Abstract
Objectives
To assess whether a phone-based breastfeeding intervention delivered by lactation educators influenced exclusive breastfeeding rates amongst low-income Hispanic women in the USA.
Design
Randomised two-group design
Setting
Pregnant low-income Hispanic women (298) were recruited from community health clinics in Los Angeles County (USA) and randomly assigned to either a control or an intervention group.
Methods
Data relating to the factors associated with breastfeeding were collected during the third trimester. Breastfeeding outcome data was collected at 72 hours, one month, three months, and six months postpartum.
Results
There were no differences between the groups in rates of breastfeeding initiation. There was a significant difference in the duration of exclusive breastfeeding among participants during the infant's first week of life. While not significant, after controlling for covariates and intent to breastfeed at third trimester, the duration of exclusive breastfeeding amongst all participants was, on average, longer for intervention group mothers than control group mothers. Additionally, , the intervention group mothers were more likely to report exclusive and only breastfeeding at all data points compared to the control group, and less likely to discontinue breastfeeding.
Conclusion
Findings from this study suggest that telephone-based breastfeeding interventions delivered by a lactation educator show promise as a cost-effective strategy for improving both the quantity and duration of breastfeeding among low-income Hispanic women in the USA. Intervention group mothers not only sustained breastfeeding for a longer durations, but also provided their infants with greater amounts of breast milk over these longer durations.
Keywords: Lactation education, telephone intervention, effects, low income, USA
Background
Breastfeeding significantly improves health outcomes of the breastfeeding mother and her baby. (Ip et al., 2009; Kramer and Kakuma, 2009). Health outcomes for both the breastfeeding mother and her baby are positively associated with the amount of breast milk an infant receives as well as the duration of breastfeeding (Armstrong and Reilly, 2002; Kramer and Kakuma, 2009; Raisler et al., 1999; Schwarz et al., 2009). Given the advantages associated with the amount of breast milk received and the duration of breastfeeding, major health organisations recommend that all infants be exclusively breastfed for the first six months of their life (American Public Health Association, 2007; Eidelman and Feldman-Winter, 2005). Exclusive breastfeeding is achieved when an infant from the time of birth, receives no other liquid or solid other than breast milk.
To date only 36% of women in the USA are exclusively breastfeeding at three months and 16% are exclusively breastfeeding at 6 months (Centers for Disease Control and Prevention, 2012). Rates are much lower amongst low-income populations: less than nine percent of mothers who are under the poverty line exclusively breastfeed their infants for six months, compared to 17.6% of mothers who are 350% above the poverty line (Centers for Disease Control and Prevention, 2007). Hispanics, the nation's largest minority ethnic group, have disproportionately higher poverty rates than the White population, respectively, 34% compared to 13% (DeNavas-Walt et al., 2010).
Exclusive breastfeeding duration rates are particularly low amongst low-income Hispanic women, For example, data suggest that, compared to Whites, Hispanics are less likely to sustain even one week of exclusive breastfeeding. In-hospital exclusive breastfeeding rates amongst Hispanics is only 27.9%, compared to 46% amongst Whites (Newton et al., 2009). Moreover, as early as one week postpartum, 33% of breastfeeding Hispanics feed their baby both formula and breast milk, compared to 23% of breastfeeding Whites (Lothian, 2006). Accordingly, interventions that are effective at improving breastfeeding exclusivity duration rates amongst low-income Hispanics are warranted.
Several factors that prevent Hispanics from exclusively breastfeeding their babies for six months have been identified (Gill et al., 2004). Some of these reasons, such as pain or problems with latch, are complex and require the assistance of an advanced clinician, such as an International Board Certified Consultant (IBCLC). Other reasons, such as lack of support for breastfeeding and inaccurate beliefs about breastfeeding including Los Dos, can be provided by a variety of knowledgeable healthcare professionals and paraprofessionals (Association, 2007). Los Dos means both, and is the inaccurate belief that the optimal way to feed an infant entails combining breastfeeding with formula (Bartick and Reyes, 2012).
One strategy that has been identified for improving six months exclusive breastfeeding rates is to increase the number of health care professionals and paraprofessionals who possess basic breastfeeding knowledge (United States Breastfeeding Committee, 2010). Clinical or licensed health care professionals (CLHCP) trained in basic breastfeeding knowledge can be effective at educating and supporting breastfeeding mothers. However, utilising a CLHCP to deliver ongoing breastfeeding education and support to pregnant and breastfeeding mothers may not be cost effective. Low cost breastfeeding peer counsellors are effective at delivering breastfeeding education and support to low-income Hispanic mothers (Anderson et al., 2005; Chapman et al., 2004). Peer counsellors are mothers who have previously breastfed their own child, do not hold a professional healthcare licence and have participated in training to provide them with the knowledge and skills needed to educate and support mothers with normal non-clinical breastfeeding concerns. Similar to breastfeeding peer counsellors, lactation educators (sometimes also called lactation counsellors or specialists) are also trained to provide basic education and support to breastfeeding mothers (Childbirth and Postpartum Professional Association, 2011). Lactation educators do not necessarily have to be mothers, who have previously breastfed their child, nor do they need to be CLHCP (Childbirth and Postpartum Professional Association, 2011). Given rising healthcare costs and the importance that breastfeeding knowledge and support have in promoting six months of exclusive breastfeeding, it is important to expand the pool of cost-effective individuals that are trained to educate and support breastfeeding mothers.
To date, no study has examined whether, trained lactation educators, who are not CLHCP, nor have prior breastfeeding experience can be effective at delivering breastfeeding education and support to Hispanic mothers. Exploring the efficacy of such a group could increase the pool of cost-effective individuals trained to promote breastfeeding amongst low-income Hispanic mothers.
Research suggests that breastfeeding interventions aimed at increasing breastfeeding rates should include both prenatal and postpartum education and support (Britton et al., 2007; Chapman et al., 2004; Olenick, 2006). Evidence suggests that breastfeeding interventions delivered entirely via phone by both LHCP or paraprofessionals who were trained to facilitate lactation education and support can be effective at promoting exclusive breastfeeding rates (Dennis et al., 2002; Simonetti et al., 2012; Tahir and Al-Sadat, 2013). Telephone-based interventions are especially effective amongst low-income populations as they reduce access barriers, transportation costs, and childcare costs (Galinsky et al., 1997). A few randomised controlled trial (RCT) studies provide evidence on the efficacy of trained individuals who were not clinical or licensed healthcare providers delivering a breastfeeding intervention that incorporates the telephone amongst other things as a modality for delivering education and support to low-income Hispanic mothers (Anderson et al., 2005; Chapman et al., 2004). To date, no study has explored the effectiveness of trained individuals who are not clinical or LHCP delivering interventions designed to increase the breastfeeding exclusivity rates of low-income Hispanic mothers delivered entirely using the telephone.
The purpose of this study was to evaluate the efficacy of a cost-effective intervention designed to improve six month exclusive breastfeeding rates amongst low-income Hispanic women. The specific research question that guided this study was: Can a prenatal and postpartum phone-based breastfeeding intervention delivered by trained lactation educators who are not clinical or LHCP nor have had prior breastfeeding experience, influence six month exclusive breastfeeding rates amongst low-income Hispanic women.
Methods
Participants
The study was approved by the California State University Northridge Institutional Review Board, Providence Holy Cross Medical Center Institutional Review Board and Northeast Valley Health Corporation Research Committee. A two-group randomised clinical trial design was used to evaluate the efficacy of an intervention consisting of lactation educator implemented prenatal and postpartum phone-based breastfeeding education and support versus a non-intervention control group.
Participants were recruited by case managers working at five community health clinics serving a large population of low-income Hispanics in Los Angeles County. These five community health clinics are a part of the Northeast Valley Health Corporation (NEVHC) which operates 13 community clinics in the Los Angeles area and 15 Women Infant and Children (WIC) Supplemental Nutrition Programmes. The health clinics provide prenatal care and monthly prenatal health education classes on a variety of topics, including one on breastfeeding. The WIC programmes provide monthly food vouchers, nutrition education, and breastfeeding support to women, infants and children aged five and under. Breastfeeding support includes breastfeeding classes, access to a free breastfeeding helpline, breast pumps and lactation consultant services. Although the NEVHC operated both the health clinics and WIC programmes, patients must actively enrol in the WIC programme to receive its services. Some of the NEVHC WIC clinics offered breastfeeding support and education using peer counsellors. We avoided recruiting participants from health clinics located near WIC sites that offered peer counsellor support.
From July 2011 through July 2012, 289 pregnant low-income Hispanic mothers were randomised to either the control or intervention group using computer software. Randomisation was blocked by weeks of recruitement. Control group mothers received the routine breastfeeding education and support offered by the NEVHC. Intervention group mothers received all of the services of the control group, plus a telephone-based breastfeeding intervention (described below). Inclusion criteria included: (a) 26 -34 weeks pregnant); (b) Medicaid recipient; (c) self-identified Hispanic; (d) available via telephone; and (e) not assigned to a WIC peer counsellor. Randomisation occurred before birth, though further assessment of study inclusion criteria was conducted following delivery to ensure that the following postpartum inclusion criteria were met: a) the birth of a healthy full-term singleton; b) an absence of congenital abnormality; and c) the infant was not admitted to a neonatal intensive care unit. These inclusion criteria were selected to avoid enrolling in this study participants whose babies had medical conditions that could significantly interfere with breastfeeding.
Intervention
The research assistants, who also served as lactation educators implementing the breastfeeding intervention, were not blinded with respect to the treatment groups. The study protocol prohibited research assistants from providing the control group participants with any breastfeeding education or support and also required that they use the same data collection strategy techniques when collecting data from participants in both groups. In an attempt to assign an equal number of control and intervention group participants to each research assistant/lactation educator, the assignment of mothers to lactation educators was performed in pairs such that each educator was assigned successive intervention and control mothers.
The lactation educators in this study were undergraduate students who completed a semester long lactation education course and ten hours of post course training. The lactation education course included content knowledge on the normal breastfeeding process and cultural sensitivity training. Post-course training focused on client-centred phone counselling techniques. Both the course and post training were developed and implemented by one of the project investigators, who is an International Board Certified Lactation Consultant (IBCLC) and had prior experience working in the community as both a lactation educator and a lactation consultant.
The breastfeeding intervention was developed by the project investigator who is an IBCLC. The intervention was designed to incorporate research relating to low-income Hispanic women's breastfeeding behaviour. Given that breastfeeding counselling that incorporates client-centred techniques is effective at influencing breastfeeding rates amongst low-income populations, the lactation educators utilised client-centred techniques to build initial rapport with participants prenatally as well as to implement subsequent breastfeeding intervention calls (Bignell et al., 2012).
The first six weeks postpartum is considered the critical period for establishing breastfeeding and is likely the time that a mother will need the most support and education (Gross et al., 2011). As such, the postpartum calls were implemented with greater frequency during this critical period (two calls during week one and one call each week during postpartum weeks 2– 8).
As mentioned earlier, Hispanic mothers endorse various inaccurate beliefs about breastfeeding, including Los Dos that contribute to them believing they need to feed their baby both breast milk and formula. It was anticipated that a trusted lactation educator could dispel inaccurate beliefs about the need to provide one's baby with both breast milk and formula by designing the intervention in such a way that the lactation educator, who has already established rapport with the mother prenatally, regularly and proactively reaches out during the postpartum period to the mother to inquire about her breastfeeding experience. This could therefore contribute to less supplementation and a longer duration of breastfeeding exclusivity amongst Hispanic mothers.
The intervention entailed four prenatal and seventeen postpartum phone calls (first call initiated when mothers were in the third trimester of pregnancy and the last call when mother was six months postpartum). With the exception of prenatal contacts 2 and 3, all phone contacts were to be between 5-7 minutes in duration or as long as needed if the mother reported a breastfeeding concern. Prenatal phone contact 2 and 3 were to last about 20 minutes in duration, and focused on ensuring that the intervention participant was equipped with critical breastfeeding knowledge prior to the birth of her baby. The intervention participants were also provided with the lactation educator's phone number so they could contact her more frequently if need be. On occasion, text messages were used to implement phone contacts with participants.
The main objectives of the prenatal telephone contacts were to increase the participant's motivation to initiate breastfeeding by: 1) increasing the support the participant had for initiating breastfeeding; 2) reducing the barriers or misconceptions related to breastfeeding that the participant may have had; 3) providing the participant with anticipatory guidance regarding what to expect during the first few weeks of breastfeeding.
The main objectives of the postpartum contacts were to: 1) increase support for exclusive six months breastfeeding; 2) reinforce knowledge disseminated during the prenatal phone contacts; 3) address any breastfeeding concerns that the participant might have had throughout the first six months of her breastfeeding experience; and 4) refer participants reporting breastfeeding problems beyond the lactation educator's scope of practice to an appropriate healthcare providers (e.g. paediatrician, IBCLC, primary care).
Intervention fidelity
To enhance the breastfeeding intervention's fidelity, the project investigator developed an intervention protocol, an intervention monitoring protocol, and facilitated regular meetings with the lactation educators to monitor their implementation of the intervention. The intervention protocol included: objectives for the prenatal and postpartum phone contacts, important content knowledge for the lactation educators to cover at specific prenatal and postpartum weeks and strategies to determine whether intervention participants had adequate breastfeeding knowledge. The intervention monitoring protocol included several tools to prevent the lactation educators from unintentionally deviating from the intervention protocol. Those tools included: 1) a call calendar which was created to help lactation educators keep track of when they needed to implement each of the 21 prenatal and postpartum phone contacts, 2) a unique documentation note for each of the 21 prenatal and postpartum contacts which included check off reminder boxes for all of the content that was to be covered during that particular contact.
Measurements
The research assistants utilised a phone questionnaire to collect data from the control and intervention group participants. Baseline data included variables that could potentially confound study results (Ahluwalia et al., 2012; Gill, 2009; Heck et al., 2006; Sussner et al., 2008; Piper and Parks, 1996; McDowell et al., 2008). These variables included: marital status, age, education level, household income, household size, number of hours worked per week, parity, prior breastfeeding experience, breastfeeding intentions, level of acculturation, and participation in their health clinic's prenatal breastfeeding class. To determine participants’ level of acculturation we utilised the short acculturation scale for Hispanics which has been found to be a reliable and valid instrument for identifying Hispanics who are low or high in acculturation (Marin et al., 1987).
To evaluate the efficacy of the breastfeeding intervention, research assistants collected self-reported breastfeeding data at the following postpartum periods: 72 hours, one month, three months and six months. Data on both duration rates in weeks as well as breastfeeding status at each data point were collected.
The following three categories were used to determine the participant's breastfeeding status at each data point. 1) Exclusive Breastfeeding (Labbok and Krasovec, 1990): Since birth the mother reported that she only fed her baby breast milk, meaning that her baby never received water, formula, folk remedies or other foods. 2) Breastfeeding, But Not Exclusive: The mother reported that she was still breastfeeding her baby; however, at least once since birth, her baby received water, formula, folk remedies or another food. 3) Not Breastfeeding: The mother reported that she was no longer placing her baby on her breast for any feedings during any time of the day.
Observations made when our first few enrolled participants reached the one month postpartum data point resulted in an ad hoc decision to collect data on an additional breastfeeding status category referred to as Current Exclusive Breastfeeding (Aarts et al., 2000). Similar to what Aarts et al. (2000) reported, we found that our study participants, who at the 72 hour data point had reported supplementing their baby, were inaccurately reporting at the one month postpartum data point that they were exclusively breastfeeding since birth. Aarts et al.'s (2000) Current Exclusive Breastfeeding category enables researchers to better capture data on mothers who may not meet Labbocks and Krasovec's (1990) strict definition of exclusive breastfeeding since birth, but nonetheless are feeding their baby no other fluid or foods but their breast milk at a particular time.
To determine participants’ exclusive breastfeeding duration rates in weeks at each data point, research assistants asked participants who were still breastfeeding, if they had given their baby any supplement at any time since the birth of their baby. Those who reported doing so were asked to recall the age of their baby in weeks when this first supplement was given. The data was used to calculate the exclusive breastfeeding duration rates in weeks. To determine the breastfeeding duration rates in weeks at each data point, participants were asked if they were still breastfeeding. Participants who reported that they were no longer breastfeeding were asked to recall the last date they put their baby on the breast. The data was used to calculate the breastfeeding duration rates.
Collecting data on Current Exclusive Breastfeeding enabled us to better assess our intervention's efficacy on exclusive breastfeeding rates. Given that six month exclusivity since birth is considered the optimal infant feeding method, we believed it was important to accurately capture the intervention's impact on breastfeeding that was exclusive from birth (Eidelman and Feldman-Winter, 2005). Given that it is common amongst Hispanic women to inaccurately perceive that optimal nutrition entails proving their infant with both formula and breast milk (i.e., Los Dos) we believed that it was also important to assess the intervention's impact on motivating mothers to feed their infants “only breast milk” regardless of whether it was since birth or currently.
While we did not recruit participants from WIC clinics that use peer counsellors to promote breastfeeding rates, it was possible that some participants may have switched to such a clinic after recruitment. To enable us to control for possible confounding effect that education and support provided by a WIC peer counsellor could have on our results, research assistants also collected data with respect to the amount of contact with a WIC peer counsellor, if any. At each postpartum data point, participants were asked whether they had received any education or support from a WIC peer counsellor, and if so, how many contacts and the duration in minutes of those contacts.
Statistical analyses
Participant characteristics were summarised for both groups, including age, household and work characteristics, socio-economic status, acculturation, previous experiences with breastfeeding, and information on the birth of this child. Baseline data was compared between participants in the control and intervention groups. For continuous outcomes, averages were compared between groups (means for normally distributed variables, and medians for non-normal distributions) using either the independent t-test or Mann-Whitney U tests. Categorical characteristics were compared using χ2 tests, Fisher's exact if there are two categories and Pearson's χ2 if 3+ categories. While the study was not powered to detect differences between groups, these comparisons were made to determine if there were potential covariates that may be problematic.
Survey completion, retention, and disenrollment rates were compared between groups at each data collection point (3rd trimester, 72 hours, 1 month, 3 months, and 6 months) using logistic regression. Active participants at a given time were those not lost to follow up or dis-enrolled. A mother was considered lost to follow up if she met the following criteria: the research assistant was unable to reach her at two different data points or her telephone number was disconnected. A mother was considered dis-enrolled if she met any of the following criteria: she did not meet the postpartum inclusion criteria, stopped breastfeeding, or indicated that she was no longer interested in participating in the study. Survey completion rates included the number of surveys completed by active participants. Retention rates at each data collection point were computed as the percent of active participants at a given point; participants who were dis-enrolled were not included in this comparison. The cumulative percentage of dis-enrolled participants was computed at each data collection point.
Breastfeeding status at 72 hours, 1 month, 3 months and 6 months are reported as N (%). Intent-to-treat (ITT) analyses were performed comparing Intervention to Control for these outcomes. Fisher's exact χ2 was utilised to test the difference in breastfeeding initiation rates at 72 hours. Breastfeeding status is a complicated construct, and so we examined it from three different perspectives: (1) status (not breastfeeding, breastfeeding but not exclusively, and exclusive breastfeeding; (2) only breastfeeding (exclusive + current exclusive) vs not breastfeeding 3) any breastfeeding rates (reported any breastfeeding since last asked vs not breastfeeding). Longitudinal generalised linear modelling was used to compare the rates of these outcomes across 6-months. All of the available data were included in analyses. Odds Ratios (ORs) comparing status variables between intervention and control were estimated for each time and across 6 months. For measurements of the total weeks of exclusive and any breastfeeding, the normality of the outcomes was assessed. ITT analyses were performed using t-tests to compare means for normally distributed outcomes, and the Wilcoxon/Mann-Whitney U test was used for non-normally distributed outcomes to compare medians. Reasons for discontinuing breastfeeding were explored between groups using Fisher's exact χ2 tests. Due to the ad hoc decision to add current exclusive breastfeeding, five women were not asked this item at 72 hours. We thus performed sensitivity analyses to assess if there would be a difference in results for the dichotomised Only Breastfeeding outcome at 72 hours by running analyses assigning these 5 women alternately to all Yes and all No.
To examine the dosing of the Intervention group, the number and duration of calls prenatally, postpartum and combined were as previously described. We also examined the number of calls required to reach mothers in order to implement the intervention calls. Analyses were performed using SPSS (v.21); for all analyses, a priori α = .05.
Results
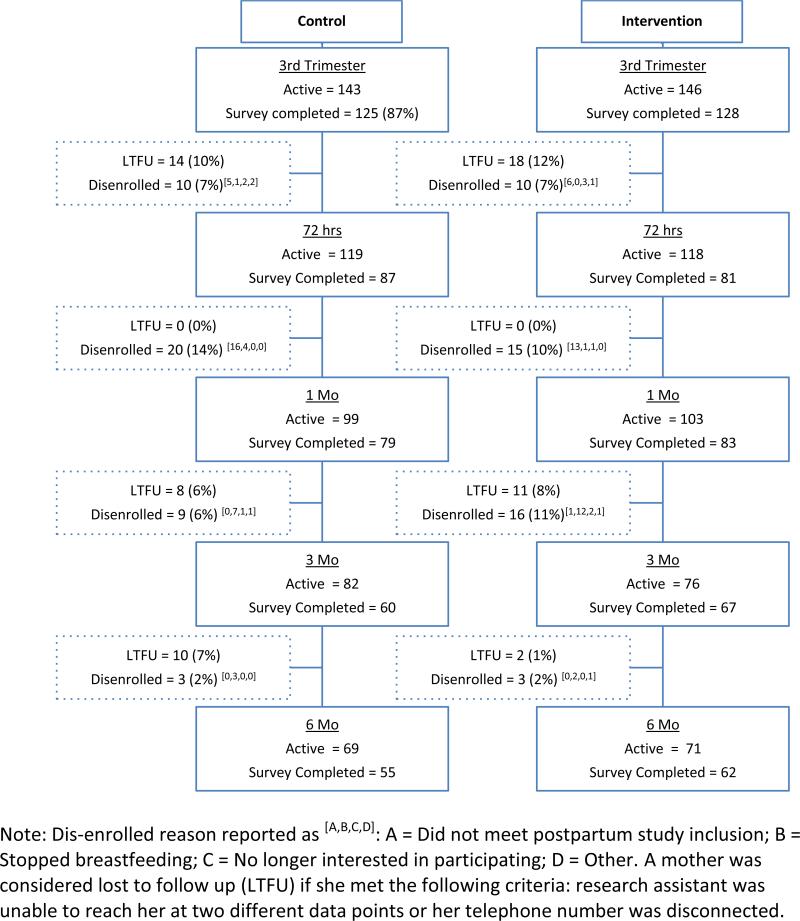
Figure 1 shows study flow by group, including: retention, active participation at each data collection point, loss to follow up (LTFU), and participants who were dis-enrolled. Survey completion rates were comparable between groups, with the exception of survey completion rate at 3 months at which 88% of the active participants in the intervention group completed the survey and 73% of the active control participants completed the survey. At 6-months 78% and 79% of Control and Intervention participants respectively were retained (not LTFU, exclusive of disenrollment), and 30% of participants had been dis-enrolled.
Figure 1.
Study flow diagram
Participant and birth characteristics are reported in Table 1. Despite randomisation, women in the Intervention group had a significantly higher intention to breastfeed (p = 0.02), thus this variable was controlled for in group comparisons. Birth characteristics of the child in this study were also largely comparable and showed no statistically significant differences between groups.
Table 1.
Study participant characteristics
| Control | Intervention | |||||||
|---|---|---|---|---|---|---|---|---|
| Mother's characteristics | N | M | SD | N | M | SD | p | |
| Week of Pregnancy at Enrollment | 109 | 29.2 | 2.4 | 111 | 29.7 | 2.5 | 0.12 | |
| Household Size (range 1-13) | 109 | 4.3 | 1.8 | 111 | 4.2 | 1.7 | 0.60 | |
| Age | 109 | 27.1 | 6.3 | 111 | 27.8 | 5.8 | 0.38 | |
| Number of Hours Work Per Week | 40 | 24.7 | 11.4 | 42 | 28.4 | 11.9 | 0.16 | |
| Annual Household Income | 58 | $18,335 | $9,991 | 64 | $20,098 | $8,273 | 0.29 | |
| Number of Children | 75 | 1.8 | 1.0 | 79 | 1.7 | 1.0 | 0.75 | |
| Acculturation | 109 | 2.1 | 1.4 | 111 | 2.0 | 1.3 | 0.49 | |
| N | % | N | % | p | ||||
| Enrolled in WIC | No | 105 | 96.3% | 104 | 93.7% | 0.28 | ||
| Yes | 4 | 3.7% | 7 | 6.3% | ||||
| Assigned a WIC Breastfeeding peer counselor | No | 3 | 2.8% | 2 | 1.8% | 0.49 | ||
| Yes | 103 | 97.2% | 107 | 98.2% | ||||
| Marital Status | Single | 47 | 43.1% | 49 | 44.1% | 0.49 | ||
| Married | 61 | 56.0% | 58 | 52.3% | ||||
| Divorced | 0 | 0.0% | 2 | 1.8% | ||||
| Separated | 1 | 0.9% | 2 | 1.8% | ||||
| Education | Some grade school | 4 | 3.7% | 7 | 6.3% | 0.44 | ||
| Completed grade school | 17 | 15.6% | 27 | 24.3% | ||||
| Some HS | 27 | 24.8% | 26 | 23.4% | ||||
| Completed HS | 41 | 37.6% | 31 | 27.9% | ||||
| Some college | 9 | 8.3% | 11 | 9.9% | ||||
| Completed College | 10 | 9.2% | 8 | 7.2% | ||||
| Some graduate school | 0 | 1 | 0.9% | |||||
| Completed graduate degree | 1 | 0.9% | 0 | |||||
| Vocational Training | No | 74 | 88.1% | 77 | 91.7% | 0.72 | ||
| Yes | 9 | 10.7% | 6 | 7.1% | ||||
| Some | 1 | 1.2% | 1 | 1.2% | ||||
| Number of other children | 0 | 2 | 2.7% | 1 | 1.3% | 0.81 | ||
| 1 | 34 | 45.3% | 40 | 50.6% | ||||
| 2 | 25 | 33.3% | 26 | 32.9% | ||||
| 3 | 9 | 12.0% | 7 | 8.9% | ||||
| 4 | 4 | 5.3% | 4 | 5.1% | ||||
| 5 | 1 | 1.3% | 0 | |||||
| 6 | 0 | 1 | 1.3% | |||||
| Breastfed prior | No | 20 | 22.5% | 12 | 13.8% | 0.10 | ||
| Yes | 69 | 77.5% | 75 | 86.2% | ||||
| N | M | SD | N | M | SD | p | ||
| Intent to breastfeed at baseline | Average | 109 | 3.8 | 1.5 | 111 | 4.3 | 1.2 | 0.02 |
| Birth data | N | % | N | % | p | |||
| Full Term Baby | No | 5 | 5.6% | 7 | 8.1% | 0.35 | ||
| Yes | 85 | 94.4% | 79 | 91.9% | ||||
| Birth defects | No | 88 | 98.9% | 86 | 100.0% | 0.51 | ||
| Yes | 1 | 1.1% | 0 | 0.0% | ||||
| NICU | No | 78 | 87.6% | 79 | 91.9% | 0.25 | ||
| Yes | 11 | 12.4% | 7 | 8.1% | ||||
| Breastfed at hospital | No | 1 | 1.3% | 1 | 1.3% | 0.74 | ||
| Yes | 79 | 98.8% | 76 | 98.7% | ||||
| Prenatal health education class | No | 27 | 36.0% | 18 | 25.4% | 0.11 | ||
| Yes | 48 | 64.0% | 53 | 74.6% | ||||
| Entire class on breastfeeding | No | 8 | 11.3% | 6 | 11.3% | 0.31 | ||
| Yes | 40 | 88.7% | 47 | 88.7% | ||||
Initiation
There were no differences in breastfeeding initiation between groups, nor was there a statistically significant difference in rate of in hospital supplementation (i.e., formula use; p = 0.51, OR =1.4), however the rate of in hospital supplementation was lower among intervention group participants (55.3%) than the control group (61.8%).
Rates of breastfeeding at each postpartum data collection point are reported in Table 2, with comparisons made within each data collection point, controlling for intent to breastfeed at third trimester.
Table 2.
Breastfeeding status at each survey: 72 hr, 1 month, 3 months, and 6 months*
| Status | Only Breastfeeding (Exclusive + Current Exclusive | Any Breastfeeding | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not Breastfeeding | Breastfeeding, Not Exclusive | Exclusive Breastfeeding | No | Yes | No | Yes | ||||||||
| N | % | N | % | N | % | N | % | N | % | N | % | N | % | |
| 72 hours | ||||||||||||||
| Control | 1 | 1.3% | 46 | 60.5% | 29 | 38.2% | 26 | 37.1% | 44 | 62.9% | 1 | 1.3% | 75 | 98.7% |
| Intervention | 0 | 0.% | 48 | 63.2% | 28 | 36.8% | 24 | 32.4% | 50 | 67.6% | 0 | 0% | 76 | 100% |
| OR | -- | -- | -- | -- | 1.13 | -- | -- | |||||||
| pGroup | 0.57 | 0.74 | 1.0 | |||||||||||
| pIntent | 0.08 | 0.09 | 0.99 | |||||||||||
| 1 month | ||||||||||||||
| Control | 6 | 8.6% | 42 | 60.0% | 22 | 31.4% | 28 | 43.1% | 37 | 56.9% | 6 | 8.6% | 64 | 91.4% |
| Intervention | 5 | 6.% | 45 | 60.8% | 24 | 32.4% | 22 | 31.4% | 48 | 68.6% | 5 | 6.% | 69 | 94.0% |
| OR | -- | -- | 1.19 | 1.17 | 1.55 | -- | 1.46 | |||||||
| pGroup | 0.97 | 0.23 | 0.58 | |||||||||||
| pIntent | 0.40 | 0.21 | 0.16 | |||||||||||
| 3 months | ||||||||||||||
| Control | 3 | 5.4% | 40 | 71.4% | 13 | 23.2% | 27 | 50.0% | 27 | 50.5% | 3 | 5.4% | 53 | 94.6% |
| Intervention | 1 | 1.8% | 37 | 67.3% | 17 | 30.9% | 19 | 35.8% | 34 | 64.2% | 1 | 1.8% | 54 | 98.2% |
| OR | -- | -- | 3.52 | 4.86 | 1.68 | -- | 3.87 | |||||||
| pGroup | 0.35 | 0.20 | 0.25 | |||||||||||
| pIntent | 0.14 | 0.06 | 1.0 | |||||||||||
| 6 months | ||||||||||||||
| Control | 7 | 14.3% | 38 | 77.6% | 4 | 8.2% | 34 | 81.0% | 8 | 19.0% | 7 | 14.3% | 42 | 85.8% |
| Intervention | 3 | 5.6% | 39 | 72.2% | 12 | 22.2% | 30 | 60.0% | 20 | 40.0% | 3 | 5.6% | 51 | 94.4% |
| OR | -- | -- | 2.69 | 7.54 | 2.56 | -- | 2.81 | |||||||
| pGroup | 0.060 | 0.06 | 0.17 | |||||||||||
| pIntent | 0.340 | 0.06 | 0.18 | |||||||||||
Note: Status included three categories: not breastfeeding, non-exclusive breastfeeding, and exclusive breastfeeding; OR are adjusted for Intent and reference category for Status is not breastfeeding. Reference category for dichotomised Breastfeeding (which combines exclusive breastfeeding and only breastfeeding) and Any Breastfeeding is No. OR at 72 hours was not calculable as there were no mothers in the intervention group not breastfeeding; Low N's in other cells for Status make the OR unstable.
Any breastfeeding
There were no significant differences between groups in the any breastfeeding rates at any of the postpartum data points. When examined across time, there was a trend for group in any breastfeeding (OR 2.1, p = 0.08); after controlling for a priori covariates the OR remained similar (OR = 1.6).
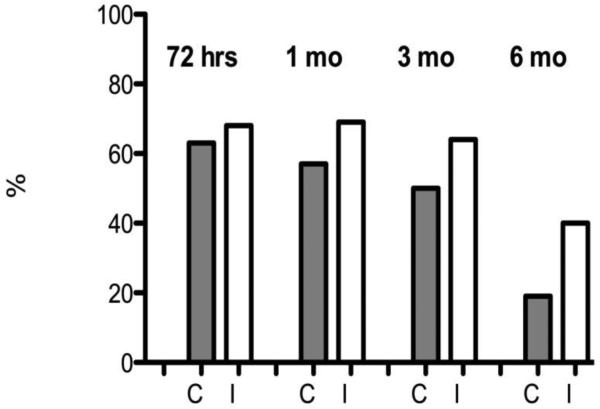
Only breastfeeding (exclusive + current exclusive)
Only breastfeeding (exclusive + current exclusive) rates were consistently higher in the intervention group than the control group; though not statistically significant at any point, there was a trend at 6 months (p = 0.06). As can be seen in Figure 2, while the differences in not breastfeeding and only breastfeeding rates were similar at 72 hrs and 1 month, they begin to diverge at 3 months with a monotonic increase in the difference in exclusive breastfeeding across time: OR72hrs = 1.1, OR1mo = 1.6, OR3mo = 1.7, OR6mo = 2.6) between intervention and control mothers. Sensitivity analyses performed for breastfeeding outcome at 72 hours had OR ranging from 1.00 – 1.30 (all p's > 0.45).
Figure 2.
Only breastfeeding vs. not breastfeeding across time
When examined across time, there was a trend for group in only breastfeeding (OR = 1.5, p = 0.11). After controlling for a priori covariates (age, martial status, education, acculturation, other children and prior breastfeeding experience), the OR increased for only breastfeeding to 1.7 (p = 0.08), indicating that across 6 months, the intervention group was much more likely to report exclusive or currently breastfeeding than control mothers, even when controlling for initial intent to breastfeed. Initial intent to breastfeed was a significant predictor of exclusive breastfeeding across 6 months (p < .001).
Status of breastfeeding
Similar monotonic trends were seen in the status variable. By 6 months, 22% of intervention mothers reported exclusive breastfeeding versus 8% of control mothers; this was coupled with a difference in those reporting not breastfeeding, where 14% of control mothers versus 6% of intervention mothers reported not breastfeeding. Across time, intervention mothers were less likely to discontinue breastfeeding, as well as report exclusive breastfeeding at a greater rate than control mothers. When compared to those reporting not breastfeeding, the OR's for breastfeeding exclusively increase from 1.2 at 1 month, to 4.9 at 3 months to 7.5 at 6 months, after adjusting for initial intent. And when compared to those reporting not breastfeeding, the OR's for breastfeeding (not exclusively) increase from 1.1 at 1 month, to 3.5 at 3 months to 2.7 at 6 months. Thus, it appears that across time, intervention mothers were less likely to discontinue breastfeeding, as well as to report exclusive breastfeeding at a greater rate than control mothers.
Breastfeeding duration rates in weeks
Table 3 reports the duration of any and exclusive breastfeeding in weeks. Duration of exclusive breastfeeding was an average of 7.8 ± 11.1 weeks for the Intervention group, three weeks more on average compared with the control group (4.8±8.7 weeks; p = 0.22 for median comparison). Median comparisons were made due to the large skew in the data; the median of both groups = 0 in a comparison of the median lengths (IQ range = 2 and 0 for intervention and control, respectively). Therefore, a group comparison was made for women who reported > 0 weeks exclusive breastfeeding. For women who reported exclusive breastfeeding for more than 0 weeks, there was a statistically significant difference between groups. Women in the intervention group reported an average of 20.2 weeks of breastfeeding, while women in the control group reported an average of 13.7 weeks. This was a large difference (Cohen's D = .7). This data was not skewed, so t-tests were the best choice of statistics. There were no differences in duration of partial breastfeeding between groups, either the total sample or those who breastfed > 0 weeks.
Table 3.
Duration of breastfeeding (weeks)
| Control | Intervention | T-test | Mann-Whitney U | |||||
|---|---|---|---|---|---|---|---|---|
| N | M | SD | N | M | SD | p-value | p-value | |
| Total Sample | ||||||||
| Duration of Exclusive Breastfeeding | 63 | 4.8 | 8.7 | 57 | 7.8 | 11.1 | 0.102 | 0.42 |
| Duration of Any Breastfeeding | 46 | 20 | 9.2 | 39 | 20.7 | 8.9 | 0.716 | 0.22 |
| Women > 0 weeks duration | ||||||||
| Duration of Exclusive Breastfeeding | 22 | 13.7 | 9.8 | 22 | 20.2 | 8.3 | 0.024 | 0.11 |
| Duration of Any Breastfeeding | 13 | 22.4 | 7.6 | 9 | 21.7 | 8.6 | 0.839 | 0.66 |
Summary of the call data within the intervention group
There was a large range in the number of calls prenatally (1 – 7) and postpartum (0 – 27). On average intervention group mothers received 1.5 prenatal calls lasting about 9.2 minutes and 4.9 postpartum calls lasting about 8 minutes.
Discussion
Breastfeeding interventions that have been previously evaluated include several features that make it difficult to compare the results of our intervention with the current literature. These features include: the mode of delivery (e.g., phone, home visits, clinic visits), credentials and training of the individuals implementing the intervention, whether they include both prenatal and postpartum contacts and intensity of the intervention. Researchers have classified interventions as low-intensity if they include only prenatal education or if postpartum support is delivered primarily through the phone. High-intensity interventions include at least 3 contacts, provide both prenatal and postpartum support, and deliver most of the contacts in person (Chapman et al., 2004).
To date, there have been two RCT studies that examined the efficacy of breastfeeding intervention that included several features similar to our study's intervention and targeted low-income Hispanics in the USA (Anderson et al., 2005, Chapman et al., 2004). Similar to our study, these interventions were implemented by non-licensed, non-clinically trained individuals, included both prenatal and postpartum education and support and incorporated phone-based contacts. Chapman et al.'s (2004) RCT was effective at improving three month any breastfeeding rates. Andersons et al.'s (2005) RCT, which incorporated a greater number of contacts than Chapman's, was effective at improving six months exclusive breastfeeding rates. While both of these interventions incorporated phone-based contacts, they were high-intensity intervention as they also included in-hospital and home visit contacts.
Our study was the first RCT targeting low-income Hispanics in the USA that evaluated the efficacy of non-licensed non-clinical trained individuals delivering prenatal and postpartum education and support entirely via the phone.
Influence on breastfeeding outcomes
The primary objective of our study was to evaluate whether a prenatal and postpartum phone-based breastfeeding intervention delivered by trained lactation educators who are not clinical or LHCP nor have had prior breastfeeding experience can influence six month exclusive breastfeeding rates amongst low- income Hispanic women. Given that six month exclusivity since birth is considered the optimal infant feeding method, we believed it was important to accurately capture the intervention's impact on breastfeeding that was exclusive since birth (Eidelman and Feldman-Winter, 2005). As it is common amongst Hispanic women to inaccurately perceive that optimal nutrition entails providing their infant with both formula and breast milk, we believed that it was also important to assess the intervention's impact on motivating mothers to feed their infants “only breast milk” regardless of whether it was since birth or currently.
The trends in exclusive and only breastfeeding (exclusive and current exclusive ) observed in our study suggests that a low-intensity intervention implemented by trained lactation educators, such as the one evaluated in this study, show promise as a cost-effective strategy for increasing breastfeeding exclusivity rates amongst low-income Hispanic women in the USA.
Findings suggest that this intervention was effective at significantly improving exclusive breastfeeding duration rates amongst participants who refrained from supplementing their baby with any fluid or solids during his or her first week of life (Cohens D= .7). Amongst this subgroup of participants, the control group participants, exclusively breastfed for only 13 weeks, whereas intervention group mothers, breastfed exclusively for 22 weeks. These findings differ from prior research that has found that when breastfeeding mothers avoid supplements in the early postpartum weeks, they are significantly more likely to reach 6 months exclusivity benchmarks. Intervention group participants in this subgroup exclusively breastfed 9 weeks longer when compared to control group participants, suggesting that mothers still need continued support and education to maintain this behaviour even when they remain exclusively breastfeeding past the first postpartum week.
Amongst all of the study participants, the intervention shows some promise with respect to improving exclusivity rates. While not statistically significant, a higher proportion of intervention group mothers left the hospital exclusively breastfeeding their baby when compared to control group mothers, 44.7% compared to 38.2% respectively. With the exception of 72 hours exclusivity rates, a higher proportion of intervention group breastfeeding mothers reported that they were exclusively breastfeeding their baby at all data points. Indeed, at 6 months 22.2% of the intervention group participants compared to 8.2% of control group participants reported exclusive breastfeeding since birth.
In addition to trends observed amongst the intervention group mothers’ exclusive breastfeeding rates, trends were also observed amongst the intervention group mothers’ only breastfeeding rates (exclusive and current exclusive). Findings suggest that across 6 months, intervention group participants were more likely to report breastfeeding without supplements of other liquids or solids. At 6 months, 40% of the intervention group participants reported only breastfeeding (exclusive and current exclusive), compared to 19% of control group participants. This suggests that the intervention shows promise with respect to reducing the propensity to supplement breastfeeding with other foods or liquids amongst low-income Hispanics.
While clear cut conclusions cannot be made regarding the trends observed, some implications can be drawn from these findings. Perhaps the frequent and continuous proactive phone contacts from a knowledgeable and supportive individual of similar ethnicity enabled the intervention mothers to trust the messages communicated by the lactation educator. In particular, it appears that the education and support provided by the lactation educator may have enabled the intervention group mothers to better withstand pervasive cultural pressure to supplement breastfeeding with formula during their babies’ first six months of life. When a breastfeeding mother supplements her baby with any fluid or solid other than breast milk, it gives her body the message to produce less breast milk. Over time, supplementation can result in the mother not producing enough breast milk to fully nourish her baby, creating a cycle which ends in quitting breastfeeding sooner.
Limitations
This study had several limitations. Multiple factors can influence a woman's decision to initiate breastfeeding, avoid supplementing breastfeeding with formula and sustain exclusive breastfeeding until her baby reaches six months. To control for some of these variables we used a randomised controlled trial as well as collected data on several variables that have been found to be associated with breastfeeding behaviour. Nonetheless, it is not possible to control for all variables that may influence breastfeeding behaviour. Another limitation of this study is that it was not blinded, and research assistants who collected data also served as lactation educators for this study. Research assistants were trained on the importance of not providing the control group with information or support on breastfeeding as well as using the same data collection protocol when administering surveys to participants in both groups. Nonetheless, given the rapport lactation educators developed with intervention group participants, intervention participants may have felt it was more socially desirable to report that they were still exclusively breastfeeding. Another limitation to our study was that it was underpowered. We did conduct an a priori power analysis, and extended our recruitment period by an entire year. However, in order to avoid recruiting participants into our study who were assigned a WIC peer counsellor, and complete our study in the allotted funding period, we did not recruit our target sample and thus were underpowered. Another limitation to our study is that lactation educators had no prior experience implementing lactation education and support. It is likely that over the duration of our study the lactation educators became more competent in implementing breastfeeding education and support, and therefore intervention group mothers enrolled in the first month of our study may have received a slightly less effective intervention that those enrolled in later months of the study.
Future research
While some implications can be drawn from this study, future research on both the value of lactation educators and low-intensity breastfeeding interventions that are delivered via phone are needed. Future research should examine the efficacy of this intervention with a larger sample size, more experienced lactation educators and utilise different staff than the lactation educators to collect data from study participants. While some implications may be drawn regarding the potential role that a trained lactation educator who is not a clinical or LHCP nor has prior breastfeeding experience has in promoting six month exclusive breastfeeding amongst low-income Hispanics, more research in this area is needed. Findings from the study provide some evidence suggesting that low-intensity breastfeeding interventions that incorporate both prenatal and postpartum proactive education and support and use a telephone as the only mode of contact may be effective at promoting six month exclusive breastfeeding amongst low-income Hispanics. However, more research in this area is warranted.
Conclusions
Currently, low-income Hispanics in the USA often endorse the belief that to adequately nourish a baby during its first 6 months of life, it is necessary to feed the baby both formula and breast milk. This belief is likely to contribute to the current low exclusive breastfeeding rates amongst low-income Hispanics. The findings from this study suggest that a prenatal and postpartum telephone-based breastfeeding intervention delivered by a trained lactation educator, who is not a clinical or LHCP nor has had prior personal breastfeeding experience, shows promise as a cost-effective strategy for improving both the quantity and duration of breastfeeding amongst low-income Hispanics. It appears that this intervention may have been effective at creating a trust relationship between lactation educators and mothers, thereby influencing mothers’ perceptions that breast milk on its own is adequate nourishment for a baby's first six months. Intervention group mothers not only sustained breastfeeding for longer durations than control group mothers, but also provided their infants with greater amounts of breast milk over these longer durations.
Given the promising findings of this study, additional research utilising trained lactation educators who are not clinical or LHCP nor have prior breastfeeding experience could provide more robust evidence to expand the pool of cost-effective individuals trained to educate and support mothers on the normal breastfeeding process. Additional research may also provide stronger evidence supporting the use of low-intensity phone only breastfeeding interventions amongst low-income Hispanics. Given the importance of adopting cost-effective strategies, the use of lactation educators and low-intensity interventions are important strategies to be considered for improving six month exclusive breastfeeding rates.
Acknowledgements
We gratefully acknowledge the assistance of Elio Spinello for technical assistance with development of the data input sheets used by the research assistants to collect data throughout the study period. The willing assistance Northeast valley Health corporation administration and staff for assistance in recruitment of participants into our research study. We thank the participants, for their participation in the study. We especially want to acknowledge the project Lactation Consultant Terry Gass, the Project coordinator Lauren Menor and 4 research assistants (Jazmine Arista, Jocceline Hernandez, Byanka Melgar and Mayra Morales) for their commitment and dedication to ensuring the success of the research study and Genevieve Dunton for research design consultation.
Funding
Funding for this study was provided by the Centers for Medicare and Medicaid Services (CMS). The statement contained in this report are solely those of the authors and do not necessarily reflect the views and policies of CMS. The authors assume responsibility for the accuracy and completeness of the information contained in this report.
The work was supported by the Centers for Medicare and Medicaid Services (Grant Number 1HOCMS330803); USDA/NIFA Hispanic-Serving Institutions (HSI) Education Grants Program; NIH-funded Research Infrastructure in Minority Institutions (RIMI) Program, and California State University Sponsored Projects.
Footnotes
Conflict of Interest
No conflict of interest for this study exists.
Contributor Information
Merav W Efrat, Department of Health Sciences California University Northridge, USA 18111 Nordhoff Street Northridge, CA 91330-8285.
Salvador Esparza, Department of Health Sciences California University Northridge, USA 18111 Nordhoff Street Northridge, CA 91330-8285.
Sherri G Mendelson, Providence Holy Cross Medical Center 15031 Rinaldi St. Mission Hills, CA 91345.
Christianne J. Lane, Department of Preventive Medicine Division of Biostatistics Keck School of Medicine, University of Southern California 2001 Soto St 2nd Floor, SSB #202X Los Angeles, CA 90089-9234, Clane@usc.edu
References
- Aarts C, Kylberg E, Hörnell A, Hofvander Y, Gebre-Medhin M, Greiner T. How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. International Journal of Epidemiology. 2000;29(6):1041–1046. doi: 10.1093/ije/29.6.1041. [DOI] [PubMed] [Google Scholar]
- Ahluwalia IB, D'Angelo D, Morrow B, McDonald JA. Association between Acculturation and Breastfeeding among Hispanic Women Data from the Pregnancy Risk Assessment and Monitoring System. Journal of Human Lactation. 2012;28(2):167–173. doi: 10.1177/0890334412438403. [DOI] [PubMed] [Google Scholar]
- Anderson AK, Damio G, Young S, Chapman DJ, Pérez-Escamilla R. A randomized trial assessing the efficacy of peer counseling on exclusive breastfeeding in a predominantly Latina low-income community. Archives of Pediatrics & Adolescent Medicine. 2005;159(9):836–841. doi: 10.1001/archpedi.159.9.836. [DOI] [PubMed] [Google Scholar]
- American Public Health Association . A call to action on breastfeeding: a fundamental public health issue. Washington, DC: 2007. [June 12, 2014]. Policy Number 200714. Available at: http://www.apha.org/advocacy/policy/policysearch/default.htm?id=1360. [Google Scholar]
- Bartick M, Reyes C. Las dos cosas: an analysis of attitudes of Latina women on non-exclusive breastfeeding. Breastfeeding Medicine. 2012;7(1):19–24. doi: 10.1089/bfm.2011.0039. [DOI] [PubMed] [Google Scholar]
- Bignell WE, Sullivan E, Andrianos A, Anderson AK. Provision of Support Strategies and Services Results from an Internet-Based Survey of Community-Based Breastfeeding Counselors. Journal of Human Lactation. 2012;28(1):62–76. doi: 10.1177/0890334411429112. [DOI] [PubMed] [Google Scholar]
- Chapman DJ, Damio G, Young S, Perez-Escamilla R. Effectiveness of breastfeeding peer counseling in a low-income, predominantly Latina population: a randomized controlled trial. Archives of Pediatrics & Adolescent Medicine. 2004;158(9):897. doi: 10.1001/archpedi.158.9.897. [DOI] [PubMed] [Google Scholar]
- Childbirth & Postpatum Professional Association [June 12, 2014];CAPPA position paper: The lactation eductor's role in providing breastfeeding information and support. 2011 Available at: http://www.cappa.net/documents/position-paper-cle.pdf.
- Centers for Disease Control and Prevention [June 12, 2014];Provisional breastfeeding rates by socio-demographic factors, among children born in 2007. 2007 Available at: http://www.cdc.gov/breastfeeding/data/NIS_data/2007/socio-demographic_any.htm.
- Centers for Disease Control and Prevention . Breastfeeding report card. Atlanta, GA.: 2012. [June 12, 2014]. Available at: http://www.cdc.gov/breastfeeding/data/reportcard/reportcard2012.htm. [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. [June 12, 2014];Income, poverty, and health insurance coverage in the United States: 2009. Report, U.S. Department of Commerce Economics and Statistics Administration. 2010 Available at: http://www.census.gov/prod/2010pubs/p60-238.pdf.
- Denni CL, Hodnett E, Gallop R, Chalmers B. The effect of peer support on breast-feeding duration among primiparous women: a randomized controlled trial. Canadian Medical Association Journal. 2002;166(1):21–28. [PMC free article] [PubMed] [Google Scholar]
- Eidelman A, Feldman-Winter L. From the American Academy of Pediatrics: Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics. 2005;115(2):496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- Gill SL. Breastfeeding by Hispanic women. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2009;38(2):244–252. doi: 10.1111/j.1552-6909.2009.01013.x. [DOI] [PubMed] [Google Scholar]
- Gill SL, Reifsnider E, Mann AR, Villarreal P, Tinkle MB. Assessing infant breastfeeding beliefs among low-income Mexican Americans. The Journal of Perinatal Education. 2004;13(3):39. doi: 10.1624/105812404X1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross SM, Resnik AK, Nanda JP, Cross-Barnet C, Augustyn M, Kelly L, Paige DM. Early postpartum: A critical period in setting the path for breastfeeding success. Breastfeeding Medicine. 2011;6(6):407–412. doi: 10.1089/bfm.2010.0089. [DOI] [PubMed] [Google Scholar]
- Hauck FR, Thompson JM, Tanabe KO, Moon RY, Vennemann MM. Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis. Pediatrics. 2011;128(1):103–110. doi: 10.1542/peds.2010-3000. [DOI] [PubMed] [Google Scholar]
- Heck KE, Braveman P, Cubbin C, Chávez GF, Kiely JL. Socioeconomic status and breastfeeding initiation among California mothers. Public Health Reports. 2006;121(1):51. doi: 10.1177/003335490612100111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinig MJ, Follett JR, Ishii KD, Kavanagh-Prochaska K, Cohen R, Panchula J. Barriers to compliance with infant-feeding recommendations among low-income women. Journal of Human Lactatio. 2006;22(1):27–38. doi: 10.1177/0890334405284333. [DOI] [PubMed] [Google Scholar]
- Ip S, Chung M, Raman G, Chew P, Magula N, DeVine D, Lau J. Evidence report/technology assessment. Vol. 153. Agency for Healthcare Research and Quality; Rockville, MD: 2009. Breastfeeding and maternal and infant health outcomes in developed countries. 2007. [PMC free article] [PubMed] [Google Scholar]
- Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. [June 12, 2014];Cochrane Database of Systematic Reviews. 2002 doi: 10.1002/14651858.CD003517. Available at: http://onlinelibrary.wiley.com/doi/10.1002/14651858.CD003517/pdf/standard. [DOI] [PubMed]
- Labbok M, Krasovec K. Toward consistency in breastfeeding definitions. Studies in Family Planning. 1990:226–230. [PubMed] [Google Scholar]
- Lothian JA. Listening to Mothers: Take Two. The Journal of perinatal education. 2006;15(4):41. doi: 10.1624/105812406X151411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin G, Sabogal F, Marin BV, Otero-Sabogal R, Perez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic Journal of Behavioral Sciences. 1987;9(2):183–205. [Google Scholar]
- McDowell MM, Wang CY, Kennedy-Stephenson J. Breastfeeding in the United States: findings from the national health and nutrition examination surveys, 1999-2006. NCHS data briefs, no. 5. National Center for Health Statistics; Hyattsville, MD: 2008. [June 12, 2014]. Available at: http://www.cdc.gov/nchs/data/databriefs/db05.htm. [PubMed] [Google Scholar]
- Newton KN, Chaudhuri J, Grossman X, Merewood A. Factors associated with exclusive breastfeeding among Latina women giving birth at an inner-city baby-friendly hospital. Journal of Human Lactation. 2009;25(1):28–33. doi: 10.1177/0890334408329437. [DOI] [PubMed] [Google Scholar]
- Piper S, Parks PL. Predicting the duration of lactation: evidence from a national survey. Birth. 1996;23(1):7–12. doi: 10.1111/j.1523-536x.1996.tb00454.x. [DOI] [PubMed] [Google Scholar]
- Schwarz EB, Ray RM, Stuebe AM, Allison MA, Ness RB, Freiberg MS, Cauley JA. Duration of lactation and risk factors for maternal cardiovascular disease. Obstetrics and gynecology. 2009;113(5):974. doi: 10.1097/01.AOG.0000346884.67796.ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simonetti V, Palma E, Giglio A, Mohn A, Cicolini G. A structured telephonic counselling to promote the exclusive breastfeeding of healthy babies aged zero to six months: A pilot study. International Journal of Nursing Practice. 2012;18(3):289–294. doi: 10.1111/j.1440-172X.2012.02040.x. [DOI] [PubMed] [Google Scholar]
- Sussner KM, Lindsay AC, Peterson KE. The influence of acculturation on breast-feeding initiation and duration in low-income women in the US. Journal of Biosocial Science. 2008;40(5):673–696. doi: 10.1017/S0021932007002593. [DOI] [PubMed] [Google Scholar]
- Tahir NM, Al-Sadat N. Does telephone lactation counselling improve breastfeeding practices?: A randomised controlled trial. International Journal of Nursing Studies. 2013;50(1):16–25. doi: 10.1016/j.ijnurstu.2012.09.006. [DOI] [PubMed] [Google Scholar]
- United States Breastfeeding Committee . Core competencies in breastfeeding care for all health professionals. Washington, DC: 2010. [June 12, 2014]. Available at: http://www.usbreastfeeding.org/HealthCare/TrainingforHealthCareProfessionals/CoreCompetencies/tabid/225/Default.aspx. [Google Scholar]