Abstract
Objective:
To compare outcome of patients with burns covering less than 15% of total body surface area(TBSA) undergoing early excision and grafting or delayed skin grafting.
Method:
This was a non-randomized clinical trial including 54 patients with less than 15% TBSA burn referring to Ghotboddin Hospital of Shiraz. They were assigned to two study groups, each group including 27 patients: the early excision and grafting group (EEG group) and the delayed grafting group (DG group). Patients were followed postoperatively for 6 months. Hospital stay, graft success rate, itching score and scar formation during 6 months of follow-up were recorded and compared between two study groups.
Results:
During the study 1 patient was lost to follow-up in early excision and grafting group. Baseline characteristics were comparable between two study groups. The graft success rate was significantly higher in those patients who underwent early excision and grafting when compared to delayed grafting group (96.88% vs. 92.88%; p=0.033). However the length of hospital stay, itching and scar scores were comparable between two study groups after 6 months of follow-up.
Conclusion:
In patients with burns covering less than 15% TBSA, early excision and grafting is associated with higher graft success rates compared to the delayed excision and grafting. How ever length of hospital stay, itching and scar formation is comparable between the two techniques.
Key Words: Deep burns, Early excision and grafting, Delayed grafting, Itching score, Scar formation
Introduction
Burns are amongst the most devastating injuries that leave not only physical deformity but also psychosocial harm, especially in places like the face and hand [1-3].Scar formation and itching are two of the most important complication which are difficult to manage in patients with deep burns. Scar formation is the definite phenomena following deep burns in which the healing usually takes 3 weeks or more. The Scars that follow deep burns can be minimized by appropriate surgical management during the first 2 weeks of injury [4]. In the surgical approach to deep burn wounds (deep second and third degree burns), two distinguished techniques are applied. In the first and oldest technique a more conservative approach is implemented by routine wound care until the shedding of the scar and the formation of granulation tissue, after which skin grafting of the burned and unhealed area can be applied. This technique consumes more time for the granulation tissue that is appropriate for the skin grafting, to form. In this chronic process patients will be more susceptible to scar formation. In the second technique, scar tissue is excised during the first days post burn (preferably in the first 2 weeks) and auto grafted simultaneously when the patient becomes stable [early excision and grafting (EEG)] [5]. Yet the optimal time for the EEG is not a consensus. In today’s practice, wounds that are unlikely to achieve spontaneous closure in about 3 weeks are excised and grafted. The estimation by the surgeon on whether or not a partial thickness burn will heal in less than 3 weeks,is approximately 70% accurate in equivocal cases, whereas this estimation by the surgeon, is usually considered as the indication for EEG [6].Theoretically both techniques have some benefits, yet very little data was found to document the superiority of one technique over the other in a population with small size burns, so our objective was to compare the newly rekindled approach with the more conservative approach in order to better clarify their benefits and disadvantages in patients with less than 15% of total body surface area (TBSA) burns.
Materials and Methods
Patients
This was anon-randomized clinical trial being performed during a 1-year period from September 2012 to September 2013 in Ghotbodin hospital, level I burn center in southern Iran affiliated with Shiraz University of Medical Sciences. The study protocol was approved by both the institutional review board (IRB) and the medical ethics committee of Shiraz University of Medical Sciences and all the participants gave their informed written consents before inclusion in the study. This clinical trial is registered with the Iranian Clinical Trials Registry (IRCT2013092313880N2). Our terms for inclusion in the study were second and third degree burns covering less than 15% of TBSA with an age limitation of 6 months-65 years, and our exclusion criteria was having associated diseases like diabetes and cardiac diseases, scars from previous burn injuries and having connective tissue disorders. From these patients, 54 met the inclusion criteria.
Group Allocation
The patients were assigned to two study groups; the early excision and grafting group (EEG group) and the delayed grafting group (DG group) based on their own choice and consent. Those who had been referred to our center less than 14-day post-injury were considered for EEG group. Overal l27 patients met the criteria for inclusion in EEG group. Those who did not have consent for EEG and those who were referred to the hospital more than 14 days post- injury were considered as DG group which included 27 patients.
Intervention and follow-up
In EEG group, patients were operated after being stabilized during the first 14 days after injury. In the operating room with sterile conditions and under generalized anesthesia the dead tissue (Scar) was excised until reaching an appropriate bed for grafting. The debrided area was then covered with a partial- thickness meshed or non-meshed (sheet) skin taken from the patient’s healthy skin of the thighs at the same stage. The dressing was then removed on the 5th postoperative day unless signs of infection (such as abnormal discharge, high grade fever, changes in general condition and etc.) were observed, in which the dressings were changed sooner. Patients were visited weekly in the first month and then every month for the next 5 months. In DG group, patients had their dressings changed 1-2 times a day with topical antibiotics including silver sulfadiazine and mafenide acetate. Nutrition was emphasized and intravenous antibiotics were started for patients in whom signs of infection or positive cultures were seen (as mentioned for EEG group). The decision for operation was made after the formation of granulation tissue as a good bed for grafting. For DG group, in the same operating conditions as EEG group, excess granulation tissue was first removed until reaching a suitable bed for grafting and then the operation followed in a similar a manner as EEG group. In the post-operative visits, progression of graft intake, infections, contracture and deformities were monitored and managed. The variables that were measured and compared amongst the two groups included: degree of scar formation, graft intake and the hospitalization time. A successful graft intake was considered as one that has a pink color and is attached to the basis of the grafted area firmly. For assessing the itch score the 5-D itch scale was used. According to this scale, each patient is given a score from 1 to 5 for each of the five following parameters: duration, degree, direction, disability and distribution. The overall score of each patient can range from 5 (no pruritus) to 25 (severe pruritus) [7]. Scar evaluation was done using the Vancouver scale. This index scores the scars based on four parameters which include: vascularity, pigmentation, pliability and height of scar tissue. Each patient receives a score ranging from 0 to 13, 0 indicating complete recovery and 13 indicating severe scaring [8].
Statistical Analysis
The statistical analysis was done using the SPSS software version 11.0 (SPSS Inc., Chicago, IL, USA). The Mann-Whitney U test was used to compare the parametric data and the Chi-square test was used to compare the qualitative data among the two groups. The results are demonstrated as mean±SD and proportions as appropriate. A two-tailed p-value of less than 0.05 was considered statistically significant.
Results
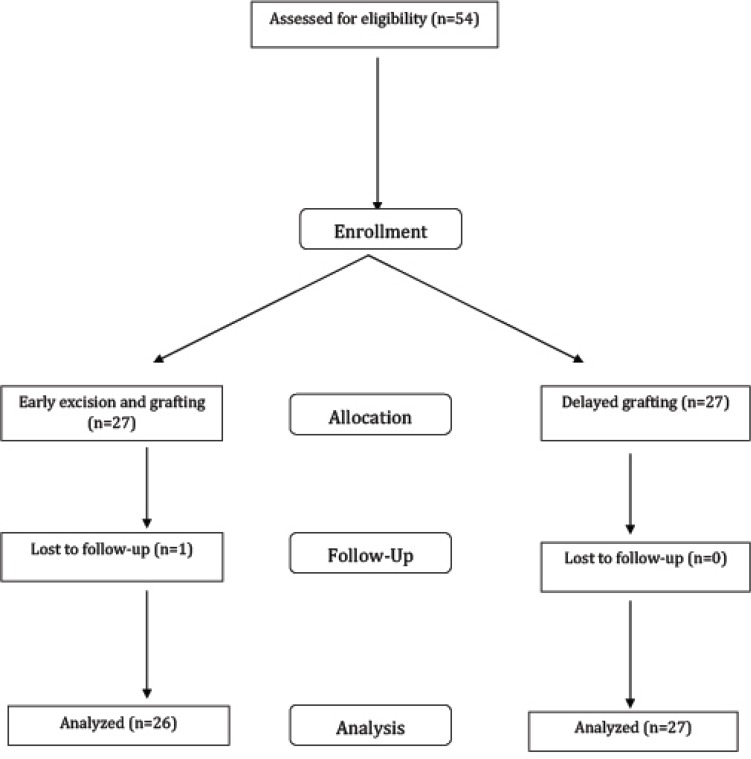
From the initial 54 patients included in the study, 1 was lost to follow-up from EEG group. Thus the final number of patients included in the study was 53 patients (26 in EEG group and 27 in DG group). The flow diagram of the patients is demonstrated in Figure 1.
Fig. 1.
CONSORT flow diagram of the study
The baseline characteristics of the patients are summarized in Table 1. There was no significant difference between two study groups regarding the demographic information as well as baseline clinical characteristics. The baseline characteristics of the wounds were comparable between two study groups. We found that the graft success rate was significantly higher in EEG group when compared to DG group (96.8±5.6 vs. 92.8±7.5; p=0.033). The duration of the hospital stay was comparable between two study groups. In the same way, the itch score was comparable between two study groups after 6-month of follow-up. Scare assessment using the Vancouver scale in the two groups along the 6 months of follow-up, showed that in EEG group,20 patients (76.9%) had complete recovery, while in group 2, 18 patients (66.7%) had complete recovery. Overall the two groups did not have any significant difference (p=0.393). Table 2 compares the study outcome between two groups.
Table 1.
Baseline characteristics of 53 patients with burns who underwent early excision and grafting or delayed grafting
| EEG group (N=26) | DG group (n=27) | p -value | |
|---|---|---|---|
| Age (years) | 21.9 ± 16.5 | 20.1 ± 14.4 | 0.789 |
| Sex | |||
| Men (%) | 16 (61.5%) | 16 (59.3%) | 0.865 |
| Women (%) | 10 (38.5%) | 11 (40.7%) | |
| Burn type | |||
| Type II (%) | 17 (65.3%) | 15 (55.5%) | 0.086 |
| Type III (%) | 6 (34.7%) | 12 (44.5%) | |
| Hospital stay (days) | 7.92 ± 4.4 | 9.38 ± 8.7 | 0.654 |
| Burn surface (TBSA) | 7.92 ± 6.1 | 6.59 ± 4.8 | 0.668 |
| Surgery surface size (TBSA) | 6.3 ± 4.19 | 5.29 ± 4.1 | 0.395 |
Table 2.
The 6-month surgical outcome of 53 patients with burns who underwent early excision and grafting or delayed grafting
| EEG group (N=26) | DG group (n=27) | p -value | |
|---|---|---|---|
| Hospital stay (days) | 7.92 ± 4.4 | 9.38 ± 8.7 | 0.654 |
| Graft success rate (percentage) | 96.8 ± 5.6 | 92.8 ± 7.5 | 0.033 |
| Itch score | 8.61 ± 10.4 | 8.9 ± 10.4 | 0.977 |
| Scar score | 0.38 ± 0.89 | 0.55 ± 0.93 | 0.393 |
Discussion
Early excision and grafting has become the standard treatment for deep burn injuries [9] with the rational that it decreases bacteremia and inflammatory mediators (by early removal of the burned skin and simultaneous wound coverage), thus decreasing the chances of sepsis and multi-organ failure and death as indicated by some studies [10,11]. The procedure requires experience and training especially for estimating the depth of the burn. An underestimation of the burn depth with unwanted delayed spontaneous healing can lead to more scarring, on the other hand an overestimation and EEG can lead to excess removal of healthy tissue and iatrogenic injury. Estimation of the wound is quite difficult as indicated by Goodwin et al. where in their study 46% of the initial wound depth estimations were erroneous [12].
The pioneer of the concept of EEG was cope et al., [13], meanwhile the interest in EEG was rekindled by the introduction of the tangential excision by Janzekovic in 1970 [1,14]. Many benefits are associated with this approach including: reduction of patient hospital stay due to early closure of the wound, bacterial colonization of the wound, virtually eliminating the pain that’s associated with the burned portion by early grafting, promoting quicker healing of the wound and decreased hospital costs [14-17]. On the other hand the approach does have some disadvantages including: the excessive removal of healthy tissue during escharectomy due to erroneous estimation of burn depth, especially if performed on the third to fifth day, also the longer operation time due to the concomitant escharectomy and skin grafting [12].
In the traditional approach patients do have prolonged hospital stays and are more prone to problems like joint contractures and hypertrophic scars due to the prolonged process of wound healing, increased hospital costs, more painful dressing changes and increased psychological stress [11].Yet some authors have shown no circumstantial differences in mortality [14], cosmetic and functional outcomes in the EEG compared to the more conservative approaches, but as surgeons have become more experienced in the approach of EEG better functional and appearance outcomes have been resulted [15,18-22].
In our study the patients were evaluated based on burn size, operated surface size, hospital stay, graft success, itching score and scar formation during a 6 month period. The patients all had less than 15% total body surface area burns. They were otherwise healthy, so mortality was not considered as a factor. The results of our study was in coherence with the study by Saaiq et al., [23]. In their study, 120 patients who underwent EEG and DG, were evaluated in a two year period. In result they also documented better graft take, as one of the ultimate goals in treating any patient with burn injuries [19,24], in the EEG group. In a Meta-analysis by Yee Siang Ong et al., [11] in 2005, they studied 6 randomized controlled trials regarding the comparison of EEG and DG. They concluded that hospital stay is significantly reduced in the group that had early excision and grafting. Hospital stay have been shown to decrease in other studies using the EEG approach [14], our study did not show a better outcome in hospital stay. This is probably due to the fact that unlike other studies, our patients all suffered minor sized burns (less than 15% of total body size), as a result they did not have prolonged hospital stays to contribute to a meaningful difference among the two groups. Although, in our study, the scare score did show better results in group 1 in comparison to group 2 (0.38±0.89 vs. 0.55±0.93), but it was statistically insignificant. This was the same with the itch score in which better results were documented in group 1 but these differences were statistically insignificant. This finding could be due to the fairly small population size that was selected for the study.
Our results were also supported by other studies that documented better results after EEG [10,14,25- 29], although these studies were all in patients with large sized burns thus making them differ in some of their results.
This study has some limitations including the small population size and the non-randomized nature of the study; moreover some confounding elements have not been taken into consideration like burns depth and the cause of the initial injury and also the preoperative condition of the patients who received the DG, which could have affected the results. Studies with larger sample populations should be designed in patients with different burn sizes, in order to better clarify the advantage or disadvantage of the EEG approach in these groups.
In conclusion, early excision and grafting has become a standard operation that is performed dealing with most deep dermal burns, our study supports the superiority of the approach in graft success rates when dealing with patients who suffer less than 15% TBSA burns. Although better outcome was also documented in hospital stay, itch score and the scar score, these results were not statistically significant.
Conflict of interest: None declared.
Note
Clinical Trial Registry: This trial is registered with the Iranian Clinical Trial Registry (IRCT2013092313880N2).
References
- 1.Druery M, Brown TL, Muller M. Long term functional outcomes and quality of life following severe burn injury. Burns. 2005;31(6):692–5. doi: 10.1016/j.burns.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Pallua N, Kunsebeck HW, Noah EM. Psychosocial adjustments 5 years after burn injury. Burns. 2003;29(2):143–52. doi: 10.1016/s0305-4179(02)00238-3. [DOI] [PubMed] [Google Scholar]
- 3.Wiechman SA, Ptacek JT, Patterson DR, Gibran NS, Engrav LE, Heimbach DM. Rates, trends, and severity of depression after burn injuries. J Burn Care Rehabil. 2001;22(6):417–24. doi: 10.1097/00004630-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Wrigley M, Trotman BK, Dimick A, Fine PR. Factors relating to return to work after burn injury. J Burn Care Rehabil. 1995;16(4):445–50. doi: 10.1097/00004630-199507000-00012. discussion 4. [DOI] [PubMed] [Google Scholar]
- 5.Janzekovic Z. A new concept in the early excision and immediate grafting of burns. J Trauma. 1970;10(12):1103–8. [PubMed] [Google Scholar]
- 6.Mohammadi AA, Bakhshaeekia AR, Marzban S, Abbasi S, Ashraf AR, Mohammadi MK, et al. Early excision and skin grafting versus delayed skin grafting in deep hand burns (a randomised clinical controlled trial) Burns. 2011;37(1):36–41. doi: 10.1016/j.burns.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Elman S, Hynan LS, Gabriel V, Mayo MJ. The 5-D itch scale: a new measure of pruritus. Br J Dermatol. 2010;162(3):587–93. doi: 10.1111/j.1365-2133.2009.09586.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16(5):535–8. doi: 10.1097/00004630-199509000-00013. [DOI] [PubMed] [Google Scholar]
- 9.Parry I, Sen S, Palmieri T, Greenhalgh D. Nonsurgical scar management of the face: does early versus late intervention affect outcome? J Burn Care Res. 2013;34(5):569–75. doi: 10.1097/BCR.0b013e318278906d. [DOI] [PubMed] [Google Scholar]
- 10.Barret JP, Herndon DN. Effects of burn wound excision on bacterial colonization and invasion. Plast Reconstr Surg. 2003;111(2):744–50. doi: 10.1097/01.PRS.0000041445.76730.23. discussion 51-2. [DOI] [PubMed] [Google Scholar]
- 11.Ong YS, Samuel M, Song C. Meta-analysis of early excision of burns. Burns. 2006;32(2):145–50. doi: 10.1016/j.burns.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Goodwin CW, Maguire MS, McManus WF, Pruitt BA, Jr. Prospective study of burn wound excision of the hands. J Trauma. 1983;23(6):510–7. doi: 10.1097/00005373-198306000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Cope O, Langohr JL, Moore FD, Webster RC. Expeditious Care of Full-Thickness Burn Wounds by Surgical Excision and Grafting. Ann Surg. 1947;125(1):1–22. [PMC free article] [PubMed] [Google Scholar]
- 14.Herndon DN, Parks DH. Comparison of serial debridement and autografting and early massive excision with cadaver skin overlay in the treatment of large burns in children. J Trauma. 1986;26(2):149–52. doi: 10.1097/00005373-198602000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Engrav LH, Heimbach DM, Reus JL, Harnar TJ, Marvin JA. Early excision and grafting vs. nonoperative treatment of burns of indeterminant depth: a randomized prospective study. J Trauma. 1983;23(11):1001–4. doi: 10.1097/00005373-198311000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Gray DT, Pine RW, Harnar TJ, Marvin JA, Engrav LH, Heimbach DM. Early surgical excision versus conventional therapy in patients with 20 to 40 percent burns. A comparative study. Am J Surg. 1982;144(1):76–80. doi: 10.1016/0002-9610(82)90605-5. [DOI] [PubMed] [Google Scholar]
- 17.Burke JF, Quinby WC, Jr, Bondoc CC. Primary excision and prompt grafting as routine therapy for the treatment of thermal burns in children. Surg Clin North Am. 1976;56(2):477–94. doi: 10.1016/s0039-6109(16)40890-x. [DOI] [PubMed] [Google Scholar]
- 18.Cole JK, Engrav LH, Heimbach DM, Gibran NS, Costa BA, Nakamura DY, et al. Early excision and grafting of face and neck burns in patients over 20 years. Plast Reconstr Surg. 2002;109(4):1266–73. doi: 10.1097/00006534-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 19.Hunt JL, Sato R, Baxter CR. Early tangential excision and immediate mesh autografting of deep dermal hand burns. Ann Surg. 1979;189(2):147–51. doi: 10.1097/00000658-197902000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mann R, Gibran NS, Engrav LH, Foster KN, Meyer NA, Honari S, et al. Prospective trial of thick vs standard split-thickness skin grafts in burns of the hand. J Burn Care Rehabil. 2001;22(6):390–2. doi: 10.1097/00004630-200111000-00007. [DOI] [PubMed] [Google Scholar]
- 21.Covey MH, Dutcher K, Heimbach DM, Marvin JA, Engrav LH, deLateur B. Return of hand function following major burns. J Burn Care Rehabil. 1987;8(3):224–6. doi: 10.1097/00004630-198705000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Matsumura H, Engrav LH, Nakamura DY, Vedder NB. The use of the Millard "crane" flap for deep hand burns with exposed tendons and joints. J Burn Care Rehabil. 1999;20(4):316–9. doi: 10.1097/00004630-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Saaiq M, Zaib S, Ahmad S. Early excision and grafting versus delayed excision and grafting of deep thermal burns up to 40% total body surface area: a comparison of outcome. Ann Burns Fire Disasters. 2012;25(3):143–7. [PMC free article] [PubMed] [Google Scholar]
- 24.Wexler MR, Yeschua R, Neuman Z. Early treatment of burns of the dorsum of the hand by tangential excision and skin grafting. Plast Reconstr Surg. 1974;54(3):268–73. doi: 10.1097/00006534-197409000-00003. [DOI] [PubMed] [Google Scholar]
- 25.Khadjibayev AM, Fayazov AD, Djabriyev DA, Kamilov UR. Surgical treatment of deep burns. Ann Burns Fire Disasters. 2008;21(3):150–2. [PMC free article] [PubMed] [Google Scholar]
- 26.Pavoni V, Gianesello L, Paparella L, Buoninsegni LT, Barboni E. Outcome predictors and quality of life of severe burn patients admitted to intensive care unit. Scand J Trauma Resusc Emerg Med. 2010;18:24. doi: 10.1186/1757-7241-18-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thompson P, Herndon DN, Abston S, Rutan T. Effect of early excision on patients with major thermal injury. J Trauma. 1987;27(2):205–7. doi: 10.1097/00005373-198702000-00019. [DOI] [PubMed] [Google Scholar]
- 28.Tompkins RG, Remensnyder JP, Burke JF, Tompkins DM, Hilton JF, Schoenfeld DA, et al. Significant reductions in mortality for children with burn injuries through the use of prompt eschar excision. Ann Surg. 1988;208(5):577–85. doi: 10.1097/00000658-198811000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Xiao-Wu W, Herndon DN, Spies M, Sanford AP, Wolf SE. Effects of delayed wound excision and grafting in severely burned children. Arch Surg. 2002;137(9):1049–54. doi: 10.1001/archsurg.137.9.1049. [DOI] [PubMed] [Google Scholar]