Abstract
Study Design Retrospective analysis of prospectively collected cohort data.
Objective Anterior lumbar interbody fusion (ALIF) is a commonly performed procedure for the treatment of degenerative diseases of the lumbar spine. Detailed and comprehensive descriptions of intra- and postoperative complications of ALIF are surprisingly limited in the literature. In this report, we describe our experience with a team model for ALIF and report all complications occurring in our patient series.
Methods Patients were prospectively enrolled between January 2009 and January 2013 by a combined spine surgeon and vascular surgeon team. All patients underwent an open ALIF using an anterior approach to the lumbosacral spine.
Results From the 227 ALIF cases, mean operative blood loss was 103 mL, ranging from 30 to 900 mL. Mean operative time was 78 minutes. The average length of stay was 5.2 days. Intraoperative vascular injury requiring primary repair with suturing occurred in 15 patients (6.6%). There were 2 cases of postoperative retroperitoneal hematoma. Three patients (1.3%) had incisional hernia requiring revision surgery; 7 (3.1%) patients had prolonged ileus (>7 days) managed conservatively. Four patients described retrograde ejaculation. Sympathetic dysfunction occurred in 15 (6.6%) patients. There were 5 (2.2%) cases of superficial wound infection treated with oral antibiotics, with no deep wound infections requiring reoperation or intravenous therapy. There were no mortalities in this series.
Conclusions ALIF is a safe procedure when performed by a combined vascular surgeon and spine surgeon team with acceptably low complication rates. Our series confirms that the team approach results in short operative times and length of stay, with rapid control of intraoperative vessel injury and low overall blood loss.
Keywords: complications, anterior lumbar interbody fusion (ALIF), vascular surgeon
Introduction
Anterior lumbar interbody fusion (ALIF) is a commonly performed procedure for the treatment of degenerative diseases of the lumbar spine. ALIF was first described by Capener in 1932 for the treatment of spondylolithesis1 and Ito et al in 1934 for the treatment of Pott disease,2 and it has since become a widely used technique for the treatment of a range of lumbar spine disorders. The common indications for ALIF include spondylolisthesis, degenerative disk disease, degenerative lumbar scoliosis, pseudarthrosis, and adjacent segment disease.3
ALIF is argued to have biomechanical advantages over posterior approaches for lumbar spinal fusion, including restoration of disk height and lumbar lordosis, reduction of anterior listhesis, and achievement of coronal and sagittal balance.4 5 6 The advantages over posterior approaches are attributed to the negated need for retraction and dissection of the posterior spinal musculature and excellent exposure of the anterior column and disk space.7 The development of adjacent segment disease has been shown to be less common in ALIF8; in addition, ALIF has fewer perioperative complications relating to injury of the dura and neural structures due to more direct visualization of and access to the disk space and anterior column.9 Other advantages of ALIF over the alternative approaches include shorter operating time, less blood loss, and reduced perioperative morbidity.5 10 11 12
Approach-related complications of ALIF are distinct from those of posterior approaches to the lumbar spine and predominantly relate to visceral and vascular injuries. The results of the major publications reporting complications of anterior spinal surgery are summarized in Table 1. The published rates of vascular injury associated with ALIF vary considerably, ranging from 1.9 to 24%,13 14 and the injuries occur most commonly in operations involving the L4–L5 disk space.15 Laceration of the left common iliac vein is the most commonly reported injury,15 whereas arterial injuries are much less frequent, with the rate of injury to the left iliac artery reported to be 0 to 0.9%.15 Other vascular injuries include laceration of the iliolumbar vein, avulsion of the median sacral and lumbar vein, and injury to the inferior vena cava or abdominal aorta, as well as thrombosis of the left iliac artery and retroperitoneal hematoma.
Table 1. Summary of published complications of anterior lumbar spinal surgery.
| Publication | Patients (n) | Vascular injuries, n (%) | Mean blood loss, mL (range) | DVT, n (%) | Visceral injuries, n (%) | Paralytic ileus, n (%) | Wound complication, n (%) | Retrograde ejaculation, n (%) | Sympathetic dysfunction, n (%) | Mean length of stay, d (range) |
|---|---|---|---|---|---|---|---|---|---|---|
| Rajaraman (1999)26 | 60 | 4 (6.7) | – | 1 (1.7) | 1 (1.7) | 3 (5) | 2 (3.3) | 2 (3.3) | 6 (10) | – |
| Mayer (2002)27 | 171 | – | 73.6 (20–400) | 1 (0.6) | – | 1 (0.6) | 1 (0.6) | – | – | – |
| Bianchi (2003)28 | 72 | 1 (1.4) | – | 1 (1.4) | 1 (1.4) | – | – | – | – | 5 |
| Brau (2004)13 | 1,310 | 25 (1.9) | – | – | – | – | – | – | – | – |
| Saraph (2004)29 | 56 | 4 (7.1) | 460 (100–2,000) | 1 (1.8) | – | 4 (7.1) | 1 (1.8) | – | 5 (8.9) | – |
| Gumbs (2005)30 | 60 | 2 (3.1) | – | – | – | – | – | – | – | 4 (2–22) |
| Sasso (2005)25 | 471 | 14 (3) | – | 2 (0.9) | – | – | – | 1 (0.4) | – | 3.8 (1–38) |
| Fantini (2007)31 | 345 | 10 (2.9) | 1,510 | – | – | – | – | – | – | – |
| Hamdan (2008)32 | 480 | 54 (11.3) | 150 | – | – | – | – | – | – | – |
| Chiriano (2009)33 | 405 | 107 (26.4) | – | 3 (0.7) | – | 6 (1.5) | – | – | – | 5.5 |
| Garg (2010)34 | 212 | 13 (6.1) | 143 (5–4,000) | 5 (2.4) | 1 (0.5) | – | 1 (0.5) | 4 (4.3) | 0 | – |
| Asha (2012)17 | 104 | 3 (2.9) | 148 (50–230) | 0 | 0 | 18 (17.3) | 1 (1) | 0 | – | Median 5 (4–9) |
Abbreviation: DVT, deep venous thrombosis.
The incidence of deep venous thrombosis following anterior spinal surgery ranges from 0 to 12.2%.16 17 Visceral complications are uncommon and include inadvertent enterotomy and ureteric injury. Injury to neural structures can result in femoral nerve palsy,18 retrograde ejaculation, erectile dysfunction, and sympathectomy manifesting in symptoms such as altered lower limb temperature and unilateral lower limb edema. Retrograde ejaculation occurs in up to 5% of ALIFs in men, with rates much higher with laparoscopic approaches (45%).19 Wound complications include infection, wound dehiscence, and incisional hernia.20 Other case reports have included rare and isolated complications including pancreatitis,21 retroperitoneal abscess and fibrosis, and latissimus dorsi rupture.22 23 24
Intraoperative complications of ALIF relating specifically to spinal instrumentation include bone fracture, dural tears, and ureteric avulsion,25 though these are uncommon. Vascular injury may also occur during the spinal instrumentation stage of ALIF, with up to 55% of vascular injuries attributed to this stage in some series.14
Detailed and comprehensive descriptions of intra- and postoperative complications of ALIF are surprisingly limited in the literature. In this report, we describe our experience with a team model for an anterior approach for lumbar spinal surgery, and we report all the complications that occurred in our patient series.
Materials and Methods
Ethics Approval
Approval was obtained from the South Eastern Sydney Local Health District, New South Wales Australia–Northern Sector ethics committee, Ref: HREC 11/183.
Patient Recruitment
Patients were prospectively enrolled between January 2009 and January 2013 by the senior author (R.J.M.) who performed all ALIF procedures in combination with a vascular surgeon (A.L.). Exclusion criteria included patients with an infection, osteoporosis, or cancer. Details regarding patient factors including age, gender, and comorbidities were collected, along with operative details including the spinal level of surgery and the intervention performed. Information regarding all complications occurring in the perioperative period was recorded, with a particular focus on the duration of surgery, blood loss, and length of hospital stay, as well as the vascular, visceral, and neurologic injuries.
Surgical Technique
All the patients underwent an open ALIF using an anterior approach to the lumbosacral spine. The vascular surgeon (A.L.) assisted with the approach in all procedures. Heparin was not used during the procedure. The incision varied on the approach level and the number of levels performed, with a mini-Pfannenstiel incision used for access to the L5–S1 level (Fig. 1A) and a midline vertical incision used for other levels and multilevel approaches (Fig. 1B). A left-sided retroperitoneal dissection exposing the affected anterior vertebral disk and retraction with a Synframe (Synthes Spine, Paoli, Pennsylvania, United States) were performed (Fig. 2). In all cases, the left ureter was identified and retracted medially. The major anterior vessels (aorta and iliac veins/arteries) were mobilized and retracted. The level of pathology was confirmed with X-ray prior to the disk removal, and the end plates were prepared. A stand-alone ALIF cage was packed with the bone graft, inserted, and fixed with integral screws. An X-ray was used to confirm correct placement, and antibiotic irrigation was used prior to closure.
Fig. 1.
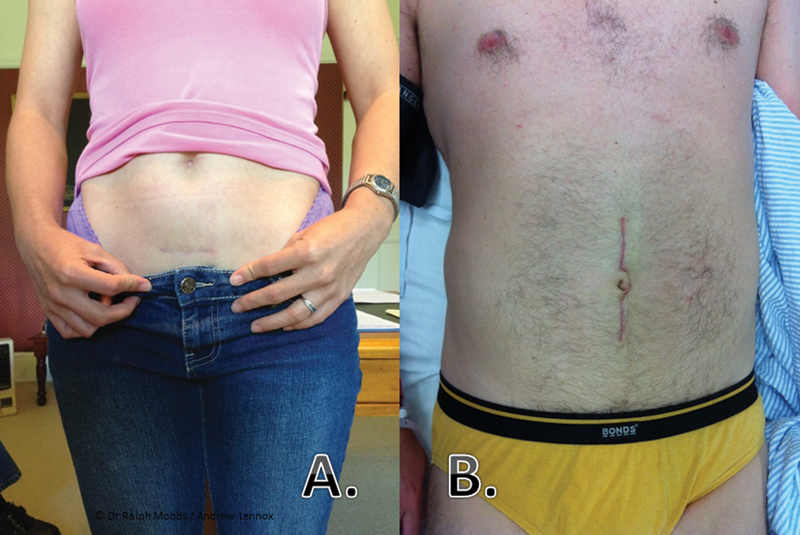
(A) L5–S1 approach: horizontal minimal access incision. (B) L3–L4 and L4–L5 approach: midline incision.
Fig. 2.
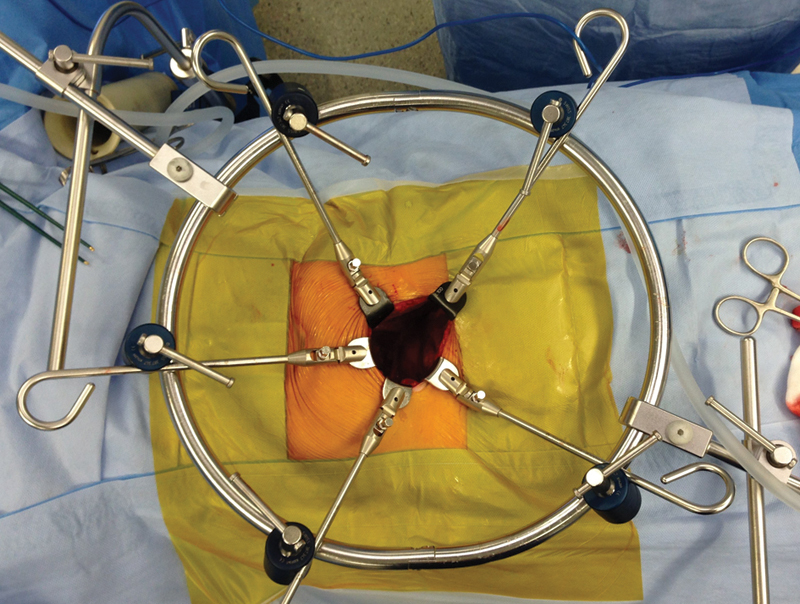
Synframe retractor (Synthes Spine, Paoli, Pennsylvania, United States).
Postoperative Care
The patients were encouraged to ambulate within 24 hours of surgery. Calf compressors were used in all the patients until mobilization. The determinations regarding rehabilitation and the level of physical exercise were based on the recommendation of the treating surgeon.
Results
Overall, 227 patients underwent anterior lumbar spinal surgery between 2009 and 2013 performed by one surgical team (R.J.M. and A.L.), as outlined in Table 2. The mean age of this cohort was 57.6 years, with a slight female preponderance, and approximately one third of the patients were overweight or obese. Of the patients, 143 (63%) underwent single-level operations, and 84 (37%) underwent multiple-level surgery at the lumbar spine level (Table 3). The L4–L5 and L5–S1 disk spaces were the most common operative levels, making up 34.7 and 59.5%, respectively. ALIF was the procedure performed on the majority of spinal levels (308 of 331 levels, 93.1%), with total disk replacement performed on the remaining 23 (6.9%).
Table 2. Patient details.
| n | % | |
|---|---|---|
| Number of patients | 227 | |
| Mean age, y (range) | 57.6 (25–86) | |
| Sex (male/female) | 105/122 | |
| Comorbidities | ||
| Overweight (BMI 25–30) | 62 | 27.3 |
| Obesity (BMI > 30) | 17 | 7.5 |
| Cigarette smoking | 36 | 16 |
| Diabetes | 20 | 8.8 |
| Work-related injury | 43 | 18 |
| Pathologies | ||
| Degenerative disk disease with radiculopathy | 104 | 45.8 |
| Degenerative disk disease without radiculopathy | 54 | 23.8 |
| Spondylolisthesis | 27 | 11.9 |
| Failed posterior fusion | 18 | 7.9 |
| Scoliosis | 14 | 6.2 |
| Adjacent segment disease | 10 | 4.4 |
Abbreviation: BMI, body mass index.
Table 3. Operative details.
| n | % | |
|---|---|---|
| Number of intervertebral levels | ||
| 1 | 143 | 63 |
| 2 | 67 | 29.5 |
| 3 | 14 | 6.2 |
| 4 | 3 | 1.3 |
| Total number of cases | 227 | |
| Operative level | ||
| L2–L3 | 3 | 0.9 |
| L3–L4 | 16 | 4.8 |
| L4–L5 | 115 | 34.7 |
| L5–S1 | 197 | 59.5 |
| Total number of levels exposed | 331 | |
| Operation performed | ||
| ALIF | 308 | 93.1 |
| Total disk replacement | 23 | 6.9 |
Abbreviation: ALIF, anterior lumbar interbody fusion.
The mean operative blood loss was 103 mL, ranging from 30 to 900 mL (Table 4). Intraoperative blood loss greater than 600 mL occurred in two cases, and no patients required blood transfusion during the procedure. The mean operative time was 78 minutes (range 40 to 195 minutes). The average length of stay was 5.2 days (range 1 to 19 days). The operative blood loss, operative time, and patient length of stay were all increased for patients undergoing multilevel surgery.
Table 4. Surgical outcomes.
| n | % | |
|---|---|---|
| Intraoperative blood loss, mL (range) | ||
| Single level | 82 (30–700) | |
| Multilevel | 162 (60–900) | |
| Total operation time, min (range) | ||
| Single level | 67 (40–125) | |
| Multilevel | 98 (60–195) | |
| Mean length of stay, d (range) | ||
| Single level | 4.6 (1–9) | |
| Multilevel | 6.2 (3–19) | |
| Complications | ||
| Major | ||
| Postoperative retroperitoneal hematoma | 2 | 0.9 |
| Acute arterial thrombosis | 1 | 0.4 |
| Acute bowel obstruction | 1 | 0.4 |
| Retrograde ejaculation | 4 | 1.8 |
| Incisional hernia requiring revision | 3 | 1.3 |
| Vascular injury | 15 | 6.6 |
| Minor | ||
| Sympathetic dysfunction | 15 | 6.6 |
| Wound infection (superficial) | 5 | 2.2 |
| Prolonged Ileus (>72 h) | 7 | 3.1 |
Intraoperative vascular injury requiring primary repair with suturing occurred in 15 patients (6.6%). These included 9 lacerations of the inferior vena cava, 2 of which occurred at the bifurcation. A further 4 lacerations were sustained to the common iliac vein, 1 to the external iliac vein, and 1 to the iliolumbar vein. There were no arterial lacerations. Other major vascular complications included 2 cases of postoperative retroperitoneal hematoma requiring surgical drainage without a source of bleeding identified (Fig. 3), and 1 case of acute arterial thrombosis required urgent reoperation and thromboendarterectomy (Fig. 4) on the background of significant iliac atheroma.
Fig. 3.
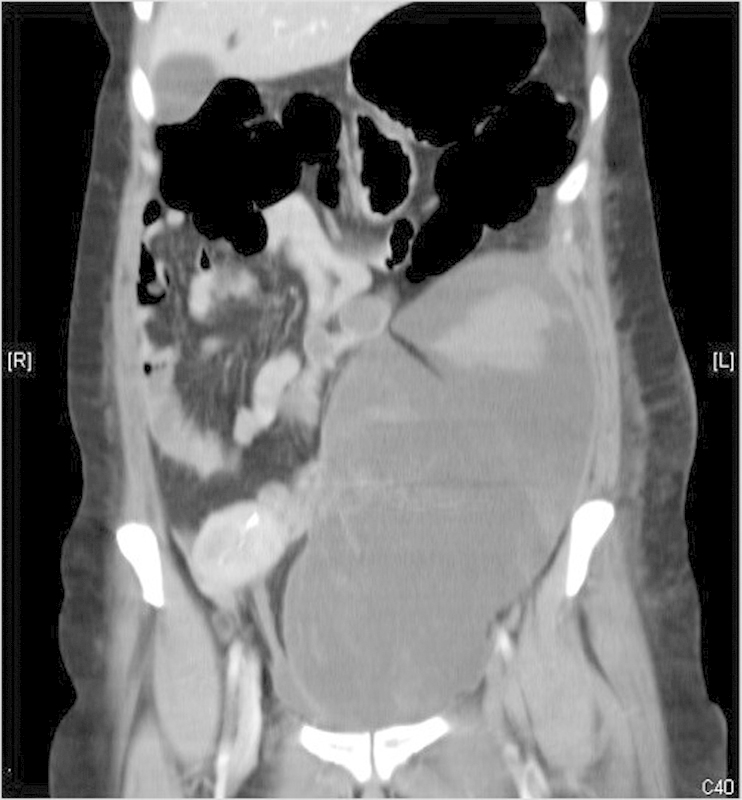
Large retroperitoneal hematoma requiring drainage and exploration.
Fig. 4.
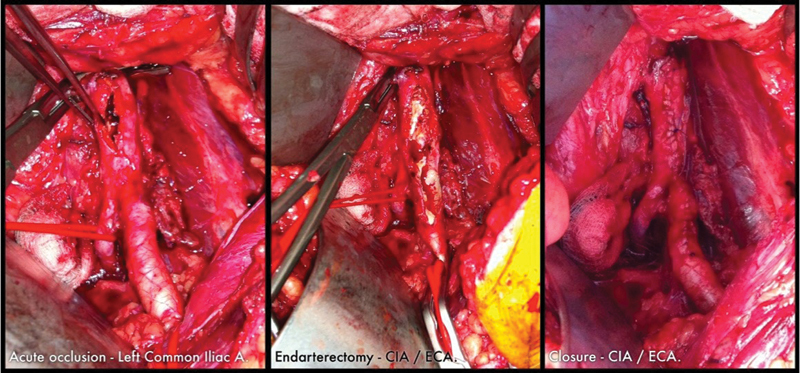
Left common iliac artery: acute occlusion and thrombectomy. Abbreviations: CIA, common iliac artery; ECA, external carotid artery.
There were no intraoperative visceral injuries. One patient with a known background of diverticular disease sustained an acute bowel obstruction requiring laparotomy 13 days post-ALIF surgery. Three patients (1.3%) had an incisional hernia requiring revision surgery; 7 (3.1%) patients had prolonged ileus (>7 days), which was managed conservatively. Four patients described retrograde ejaculation, 3 of which had resolved within 3 months of surgery. Sympathetic dysfunction occurred in 15 (6.6%) patients, manifesting as left-sided leg warmth and/or swelling. These symptoms resolved within 6 months in all cases. There were 5 (2.2%) cases of superficial wound infection treated with oral antibiotics, with no deep wound infections requiring reoperation or intravenous therapy.
All the patients with major complications requiring early return to the operative theater had a good outcome (two cases of postoperative hematoma and one case of arterial obstruction). There were no mortalities in this series.
Discussion
ALIF is a well-established and increasingly utilized procedure for treating a range of lumbar spinal pathologies. Its continued uptake among spinal surgeons may be limited by the perceived seriousness of the potential complications, in particular major vascular injury. Our results corroborate those of previous studies showing that such complications are uncommon, and major harm can be minimized by the implementation of a team approach including a vascular-trained access surgeon accompanying the spinal surgeon.
Approach
Our study reports the experience with a solely retroperitoneal approach, which has been shown to have a major advantage of reduced incidence of retrograde ejaculation in male patients when compared with the transperitoneal laparoscopic approach.19 This result has been attributed to the proximity of the superior hypogastric plexus to the posterior peritoneum, and as such, authors including Than et al have advised against the use of this approach in male patients.7 On the contrary, however, is a series of 104 (53 male) patients described by Asha et al who used an open transperitoneal approach with no instances of retrograde ejaculation.17 Similarly, they had very low rates of vascular complications but did report a high proportion of paralytic ileus. As such, there remains much scope for further investigation in comparing trans- and retroperitoneal approaches to the lumbar spine.
Vascular Injury
The rates of vascular injury reported here are acceptably low, comparable to those published in the available literature (Table 1). Higher rates of both major and minor vascular complications occur in operations performed at the L4–L5 level and above, due to the need for retraction and mobilization of the iliac and major vessels.14 Prolonged retraction and occlusion of the left internal iliac artery attribute to the uncommon but potentially serious complication of acute arterial thrombosis.13 We have experienced this complication on one occasion; it was detected on early postoperative review, and thrombectomy was performed acutely with an excellent result. The combination of a spine surgeon and a vascular surgeon working in combination has resulted in very low rates of total blood loss for both single-level and multilevel procedures.
Learning Curve
As with any operation that has technique- and approach-related issues, a learning curve is encountered. In our series, the majority of the complications were in the initial 100 patients performed. Both retroperitoneal hematomas and 3 of 4 cases of retrograde ejaculation were in the initial 100 cases performed. Techniques to reduce potential postoperative hematomas and retrograde ejaculation have resulted in a substantial reduction in these complications in the later ALIF procedures in this series.
Combined Vascular Surgeon and Spine Surgeon
There are many benefits of a combined vascular surgeon and spine surgeon approach. The operative times are relatively short as compared with previously documented studies (Table 1), as the approach is performed by a surgeon specializing in the manipulation and mobilization of the vessels, therefore reducing the overall operative time. If bleeding is encountered, rapid control of the bleeding and efficient repair of the vessel are achieved with the dual surgical approach.
Although some have documented the success rates of ALIF surgery performed by a single surgeon, we recommend the shared surgical responsibility, with each surgeon performing the aspects of the ALIF surgery corresponding to training and skill level.14 Considering the current high rates of legal action with surgical misfortune, the combined team approach will most likely reduce surgical risk and issues of litigation.
Tricks/Techniques to Minimize Vascular and Abdominal Injury
All patients had a preoperative vascular assessment and mapping of their peripheral pulses for postoperative monitoring of perfusion. Intraoperative toe oximetry was not performed, and vascular retraction was limited to an amount required to give adequate exposure to perform the diskectomy and implant insertion. When venous injury occurred, the most important method of vascular control was direct pressure over the vein prior to attempt to extend the surgical field, as extra retraction against the vessel can result in extension of the laceration and further uncontrollable hemorrhage. Bleeding was often encountered on the posterior aspect of the vein as it was retracted by the lip of the retractor blade and careful exposure was required. A continuous 5–0 suture repair was used to control the bleeding.
Over time and with experience, the treating surgeons have adopted the following techniques to reduce the complication rate:
L5–S1 Level
Peanuts. A small compacted cotton pledget in the jaws of a curved hemostatic forcep is used to reduce the risk of retrograde ejaculation. Also, peanuts are used for blunt dissection on the anterior longitudinal ligament and disk, rather than monopolar diathermy, to clear the anterior aspect of the L5–S1 disk space.
Median sacral artery and vein. The median sacral artery and vein are routinely divided using either vascular clip or loop tie. There may be multiple vessels anterior to the L5–S1 disk space, however, and all need to be divided prior to diskectomy.
Right-sided approach. For cases where there is a high likelihood of further surgery at the L4–L5 level, thought should be given to a right-sided approach to provide ease of left-sided retroperitoneal access without retroperitoneal scarring should the L4–L5 level be approached at a future date.
L4–L5 Level
Iliolumbar vein. We now routinely divide the iliolumbar vein due to risk of a retraction tear of this vessel, which allows for extended retraction of the left common iliac vein. Repair of the iliolumbar vein can be very difficult as the distal aspect of the divided vessel can retract, with significant blood loss.
Sympathetic trunk. We do not use diathermy in the vicinity of the sympathetic trunk; we use blunt dissection only to dissect laterally on the disk space.
L2–L3 and L3–L4 Levels
Preoperative angiogram. With higher-level ALIF procedures, we routinely perform computed tomography angiography with three-dimensional vascular reconstruction to assess the renal arterial anatomy, as aberrant lower pole renal arteries are present in up to 5% of patients and could be encountered at this level.
Conclusion
ALIF is a safe procedure when performed by a team consisting of a vascular surgeon and a spine surgeon, with acceptably low complication rates. Our series confirms that the team approach to this procedure results in short operative times, short length of stay, rapid control of intraoperative vessel injury, low overall blood loss, and shared surgical responsibility with benefits to overall patient outcomes.
Footnotes
Disclosures Ralph J. Mobbs, Payment for lectures: Stryker Spine, Synthes; Royalties: Stryker Spine; Stock/stock options: Medtronic, J&J; Travel expenses: Orthotec Kevin Phan, none Daniel Daly, none Prashanth J. Rao, none Andrew Lennox, none
References
- 1.Capener N. Spondylolisthesis. Br J Surg. 1932;19(75):374–386. [Google Scholar]
- 2.Ito H, Tsuchiya J, Asami G. A new radical operation for Pott's disease. J Bone Joint Surg. 1934;16:499–515. [Google Scholar]
- 3.Mobbs R J, Loganathan A, Yeung V, Rao P J. Indications for anterior lumbar interbody fusion. Orthop Surg. 2013;5(3):153–163. doi: 10.1111/os.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim N H, Kim H K, Suh J S. A computed tomographic analysis of changes in the spinal canal after anterior lumbar interbody fusion. Clin Orthop Relat Res. 1993;(286):180–191. [PubMed] [Google Scholar]
- 5.Pradhan B B, Nassar J A, Delamarter R B, Wang J C. Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech. 2002;15(5):355–361. doi: 10.1097/00024720-200210000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Mummaneni P V, Haid R W, Rodts G E. Lumbar interbody fusion: state-of-the-art technical advances. Invited submission from the Joint Section Meeting on Disorders of the Spine and Peripheral Nerves, March 2004. J Neurosurg Spine. 2004;1(1):24–30. doi: 10.3171/spi.2004.1.1.0024. [DOI] [PubMed] [Google Scholar]
- 7.Than K D, Wang A C, Rahman S U. et al. Complication avoidance and management in anterior lumbar interbody fusion. Neurosurg Focus. 2011;31(4):E6. doi: 10.3171/2011.7.FOCUS11141. [DOI] [PubMed] [Google Scholar]
- 8.Min J H, Jang J S, Lee S H. Comparison of anterior- and posterior-approach instrumented lumbar interbody fusion for spondylolisthesis. J Neurosurg Spine. 2007;7(1):21–26. doi: 10.3171/SPI-07/07/021. [DOI] [PubMed] [Google Scholar]
- 9.Scaduto A A, Gamradt S C, Yu W D, Huang J, Delamarter R B, Wang J C. Perioperative complications of threaded cylindrical lumbar interbody fusion devices: anterior versus posterior approach. J Spinal Disord Tech. 2003;16(6):502–507. doi: 10.1097/00024720-200312000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Burke P J. Anterior lumbar interbody fusion. Radiol Technol. 2001;72(5):423–430. [PubMed] [Google Scholar]
- 11.Strube P, Hoff E, Hartwig T, Perka C F, Gross C, Putzier M. Stand-alone anterior versus anteroposterior lumbar interbody single-level fusion after a mean follow-up of 41 months. J Spinal Disord Tech. 2012;25(7):362–369. doi: 10.1097/BSD.0b013e3182263d91. [DOI] [PubMed] [Google Scholar]
- 12.Kim J S, Kim D H, Lee S H. et al. Comparison study of the instrumented circumferential fusion with instrumented anterior lumbar interbody fusion as a surgical procedure for adult low-grade isthmic spondylolisthesis. World Neurosurg. 2010;73(5):565–571. doi: 10.1016/j.wneu.2010.02.057. [DOI] [PubMed] [Google Scholar]
- 13.Brau S A, Delamarter R B, Schiffman M L, Williams L A, Watkins R G. Vascular injury during anterior lumbar surgery. Spine J. 2004;4(4):409–412. doi: 10.1016/j.spinee.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 14.Chiriano J, Abou-Zamzam A M Jr, Urayeneza O, Zhang W W, Cheng W. The role of the vascular surgeon in anterior retroperitoneal spine exposure: preservation of open surgical training. J Vasc Surg. 2009;50(1):148–151. doi: 10.1016/j.jvs.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 15.Inamasu J, Guiot B H. Vascular injury and complication in neurosurgical spine surgery. Acta Neurochir (Wien) 2006;148(4):375–387. doi: 10.1007/s00701-005-0669-1. [DOI] [PubMed] [Google Scholar]
- 16.Oskouian R J Jr Johnson J P Vascular complications in anterior thoracolumbar spinal reconstruction J Neurosurg 200296(1, Suppl):1–5. [DOI] [PubMed] [Google Scholar]
- 17.Asha M J, Choksey M S, Shad A, Roberts P, Imray C. The role of the vascular surgeon in anterior lumbar spine surgery. Br J Neurosurg. 2012;26(4):499–503. doi: 10.3109/02688697.2012.680629. [DOI] [PubMed] [Google Scholar]
- 18.Papastefanou S L, Stevens K, Mulholland R C. Femoral nerve palsy. An unusual complication of anterior lumbar interbody fusion. Spine (Phila Pa 1976) 1994;19(24):2842–2844. [PubMed] [Google Scholar]
- 19.Kaiser M G Haid R W Jr Subach B R Miller J S Smith C D Rodts G E Jr Comparison of the mini-open versus laparoscopic approach for anterior lumbar interbody fusion: a retrospective review Neurosurgery 200251197–103., discussion 103–105 [DOI] [PubMed] [Google Scholar]
- 20.Paik N C. Incisional hernia after anterior lumbar interbody fusion. Spine J. 2010;10(9):844. doi: 10.1016/j.spinee.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 21.Rajaraman V, Heary R F, Livingston D H. Acute pancreatitis complicating anterior lumbar interbody fusion. Eur Spine J. 2000;9(2):171–173. doi: 10.1007/s005860050230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hresko M T, Hall J E. Latent psoas abscess after anterior spinal fusion. Spine (Phila Pa 1976) 1992;17(5):590–593. doi: 10.1097/00007632-199205000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Chan F L, Chow S P. Retroperitoneal fibrosis after anterior spinal fusion. Clin Radiol. 1983;34(3):331–335. doi: 10.1016/s0009-9260(83)80354-7. [DOI] [PubMed] [Google Scholar]
- 24.Lazio B E, Staab M, Stambough J L, Hurst J M. Latissimus dorsi rupture: an unusual complication of anterior spine surgery. J Spinal Disord. 1993;6(1):83–86. [PubMed] [Google Scholar]
- 25.Sasso R C, Best N M, Mummaneni P V, Reilly T M, Hussain S M. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 2005;30(6):670–674. doi: 10.1097/01.brs.0000155423.18218.75. [DOI] [PubMed] [Google Scholar]
- 26.Rajaraman V Vingan R Roth P Heary R F Conklin L Jacobs G B Visceral and vascular complications resulting from anterior lumbar interbody fusion J Neurosurg 199991(1 Suppl):60–64. [DOI] [PubMed] [Google Scholar]
- 27.Mayer H M Wiechert K Microsurgical anterior approaches to the lumbar spine for interbody fusion and total disc replacement Neurosurgery 200251(5 Suppl):S159–S165. [PubMed] [Google Scholar]
- 28.Bianchi C, Ballard J L, Abou-Zamzam A M, Teruya T H, Abu-Assal M L. Anterior retroperitoneal lumbosacral spine exposure: operative technique and results. Ann Vasc Surg. 2003;17(2):137–142. doi: 10.1007/s10016-001-0396-x. [DOI] [PubMed] [Google Scholar]
- 29.Saraph V, Lerch C, Walochnik N, Bach C M, Krismer M, Wimmer C. Comparison of conventional versus minimally invasive extraperitoneal approach for anterior lumbar interbody fusion. Eur Spine J. 2004;13(5):425–431. doi: 10.1007/s00586-004-0722-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gumbs A A, Shah R V, Yue J J, Sumpio B. The open anterior paramedian retroperitoneal approach for spine procedures. Arch Surg. 2005;140(4):339–343. doi: 10.1001/archsurg.140.4.339. [DOI] [PubMed] [Google Scholar]
- 31.Fantini G A, Pappou I P, Girardi F P, Sandhu H S, Cammisa F P Jr. Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine (Phila Pa 1976) 2007;32(24):2751–2758. doi: 10.1097/BRS.0b013e31815a996e. [DOI] [PubMed] [Google Scholar]
- 32.Hamdan A D, Malek J Y, Schermerhorn M L, Aulivola B, Blattman S B, Pomposelli F B Jr. Vascular injury during anterior exposure of the spine. J Vasc Surg. 2008;48(3):650–654. doi: 10.1016/j.jvs.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 33.Chiriano J, Abou-Zamzam A M Jr, Urayeneza O, Zhang W W, Cheng W. The role of the vascular surgeon in anterior retroperitoneal spine exposure: preservation of open surgical training. J Vasc Surg. 2009;50(1):148–151. doi: 10.1016/j.jvs.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 34.Garg J, Woo K, Hirsch J, Bruffey J D, Dilley R B. Vascular complications of exposure for anterior lumbar interbody fusion. J Vasc Surg. 2010;51(4):946–950. doi: 10.1016/j.jvs.2009.11.039. [DOI] [PubMed] [Google Scholar]


