Abstract
Objective:
To determine the prediction value of disorder of consciousness scale (DOCS) for consciousness recovery after traumatic brain injury (TBI) leading to coma.
Methods:
This is a descriptive-cross-sectional study of the correlation between the level of patients’ consciousness in the first and second weeks and the first 2 months after traumatic brain injury, using DOCS scale.
Results:
The findings of the present study showed that the sensitivity and specificity of DOCS in determining individual’s consciousness after first week and two months after injury are 66% and 41% respectively, and regarding DOCSU2 the corresponding values were 94% and 50% (p=0.001).
Conclusion:
Passage of time is one of the most significant factors in predicting the resumption of consciousness in patients with brain injury, and more accurate results are expected following the acute phase. However, the application of disorder of consciousness scale could be of a great help to patients’ families and rehabilitation staff in regard to providing a better services to meet the patients” future needs.
Key Words: Disorder of consciousness scale (DOCS), Traumatic brain injury (TBI), Coma recovery, Consciousness
Introduction
Head injury is considered as one of the most important issues in general health, with regard to the needs of patients to intensive medical care, long-term rehabilitation and social-mental support. Following head injuries, individuals develop consciousness, sensory, behavioral, cognitive, and physical disorders and become comatose. Consciousness disorder includes a changing sequence and is named according to the time and changes in patient’s condition and symptoms [1]. Comatose patients either improve to regain their consciousness within the first 2 to 4 weeks or they are diagnosed with vegetative state, chronic coma and minimal state of consciousness [2]. Most brain injuries do not lead to death and the patients survive for a prolonged period. Therefore, the rehabilitation program after head injury improves individual’s condition and makes life more satisfiable for the patient in proportion to the level of injury determined by disorder of consciousness scale (DOCS). Meanwhile, predicting the results after head injury could be of assistance in designing effective and special rehabilitation programs for each patient [3,4].
Most researchers have made efforts to study factors that can affect outcome in patients after coma. Some of these factors include age, Glasgow Coma Scale (GCS), pupil reaction and eye movements, CT-scan findings, duration of post-traumatic amnesia, brainstem dysfunction, and intracranial pressure (ICP) or a combination of all these factors, for example patients’ age at the time of accident is one of such prognosis factors, as increasing age leads to higher mortality rate. Despite the application of radiological techniques and clinical observations during the first days after injury, it is not yet possible to accurately predict the result for adopting the best and efficient rehabilitation treatment [1,5,6].
Frequent observations of neurological status within weeks and months is the best way for predicting the outcome. However, this could only indicate the probability of death or chance of survival and also the rate of disability, as they have a low accuracy in determining the recovery, partial disability or complete disability [7]. GCS in the first 24 hours after head injury can predict the vital signs and functional results during the second and third day after the accident. Scores less than 8 could raise the mortality increase to 35%, and the values less than 7 during early phase indicate the probability of gaining optimum performance in 12% of cases [5-8]. The coma depth and duration are determinant of various motor and cognitive recovery aspects.
Various scales are used in patients to evaluate and follow the recovery process. These include disorder of consciousness scale (DOCS), coma recovery scale-revised, sensory modality assessment rehabilitation technique (SMART), Wessex head injury matrix (WHIM) and specific assessment tests. It should be mentioned that specific scales used to assess consciousness disorders including coma, vegetative response and minimal consciousness state were first proposed in 1990 in relation to rehabilitation discussions and by neural rehabilitation experts, who had identified the GCS limitations in detecting neurobehavioral sub-performance changes, developed these scales [8-11]. Pape claimed that DOCS could predict the patient’s neurobehavioral performance over time [11]. They concluded that DOCS score in the second to sixth weeks after injury could predict the state of patient’s consciousness during the subsequent third, fifth and twelfth months [11].
Patients studied in most centers across the world received rehabilitation treatments in post-acute wards subsequent to discharge from intensive care units [12]. Considering that DOCS scale is among the newest scales used worldwide, and the rehabilitation of these patients is costly and time-consuming, the following research was conducted to determine the relationship between DOCS score in the first two weeks after the injury and the level of patient’s consciousness in the second month after concussion.
Materials and Methods
Study population
This is a descriptive cross-sectional study using DOCS scale to determine the correlation between the level of patients’ consciousness in the first and second weeks after the injury and their consciousness level in the first 2 months after concussion. The study included 30 comatose patients admitted to Intensive Care Unit of Shahid Rajaee Hospital affiliated with Shiraz University of Medical Sciences, Shiraz Iran for 3 months. We included adult (>18 years) patients with traumatic brain injury with GCS Less than 8, stable medical condition approved by the physician, and admission not longer than one week. Those who were discharged from the hospital before the second week after admission were excluded from the study. We also excluded those who lacked of face to face contact or telephone access after assessments and hospital discharge and those with full consciousness before completing assessments. The study protocol was approved by institutional review board (IRB) and ethics committee of Shiraz University of Medical Sciences and the patients’ guardians.
Study Protocol
Having fulfilled the criteria to enter the study and obtaining permissions from the ward physician and nurse in charge, the patient’s neurobehavioral performance was assessed by using DOCS scale two times within a week. DOCS scale subsets studied comprised social communication, taste and swallowing, olfactory, vestibular and proprioceptive, touch, auditory, vision and awareness. The first assessment was conducted at the end of the first week and the second evaluation was carried out at the end of the second week and the consciousness level scores were recorded in each case. By the end of the second month after injury, the patient’s consciousness was assessed by asking two questions of patient’s family, on the phone. Of 30 patients investigated, 6 died in second month after the injury and before reaching the third phase of the study. The remaining 24 cases survived until the end of the research. To determine the consciousness state of the patients, the following questions were asked of patients’ families [10]:
1. Was patient able to have proper interaction and appropriate communications, such as asking others to open the door, moving their bed or being helped to carry out carrying out tasks?
2. Was patient able to use objects correctly, such as knowing how to use the glass, tooth brush and comb?
3. Did patients show behaviors implying their awareness of their surroundings? Did they know where they were, what time of the day it was, or how many days they stayed at home?
Positive response to any of these questions showed that the patient was conscious. Thus based on these criteria, patients studied were considered as conscious, unconscious or dead by the end of the second month after the injury.
Statistical analysis
The Statistical Package for Social Science, SPSS for Windows, version 15.0 (SPSS, Chicago, IL) was used for data analysis. The data analysis was performed using nonparametric ANOVA and Sensitivity and Specificity tests. According to the existing conditions, patients presented as conscious, unconscious or dead in the second months after the injury. These states were assessed by considering the differences between DOCS scores, using repeat Kruskal-Wallis test. A two-sided p-value less than <0.05 was considered statistically significant.
Results
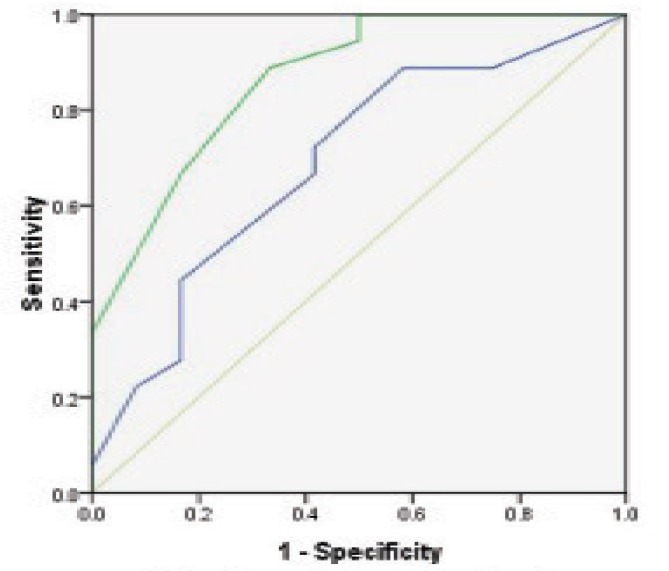
Overall we included 30 patients suffering from severe traumatic brain injury. The mean age of the patients was 38.66 ± 12.87 (range 18-50) years. Among the patients there were 26 (86.7%) men and 4 (13.3%)women. The results of the study are summarized in Table 1. Regarding DOCS scores, significant difference was found between the first and second weeks after injury in three groups of conscious, unconscious and dead subjects (p=0.001). According to the test, sensitivity and specificity of DOCS1 in determining individual’s consciousness two months after injury were 66% and 41% respectively, and corresponding values for sensitivity and specificity of DOCS2 were 94% and 50% (p=0.001) (Figure 1). As demonstrated in Figure 2, the area under the curve and sensitivity and specificity were used to assess the prediction power of consciousness state by criterion score changes in the first and second weeks after injury. The sensitivity and specificity of DOCS1 and DOCS2 in predicting the states of individual’s consciousness two months after the injury were72% and 50% respectively (p=0.009).
Table 1.
ISS and total number of injuries according to age groups
| Consciousness State after 2 Months | Mean | Minimum | Maximum | Number | P -value | |
|---|---|---|---|---|---|---|
| DOCS1 | Conscious | 25.91 ± 8.76 | 4.4 | 35.20 | 18 | 0.045 |
| Unconscious | 24.46 ± 10.55 | 4.4 | 33.7 | 6 | ||
| Dead | 15.21 ± 9.31 | 4.4 | 26.9 | 6 | ||
| DOCS2 | Conscious | 37.41 ± 5.52 | 21.9 | 45.3 | 18 | 0.001 |
| Unconscious | 29.95 ± 12.69 | 4.4 | 37.9 | 6 | ||
| Dead | 10.96 ± 11.30 | 4.4 | 31.9 | 6 |
Fig. 1.
Area under the curve for DOCS1 and DOCS2 in 24 patients with severe traumatic brain injury.
Fig. 2.
Area under the curve for changes in DOCS1 and DOCS2 in 24 patients with severe traumatic brain injury
Discussion
In studies carried out by Giacino and Trott [1] and Kazanis [3] it was concluded that GCS score in the first 24 hours was crucial in predicting vital signs, and the results of performance could be predicted in the first 2-3 days after the injury. Thus, scores lower than 8 indicated 35% probability of death, and the chance of reaching optimum performance was 12% if the scores lower than 7 persisted for a week [1,3]. However, there has been no report on predicting the outcome of head injury by using DOCS scale in acute phase. The results of present research is in agreement with those of several studies using other criteria to predict consciousness, unconsciousness or death of the subjects during the first few days following head injury [4-7]. Thus consciousness is likely to recur if the DOCSU score in the first and second weeks are 25.3 and 26.9 respectively. Giacion [13] indicated that the probability of least mortality and the highest performance results were due to the GCS score between 6 to 8 and less than 24 hours of coma. There was no data found on the prediction of patient performance results using assessing criteria of consciousness in acute phase.
Our results were consistent with those of Pape et al., [8]. In this research, DOCS scale was used in the second, third, fourth, fifth and sixth weeks to predict consciousness state in the fourth, eighth and twelfth months after injury. The sensitivity and specificity of this scale in determining the recovery level after 4 months were 86% and 83% respectively, whereas it had 88% sensitivity and 92% specificity 12 months following injury. In this study, the area under the curve indicated that the sensitivity and specificity for DOCSU2 test in determining the patient’s consciousness state during the second week were 94% and 50% respectively, which were higher the respective values of 66% and 41% in the first week (p=0.001). It seems that the variety of scales derived from the tests decreases with higher physiologic stability and consciousness of patients over time. Hence, the scores obtained in the second week are better predictors of consciousness state than those of the second month after injury. There are no other studies reported on the predictability of the outcome of head injuries by consciousness state scores. According to Pape et al., [9] research the predictive value of DOCS1 in fourth, eighth and twelfth months after the injury, indicated that the ratio of sensitivity and specificity tests in relation to recovery and failure of gaining consciousness were 87% and 88%, respectively. In this context, the changes in baseline of stage 5 and DOCS1-2 were the best indicators for predicting the times of gaining back consciousness in the eighth and twelfth months after the injury. The changes of DOCS1-2 ratios in twelfth month after injury indicated that the DOCS assessments were correctly categorized between 83% and 97%. Moreover, the highest balanced and predictability ratio was obtained between assessments made in the first and second weeks of the eighth month after injury.
The study of the area under the curve showed that significant changes in sensitivity and specificity of DOCSU1-2 were 72% and 50% respectively. Generally, the greater the consciousness level between the first and second week, the faster is recovery. However, further studies are required to determine the sustainability of the consciousness level beyond the second week of head injury
In conclusion, passage of time is one of the most significant factors in predicting consciousness recovery in comatose patients with brain injury, and more accurate results could be expected over time. However, using DOCS could be of great help to patients’ families and rehabilitation staff in regard to covering patients’ need.
Funding/Support
This study was financially supported by Shiraz University of Medical Science (Grant number 5159).
Conflict of Interest: None declared.
References
- 1.Giacino TJ, Trott CT. Rehabilitative management of patients with disorders of consciousness: Grand rounds. J Head Trauma Rehabil. 2004;19(3):254–65. doi: 10.1097/00001199-200405000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Masson F, Thicoipe M, Mokni T, Aye P, Erny P, Dabadie P. Aquaitaine Group for Severe Brain Injury Study. Epidemiology of traumatic comas: a prospective population-based study. Brain Inj. 2003;17(4):279–93. doi: 10.1080/0269905021000030805. [DOI] [PubMed] [Google Scholar]
- 3.Kazanis I. CNS injury research; reviewing the last decade: methodological errors and a proposal for a new strategy. Brain Res Brain Res Rev. 2005;50(2):377–86. doi: 10.1016/j.brainresrev.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 4.Lippert-Grüner M, Wedekind C, Klug N. Outcome of prolonged coma following severe traumatic brain injury. Brain Inj. 2003;17(1):49–54. doi: 10.1080/0269905021000010230. [DOI] [PubMed] [Google Scholar]
- 5.Duff D. Review article: altered states of consciousness, theories of recovery, and assessment following a severe traumatic brain injury. Axone. 2001;23(1):18–23. [PubMed] [Google Scholar]
- 6.Sternbach GL. The Glasgow coma scale. J Emerg Med. 2000;19(1):67–71. doi: 10.1016/s0736-4679(00)00182-7. [DOI] [PubMed] [Google Scholar]
- 7.Majerus S, Gill-Thwaites H, Andrews K, Laureys S. Behavioral evaluation of consciousness in severe brain damage. Prog Brain Res. 2005;150:397–413. doi: 10.1016/S0079-6123(05)50028-1. [DOI] [PubMed] [Google Scholar]
- 8.Pape TL, Senno RG, Guernon A, Kelly JP. A measure of neurobehavioral functioning after coma. Part II: Clinical and scientific implementation. J Rehabil Res Dev. 2005;42(1):19–27. doi: 10.1682/jrrd.2004.03.0033. [DOI] [PubMed] [Google Scholar]
- 9.Pape TL, Heinemann AW, Kelly JP, Hurder AG, Lundgren S. A measure of neurobehavioral functioning after coma. Part I: Theory, reliability, and validity of Disorders of Consciousness Scale. J Rehabil Res Dev. 2005;42(1):1–17. doi: 10.1682/jrrd.2004.03.0032. [DOI] [PubMed] [Google Scholar]
- 10.Giacino JT, Kalmar K, Whyte J. The JFK Coma Recovery Scale-Revised: measurement characteristics and diagnostic utility. Arch Phys Med Rehabil. 2004;85(12):2020–9. doi: 10.1016/j.apmr.2004.02.033. [DOI] [PubMed] [Google Scholar]
- 11.Pape TL, Tang C, Guernon A, Lundgren S, Blahnik M, Wei Y, et al. Predictive value of the Disorders of Consciousness Scale (DOCS) PM R. 2009;1(2):152–61. doi: 10.1016/j.pmrj.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Amy C, Zagorski B, Chan V, Parsons D, Vander Laan R, Colantonio A. Acute Care Alternate-Level-of-Care Days Due to Delayed Discharge for Traumatic and Non-Traumatic Brain Injuries. Healthc Policy. 2012;7(4):41–55. [PMC free article] [PubMed] [Google Scholar]
- 13.Giacino JT, Kezmarsky MA, DeLuca J, Cicerone KD. Monitoring rate of recovery to predict outcome in minimally responsive patients. Arch Phys Med Rehabil. 1991;72(11):897–901. doi: 10.1016/0003-9993(91)90008-7. [DOI] [PubMed] [Google Scholar]