Abstract
There has been much evidence suggesting that reactive oxygen species (ROS) generated in mitochondria during cerebral ischemia play a major role in programming the senescence of organism. Antioxidants dealing with mitochondria slow down the appearance and progression of symptoms in cerebral ischemia and increase the life span of organisms. The mechanisms of mitochondrial targeted antioxidants, such as SKQ1, Coenzyme Q10, MitoQ, and Methylene blue, include increasing adenosine triphosphate (ATP) production, decreasing production of ROS and increasing antioxidant defenses, providing benefits in neuroprotection following cerebral ischemia. A number of studies have shown the neuroprotective role of these mitochondrial targeted antioxidants in cerebral ischemia. Here in this short review we have compiled the literature supporting consequences of mitochondrial dysfunction, and the protective role of mitochondrial targeted antioxidants.
Keywords: Mitochondria, Cerebral ischemia, Antioxidants, Reactive oxygen species
Introduction
Cerebral ischemia limits the delivery of substrates, mainly oxygen, glucose and impairs the energy requirement to the brain [1]. It is a leading cause of death in industrialized and developing countries. There is growing evidence that mitochondria play a major role in both necrotic and apoptotic neuronal cell death after cerebral ischemia [2,3]. Cerebral ischemia induced mitochondrial swelling, opening of mitochondrial permeability transition pore leading to either necrotic or apoptotic cell death, is currently being explored intensely [4-6]. Existing concepts advocate that mitochondrial swelling may be the result of membrane permeability transition initiated by a variety of stimuli. The stimuli for membrane permeability shift differ between ischemia alone versus ischemia with reperfusion as a consequence of the generation of reactive oxygen species. Mitochondrial dysfunction and oxidative stress are mutually dependent and reinforce damages that play a central role, not only in brain aging, but also in neurodegenerative disease [7]. Overproduction of reactive oxygen species (ROS), which may arise either from mitochondrial electron-transport chain or excessive stimulation of NAD(P)H, results in oxidative stress, a toxic process that can play a crucial role in damage of cellular components, including lipids and membranes, proteins, and DNA. At moderate levels, ROS participate in physiological signaling by contributing to the adjustment of brain function to cellular metabolism and metabolic supply. Mitochondrial dysfunction acts through a number of destructive pathways, including excessive production of ROS resulting in oxidative modification of mitochondrial proteins. This in turn causes impairment of oxidative phosphorylation, contributing to the onset and progression of disease. 10-(6-plastoquinonel) decyltriphenyl-phosphonium (SkQ1), mitoquinone (MitoQ), Coenzyme Q10 (CoQ10) and Methylene blue (MB) are antioxidants that selectively target mitochondria and protect it from oxidative damage and which have been shown to decrease mitochondrial damage in animal models of oxidative stress [8,9].
Effects of mitochondrial dysfunction on ischemic brain
Mitochondria play an essential role in the life and death of living cells, performing several fundamental regulatory processes. Destruction of the mitochondrial energy metabolism is the immediate cause of mitochondrial dysfunction and disruption of oxidative phosphorylation a key mechanism of producing adenosine triphosphate (ATP) in cerebral ischemia [10,11]. The maintenance of the mitochondrial membrane potential (MMP), which helps to establish a proton gradient across the inner mitochondrial membrane to activate the adenosine triphosphate (ATP) synthase to generate high-energy phosphates, is disturbed during cerebral ischemia. Loss of MMP may be a common feature of ischemic destructive processes; these processes favour the progression and initiation of the apoptotic cell death [12,13]. Moreover, mitochondria are main targets and source of oxidative stress, and an excess of ROS has been implicated in the pathogenesis of cerebral ischemia. These oxygen free radicals are main contributors to necrotic or delayed neuronal death and powerful initiators of inflammation and apoptosis [14].
Oxidative stress
Oxidative stress is a phenomenon in which there is an imbalance between free radicals and antioxidants in the living system, which plays a major role in the pathophysiology of neurodegenerative disorder [15]. The brain is at higher risk to the damage caused by oxidative stress due to high content of polyunsaturated fatty acid, high consumption of oxygen, elevated metabolic activity and relatively limited ability to combat with oxidative stress [16]. ROS act as secondary messengers in many intracellular signaling pathways and as mediators of oxidative damage and inflammation [17]. Free radicals can attack directly polyunsaturated fatty acids in membranes and initiate lipid peroxidation (LPO). These features may make the brain a target tissue for the onset and pathogenesis of a number of neurological disorders via oxygen radical production [18,19].
Inflammation
Cerebral ischemia is accompanied by a marked inflammatory reaction that is initiated by ischemia induced expression of cytokines, adhesion molecules, and other inflammatory mediators. Many inflammatory mediators and pro-inflammatory cytokines like TNF-α and IL-1β, are up-regulated during this period. The release of IL-1β is totally dependent on the response to pathogen-associated molecular patterns (PAMPs) or damage-associated molecular patterns (DAMPs) that attach and bind to pattern recognition receptors (PRRs) to up-regulate proinflammatory gene expression [20,21]. PAMPs are patterns carried by pathogens, such as bacterial endotoxin and DAMPs are commonly endogenous substances released by necrosis.
A number of inflammasome forming PRRs have been identified, including the Nod-like receptors (NLR) family, pyrin domain containing proteins (NLRP1, NLRP3, NLRP6, NLRP7, NLRP12, NLRC4) and AIM2. Among all inflammasomes identified until now, the best characterized and most strongly related with inflammation, is formed by NLRP3 [22]. NLRP3 can be activated by a various groups of disease associated molecules, where it oligomerizes with the adaptor ASC (apoptosis-associated speck-like protein containing a caspase recruitment domain) and caspase-1 to form the NLRP3-inflammasome, resulting in the processing of pro to mature IL-1β and its subsequent release. Massive amounts of ATP are rapidly released into the extracellular space after traumatic or ischemic injuries [23-26] and a high concentration of ATP activates NLRP3 inflammasome [23,27-28]. This indicates that NLRP3 inflammasome senses mitochondrial dysfunction and may explain the frequent association of mitochondrial dysfunction with inflammation. In a renal ischemic model, NLRP3 activation was found to be mediated at least partly via mitochondrial ATP released from disrupted cells [29].
Apoptosis
Mitochondria also plays important role in neuronal apoptosis, primarily the release of proapoptotic factors into the cytoplasm after the opening of mitochondrial transition pore. The first proapoptotic proteins, cytochrome c are released from the membrane space into cytosol [30]. Once released, these proteins activate the caspase dependent mitochondrial pathway and activate Apaf-1, as well as procaspase-9. Together with ATP these proteins form the apoptosome [31]. The aggregation of procaspase-9 leads to the activation of caspase-9 which is most probably an initiator of cytochrome c dependent caspase cascade, leading to the activativation of caspase-3. Caspase-3 has been reported as a key mediator of apoptosis in the ischemic brain, which cleaves many substrate proteins, including poly (ADP-ribose) polymerase (PARP) [32,33] and translocates AIF to the nucleus [34] as well as facilitating the accessibility of nuclear chromatin to endonucleases [35]. Activation of PARP after cleavage by caspase-3 leads to DNA damage. Subsequently, tumour suppressor transcription factor, p53, stops the cell cycle and prompts programmed cell death by up-regulation of pro-apoptotic protein expression, and down regulation of anti-apoptotic protein leading to subsequently cell death [36].
Mitochondrial targeted antioxidant
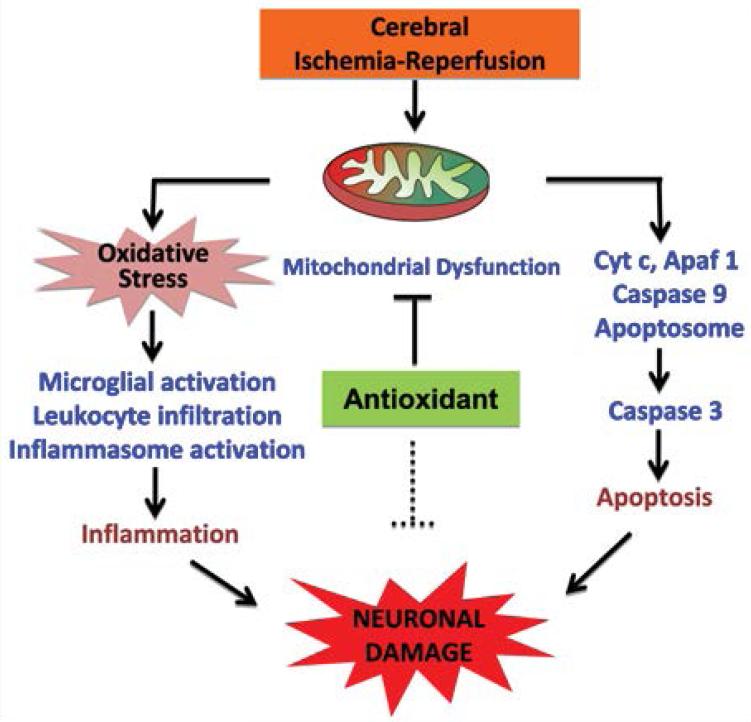
Mitochondria are the primary source of intracellular reactive oxygen species (ROS) and are mainly susceptible to oxidative stress. Oxidative damage to mitochondria has been shown to impair mitochondrial function and lead to cell death via apoptosis and necrosis. There is evidence that antioxidant treatments can ameliorate or delay disease progression in animal models of neurodegenerative diseases. Naturally occurring antioxidants SKQ1, CoQ10, MitoQ and MB have shown protective effects in the ischemic brain. The nature of these antioxidants and their protective role in ischemic brain are explained below and a schematic diagram has been shown in Figure 1.
Figure 1.
This diagram shows the effects of cerebral ischemia injuries on mitochondrial dysfunction, oxidative stress, release of pro-apoptotic factor and proinflammatory cytokines, and the eventually neuronal death. The neuroprotective effects of mitochondrial targeted antioxidant is indicated.
SKQ1
Mitochondria are important in the aging process, and one of the ways in which they interact with surrounding cell biology by ROS. The lipophilic cation SkQ1 is a mitochondrial targeted antioxidant, which accumulates inside the mitochondria, as these organelles form the only negatively charged compartment in the cell. High membrane potential of the inner mitochondrial membrane together with membrane potential (inside negative) of the plasma membrane and the strong hydrophobicity of SkQ1 results in the accumulation of SkQ1 in the inner leaflet of the inner mitochondrial membrane [37]. Oxidized SkQ1 formed after the scavenging of ROS is rapidly reduced by the mitochondrial respiratory chain, resulting in regeneration of reduced form of SkQ1. It has been observed that SkQ1 diminished the mitochondrial fragmentation (fission) after cerebral ischemia and prevent progression of the apoptotic cascade [38].
CoQ10
CoQ10 is fat soluble quinine with 10 five-carbon isoprenoid units, acts as an anti oxidant, protecting the cells against oxidative damage. CoQ10 is a component of the mitochondrial electron transport chain, transfering electron in the respiratory chain and playing a role in membrane stabilization [39]. CoQ10 is normally involved in a series of enzymatically catalyzed sequential reactions necessary to carry out oxidative phosphorylation via the electron transport chain (ETC). It collects reducing electrons from flavoprotein. Oxidative phosphorylation is a fundamental process used in the production of energy to maintain the brain function through the production of ATP [40,41]. CoQ10 has been reported to decrease brain lactate levels and lessen the diameter of ischemic lesions in animal models [42,43]. CoQ10 improves neurological outcomes and prevents neuronal damage by reducing the production of free radicals and preventing lipid peroxidation, a major cause of damage by free oxygen radicals. In addition, transient cerebral ischemia leads to decrease in tissue levels of CoQ10 [44]. Moreover, it has also been reported that CoQ10 lessens the diameter of ischemic lesions in animal models [45-47].
Mito Q
Mitochondria are vulnerable to oxidative damage and are also a major source of superoxide free radicals. Consequently, mitochondria accumulate oxidative damage that could contribute to mitochondrial dysfunction and cell death in cerebral ischemia. MitoQ is a lipophilic triphenylphosphonium (TPP) cation which helps it to pass easily through the phospholipid bilayer of mitochondria [48,49]. Within mitochondria, MitoQ is reduced by the respiratory chain reaction to its active form ubiquinol which is an effective antioxidant that prevents lipid peroxidation and mitochondrial damage [50]. MitoQ has been tested in a number of animal models of disease: supplementation of rats with MitoQ decreased heart dysfunction, cell death and mitochondrial damage subsequent to ischemia reperfusion in isolated heart [51,52]. It also protected endothelial cell function and damage to mitochondrial enzymes in a rat model of oxidative stress [53]. It has been found that MitoQ prevents ischemia reperfusion induced injury after the release of cytochrome c and caspase activation leading to massive tissue damage and cell death [54].
Methylene blue
Cerebral ischemia is a main cause of mortality and disability worldwide. The treatment of cerebral ischemia is controlled by a therapeutic window consisting of a few hours, and efficient drugs for the treatment of ischemia are extremely limited. MB has been proved to perform various biological functions and has been used for various medical applications [55]. MB crosses the blood–brain barrier and accumulates in the mitochondrial matrix [56,57]. MB has auto-oxidizing property and acts as an electron cycler which allows MB to pass on electrons to the mitochondrial electron transport chain (in the absence of oxygen), thereby enhancing ATP production, cytochrome c oxidase activity and helping in cell survival via bypassing complex I–III activity to generate ATP [58,59]. MB reduces reactive oxygen species production from the mitochondrial electron transport chain species [60,61] which has the potential to minimize ischemic and reperfusion injury.
Mito PBN
Alpha-phenyl-tert-butyl-nitrone (PBN) is a potent free radical scavenger believed to have protective actions in ischemia-reperfusion injury of brain by forming adducts of oxygen free radicals including OH radical [62,63]. It significantly reduces the cerebral infarction, neurological deficit, inducible cytochrome (cyclooxygenase-2) levels and activity, inducible nitric oxide synthase, inhibits mechanisms involved in nuclear factor-kB transduction, induces heme oxygenase-1, promotes mitochondrial function, enhances cholinergic function via acetyl cholinesterase inhibition, and inhibits calcium channels in ischemic brain [64-67].
Conclusion and Future Direction
Mitochondrial targeted antioxidants are one of the most important therapies for providing neuroprotection in cerebral ischemia. A large body of evidence supports the essential role of mitochondrial oxidative stress in ischemic brain injuries and despite the unsatisfactory results of non-targeted antioxidants in clinical trials, there is promising evidence in favor of beneficial effects of mitochondrial targeted antioxidants in ischemic brain injuries. These antioxidants SKQ1, CoQ10, MitoQ and MB reduce the mitochondrial oxidative stress either by direct antioxidant or indirectly through protection of mitochondrial structure and its function. Experimental studies will be needed to establish the significant impact of these treatments in both animal and clinical models of cerebral stroke.
It may be possible to combine these antioxidants with other therapeutic agents, to extend the therapeutic window of the drugs or of the effects of the mitochondrial targeted antioxidant itself. The use of mitochondrial targeted antioxidant in combination with other therapeutic agents may lead to the re-examination of the many neuroprotective drugs that failed at the clinical level, as many drugs may not have been studied in the most effective possible manner. However, it is clear that more research is still needed to understand their biological significance as well as how they can be effectively applied in additional clinical conditions.
Acknowledgement
This research was supported by Research Grant (NS086929) from the National Institutes of Neurological Disorders and Stroke, National Institutes of Health.
Footnotes
Conflict of Interests
The authors declare that there is no conflict of interests regarding the publication of this review.
References
- 1.Watts LT, Lloyd R, Garling RJ, Duong T. Stroke Neuroprotection: Targeting Mitochondria. Brain Sci. 2013;3:540–560. doi: 10.3390/brainsci3020540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu J, Li J, Yang Yi, Wang X, Zhang Z, et al. Neuronal apoptosis in cerebral ischemia/reperfusion area following electrical stimulation of fastigial nucleus. Neural Regen Res. 2014;9:727–34. doi: 10.4103/1673-5374.131577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Niizuma K, Yoshioka H, Chen H, Kim GS, Jung JE, et al. Mitochondrial and apoptotic neuronal death signaling pathways in cerebral ischemia. Biochim Biophys Acta. 2010;1802:92–9. doi: 10.1016/j.bbadis.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song T, Liu J, Tao X, Deng JG. Protection effect of atorvastatin in cerebral ischemia-reperfusion injury rats by blocking the mitochondrial permeability transition pore. Genet. Mol. Res. 2014;13:10632–10642. doi: 10.4238/2014.December.18.5. [DOI] [PubMed] [Google Scholar]
- 5.Li J, Yu W, Li XT, Qi SH, Li B. The effects of propofol on mitochondrial dysfunction following focal cerebral ischemiareperfusion in rats. Neuropharmacology. 2014;77:358–68. doi: 10.1016/j.neuropharm.2013.08.029. [DOI] [PubMed] [Google Scholar]
- 6.Hagberg H, Mallard C, Rousset CI, Thornton C. Mitochondria: hub of injury responses in the developing brain. Lancet Neurol. 2014;13:217–32. doi: 10.1016/S1474-4422(13)70261-8. [DOI] [PubMed] [Google Scholar]
- 7.Ruszkiewicz J, Albrecht J. Changes in the mitochondrial antioxidant systems in neurodegenerative diseases and acute brain disorders. Neurochem Int. 2015:S0197–0186(15)00004-2. doi: 10.1016/j.neuint.2014.12.012. [DOI] [PubMed] [Google Scholar]
- 8.Miclescu A, Sharma HS, Martijin C, Wicklund L. Methylene blue protects the cortical blood brain barrier against ischemia-reperfusion- induced disruption. Crit Care Med. 2010;38:2199. doi: 10.1097/CCM.0b013e3181f26b0c. [DOI] [PubMed] [Google Scholar]
- 9.Skulachev MV, Antonenko YN, Anisimov VN, Chernyak BV, Cherepanov DA, et al. Mitochondrial-targeted plastoquinone derivatives. Effect on senescence and acute age-related pathologies. Curr Drug Targets. 2011;12:800–826. doi: 10.2174/138945011795528859. [DOI] [PubMed] [Google Scholar]
- 10.Sanderson TH, Reynolds CA, Kumar R, Przyklenk K, Hüttemann M. Molecular mechanisms of ischemia-reperfusion injury in brain: pivotal role of the mitochondrial membrane potential in reactive oxygen species generation. Mol Neurobiol. 2013;47:9–23. doi: 10.1007/s12035-012-8344-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Panickar KS, Anderson RA. Effect of Polyphenols on Oxidative Stress and Mitochondrial Dysfunction in Neuronal Death and Brain Edema in Cerebral Ischemia. Int J Mol Sci. 2011;12:8181–8207. doi: 10.3390/ijms12118181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang S, Li Y, Song X, Wang X, Zhao C, et al. Febuxostat pretreatment attenuates myocardial ischemia/reperfusion injury via mitochondrial apoptosis. J Transl Med. 2015;13:209. doi: 10.1186/s12967-015-0578-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sun J, Li YZ, Ding YH, Wang J, Geng J, et al. Neuroprotective effects of gallic acid against hypoxia/reoxygenation-induced mitochondrial dysfunctions in vitro and cerebral ischemia/reperfusion injury in vivo. Brain Res. 2014;1589:126–39. doi: 10.1016/j.brainres.2014.09.039. [DOI] [PubMed] [Google Scholar]
- 14.Lee JC, Won MH. Neuroprotection of antioxidant enzymes against transient global cerebral ischemia in gerbils. Anat Cell Biol. 2014;47:149–56. doi: 10.5115/acb.2014.47.3.149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tabassum R, Vaibhav K, Shrivastava P, Khan A, Ahmed ME, et al. Perillyl alcohol improves functional and histological outcomes against ischemia-reperfusion injury by attenuation of oxidative stress and repression of COX-2, NOS-2 and NF-κB in middle cerebral artery occlusion rats. Eur J Pharmacol. 2015;747:190–199. doi: 10.1016/j.ejphar.2014.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Panickar KS, Qin B, Anderson RA. Ischemia-induced endothelial cell swelling and mitochondrial dysfunction are attenuated by cinnamtannin D1, green tea extract, and resveratrol in vitro. Nutr Neurosci. 2014 Apr 28; doi: 10.1179/1476830514Y.0000000127. [DOI] [PubMed] [Google Scholar]
- 17.Waldbaum S, Patel M. Mitochondrial dysfunction and oxidative stress a contributing link to acquired epilepsy. Journal of Bioenergetics and Biomembranes. 2010;42:449–455. doi: 10.1007/s10863-010-9320-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ates S, Cayli E. Neuroprotection by resveratrol against traumatic brain injury in rats. Molecular and Cellular Biochemistry. 2007;294:137–144. doi: 10.1007/s11010-006-9253-0. [DOI] [PubMed] [Google Scholar]
- 19.Tsai MJ, Liao JF, Lin DY. Silymarin protects spinal cord and cortical cells against oxidative stress and lipopolysaccharide stimulation. Neurochemistry International. 2010;57:867–875. doi: 10.1016/j.neuint.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 20.Chen GY, Nuñez G. Sterile inflammation sensing and reacting to damage. Nat Rev Immunol. 2010;10:826–837. doi: 10.1038/nri2873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Takeuchi O, Akira S. Pattern recognition receptors and inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 22.Cassel SL, Sutterwala FS. Sterile inflammatory responses mediated by the NLRP3 inflammasome. Eur J Immunol. 2010;40:607–611. doi: 10.1002/eji.200940207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Khakh BS, North RA. P2X receptors as cell-surface ATP sensors in health and disease. Nature. 2006;442:527–32. doi: 10.1038/nature04886. [DOI] [PubMed] [Google Scholar]
- 24.Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol Rev. 1998;50:413–92. [PubMed] [Google Scholar]
- 25.Latini S, Corsi C, Pedata F, Pepeu G. The source of brain adenosine outflow during ischemia and electrical stimulation. Neurochem Int. 1996;28:113–118. doi: 10.1016/0197-0186(95)00062-d. [DOI] [PubMed] [Google Scholar]
- 26.Peng W, Cotrina ML, Han X, Yu H, Bekar L, et al. Systemic administration of an antagonist of the ATP-sensitive receptor P2X7 improves recovery after spinal cord injury. Proc Natl Acad Sci U S A. 2009;106:12489–12493. doi: 10.1073/pnas.0902531106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gombault A, Baron L, Couillin I. ATP release and purinergic signaling in NLRP3 inflammasome activation. Front Immunol. 2012;3:414. doi: 10.3389/fimmu.2012.00414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dubyak GR. P2X7 receptor regulation of non-classical secretion from immune effector cells. Cell Microbiol. 2012;14:1697–1706. doi: 10.1111/cmi.12001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Iyer SS, Pulskens WP, Sadler JJ, B utter LM, Teske GJ, et al. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Proc Natl Acad Sci U S A. 2009;106:20388–20393. doi: 10.1073/pnas.0908698106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elmore S. Apoptosis a review of programmed cell death. Toxicol Pathol. 2007;35:495–516. doi: 10.1080/01926230701320337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Love S. Apoptosis and brain ischaemia. Prog Neuropsychopharmacol Biol Psychiatry. 2003;27:267–282. doi: 10.1016/S0278-5846(03)00022-8. [DOI] [PubMed] [Google Scholar]
- 32.Namura S, Zhu J, Fink K, Endres M, Srinivasan A, et al. Activation and cleavage of caspase-3 in apoptosis induced by experimental cerebral ischemia. J Neurosci. 1998;18:3659–3668. doi: 10.1523/JNEUROSCI.18-10-03659.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Haile WB, Echeverry R, Wu F, Guzman J, An J, et al. ecrosis factor-like weak inducer of apoptosis and fibroblast growth factor-inducible 14 mediate cerebral ischemia-induced poly(ADP-ribose) polymerase-1 activation and neuronal death. Neuroscience. 2010;171:1256–1264. doi: 10.1016/j.neuroscience.2010.10.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu SW, Wang H, Poitras MF, Coombs C, Bowers WJ, et al. Mediation of poly(ADP-ribose) polymerase-1-dependent cell death by apoptosis-inducing factor. Science. 2002;297:259–263. doi: 10.1126/science.1072221. [DOI] [PubMed] [Google Scholar]
- 35.Duriez PJ, Shah GM. Cleavage of poly (ADP-ribose) polymerase: a sensitive parameter to study cell death. Biochem Cell Biol. 1997;75:337–349. [PubMed] [Google Scholar]
- 36.Culmsee C, Mattson MP. p53 in neuronal apoptosis. Biochem Biophys Res Commun. 2005;331:761–777. doi: 10.1016/j.bbrc.2005.03.149. [DOI] [PubMed] [Google Scholar]
- 37.Skulachev VP, Anisimov VN, Antonenko YN, Bakeeva LE, Chernyak BV, et al. An attempt to prevent senescence; A mitochondrial approach. Biochemistry (Moscow) 2007;72:1385–1396. [Google Scholar]
- 38.Obukhova MR, Pasyukova LA, Pisarenko EG, Roginsky OI, Ruuge VA, et al. An attempt to prevent senescence a mitochondrial approach. Biochim Biophys Acta. 2009;1787:437–461. doi: 10.1016/j.bbabio.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 39.Folkers K, Langsjoen P, Willis R, Richardson P, Xia LJ, et al. Lovastatin decreases coenzyme Q levels in humans. Proc Natl Acad SciUSA. 1990;87:8931–8934. doi: 10.1073/pnas.87.22.8931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lehninger AL. The molecular organization of mitochondrial membranes. Adv Cytopharmacol. 1971;1:199–208. [PubMed] [Google Scholar]
- 41.Beal MF. Bioenergetic approaches for neuroprotection in Parkinson's disease. Ann Neurol. 2003;53:S39–S47. doi: 10.1002/ana.10479. [DOI] [PubMed] [Google Scholar]
- 42.Kalayci M, Unal MM, Gul S, Acikgoz S, Kandemir N, et al. of co-enzyme Q10 on ischemia and neuronal damage in an experimental traumatic brain-injury model in rats. BMC Neurosci. 2011;29:12–75. doi: 10.1186/1471-2202-12-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mellors A, Tappel AL. the inhibition of mitochondrial peroxidation by ubiquinone and ubiquinol. J Biol Chem. 1966;241:4353–4356. [PubMed] [Google Scholar]
- 44.Horecký J, Gvozdjáková A, Kucharská J, Obrenovich ME, Palacios HH, et al. Effects of coenzyme Q and creatine supplementation on brain energy metabolism in rats exposed to chroniccerebral hypoperfusion. Curr Alzheimer Res. 2010;8:868–875. doi: 10.2174/156720511798192727. [DOI] [PubMed] [Google Scholar]
- 45.Lemke M, Frei B, Ames BN, Faden AI. Decreases in tissue levels of ubiquinol -9 and -10, ascorbate and alpha toco-pherol following spinal cord impact trauma in rats. Neurosci Lett. 1990;108:201–206. doi: 10.1016/0304-3940(90)90731-n. [DOI] [PubMed] [Google Scholar]
- 46.Piotrowski P, Ostrowski RP, Pankowska T, Smialek M. The effect of coenzyme Q10 on lactate acidosis at the beginning of experimental cerebral ischemia in rats after the use of endothelin 1 (preliminary results) Neurol Neurochir Pol. 1998;32:1397–1404. [PubMed] [Google Scholar]
- 47.Lemke M, Frei B, Ames BN, Faden AI. Decreases in tissue levels of ubiquinol 9 and 10, ascorbate and alpha-tocopherol following spinal cord impact trauma in rats. Neurosci Lett. 1990;108:201–206. doi: 10.1016/0304-3940(90)90731-n. [DOI] [PubMed] [Google Scholar]
- 48.Murphy MP, Smith RA. Drug delivery to mitochondria: the key to mitochondrial medicine. Adv. Drug Deliv Rev. 2000;41:235–250. doi: 10.1016/s0169-409x(99)00069-1. [DOI] [PubMed] [Google Scholar]
- 49.Smith RA, Porteous J, Gane CM, Murphy MP. Delivery of bioactive molecules to mitochondria in vivo. Proc. Natl Acad Sci USA. 2003;100:5407–5412. doi: 10.1073/pnas.0931245100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kelso GF, Porteous CM, Coulter CV, Hughes G, Porteous WK, et al. Selective targeting of a redox active ubiquinone to mitochondria within cells. J Biol Chem. 2001;276:4588–4596. doi: 10.1074/jbc.M009093200. [DOI] [PubMed] [Google Scholar]
- 51.Neuzil J. Mitochondria transmit apoptosis signaling in cardiomycetes like cells and isolated hearts exposed to experimental ischemia reperfusion injury. Redox Rep. 2007;12:148–162. doi: 10.1179/135100007X200227. [DOI] [PubMed] [Google Scholar]
- 52.Ross MF. Rapid and extensive uptake and activation of hydrophobic triphenyle phosphonium Cations within cells. Biochem. 2008;411:633–645. doi: 10.1042/BJ20080063. [DOI] [PubMed] [Google Scholar]
- 53.Adlam VJ, Harrison JC, Porteous CM, James AM, Smith RA, et al. Targeting an antioxidant to mitochondria decreases cardiacischemia reperfusion injury. FASEB J. 2005;19:1088–1095. doi: 10.1096/fj.05-3718com. [DOI] [PubMed] [Google Scholar]
- 54.Esplugues JV, Rocha M, Nunez C, Bosca I, Ibiza S, et al. Complex1 dysfunction and tolerance to nitroglycerine and approach based on mitochondria targeted antioxidant. Circ Res. 2006;99:1067–1075. doi: 10.1161/01.RES.0000250430.62775.99. [DOI] [PubMed] [Google Scholar]
- 55.Wainwright M, Crossley KB. Methylene Blue a therapeutic dye for all seasons. J Chemother. 2002;14:431–443. doi: 10.1179/joc.2002.14.5.431. [DOI] [PubMed] [Google Scholar]
- 56.Tretter L, Horvath G, Holgyesi A, Essek F, AdamVizi V. Enhanced hydrogen peroxide generation accompanies the beneficial bioenergetic effects of methylene blue in isolated brain mitochondria. Free Radic Biol Med. 2014;77:317–330. doi: 10.1016/j.freeradbiomed.2014.09.024. [DOI] [PubMed] [Google Scholar]
- 57.Oz M, Lorke DE, Hasan M, Petroianu GA. Cellular and molecular actions of Methylene Blue in the nervous system. Med Res Rev. 2011;31:93–117. doi: 10.1002/med.20177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shen Q, Du F, Huang S, Rodriguez P, Watts LT, et al. Neuroprotective Efficacy of Methylene Blue in Ischemic Stroke: An MRI Study. PLoS ONE. 2013;8:e79833. doi: 10.1371/journal.pone.0079833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Di Y, He YL, Zhao T, Huang S, Wu KW, et al. Methylene Blue Reduces Acute Cerebral Ischemic Injury via the Induction of Mitophagy. Mol Med. 2015 doi: 10.2119/molmed.2015.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Callaway NL, Riha PD, Bruchey AK, Munshi Z, Gonzalez-Lima F. Methylene blue improve brain oxidative metabolism and memory retention in rats. Pharmacol Biochem. 2004;77:175–181. doi: 10.1016/j.pbb.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 61.Chen Q, Vazquez EJ, Moghaddas S, Hoppel CL, Lesnefsky EJ. Production of reactive oxygen species by mitochondria central role of complex III. J Biol Chem. 2003;278:36027–36031. doi: 10.1074/jbc.M304854200. [DOI] [PubMed] [Google Scholar]
- 62.Sen S, Phillis JW. alpha-Phenyl-tert-butyl-nitrone (PBN) attenuates hydroxyl radical production during ischemiareperfusion injury of rat brain: an EPR study. Free Radical Research Communications. 1993;19:255–265. doi: 10.3109/10715769309056513. [DOI] [PubMed] [Google Scholar]
- 63.Kuroda S, Tsuchidate R, Smith ML, Maples KR, Siesjo BK. Neuroprotective effects of a novel nitrone, NXY-059, after transient focal cerebral ischemia in the rat . J. Cereb. Blood Flow Metab. 1999;19:778–787. doi: 10.1097/00004647-199907000-00008. [DOI] [PubMed] [Google Scholar]
- 64.Cao X, Phillis WJ. Alpha-Phenyl-tert-butyl-nitrone reduces cortical infarct and edema in rats subjected to focal ischemia. Brain Research. 1994;644:267–272. doi: 10.1016/0006-8993(94)91689-6. [DOI] [PubMed] [Google Scholar]
- 65.Li PA, He QP, Nakamura, Csiszar KL. Free radical spin trap alpha-phenyl-N-tert-butyl-nitron inhibits caspase-3 activation and reduces brain damage following a severe forebrain ischemic injury. Free Radical Biology and Medicine. 2001;31:1191–1197. doi: 10.1016/s0891-5849(01)00700-6. [DOI] [PubMed] [Google Scholar]
- 66.Kotake Y, Sang H, Miyajima T, Wallis GL. Inhibition of NF-kappaB, iNOS mRNA, COX2 mRNA, and COX catalytic activity by phenyl-Nbutylnitrone (PBN). Biochim Biophys Acta. 1998;1448:77–84. doi: 10.1016/s0167-4889(98)00126-8. [DOI] [PubMed] [Google Scholar]
- 67.Alberts MJ. Diagnosis and treatment of ischemic stroke. Am J bed. 1999;106:211–221. doi: 10.1016/s0002-9343(98)00414-8. [DOI] [PubMed] [Google Scholar]