Abstract
Objective:
To determine the presentation, anatomical distribution, diagnostic method, management and outcome of hollow viscus injury (HVI) from blunt abdominal trauma.
Methods:
This was a retrospective cross-ecnal study including patients with blunt abdominal trauma leading to HVI admitted at Rajendra Institute of Medical Sciences, Ranchi, over a period of 4.5 years (January 2009 to July 2014). Data were retrieved from patients’ medical records. Total 173 patients with HVI due to blunt abdominal trauma, who underwent laparotomy at our institute, were reviewed. Data regarding clinical presentation, anatomical distribution, management and outcome were recorded and analysed.
Results:
Out of 173 patients 87.1% were men and 12.9% were women. Mean age of patients was 29±14.02 years. The most common site of injury was ileum (46.2%) followed by jejunum (44.5%). There were 5 gastric perforations (2.9%), 2 (1.15%) duodenal, 2 (1.15%) colonic, 2 (1.15%) sigmoidal and 2 (1.15%) rectal injuries. One caecal injury was also recorded. Road traffic accident was the most common mechanism of injury (57.2%) followed by fall from height (36.4%) and assault (6.4%). Free gas under diaphragm on erect abdomen radiography was seen in 85.5% of cases while preoperative CT Abdomen was done in 11.6% of cases. Treatment consisted of simple closure of the perforation (66.5%), resection and anastomosis (11.0%) and stoma (22.5%). Major complication was anastamotic leak which was recorded in 6.4% cases and 15.6% patients developed burst abdomen. Average hospital stay was 13±6 days. Overall mortality rate was 12.7%.
Conclusion:
Although early recognition of intestinal injuries from blunt abdominal trauma may be difficult in all cases, it is very important due to its tremendous life threatening potential. Age of the patient, anatomical site and time of presentation are probably main prognostic factors.
Key Words: Hollow viscus injury (HVI), Blunt abdominal trauma, Diagnostic modality, Complication, Mortality
Introduction
Traumatic injuries remain the leading cause of death among patients aged 12–45 years and continue to account for substantial morbidity in this population [1]. Hollow viscus injury (HVI) following blunt abdominal trauma is an infrequent diagnosis [2]. The incidence of hollow viscus injuries following blunt abdominal trauma varies from 4 to 15% [3]. Patients with penetrating abdominal trauma have mostly HVI; however this diagnosis is infrequent in blunt abdominal trauma because the trauma should be very severe. Solid organ injury and resultant hemodynamic instability present a higher priority in the management of the patient with blunt abdominal trauma, and HVI is not usually suspected unless the clinical picture is highly suggestive [4-7].It is well known that delay in diagnosis and treatment of the hollow viscus injury results in early peritonitis, hemodynamic instability and increased mortality and morbidity [8]. The decrease in the rate of penetrating abdominal trauma and the increase in the rate of blunt abdominal trauma have resulted in increased rate of hollow viscus injury. Thus the early diagnosis and treatment remains the most important part of the management [9].
Management of blunt abdominal trauma leading to hollow viscus injury is a major challenge for both surgeons and anaesthesiologists [10]. In contradiction to non-operative management of maximum solid visceral injury, early surgical intervention is of paramount importance in case of hollow viscus injury. A delay in diagnosis and hence treatment increases morbidity and mortality [5-7].
As the incidence of HVI following blunt abdominal trauma is low, the experience of the surgeons with this diagnosis is limited. In the same way few centers have extensive experience in this field and there is lack of large data sets and epidemiological data about the incidence, prevalence, diagnosis, and outcomes of these injuries are limited. Thus we preformed the present study to review our experience with HVIfollowing blunt abdominal trauma in tertiary care centre of east zone of India.
Materials and Methods
Study Population
This was a cross-sectional study being performed in during a 4.5-year period from January 2009 to July 2014 in Rajendra Institute of Medical Sciences hospital, a tertiary healthcare centre in eastern India. The study protocol was approved by institutional review board (IRB) and medical ethics committee of Rajendra Institute of Medical Sciences. As this was a retrospective study, no informed written consent was required for inclusion in the study. We included all the patients who were referred to our center with blunt abdominal trauma who were diagnosed to have hollow viscus injury. We included those patients who their medical charts had complete data on baseline characteristics, clinical findings and radiological work-ups. We also included those patients who had abdominal work-ups. A patient was defined as having had an abdominal workup if they had any one or more of the following tests or procedures performed: abdominal computed tomographic scan, diagnostic peritoneal lavage, abdominal ultrasound, or exploratory laparotomy.
Study Protocol
The medical charts of the patients who were found to be eligible for the study were reviewed and the data was extracted using a data gathering form.
Patient data were abstracted while protecting patient confidentiality by individual chart review. Data were collected on age, sex, mechanism of injury, presentation, location of injury, associated injuries, treatment, mortality and morbidity. HVI diagnosis, operations, and discharge/death was also recorded. Data was prospectively entered into a computer database.
Statistical Analysis
All the statistical analyses were performed using statistical package for social sciences (SPSS Inc., Chicago, Illinois, USA). Data are presented as mean±SD and proportions as appropriate. Descriptive analysis was used for the study.
Results
Overall we included 173 patients with hollow viscus injury following blunt abdominal trauma. The mean age of the patients was 29.1±14.1 (ranging from 3 to 80) years. There were 152 (87.1%) men and 21 (12.9%) women among the patients. Road traffic accident were the most common cause of injury (57.2%) followed by fall from height (36.4%) and assault trauma (6.4%).
Free gas under diaphragm in erect abdominal radiography was recorded in 148 (85.5%) patients while preoperative abdominal CT-Scan/ Ultrasonography was performed in 20 (11.6%) patients. Exploratory laparotomy was performed in 151 (87.3%) patients based on clinical or radiological findings. The mean time from injury to laparotomy was 2.69±0.78 Days.
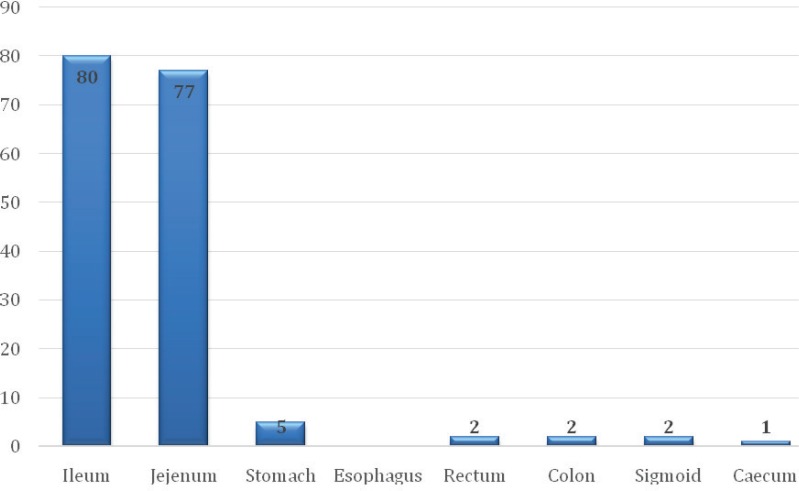
Ileum was the most common site of injury recorded in 80 (46.2%) patients followed by jejunum in 77 (44.5%). There were 5 gastric perforations (2.9%), 2 (1.15%) duodenal, 2 (1.15%) colonic, 2 (1.15%) sigmoidal and 2 (1.15%) rectal injuries. One (0.57%) caecal injury was also seen. The frequency of hollow viscus injury in our series is summarized in Figure 1. Treatment consisted of simple closure of the perforation (66.5%), resection and anastomosis (11.0%) and stoma (22.5%). All gastric and duodenal injuries were treated by primary closure. Most of the small intestinal perforations were treated by primary closure, resection and anastamosis while few required ileostomy. One caecal injury was closed primarily while two colonic injuries required diversion ileostomy. All four rectosigmoidal injuries were treated by diversion colostomy followed by stoma closure at 3 months. Major complications were encountered in 38 (22.00%) patients. 11 (6.35%) patients had anastmosis leak while 27 (15.6%) developed burst abdomen. Minor complications such as wound infection; chest infection and prolonged ileus have not been included. Overall 22 (12.7%) patients passed away due to HVI. Six (3.4%) patients expired due to shock or renal failure within 24 hours of laparotomy. The causes of mortality in our series in summarized in Table 1. Associated injuries were present in 37 (21.38%) patients (Table 2). Intra-abdominal injuries were mainly to the liver. Extra-abdominal injuries were mainly to the skeletal system.The mean hospital stay was 13.2±6.4 (ranging from 7 to 30) days.
Fig. 1.
Frequancy of hollow viscus injury in 173 patients with blunt abdominal trauma refered to our center.
Table 1.
The mortality and complications of hollow viscus injury in 173 patients with blunt abdominal trauma
| Complication/solid viscera injury | Frequency (n=173) | Mortality |
|---|---|---|
| Anastamotic leak | 11 (6.35%) | 10 (5.78%) |
| Burst abdomen | 27 (15.6%) | 2 (1.15%) |
| Liver injury | 11 (6.35%) | 3 (1.73%) |
| Pancreatic injury | 1 (0.57%) | 1 (0.57%) |
Table 2.
Frequency of associated injuries in 173 patients with blunt abdominal trauma and hollow viscus injury.
| Site of injury | Frequency (n=173) |
|---|---|
| Liver | 11 (6.35%) |
| Pancreas | 1 (0.57%) |
| Renal | 2 (1.15%) |
| Skeletal | 17 (9.82%) |
| Liver + skeletal | 6 (3.46%) |
Discussion
An analysis of more than 275,557 patients with blunt abdominal trauma enrolled in the EAST Multi- Institutional Hollow Viscus Injury Research study, the largest retrospective hollow viscus injury to date, found the incidence of blunt colonic injury to be 0.3% and the incidence of blunt small bowel injury to be 1.1% [11]. Motor vehicle accidents were the most common cause of these injuries. Child abuse, fall from height, sports, industrial accidents and even Heimlich manoeuvre also have been implicated in bowel and mesentery injury [11]. In our series also most common cause was road traffic accident (57.2%). Injury to the intra-abdominal structures can be classified into two primary mechanisms of injury; compression forces and deceleration forces. Compression or concussive forces may result from direct blows or external compression against a fixed object (e.g. lap belt, spinal column). These forces may deform hollow organs and transiently increase intraluminal pressure, resulting in rupture. Deceleration forces cause stretching and linear shearing between relatively fixed and free objects. As bowel loops travel from their mesenteric attachments, thrombosis and mesenteric tears, with resultant splanchnic vessel injuries can result [12]. Approximately 25% of patients requiring surgical treatment for bowel trauma have more than one bowel injury and likely more than one mechanism [11]. Whatever the mechanism, early recognition of these lesions can be difficult. Bowel injuries vary from minor hematoma to perforation. Small perforations may go clinically unrecognized. Abdominal pain and peritoneal irritation may be present early after major perforations or develop slowly because bowel contents, particularly jejunal contents, are not enzymatically active and have low pH and bacterial counts.
The greater the number of organs injured, the more likely there is associated bowel and mesenteric injury and in one third of the patient’s bowel and mesenteric injury coexists with pancreatic or other solid organs [11]. In our series, associated viscera injury was seen in 37 (21.4%) cases. As with others studies, the small intestine were also the most commonly injured in the present study [13-15]. In this study, it was observed that the proximal jejunum and distal ileum were more prone to perforation (n=157). Colonic injuries occurred less frequent (n=7) than small intestinal injuries. This has also been reported in others studies [15,16]. This is mainly due to its location and the lack of redundancy, which prevents formation of closed loops [16,17]. Diagnostic tests in evaluation of blunt abdominal trauma include X-ray erect abdomen, ultrasonography (US), diagnostic peritoneal lavage (DPL), computed tomography (CT) and diagnostic laparoscopy (DL). Ultrasonography is convenient, cheap and non- invasive. DPL was the diagnostic method of choice for evaluating blunt abdominal injury in the past, but recently has been often replaced by CT imaging [18]. Although DPL is sensitive in identifying hemoperitoneum and associated hollow viscus injury, it has been criticized for its higher rate of non-therapeutic laparotomy.
Nural et al., [19] reported that the sensitivity, specificity, positive predictive value, negative predictive value and accuracy of US in detecting intra-abdominal injury were 86.5%, 95.4%, 62.7%, 98.7% and 94.7%, respectively. They concluded that US has high diagnostic performance in the screening of patients with blunt abdominal trauma (19). Killeen et al., [20] found a high level of accuracy for detection of bowel injuries, with an accuracy of 86%, sensitivity of 94%, and a positive predictive value of 92% for CT abdomen. Bowel trauma can be classified as a partial or full-thickness injury. Partial thickness bowel injury can be seen on MDCT as a focal region of bowel wall thickening, usually greater than 3 mm in thickness. Although most cases of bowel wall contusion resolve spontaneously, serial physical examination or follow-up MDCT in 4–6 h are useful to demonstrate healing of this injury [21]. Full thickness bowel injury can be suspected if there is: extraluminal oral contrast or luminal content extravasation and discontinuity of hollow viscus wall. While, CT findings considered suggestive of bowel injury include: pneumoperitoneum, air foci near hollow viscus, thickened (>4–5 mm) bowel wall, bowel wall hematoma, intraperitoneal fluid of unknown source [22]. Lawson et al., [23] in their review of trauma patients for delayed diagnosis found that the most common missed injury is bowel injury so a high index of suspicion and tertiary survey remain a mainstay of therapy. In our series time of presentation to surgical facility was late (Mean 2.69 days). This is in contrast to most case series in developed countries where presentation is early.
X ray erect abdomen was able to diagnose hollow viscus perforation in more than 85% of our patients. Regarding treatment, exploratory laparotomy, drainage of septic peritoneal fluid and wound saline lavage are very important. Prophylactic antibiotics are required. Simple closure is usually adequate for single perforation of the small intestine. In our study various surgical techniques were performed, though mortality and morbidity remained high and most dreaded complication being anastamotic leak and wound dehiscence. Simple closure of the perforation was the commonly used technique for gastric, duodenal and jejunal perforations, for single perforation with minimum contamination of the peritoneum. And for multiple perforations of jejunum, close to each other, we preferred resection and anastomosis in our set up. In toxic and moribund patients with grossly contaminated peritoneum a temporary ileostomy was opted. Though the maintainance postoperatively was cumbersome and required a second surgery, this technique showed good results in the patient’s wellbeing postoperatively, and were allowed oral feeds early, and discharged early in our study. Resection and anastomosis carried high morbidity and mortality in our study.
There is clear evidence supporting primary repair in colorectal injuries [24]. However in our set up management of colorectal injuries was in favour of a loop colostomy for diversion in view of the faecal contamination of the peritoneal cavity (6 of 7 cases). One sigmoid colon injury was repaired primarily. One patient of caecal injury expired while all others survived. There is universal agreement regarding the need for complete diversion of the faecal stream with colorectal injuries involving all layers. For extensive rectal injuries Hartmann’s procedure is recommended [25]. The mortality in this series was 12.7%. Mortality rates quoted from blunt intestinal trauma range from 10-30% [25]. Reports have shown that mortality increases with the number of associated injuries [11].
In conclusion,in most cases of hollow viscus injury due to blunt abdominal trauma, presence of signs of peritonitis with obliteration of liver dullness supported by plain X-ray abdomen in erect posture are diagnostic and exploration is mandatory. Time scale of surgical intervention is important prognostic factor. It is interesting to note that most of the hemodynamically stable patients of solid viscera injury are managed conservatively, while rarely in hollow viscus injury. Follow up of a suspected case of hollow viscus injury is more clinical than imaging based even in hemodynamically stable patients.
Conflict of Interest: None declared.
References
- 1.TraumaRegisterDGU(®) 20years of trauma documentation in Germany-Actual trends and developments. Injury. 2014;45(Suppl 3):S14–9. doi: 10.1016/j.injury.2014.08.012. [DOI] [PubMed] [Google Scholar]
- 2.Fakhry SM, Brownstein M, Watts DD, Baker CC, Oller D. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000;48(3):408–14. doi: 10.1097/00005373-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Bruscagin V1, Coimbra R, Rasslan S, Abrantes WL, Souza HP, Neto G, et al. Blunt gastric injury. A multicentre experience. Injury. 2001;32(10):761–4. doi: 10.1016/s0020-1383(01)00081-x. [DOI] [PubMed] [Google Scholar]
- 4.Magu S, Agarwal S, Gill RS. Multi detector computed tomography in the diagnosis of bowel injury. Indian J Surg. 2012;74(6):445–50. doi: 10.1007/s12262-011-0405-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swaid F, Peleg K, Alfici R, Matter I, Olsha O, Ashkenazi I, et al. Concomitant hollow viscus injuries in patients with blunt hepatic and splenic injuries: An analysis of a National Trauma Registry database. Injury. 2014;45(9):1409–12. doi: 10.1016/j.injury.2014.02.027. [DOI] [PubMed] [Google Scholar]
- 6.Abbasi HR, Mousavi SM, TaheriAkeri A, Niakan MH, Bolandparvaz S, Paydar S. Pattern of Traumatic Injuries and Injury Severity Score in a Major Trauma Center in Shiraz, Southern Iran. Bull Emerg Trauma. 2013;1(2):81–85. [PMC free article] [PubMed] [Google Scholar]
- 7.Pekkari P, Bylund PO, Lindgren H, Öman M. Abdominal injuries in a low trauma volume hospital--a descriptive study from northern Sweden. Scand J Trauma Resusc Emerg Med. 2014;22 doi: 10.1186/s13049-014-0048-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arikanoglu Z, Turkoglu A, Taskesen F, Ulger BV, Uslukaya O, Basol O, et al. Factors affecting morbidity and mortality in hollow visceral injuries following blunt abdominal trauma. Clin Ter. 2014;165(1):23–6. doi: 10.7417/CT.2013.1656. [DOI] [PubMed] [Google Scholar]
- 9.Matsushima K, Mangel PS, Schaefer EW, Frankel HL. Blunt hollow viscus and mesenteric injury: still underrecognized. World J Surg. 2013;37(4):759–65. doi: 10.1007/s00268-012-1896-2. [DOI] [PubMed] [Google Scholar]
- 10.Gonser-Hafertepen LN, Davis JW, Bilello JF, Ballow SL, Sue LP, Cagle KM, et al. Isolated free fluid on abdominal computed tomography in blunt trauma: watch and wait or operate? J Am Coll Surg. 2014;219(4):599–605. doi: 10.1016/j.jamcollsurg.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 11.Watts DD, Fakhry SM. EAST Multi-Institutional Hollow Viscus Injury Research Group. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. J Trauma. 2003;54(2):289–94. doi: 10.1097/01.TA.0000046261.06976.6A. [DOI] [PubMed] [Google Scholar]
- 12.Kulvatunyou N, Albrecht RM, Bender JS, Friese RS, Joseph B, Latifi R, et al. Seatbelt triad: severe abdominal wall disruption, hollow viscus injury, and major vascular injury. Am Surg. 2011;77(5):534–8. doi: 10.1177/000313481107700509. [DOI] [PubMed] [Google Scholar]
- 13.Kane NM, Francis IR, Burney RE, Wheatley MJ, Ellis JH, Korobkin M. EAST Multi-Institutional Hollow Viscus Injury Research Group. Incidence of hollow viscus injury in blunt trauma: an analysis from 275,557 trauma admissions from the East multi-institutional trial. Invest Radiol. 1991;26(6):574–8. [Google Scholar]
- 14.Chirdan LB, Uba AF, Chirdan OO. Gastrointestinal injuries following blunt abdominal trauma in children. Niger J Clin Pract. 2008;11(3):250–3. [PubMed] [Google Scholar]
- 15.Ameh EA, Nmadu PT. Gastrointestinal injuries from blunt abdominal trauma in children. East Afr Med J. 2004;81(4):194–7. doi: 10.4314/eamj.v81i4.9154. [DOI] [PubMed] [Google Scholar]
- 16.Sule AZ, Kidmas AT, Awani K, Uba F, Misauno M. Gastrointestinal perforation following blunt abdominal trauma. East Afr Med J. 2007;84(9):429–33. doi: 10.4314/eamj.v84i9.9552. [DOI] [PubMed] [Google Scholar]
- 17.Khan I, Bew D, Elias DA, Lewis D, Meacock LM. Mechanisms of injury and CT findings in bowel and mesenteric trauma. Clin Radiol. 2014;69(6):639–47. doi: 10.1016/j.crad.2014.01.021. [DOI] [PubMed] [Google Scholar]
- 18.Fraga GP, Silva FH, Almeida NA, Curi JC, Mantovani M. Blunt abdominal trauma with small bowel injury: are isolated lesions riskier than associated lesions? Acta Cir Bras. 2008;23(2):192–7. doi: 10.1590/s0102-86502008000200013. [DOI] [PubMed] [Google Scholar]
- 19.Nural MS, Yardan T, Güven H, Baydin A, Bayrak IK, Kati C. Diagnostic value of ultrasonography in the evaluation of blunt abdominal trauma. Diagn Interv Radiol. 2005;11(1):41–4. [PubMed] [Google Scholar]
- 20.Killeen KL, Shanmuganathan K, Poletti PA, Cooper C, Mirvis SE. Helical computed tomography of bowel and mesenteric injuries. J Trauma. 2001;51(1):26–36. doi: 10.1097/00005373-200107000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Miller LA, Shanmuganathan K. Multidetector CT evaluation of abdominal trauma. 2005;43(6):1079–viii. doi: 10.1016/j.rcl.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Scaglione M1, de Lutio di Castelguidone E, Scialpi M, Merola S, Diettrich AI, Lombardo P, et al. Blunt trauma to the gastrointestinal tract and mesentery: is there a role for helical CT in the decision-making process? Eur J Radiol. 2004;50(1):67–73. doi: 10.1016/j.ejrad.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Lawson C, Daley BJ, Ormsby CD, Enderson B. Missed injuries in the era of the trauma scan. J Trauma. 2011;70(2):452–6. doi: 10.1097/TA.0b013e3182028d71. discussion 456-8. [DOI] [PubMed] [Google Scholar]
- 24.Curran TJ, Borzotta AP. Complications of primary repair of colon injury: literature review of 2964 cases. Am J Surg. 1999;177(1):42–7. doi: 10.1016/s0002-9610(98)00293-1. [DOI] [PubMed] [Google Scholar]
- 25.Burch JM. Injury to the colon and rectum. In: Moore EE, Feliciano DV, Mattox KL, editors. Trauma. 5th ed. New York: McGraw Hill; 2004. [Google Scholar]