Abstract
Traumatic basal ganglia hematoma is a rare condition defined as presence of hemorrhagic lesions in basal ganglia or adjacent structures suchas internal capsule, putamen and thalamus. Bilateral basal ganglia hematoma are among the devastating and rare condition. We herein report a 28-year old man, a victim of car-car accident who was brought to our surgical emergency room by immediate loss of consciousness and was diagnosed to have hyperdense lesion in the basal ganglia bilaterally, with the presence of right parietal epidural hematoma. Craniotomy and epidural hematoma drainage were considered, associated to conservative management of gangliobasal traumatic contusions. On day 7 the patient had sudden neurologic deterioration, cardiac arrest unresponsive to resuscitation. Management of these lesions is similar to any other injury in moderate to severe traumatic injury. The use of intracranial pressure monitoring must be guaranteed.
Key Words: Traumatic brain injury, Cerebral contusion, Basal ganglia hemorrhage, Neurotrauma
Introduction
Traumatic brain injury (TBI) can be referred as a silent epidemic which remains a major cause of disability and mortality worldwide leading to high healthcare expenses [1]. During TBI many primary lesions of the cranial vault and its contents may occur. One of these injuries are brain contusion. Traumatic basal ganglia hematoma is a rare condition defined as presence of hemorrhagic lesions in basal ganglia or adjacent structures suchas internal capsule, putamen and thalamus [2]. Previous reports have demonstrated that the incidence of basal ganglia hemorrhage after closed head injury is approximately 3% in population studies while autopsy studies have reported an incidence of 10-12% [3-5]. Although the exact mechanism of injury leading to basal ganglia hematoma remains unclear, it is postulated that shearing of lenticulostriate or anterior choroidal blood vessels secondary to severe acceleration deceleration injury could be the possible mechanism in most cases [2,5].
Previous reports have demonstrated that most of the cases with isolated basal ganglia hemorrhage have good outcome [3]. However they can occur with other intracranial pathologies including diffuseaxonal injury, cerebral contusion, and subdural or extraduralhematoma. Bilateral basal ganglia hemorrhage associated with extradural hematoma is extremely rare condition being reported rarely [5-8]. We herein report a case of bilateral basal ganglia hemorrhage after closed traumatic brain injury associated with extradural hematoma.
Case Report
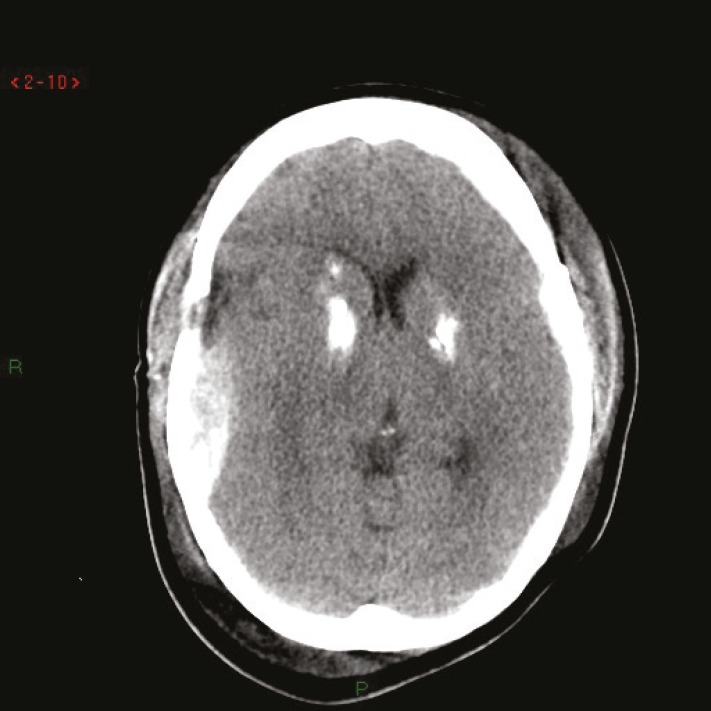
A 28-year old man, merchant, who suffered an accident while driving a two-wheeled vehicle, being hit by a car wheel in rapid motion was brought to our surgical emergency room by immediate loss of consciousness. There was no history of any substance abuse, previous illnesses or bleeding diathesis; not receiving any regular medication. Patient was not diabetic and hypertensive before the accident. On examination, the Glasgow score at admission was 6 (M:4; V:1; E:1). The pupils were 4 mm bilaterally reacting to light. Bilateral limb movements were the same. Hemopneumothorax was identified. All other parameters were normal. The pulse and blood pressure were normal. The patient was intubated and underwent mechanical ventilation. Brain CT-scan revealed a hyperdense lesion in the basal ganglia bilaterally, with the presence of right parietal epidural hematoma. Basal cisterns were obliterated (Figure 1). Craniotomy and epidural hematomadrainage were considered, associated to conservative management of gangliobasal traumatic contusions. The patient was transferred to intensive care unit and receiving derivative treatment (mannitol and hypertonic saline). Also he was given antibiotics and phenytoin. Patient continued ventilator support, with subsequent tracheostomy on day 6. Nasogastric feeding was started gradually. On day 7 the patient had sudden neurologic deterioration, cardiac arrest unresponsive to resuscitation.
Fig. 1.
CT Brain Scan showing a bilateral gangliobasalhemorraghe and a right epidural hematoma
Discussion
TBI is a major public health problem and is the leading cause of mortality, morbidity and disability in children and young adults, especially young men (15-35 years). Internationally, the socioeconomic cost of managing contusion is of high impact, in the U.S. alone, over 1.7 million people suffer TBI each year (one of it’s the main features). In severe TBI, patient can experience mental health and/or medical post- acute consequences, representing only half of the problem, the long-term implications of patients with TBI are substantial, especially among teenagers and young adults, whose brains continue to mature and develop [1].
Focal brain injury is defined as a localized damage as a laceration, bruising and hematoma, whichoccurs in the presence or absence of an opening including a skull fracture caused by mechanical impact itself [2]. From focal brain injuries, concussions are one of the findings in the context of most common traumas, being present in up to 31% of initial imaging studies (brain CT) of patients with TBI. It is reported that bruising occurred in 89% of examined postmortem brains. Cerebral contusion is a type of traumatic focal brain injury resulting from the direct loading and often occurs in the absence of widespread injury, indicating that these represent focal areas of subpial hemorrhage induced by trauma and edema, stopping the microvasculature. Pure concussions are quite common, finding in 8% of all TBI and 13 % to 35 % of serious injuries [2,3].
The vast majority of concussions occur in the frontal and temporal lobes, although they can occur almost anywhere, including the cerebellum and brainstem. It has also been established that most of the hits that cause concussions are back of the head, the majority of concussions caused by backlash affecting the frontal and temporal lobes. It has been established that any intracranial contusion, and other focal lesions such as hematoma or cerebral laceration falls within the category of severe TBI [4], at this point we disagree, because is usually to observe patients with concussions in the context of a mild TBI.
Brain contusions with gangliobasal location are rare. Gangliobasal traumatic contusions are rarely been described in the literature [3-8]. It has been proposed that brain contusions in gangliobasal location and traumatic origin are usually small, multiple and are located mainly in the lentiform nucleus and the external capsule. In a patient with bilateral basal ganglia concussion commitment of the lateral branches of the perforating arteries of the middle cerebral artery was proposed [5]. Other authors have suggested that in these lesions rupture of the anterior choroidal artery occurs. On the other hand it has been postulated that traumatic dissection of the middle cerebral artery causes bleeding and infarction of the basal ganglia and thalamus [7].
Recently Jain and colleagues [5] reported a38-year oldfullyconsciousmale, whopresentedwith bilateral basal gangliahaematoma and extradural hematoma. The patient was also undergone craniotomy and hematoma evacuation [5]. Another recent report by Kaushal et al., [6] included a 42-year old male with isolated bilateral (mirror-image) traumatic basal ganglia bleed. Some other similar reports [9,10] exist in the literature. However the precise management and outcome is yet to be identified because of rarity of the condition [11].
Management of these lesions is similar to any other injury in moderate to severe traumatic injury. The use of intracranial pressure monitoring must be guaranteed. Surgical options include drainage and stereotactic guidance, ultrasound-guided aspiration and craniotomy, with increased risk of neural injury by the approach.
Conflict of Interest: None declared.
References
- 1.Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9(4):231–6. doi: 10.1038/nrneurol.2013.22. [DOI] [PubMed] [Google Scholar]
- 2.Boto GR, Lobato RD, Rivas JJ, Gomez PA, de la Lama A, Lagares A. Basal ganglia hematomas in severely head injured patients: clinicoradiological analysis of 37 cases. J Neurosurg. 2001;94(2):224–32. doi: 10.3171/jns.2001.94.2.0224. [DOI] [PubMed] [Google Scholar]
- 3.Katz DI, Alexander MP, Seliger GM, Bellas DN. Traumatic basal ganglia hemorrhage: clinicopathologic features and outcome. Neurology. 1989;39(7):897–904. doi: 10.1212/wnl.39.7.897. [DOI] [PubMed] [Google Scholar]
- 4.Macpherson P, Teasdale E, Dhaker S, Allerdyce G, Galbraith S. The significance of traumatic haematoma in the region of the basal ganglia. J Neurol Neurosurg Psychiatry. 1986;49(1):29–34. doi: 10.1136/jnnp.49.1.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain SK, Sundar IV, Sharma V, Prasanna KL, Kulwal G, Tiwari RN. Bilateral large traumatic basal ganglia haemorrhage in a conscious adult: a rare case report. Brain Inj. 2013;27(4):500–3. doi: 10.3109/02699052.2013.765597. [DOI] [PubMed] [Google Scholar]
- 6.Kaushal R, Kataria R, Gupta A, Sinha V. Traumatic bilateral (mirrorimage) basal gangliableed. The Indian Journal of Neurotrauma. 2011;8(2):109–110. [Google Scholar]
- 7.Moriya T, Tagami R, Furukawa M, Sakurai A, Kinoshita K, Tanjoh K. A case of traumatic hematoma in the basal ganglia that showed deterioration after arrival at the hospital. Acta Neurochir Suppl. 2013;118:147–9. doi: 10.1007/978-3-7091-1434-6_27. [DOI] [PubMed] [Google Scholar]
- 8.Jang KJ, Jwa CS, Kim KH, Kang JK. Bilateral Traumatic Hemorrhage of the Basal Ganglia. Journal of Korean Neurosurgical Society. 2007;41(4):272–274. [Google Scholar]
- 9.Yanaka K, Egashira T, Maki Y, Takano S, Okazaki M, Matsumaru Y, et al. Bilateral traumatic hemorrhage in the basal ganglia: report of two cases. No Shinkei Geka. 1991;19(4):369–73. [PubMed] [Google Scholar]
- 10.Kimura M1, Sobata E, Suzuki S, Nonogaki Y, Iwabuchi T. Traumatic hematoma in the basal ganglia (caudate) with favorable prognosis: report of two cases. No Shinkei Geka. 1994;22(2):155–8. [PubMed] [Google Scholar]
- 11.Kumar S, Jha D, Abbey P, Mishra V, Handa A. Outcome of Traumatic Basal Ganglia Hemorrhage. Internet J Neurosurg. 2009;6(1) [Google Scholar]