now a worldwide problem.1 More than 1.5 billion people are overweight, and obesity rates have increased in both developed and emerging countries. In the United States alone, the prevalence of obesity reached 35.8% among adult women and 35.5% among adult men.2
Many consider obesity as a problem of energy regulation only: energy intake exceeds energy expenditure. However, as obese subjects know well, metabolic needs can easily be overwhelmed by a willingness to eat when not hungry.3 On one side, living in an obesogenic environment characterized by the increased accessibility of palatable energy-rich foods may push subjects without self-regulatory competence to overeating.4 On the other side, a recent systematic review clearly underlined that higher stress is associated with higher body weight and unhealthy dietary behaviors.5 Furthermore, different research suggests a comorbidity between obesity and eating disorders6,7: individuals with binge-eating disorder have a lifetime prevalence of obesity of >80%.
In sum, obese subjects can be considered a heterogeneous population with different adaptive characteristics who may show complex and synergic metabolic, environmental, social, and psychological distresses and causes. For this reason, obesity treatment requires a more integrated approach than the standard behavioral treatment based on dietary and physical activity only. This approach, even if effective in the short term, is not effective in the long term: obese individuals usually regain most of the weight lost (a third to half of the loss) within the first year after treatment and return to baseline weight in the next 3–5 years.8,9
The recent report prepared by the National Institutes of Health (NIH) working group on weight regain after weight loss10 identifies in decreased adherence and its causes a critical behavioral challenge to weight loss maintenance. The report suggests: “One explanation for the declining adherence is that the perceived costs of adherence gradually exceed the perceived benefits. Initially, the positive consequences of weight loss (e.g., sense of accomplishment; better fit of clothes) outweigh the cognitive and physical effort needed to lose weight. Later, when the goal is to maintain lost weight, the positive feedback is less compared to the effort required to keep adhering to the same regimen. Thus, the benefits no longer seem to justify the costs.”10(p8) Bray and Wadden,11 commenting on the report, underline the critical role of behavioral fatigue in which dieters grow weary of diet and exercise regimens that appear to yield little benefit after the first 6 months.
Different studies suggest that critical variables that dieters use to evaluate the benefit of their weight-loss behavior are body dissatisfaction,12 the level of attributed self-efficacy13,14—the individual's belief that one has the ability to engage successfully in a specific behavior—and the level of self-worth in terms of weight and shape.15 For example, a recent study assessing the psychological and behavioral predictors of 3 year weight-loss maintenance in women16 clearly showed that improving body image and increasing autonomous and intrinsic motivation for exercise also significantly improves long-term weight-loss maintenance: women with a better body image after the 1 year intervention were most likely to achieve at least 3% or 5% weight loss.
Body dissatisfaction also appears to be related to the etiology of eating disorders, including binge eating. Dakanalis et al. used both a cross-sectional (583 women aged 18–28 years) and a longitudinal study (361 adolescent girls over a 2 year period) study design17,18 to explore the effects of this variable on the development of eating disorders. They found that body dissatisfaction was strongly and positively related to ED symptoms. Specifically, initial levels of body dissatisfaction (T1) influenced the development of future general negative affect and dieting behaviors (T2), which, in turn, both contributed to future eating disturbances (T3).
Different studies19–21 suggest that, in both male and female overweight adolescents, the impairment in emotional well-being is primarily due to dissatisfaction with body size and shape. On one side, as demonstrated by Foster et al., changes in weight are not related to changes in body image.22–24 On the other side, however, individuals who improve self-esteem and body dissatisfaction at the end of a weight-loss treatment have a higher likelihood of achieving a significant weight loss in the long term, independently of their initial weight loss.24
These apparently contradictory findings—body dissatisfaction is related to the shape and the weight of the individual, but changing shape and weight does not modify body dissatisfaction—can be explained by the Allocentric Lock Hypothesis (ALH).25–29 It suggests that maintenance of body dissatisfaction after weight loss may be caused by a primary disturbance in the way the body is experienced and remembered29: obese patients may be locked to an allocentric (observer view) disembodied negative memory of the body that is no more updated by contrasting egocentric representations driven by perception.30 In other words, these patients may be locked to a negative image of their body, a mental representation that perception is not able to update even after a demanding diet and a significant body shape improvement due to weight loss. The impossibility of experiencing a better body can explain the behavioral fatigue underlined by the NIH working group on weight regain after weight loss.10 Furthermore, if even successful dieting attempts are not able to improve body dissatisfaction, then people may either stop adhering to diet prescriptions, or, at the opposite end, start more radical dieting attempts, which, however, can sooner or later lead to even worst outcomes (i.e., eating disinhibition and binge eating).
To counter a possible allocentric lock in obese patients, this study included a virtual reality (VR) clinical module aimed both at unlocking the negative memory of the body27 and at modifying its behavioral and emotional correlates within an inpatient form of the standard cognitive–behavioral treatment (CBT) of obesity. A previous randomized clinical trial31 demonstrated the superior efficacy of this VR-enhanced CBT program over standard CBT and an inpatient, medically managed program in improving the long-term outcome of obese patients with a binge eating disorder.
Similarly, this study aimed to evaluate the brief and long-term incremental efficacy of the VR-enhanced CBT of obesity in a randomized controlled trial with morbid (body mass index [BMI] >40) female obese patients referred to an inpatient behavioral program. The primary outcome measure was weight-loss maintenance. It was hypothesized that the VR-enhanced CBT is more effective than the inpatient program only as well as standard CBT in maintaining or further improving weight loss at 1 year follow-up.
Methods
Participants
Three hundred consecutive obese inpatients admitted to the obesity unit of the Istituto Auxologico Italiano, Verbania, Italy, for the treatment of obesity and related comorbidities were seen a few days after hospitalization for screening interviews. Criteria for participation in the study included: (a) a BMI ≥40; (b) 18–50 years of age; (c) no other concurrent severe eating (bulimia, binge eating, or eating disorder not otherwise specified) or psychiatric disturbances (psychosis, depression with suicidal risk, or alcohol or drug abuse); (d) no concurrent involvement in other treatment, including medication; (e) no concurrent medical condition not related to the disorder; and (f) written and informed consent to participate.
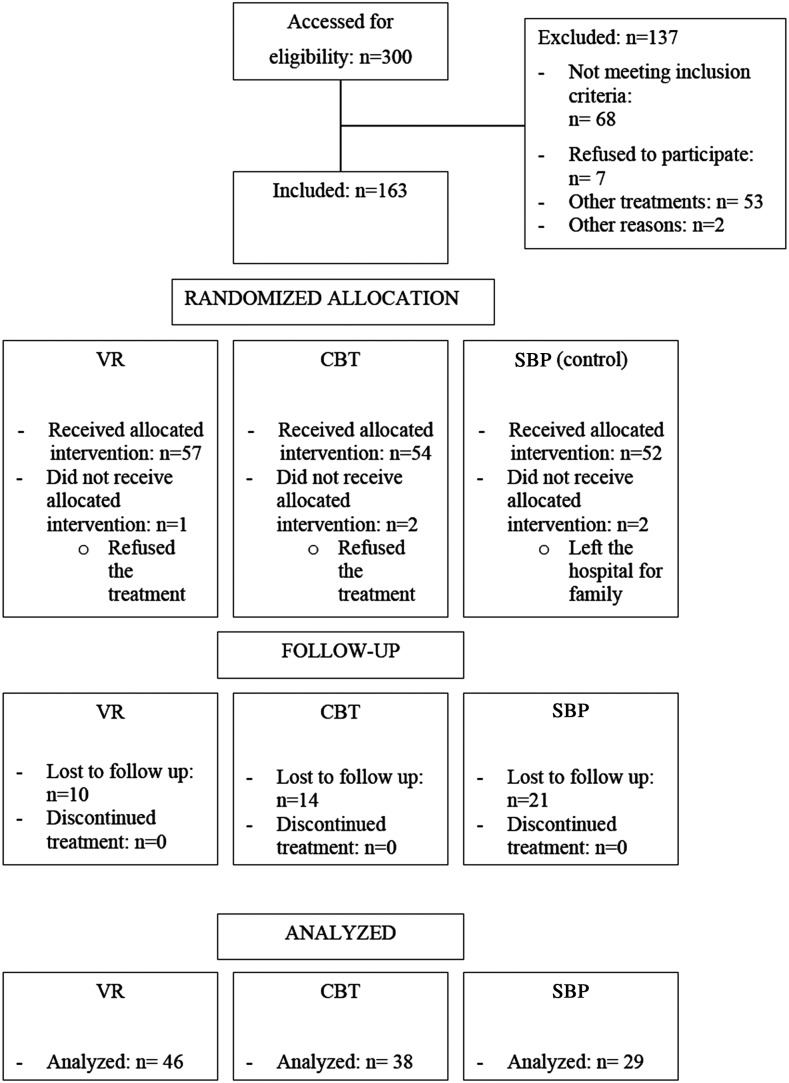
Of the 300 patients who were admitted, 137 either did not fulfill the inclusion criteria or were excluded for other reasons (e.g., time constraints, involvement in a different protocol). Notably, no males were included because none of the male inpatients who were admitted to the obesity unit during the recruitment period had a BMI ≥40. Patients meeting the inclusion criteria were then assigned to one of the three treatment conditions described in below, all conducted on an inpatient basis (see Fig. 1 for detail). The randomization scheme used for selecting the condition was generated by using the Web site www.randomization.com.
FIG. 1.
Study flowchart. VR, virtual reality; CBT, cognitive-behavioral therapy; SBP, standard behavioral program.
After randomization, five patients rejected participation in the study because in their opinion a psychological intervention was not required (one in the VR condition and two in the CBT condition). Two patients in the standard behavioral inpatient program (SBP) left the hospital for family and work reasons. A chi-square analysis did not show any statistically significant differences in the rejection rates between the groups.
Finally, 158 patients (Mage = 35.63 ± 8.04 years; Mweight = 110.33 ± 12.27 kg; Mheight = 1.61 ± 0.03 m; MBMI = 42.24 ±6.01) entered the treatment phase and were deemed sufficient to detect a medium treatment effect with a 90% statistical power in the analysis of variance (ANCOVA) described below. This sensitivity power analysis was run with the G*Power software (v3.1.3).
The majority (51%) had graduated from upper secondary school, were employed at the time of the study (68.2%), and were not married.
The study was approved by the Ethical Committee of the Istituto Auxologico Italiano and received by Current Controlled Trials Organization the official trial number ISRCTN59019572.
Procedures
Each patient was assigned to one of the following treatment conditions:
SBP
This was the common treatment condition for all the participants. It consists of hospital-based living for 6 weeks. Inpatients receive medical, nutritional, physical, and psychological care the goal of which is to provide practical guidelines (e.g., stressing gradual weight loss with the caloric restriction achieved largely by reductions in fat intake), plus a low-calorie diet (1,200 kcal/day) and physical training (30 minutes of walking twice a week as a minimum).
CBT
Therapists followed a detailed manual that outlined the content of each session. This manual was based on the CBT approach described by Cooper et al.32,33 It was developed during a year of intensive pilot work and adapted to the inpatient setting. Patients were taught to self-monitor their food intake and eating patterns thoughts, as well as the circumstances and environment surrounding eating (e.g., whether eating alone or with others, speed of eating, and place of eating). Patients were also taught to identify problems in eating, mood, and thinking patterns and to develop alternative patterns gradually.
In particular, after the first week, the patients entered five weekly group sessions aimed at addressing weight and primary goals, and 10 biweekly individual sessions aimed at establishing and maintaining weight loss, addressing barriers to weight loss, increasing activity, addressing body image concerns, and supporting weight maintenance.
VR-enhanced CBT
Like the CBT condition, participants allocated to this treatment received 15 additional sessions over 5 weeks.34 After the first inpatients week, participants entered five weekly group sessions similar to the CBT ones (focused on concerns about body weight and shape and problematic eating) and 10 biweekly VR sessions. The treatment was based on a detailed protocol describing the contents of each of the 15 sessions.31,34 For the VR sessions, the NeuroVR open source software (www.neurovr.org) was used.35–37 NeuroVR includes 14 virtual environments used by the therapist during a 60 minute session with the patient. The environments present critical situations related to the maintaining/relapse mechanisms (home, supermarket, pub, restaurant, swimming pool, beach, gymnasium) and two body-image comparison areas. Through the VR experience, patients practice both eating/emotional/relational management and general decision-making and problem-solving skills. By directly practicing these skills within the VR environment, patients are helped in developing specific strategies for avoiding and/or coping with triggering situations.
The first session is used to assess any stimuli that could elicit abnormal eating behavior. Specifically, attention is focused on the patient's concerns about food, eating, shape, and weight. At the end of the first VR session, the therapist uses the miracle question, a typical approach used by the solution-focused brief therapy.38,39 According to this approach, the therapist asks the patient to imagine what life would be like with a lower weight. Using VR to experience the effects of the miracle34—a virtual balance shows the weight expected by the patient—individuals are more likely not only to gain an awareness of their need to do something to create change but also to experience a greater sense of personal efficacy.
The next nine sessions are used to assess and modify:
• The expectations and emotions related to food and weight (functional analysis). The therapist helps patients to recognize why they eat and what they need either to avoid or to cope with the specific emotional/behavioral triggers. This is achieved by integrating different CBT methods: countering, alternative interpretation, label shifting, and deactivating the illness belief.
• The body experience of the subject. We included a specific VR body-image rescripting protocol (see [27] for a detailed description) aimed at updating the memory of the body. In the protocol different body related situations are experienced in both first-person (the patient does not see his/her body in the scene) and third-person perspective (the patient sees his/her body in the scene) integrating the therapeutic methods used by Butter and Cash40 and Wooley and Wooley.41 Specifically, the body image comparison areas are used in the same way as guided imagery42 is used in the cognitive and visual/motorial approach. In general, the therapist asks the patient to give detailed descriptions of the virtual experience and of the feelings associated with it. Furthermore, the patient is taught how to cope with them using different techniques.42
The VR-enhanced CBT and traditional CBT were administered by two licensed clinical psychologists and one licensed psychotherapist under the supervision of a senior licensed psychotherapist. The three therapists were randomized to the two treatment conditions.
After hospital discharge, continuity of care and support through telecommunication devices (e-mail, chat, and telephone as preferred) were offered to each patient. Contacts were not scheduled and were dependent only on each patient's needs.
Assessment
Participants' data were obtained 1 week after the start of the inpatient program, during the last week of hospitalization, and at 1 year follow-up (by postal mail). Height was measured with a stadiometer, and weight was assessed on a balance beam scale with the participant in lightweight clothing with shoes removed. Data at follow-up were self-reported. The following psychometric tests were also administered to the study participants at entry to the study and at the end of the inpatient treatment:
• The Italian version43 of the Body Satisfaction Scale—BSS.44 The scale consists of a list of 16 body parts, half involving the head (above the neck) and the other half involving the body (below the head). The subjects rate their satisfaction with each of these body parts on a 7-point scale: the higher the rating, the more dissatisfied the individual. In the Italian validation study, the Cronbach's alpha for the total score was 0.86 in the high-school sample, 0.83 in the university sample, and 0.86 in the eating disorders sample.
• The Italian version45 of the Body Image Avoidance Questionnaire—BIAQ.46 This is a 19-item self-report questionnaire on avoidance of situations that provoke concern about physical appearance, such as avoidance of tight-fitting clothes, social outings, and physical intimacy. In particular, the questionnaire measures the avoidance behaviors and grooming habits associated with negative body image. In the Italian validation study, the Cronbach's alpha for the total score was 0.77 in the high-school sample, 0.76 in the university sample, and 0.75 in the eating disorders sample.
• The Contour Drawing Rating Scale—CDRS.47 This is a set of nine male and female figures with precisely graduated increments between adjacent size. Subjects are asked to rate the figures based on the following instructional protocol: (a) current size and (b) ideal size. The difference between the ratings is called the “self-ideal discrepancy score” and is considered to represent the individual's body dissatisfaction.
Statistical analysis
Before testing the effect of the VR treatment on the outcome measure (weight-loss maintenance), a series of individual one-way analyses of variance (ANOVA) were conducted to identify possible pretreatment differences among conditions in demographic characteristics, weight, BMI, and the psychological variables.
The ANCOVA on gain scores (differences in weight and psychological scores between time points) adjusting for the pretreatment data was used to test between-group differences in brief and long-term changes. This approach is considered more effective than classical repeated measures ANOVA.48
Finally, the odds of maintaining or further improving weight loss at 1 year follow-up were compared between each pair of the three conditions. Confidence intervals (95%) were used to establish the statistical significance of the ratios. The associations between the maintenance or further improvement of weight loss and the experimental conditions were also tested by means of the chi-square test. Critical alpha was set to 0.015 because of the multiple comparisons among the conditions.
Results
Pre- and post-treatment analysis
No statistically significant difference was found among conditions either in the pretreatment characteristics or in all gain scores at the end of the inpatient treatment. The whole sample achieved a significant weight loss (effect size 0.72). In particular, the control group lost on average 6.2% of the starting body weight, 7.4% the CBT group, and 6.25% the VR group (Table 1).
Table 1.
Weight Features in the Three Experimental Conditions
| Weight | ||||
|---|---|---|---|---|
| Treatments: | Start (n = 158) | End (n = 158) | 12 month follow-up (n = 113) | Effect size (Hedges g): start/12 month follow-up |
| VR | 112.1 ± 15.6 | 105 ± 14.3 | 105.4 ± 16.2 | −0.472 |
| CBT | 108 ± 12.1 | 100.5 ± 11.3 | 105.8 ± 17.1 | −0.151 |
| SBP | 110 ± 15.2 | 103.2 ± 14.5 | 114.7 ± 19.3 | 0.277 |
| Feature: | Subjects who maintained or improved the weight reduction achieved after the treatment (12 month follow-up) | |||
|---|---|---|---|---|
| Treatments: | Yes | No | Total | Enrolled at start |
| VR | 22 | 24 | 46 | 56 |
| CBT | 11 | 27 | 38 | 52 |
| SBP | 3 | 26 | 29 | 50 |
| χ2 = 11.73 | df = 2, p = 0.003 | |||
| Feature: | Subjects with a weight equal or higher than the initial one (12 month follow-up) | |||
|---|---|---|---|---|
| Treatments: | No | Yes | Total | Enrolled at start |
| VR | 38 | 8 | 46 | 56 |
| CBT | 25 | 13 | 38 | 52 |
| SBP | 8 | 21 | 29 | 50 |
| χ2 = 23.27 | df = 2, p = 0.000 | |||
SBP, standard behavioral program, including nutritional groups, a low-calorie diet (1,200 kcal/day), and physical training; CBT, SBP plus cognitive–behavioral therapy; VR, SBP plus VR-enhanced cognitive–behavioral therapy.
On average, the psychological variables, that is, eating behavior characteristics (DIET) and body satisfaction (BSS, BIAQ, and CDRS), also improved significantly after the inpatient treatment (effect size 0.16–0.26). Unexpectedly, no statistically significant difference was found among the three conditions, even if the VR group showed higher improvements in all measures.
Follow-up analysis
Out of 158 patients, 113 responded to the follow-up call and provided their weight data. The majority of patients who did not respond were in the SBP group (n = 21), followed by CBT (n = 14) and VR (n = 10). The chi-square test showed a significant association between the dropout rates and the experimental conditions (p = 0.02). Given this and the high probability that dropped patients had regained back most of the baseline weight, no data imputation was performed, and only available data were analyzed (for a discussion of this choice, see the Discussion). In the explorative comparison of pre versus follow-up mean scores within each condition, only the VR group kept on showing a statistically significant weight loss. In a comparison of post versus follow-up data, only the SBP group showed a statistically significant weight regain. The CBT group showed a nonsignificant weight increase, while no change was found within the VR group (Table 1). The one-way ANCOVA on the post to follow-up weight changes showed a significant group effect. Post hoc analyses revealed a significant difference between the VR and the SBP conditions, and also between the CBT and the SBP conditions, but not between VR and CBT.
Finally, odds ratios showed that patients in the VR condition had a greater probability of maintaining or further improving weight loss at 1 year follow-up than patients in the SBP condition had (% of subjects who maintained or improved the weight reduction: VR [22/46, 48%] vs. SBP [3/26, 11.5%], OR 7.03 [95% CI 1.85–26.70]) and, to a lesser extent, than patients in the CBT condition had (% of subjects who maintained or improved the weight reduction: VR [22/46, 48%] vs. CBT [11/38, 29%], OR 2.25 [95% CI 0.91–5.58]).
Discussion
A randomized controlled clinical trial (ISRCTN59019572) testing the long-term incremental efficacy of a new VR-enhanced CBT for morbid obese patients (BMI >40) was presented. Starting from the ALH,28 a VR-based clinical module aimed at both unlocking the negative memory of the body and modifying its behavioral and emotional correlates was integrated into a reduced form of the standard CBT of obesity.
The incremental efficacy of the VR-enhanced CBT over a standard behavioral inpatient program and also over a reduced form of the standard CBT in maintaining or further improving weight loss in the long term was tested in a three-arm RCT involving 158 female obese inpatients.
As expected, the inpatient program was effective in significantly reducing the weight of all patients (>5% of the baseline weight on average) in a relatively brief period (6 weeks) and independently from the added CBT and VR treatments. This was a largely expected result given the highly controlled environment where patients attended the inpatient program. However, the VR-enhanced CBT that was delivered during the inpatient program was shown to be more effective in the long term. In fact, it proved superior to both the inpatient program and, to a lesser extent, to the standard CBT in preventing weight regain and in further improving weight loss after 1 year from the end of treatment. The reduced form of the standard CBT was effective over the inpatient program in preventing weight regain, but follow-up data showed an almost significant difference in favor of the VR condition (Table 1). Indeed, only the VR-enhanced CBT was effective in further improving weight loss at 1 year follow-up. On the contrary, participants who received only the inpatient program regained back, on average, most of the weight they had lost.
Limitations
Some study limitations deserve attention. The first one is the medium rate of patients who dropped out from follow-up (28.5%). The reasons for not completing the last assessment were not investigated, but it is hypothesized that most of the dropped patients had regained the weight they had lost with treatment or put on even more weight. Given the significant association of dropout rates with the treatment conditions and the possible relationship between missing data and the study outcome (weight loss maintenance), the missing process was hypothesized to be not at random in all likelihood and no data imputation was thus used. Unlike the previous study on obese patients with a binge eating disorder where no significant difference in dropout rates was found between conditions,31 only available data were considered in the follow-up analysis and, even if the long-term results of this study can be biased, their reliability is probably equal to or even higher than that of any other results that could have been found with an intention-to-treat approach. Indeed, given the higher rate of dropouts in the SBP group and, to a lesser extent, in the CBT condition compared with VR, imputing weight data according to the credible hypothesis that dropped patients had regained back most of the baseline weight would have done nothing other than increase the statistical and clinical significance of the VR-enhanced CBT effect.
Second, the standard CBT used in this study was a reduced (6-week) version of the Oxford outpatient protocol.32,33 Given the major changes that were made to the original format, comparing the present results with the ones obtained in studies that implemented the original protocol is impossible. Third, no males were included in the clinical trial because none of the male inpatients who were screened during the recruitment period fulfilled the BMI criterion. Thus, findings can be generalized only to obese female patients with a BMI ≥40. Fourth, the psychosocial variables were not measured at follow-up. The assessment of psychological, emotional, and social variables that can act as outcomes as well as mediators or moderators of the treatment effect would have added further information on the efficacy of the VR-enhanced CBT.
Conclusions
Obese subjects are a heterogeneous population with complex and synergic metabolic, environmental, social, and psychological distresses and causes. For this reason, obesity treatment requires a more integrated approach than the standard behavioral treatment based on dietary and physical activity only. Specifically, a common problem within obese patients is the experience of a significant level of body dissatisfaction even after a significant weight loss.
The ALH28 suggests that these patients may be locked to an allocentric negative representation of their body that their sensory inputs are no longer able to update. To address this issue, this study tested the long-term efficacy of an enhanced CBT of obesity including a VR module aimed at both unlocking the negative memory of the body and modifying its behavioral and emotional correlates.
Despite some study limitations, results suggest that VR-enhanced CBT has the potential to enhance the efficacy of the standard CBT of obesity on weight-loss maintenance in the long term. However, they do not fully clarify what is the specific role of VR in the process. Future research should examine the psychological variables that moderate and mediate the effects of the VR-based approach,49,50 test carefully the explanatory validity of the ALH, and explore its links with related psychological variables such as body dissatisfaction, body checking, emotional dysregulation, perfectionism, insecure-anxious attachment, and self-esteem.51–53
Acknowledgments
A preliminary version of this paper was presented at the Medicine 2.0 ’12 conference (Boston, MA).
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Nguyen T, Lau DCW. The obesity epidemic and its impact on hypertension. Canadian Journal of Cardiology 2012; 28:326–333 [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. Journal of the American Medical Association 2012; 307:491–497 [DOI] [PubMed] [Google Scholar]
- 3.Baqai N, Wildin JH. Pathophysiology and aetiology of obesity. Medicine 2015; 43:73–76 [Google Scholar]
- 4.Martin AA, Davidson TL. Human cognitive function and the obesogenic environment. Physiology & Behavior 2014; 136:185–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moore CJ, Cunningham SA. Social position, psychological stress, and obesity: a systematic review. Journal of the Academy of Nutrition & Dietetics 2012; 112:518–526 [DOI] [PubMed] [Google Scholar]
- 6.Villarejo C, Fernandez-Aranda F, Jimenez-Murcia S, et al. Lifetime obesity in patients with eating disorders: increasing prevalence, clinical and personality correlates. European Eating Disorders Review 2012; 20:250–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Loth KA, MacLehose R, Bucchianeri M, et al. Predictors of dieting and disordered eating behaviors from adolescence to young adulthood. Journal of Adolescent Health 2014; 55:705–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeffery RW, Drewnowski A, Epstein LH, et al. Long-term maintenance of weight loss: current status. Health Psychology 2000; 19:5–16 [DOI] [PubMed] [Google Scholar]
- 9.Middleton KMR, Patidar SM, Perri MG. The impact of extended care on the long-term maintenance of weight loss: a systematic review and meta-analysis. Obesity Reviews 2012; 13:509–517 [DOI] [PubMed] [Google Scholar]
- 10.MacLean PS, Wing RR, Davidson T, et al. NIH working group report: innovative research to improve maintenance of weight loss. Obesity 2015; 23:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bray GA, Wadden TA. Improving long-term weight loss maintenance: can we do it? Obesity 2015; 23:2–3 [DOI] [PubMed] [Google Scholar]
- 12.Goldfield GS, Moore C, Henderson K, et al. Body dissatisfaction, dietary restraint, depression, and weight status in adolescents. Journal of School Health 2010; 80:186–192 [DOI] [PubMed] [Google Scholar]
- 13.Shin H, Shin JY, Liu PY, et al. Self-efficacy improves weight loss in overweight/obese postmenopausal women during a 6-month weight loss intervention. Nutrition Research 2011; 31:822–828 [DOI] [PubMed] [Google Scholar]
- 14.Byrne S, Barry D, Petry NM. Predictors of weight loss success. Exercise vs. dietary self-efficacy and treatment attendance. Appetite 2012; 58:695–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byrne S, Cooper Z, Fairburn C. Weight maintenance and relapse in obesity: a qualitative study. International Journal of Obesity 2003; 27:955–962 [DOI] [PubMed] [Google Scholar]
- 16.Santos I, Mata J, Silva MN, et al. Predicting long-term weight loss maintenance in previously overweight women: a signal detection approach. Obesity (Silver Spring) 2015; 23:957–964 [DOI] [PubMed] [Google Scholar]
- 17.Dakanalis A, Timko CA, Carra G, et al. Testing the original and the extended dual-pathway model of lack of control over eating in adolescent girls. A two-year longitudinal study. Appetite 2014; 82:180–193 [DOI] [PubMed] [Google Scholar]
- 18.Dakanalis A, Zanetti MA, Riva G, et al. Psychosocial moderators of the relationship between body dissatisfaction and symptoms of eating disorders: a look at a sample of young Italian women. European Review of Applied Psychology 2013; 63:323–334 [Google Scholar]
- 19.Dakanalis A, Zanetti AM, Riva G, et al. Male body dissatisfaction and eating disorder symptomatology: moderating variables among men. Journal of Health Psychology 2015; 20:80–90 [DOI] [PubMed] [Google Scholar]
- 20.Dakanalis A, Timko CA, Clerici M, et al. Comprehensive examination of the trans-diagnostic cognitive behavioral model of eating disorders in males. Eating Behaviors 2014; 15:63–67 [DOI] [PubMed] [Google Scholar]
- 21.Mond J, van den Berg P, Boutelle K, et al. Obesity, body dissatisfaction, and emotional well-being in early and late adolescence: findings from the Project EAT study. Journal of Adolescent Health 2011; 48:373–378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarwer DB, Wadden TA, Foster GD. Assessment of body image dissatisfaction in obese women: specificity, severity, and clinical significance. Journal of Consulting & Clinical Psychology 1998; 66:651–654 [DOI] [PubMed] [Google Scholar]
- 23.Foster GD, Wadden TA, Vogt RA. Body image in obese women before, during, and after weight loss treatment. Health Psychology 1997; 16:226–229 [DOI] [PubMed] [Google Scholar]
- 24.Palmeira AL, Branco TL, Martins SC, et al. Change in body image and psychological well-being during behavioral obesity treatment: associations with weight loss and maintenance. Body Image 2010; 7:187–193 [DOI] [PubMed] [Google Scholar]
- 25.Riva G. Neuroscience and eating disorders: the allocentric lock hypothesis. Medical Hypotheses 2012; 78:254–257 [DOI] [PubMed] [Google Scholar]
- 26.Riva G, Gaudio S. Allocentric lock in anorexia nervosa: new evidences from neuroimaging studies. Medical Hypotheses 2012; 79:113–117 [DOI] [PubMed] [Google Scholar]
- 27.Riva G. The key to unlocking the virtual body: virtual reality in the treatment of obesity and eating disorders. Journal of Diabetes Science & Technology 2011; 5:283–292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Riva G. Out of my real body: cognitive neuroscience meets eating disorders. Frontiers in Human Neuroscience 2014; 8:236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riva G, Gaudio S, Dakanalis A. I'm in a virtual body: a locked allocentric memory may impair the experience of the body in both obesity and anorexia nervosa. Eating & Weight Disorders 2013; 19:133–134 [DOI] [PubMed] [Google Scholar]
- 30.Riva G, Gaudio S, Dakanalis A. The neuropsychology of self objectification. European Psychologist 2015; 20:34–43 [Google Scholar]
- 31.Cesa GL, Manzoni GM, Bacchetta M, et al. Virtual reality for enhancing the cognitive behavioral treatment of obesity with binge eating disorder: randomized controlled study with one-year follow-up. Journal of Medical Internet Research 2013; 15:e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cooper Z, Doll HA, Hawker DM, et al. Testing a new cognitive behavioural treatment for obesity: a randomized controlled trial with three-year follow-up. Behaviour Research & Therapy 2010; 48:706–713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cooper Z, Fairburn CG, Hawker DM. (2003) Cognitive–behavioral treatment of obesity: a clinician's guide. New York: Guilford Press [Google Scholar]
- 34.Riva G, Bacchetta M, Cesa G, et al. Is severe obesity a form of addiction? Rationale, clinical approach, and controlled clinical trial. CyberPsychology & Behavior 2006; 9:457–479 [DOI] [PubMed] [Google Scholar]
- 35.Riva G, Gaggioli A, Villani D, et al. NeuroVR: an open source virtual reality platform for clinical psychology and behavioral neurosciences. Studies in Health Technology & Informatics 2007; 125:394–399 [PubMed] [Google Scholar]
- 36.Riva G, Gaggioli A, Grassi A, et al. NeuroVR 2—a free virtual reality platform for the assessment and treatment in behavioral health care. Studies in Health Technology & Informatics 2011; 163:493–495 [PubMed] [Google Scholar]
- 37.Riva G, Carelli L, Gaggioli A, et al. NeuroVR 1.5—a free virtual reality platform for the assessment and treatment in clinical psychology and neuroscience. Studies in Health Technology & Informatics 2009; 142:268–270 [PubMed] [Google Scholar]
- 38.deShazer S. (1985) Keys to solutions in brief therapy. New York: W.W. Norton [Google Scholar]
- 39.McFarland B. (1995) Brief therapy and eating disorders. San Francisco: Jossey-Bass [Google Scholar]
- 40.Butters JW, Cash TF. Cognitive-behavioral treatment of women's body image satisfaction: a controlled outcome-study. Journal of Consulting & Clinical Psychology 1987; 55:889–897 [DOI] [PubMed] [Google Scholar]
- 41.Wooley SC, Wooley OW. (1985) Intensive out-patient and residential tratment for bulimia. In Garner DM, Garfinkel PE, eds. Handbook of psychotherapy for anorexia and bulimia. New York: Guilford Press, pp. 120–132 [Google Scholar]
- 42.Leuner H. Guided affective imagery: a method of intensive psychotherapy. American Journal of Psychotherapy 1969; 23:4–21 [DOI] [PubMed] [Google Scholar]
- 43.Riva G, Molinari E. Factor structure of the Italian version of the Body Satisfaction Scale: a multisample analysis. Perceptual & Motor Skills 1998; 86:1083–1088 [DOI] [PubMed] [Google Scholar]
- 44.Slade PD, Dewey ME, Newton T, et al. Development of the Body Satisfaction Scale (BSS). Psychology & Health 1990; 4:213–226 [Google Scholar]
- 45.Riva G, Molinari E. Replicated factor analysis of the Italian version of the Body Image Avoidance Questionnaire. Perceptual & Motor Skills 1998; 86:1071–1074 [DOI] [PubMed] [Google Scholar]
- 46.Rosen JC, Srebnik D, Saltzberg E, et al. Development of a Body Image Questionnaire. Psychological Assessment 1991; 1:32–37 [Google Scholar]
- 47.Thompson MA, Gray JJ. Development and validation of a new body-image assessment scale. Journal of Personality Assessment 1995; 2:258–269 [DOI] [PubMed] [Google Scholar]
- 48.Weinfurt KP. (2000) Repeated measures analyses: ANOVA, MANOVA and HLM. In Grimm GL, Yarnold PR, eds. Reading and understanding more multivariate statistics. Washington, DC: American Psychological Association, pp. 285–316 [Google Scholar]
- 49.Pla-Sanjuanelo J, Ferrer-Garcia M, Gutierrez-Maldonado J, et al. Identifying specific cues and contexts related to bingeing behavior for the development of effective virtual environments. Appetite 2015; 87:81–89 [DOI] [PubMed] [Google Scholar]
- 50.Ferrer-Garcia M, Gutierrez-Maldonado J, Pla J, et al. Development of a VR application for binge eating treatment: identification of contexts and cues related to bingeing behavior in Spanish Italian patients. Studies in Health Technology & Informatics 2014; 199:71–75 [PubMed] [Google Scholar]
- 51.Dakanalis A, Favagrossa L, Clerici M, et al. Body dissatisfaction and eating disorder symptomatology: a latent structural equation modeling analysis of moderating variables in 18-to-28-year-old males. Journal of Psychology 2015; 149:85–112 [DOI] [PubMed] [Google Scholar]
- 52.Dakanalis A, Carrà G, Clerici M, et al. Efforts to make clearer the relationship between body dissatisfaction and binge eating. Eating & Weight Disorders 2015; 20:145–146 [DOI] [PubMed] [Google Scholar]
- 53.Dakanalis A, Carra G, Calogero R, et al. The developmental effects of media-ideal internalization and self-objectification processes on adolescents' negative body-feelings, dietary restraint, and binge eating. European Child & Adolescent Psychiatry 2015; 24:997–1010 [DOI] [PubMed] [Google Scholar]