Abstract
Suicidal thoughts and behaviors are highly prevalent public health problems with devastating consequences. There is an urgent need to improve our understanding of risk factors for suicide to identify effective intervention targets. The aim of this meta-analysis was to examine the magnitude and clinical utility of anxiety and its disorders as risk factors for suicide ideation, attempts, and deaths. We conducted a literature search through December 2014; of the 65 articles meeting our inclusion criteria, we extracted 180 cases in which an anxiety-specific variable was used to longitudinally predict a suicide-related outcome. Results indicated that anxiety is a statistically significant, yet weak, predictor of suicide ideation (OR=1.49, 95% CI: 1.18, 1.88) and attempts (OR=1.64, 95% CI: 1.47, 1.83), but not deaths (OR=1.01, 95% CI: 0.87, 1.18). The strongest associations were observed for PTSD. Estimates were reduced after accounting for publication bias, and diagnostic accuracy analyses indicated acceptable specificity but poor sensitivity. Overall, the extant literature suggests that anxiety and its disorders, at least when these constructs are measured in isolation and as trait-like constructs, are relatively weak predictors of suicidal thoughts and behaviors over long follow-up periods. Implications for future research priorities are discussed.
Keywords: Suicide, Anxiety, Risk factor, Meta-analysis
1. Introduction
Suicidal behavior is a leading cause of injury and death across the globe (Centers for Disease Control and Prevention, 2011), with upwards of one million individuals who take their own lives annually (World Health Organization, 2012). In the United States alone, over 40,000 people die by suicide each year. In addition to completed suicides, approximately 3% of individuals make a suicide attempt during their lifetime (Borges et al., 2010; Nock et al., 2008). It is also estimated that approximately 9% of people report experiencing serious thoughts of suicide during their lives. Unfortunately, the U.S. suicide rate has risen steadily over the past decade (Centers for Disease Control and Prevention, 2011) and is projected to continue increasing over upcoming years (Mathers & Loncar, 2006).
One promising avenue toward reducing the global impact of suicide is to identify risk factors that predict suicidal thoughts and behaviors. Risk factors are not to be confused with correlates; whereas correlates represent concomitants or consequences of a phenomenon of interest and can be identified through cross-sectional methods, establishing risk factors necessitates longitudinal designs (Kraemer et al., 1997). For example, from a study showing that individuals who attempt suicide are more likely to be diagnosed with an anxiety disorder than those who do not attempt suicide, one may conclude that anxiety is a correlate of suicidal behavior. However, to determine that anxiety functions as a risk factor for suicidal behavior, it would need to be established that anxiety disorders precede and heighten future risk for suicide attempts. Establishing risk factors for suicidality is essential for a number of reasons, including improved understanding of underlying mechanisms, identification of at-risk individuals, and development of evidence-based prevention and treatment programs. Most previous studies have focused exclusively on correlates, which are unlikely to be as informative for prediction and intervention purposes. Accordingly, the primary goal of this study was to conduct a meta-analytic review of prospective studies that have evaluated anxiety and its disorders as risk factors for suicidal thoughts and behaviors. In a narrative review, it can be difficult to provide a comprehensive account of all relevant studies, reconcile contradictory findings, account for methodological variations across the literature, and ascertain overall magnitudes of risk factors under investigation. A meta-analysis can overcome these limitations, and thus would be very helpful in summarizing current knowledge about anxiety as a risk factor for suicidality.
There are several reasons why we chose to focus on anxiety in this meta-analysis. First, anxiety and its disorders are listed as important risk factors for suicide by a number of national organizations (e.g., American Association of Suicidology, 2015; American Foundation for Suicide Prevention, 2015; National Suicide Prevention Lifeline, 2015). Determining the strength of empirical evidence to support this information, which is widely disseminated to clinicians, researchers, and the public, is necessary.
Second, anxiety is implicated in many prominent theories of suicide. For example, according to Beck's cognitive model of suicide, once a suicide schema is activated, anxiety (and agitation) can serve as an expression of attentional fixation on suicide, which interacts with hopelessness to increase suicide risk (e.g., Wenzel & Beck, 2008; Wenzel, Brown, & Beck, in press). Although anxiety is not explicitly addressed in Joiner's interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010), this model's emphasis on the fearsome nature of suicidal behavior is consistent with evidence showing that acute anxious states (e.g., heightened arousal/agitation, severe panic attacks) are often present immediately prior to lethal or near-lethal suicidal acts (e.g., Britton, Ilgen, Rudd, & Conner, 2012; Busch, Fawcett, & Jacobs, 2003; Conrad et al., 2009; Fawcett et al., 1990; Hall, Platt, & Hall, 1999; Ribeiro et al., 2015; Ribeiro, Silva, & Joiner, 2014). These findings align with Fawcett's influential conceptualizations of anxiety/agitation as a determinant for acute suicide risk (e.g., Fawcett, 2001; Fawcett, Busch, Jacobs, Kravitz, & Fogg, 1997), and expert clinical consensus identifying agitation as a “warning sign” for suicide (e.g., Rudd et al., 2006). Furthermore, Baumeister (1990) conceptualizes suicide as the ultimate escape from aversive self-awareness and associated negative affect, which often includes anxiety. Along similar lines, Riskind and colleagues have theorized that a specific cognitive risk factor for anxiety (looming vulnerability), when coupled with hopelessness, enhances urges to escape psychological pain and elevates risk for suicide (e.g., Rector, Kamkar, & Riskind, 2008; Riskind, 1997; Riskind, Long, Williams, & White, 2000).
Third, anxiety and related disorders (broadly defined here as anxiety, obsessive–compulsive, trauma and stressor-related, and somatic symptom disorders) have received theoretical and empirical attention as potential risk factors for suicide. First and foremost, these disorders are characterized by aversive, avoidant reactions to emotional experiences (Barlow, Sauer-Zavala, Carl, Bullis, & Ellard, 2014). Suicidal thoughts and behaviors have similarly been conceptualized as avoidant or escape-based responses to the experience of strong emotions (Baumeister, 1990; Boergers, Spirito, & Donaldson, 1998; Briere, Hodges, & Godbout, 2010; Bryan, Rudd, & Wertenberger, 2013; Shneidman, 1993), highlighting the potential functional similarities of these phenomena. Further, behavioral avoidance, a hallmark feature of anxiety disorders, often results in significant isolation, reduced quality of life, and impaired functioning (e.g., Massion, Warshaw, & Keller, 1993; Olatunji, Cisler, & Tolin, 2007), which confer additional risk to suicidality (Kanwar et al., 2013; Kaplan, McFarland, Huguet, & Newsom, 2007). Other avoidance strategies (e.g., suppression) often used by individuals with an anxiety disorder have also been shown to exacerbate vulnerability to suicidal thoughts and behaviors (Amir, Kaplan, Efroni, & Kotler, 1999).
In addition to promising theoretical relevance of anxiety disorders to suicidality, empirical investigations of this relationship generally show that anxiety disorders are independently associated with suicidal thoughts and behaviors. Although several earlier studies indicated that anxiety disorders are not related to suicidality (e.g., Hornig & McNally, 1995; Warshaw, Massion, Peterson, Pratt, & Keller, 1995), converging empirical evidence suggests that a broad range of anxiety and related disorders (including panic disorder, posttraumatic stress disorder [PTSD], social anxiety disorder, and generalized anxiety disorder [GAD]) function as statistically significant risk factors for suicidal thoughts and behaviors (Boden, Fergusson, & Horwood, 2007; Bolton et al., 2008; Borges, Angst, Nock, Ruscio, & Kessler, 2008; Gradus et al., 2010; Nepon, Belik, Bolton, & Sareen, 2010; Nock et al., in press, 2009, 2010a; Noyes, 1991; Sareen, 2011; Sareen et al., 2005; Thibodeau, Welch, Sareen, & Asmundson, 2013; Weissman, Klerman, Markowitz, & Ouellette, 1989; Wilcox, Storr, & Breslau, 2009).
For example, Nock and colleagues (2010a) observed that anxiety disorders significantly predicted future suicide attempts in a large, nationally representative sample (N = 9282), when controlling for psychiatric comorbidity. Indeed, anxiety disorders produced larger population attributable risk proportions (PARPs), which take into account the prevalence of predictors and distribution of comorbidity, for suicide ideation and attempts than impulse-control and substance use disorders. Among suicide ideators, anxiety disorders played a larger role than mood disorders, impulse-control disorders, and substance use disorders in accounting for subsequent suicide attempts. Findings from a cross-national study by Nock and colleagues (2009) are similar, with anxiety serving as a more powerful predictor of suicide attempts among ideators than mood, impulse-control, and substance use disorders. A recent meta-analysis of 42 studies further supports the notion that anxiety disorders and suicidal behavior are related (Kanwar et al., 2013); however, by including a combination of cross-sectional and longitudinal studies, the conclusions that can be drawn from this previous meta-analysis regarding anxiety (and specific disorders) as risk factors are tempered.
In summary, researchers, theorists, and clinicians have evidenced a longstanding interest in the role of anxiety and its disorders in suicide. A meta-analysis of longitudinal studies is necessary to synthesize the available literature on anxiety as a risk factor for suicidal thoughts and behaviors. Specifically, we aimed to: (1) estimate the predictive power (i.e., risk factor magnitude and accuracy) of anxiety as a risk factor for suicide-related outcomes, (2) compare the strength of effect sizes across types of anxiety (e.g., disorders, symptoms), and (3) examine potential moderators of the association between anxiety and suicide-related outcomes, including sample type, sample age, and length of follow-up period. To our knowledge, this represents the first effort to provide a comprehensive, quantitative review of the predictive ability of anxiety and its disorders for suicidal thoughts and behaviors.
2. Method
This meta-analysis complies with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement (PRISMA; Moher, Liberati, Tetzlaff, & Altman, 2009).
2.1. Search strategy and selection
We conducted a comprehensive literature search of PsycINFO, PubMed, and Google Scholar from database inception through December 2014 to identify studies eligible for the current review. The prediction-related terms longitudinal, longitudinally, predicts, prediction, prospective, prospectively, future, later, and follow-up were entered simultaneously with the self-injury-related terms self-injury, suicidality, self-harm, suicide, suicidal behavior, suicide attempt, suicide death, suicide plan, suicide thoughts, suicide ideation, suicide gesture, suicide threat, self-mutilation, self-cutting, cutting, self-burning, self-poisoning, deliberate self-harm, DSH, nonsuicidal self-injury, and NSSI. Given the inconsistent and ambiguous terminology used to describe self-injury (with or without suicidal intent) in the literature (Nock, 2010), we employed a wide range of self-injury-related terms to reduce the likelihood of missing relevant studies. The reference sections of identified articles were also searched for other relevant publications.
Fig. 1 presents a PRISMA diagram of the study selection process. A total of 2385 unique publications were identified by initial literature searches; after reviewing each abstract, 642 studies were deemed eligible for further review. The authors then reviewed each full-text study and identified 65 publications that met criteria for inclusion in the meta-analysis (see Appendix A for references for articles included in meta-analyses).
Fig. 1.
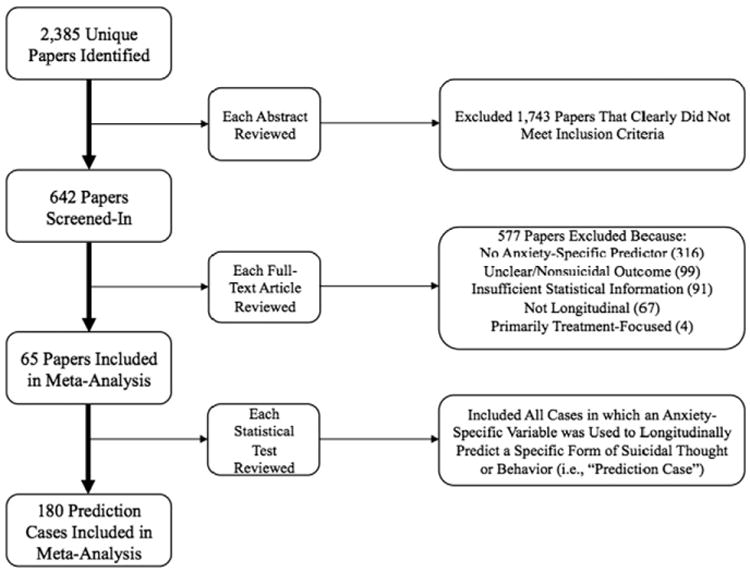
PRISMA diagram.
2.2. Inclusion and exclusion criteria
To be included in this meta-analysis, studies had to first include a longitudinal analysis predicting one or more of the following suicide-related outcomes: suicide ideation, suicide plan, suicide gesture, suicide attempt, or suicide death. Correspondingly, we excluded studies with outcomes that included nonsuicidal self-injury (NSSI) only. We also excluded studies that lumped nonsuicidal and suicidal behavior together into a single outcome (e.g., “deliberate self-harm”) because including these combined variables would render it difficult to draw strong conclusions about the association between anxiety and suicidal outcomes specifically. Second, included studies had to use one or more of the following anxiety-specific predictors: any individual anxiety diagnosis (i.e., agoraphobia, anxiety disorder not otherwise specified, GAD, panic disorder, social anxiety disorder, specific phobia) or anxiety diagnosis grouping (e.g., “any anxiety disorder” as defined by study authors), any obsessive–compulsive or related disorder (e.g., OCD), any trauma or stressor-related disorder (e.g., adjustment disorder, PTSD), any somatic symptom disorder, symptoms of anxiety (diagnosis-specific and general; e.g., scores on self-report and clinician-rated measures such as the Beck Anxiety Inventory [BAI; Beck, Epstein, Brown, & Steer, 1988], Hamilton Anxiety Rating Scale [HARS; Hamilton, 1959], or Yale-Brown Obsessive Compulsive Scale [Y-BOCS; Goodman et al., 1989], panic attacks). Correspondingly, we excluded studies only examining constructs or symptoms broadly related but not specific to anxiety (e.g., neuroticism, negative affect, emotion dysregulation). We also excluded studies combining anxiety and mood disorders into a single variable (e.g., internalizing problems, “mood or anxiety diagnosis”) because including these overlapping predictors would undermine our conclusions regarding the specific effect of anxiety on suicidal thoughts and behaviors. Finally, studies had to provide sufficient statistical information to conduct the present analyses, appear in a publication, and present original data not already reported in another study.
2.3. Data abstraction
Authors systematically extracted relevant information from each article included in the present meta-analysis using a predefined coding strategy. Recorded information included: (a) year of study publication, (b) sample age (i.e., adult, adolescent, mixed), (c) sample size, (d) sample type (i.e., general, clinical, or history of prior SITBs), (e) length of study follow-up (in months), (f) statistical information for each unique prediction case (i.e., any instance using an anxiety-specific variable to longitudinally predict a suicide-related outcome), and (g) whether the prediction case was hypothesized to be a risk or protective factor (e.g., no psychopathology, reduction in anxiety). Whenever possible, we used the most unadjusted estimate(s) or extracted raw diagnostic data for our meta-analytic calculations; of note, only 10% of cases included our analyses were coded as adjusted (e.g., controlling for related variables such as age, gender, etc.).
2.4. Data analysis
Our outcomes of interest were suicidal thoughts and behaviors (i.e., suicide ideation, suicide attempt, suicide death); due to the fact that only one study reported on suicide gestures and plans (Borges et al., 2008), we did not conduct any analyses specific to these outcomes. Our predictors of interest were anxiety-specific constructs. From each study, we extracted relevant statistics (e.g., zero-order correlation, 2 × 2 contingency table, odds ratio, hazard ratio, independent group means) for each unique predictor case. Protective factor cases (i.e., when a variable could be reasonably assumed to correspond to a reduction in risk for future suicidal behavior, such as absence of PTSD) and redundant cases (e.g., a non-unique case reported in two studies using the same sample) were removed. In addition, when one publication reported cases using the same predictor and outcome at multiple time points, we selected only the longest time point to reduce data dependency. Accordingly, we removed 6 cases, which resulted in a total of 180 unique prediction cases used in this review.
Prior to conducting our meta-analytic analyses, all relevant study statistics were converted to ORs and their 95% confidence interval (CI) in the program Comprehensive Meta-Analysis (CMA, Version 2; Borenstein, Hedges, Higgins, & Rothstein, 2005). Cases that reported hazard ratio (HRs) and lacked the raw data necessary to be converted to ORs were analyzed separately. We used random-effects models (Field, 2001; Hedges & Olkin, 1985; Hedges & Vevea, 1998) for all calculations. These models assume that reported effect sizes across studies represent a random sampling of studies distributed around a true effect size for the population whereas the assumption of fixed effects models is that included studies reflect the true population effect size. Thus, we chose random-effects models to take into account both between- and within-study heterogeneity across the publications included in our meta-analysis.
First, we pooled all ORs from included studies to estimate overall effect sizes for any anxiety construct (i.e., any type of anxiety diagnosis and symptoms) predicting suicide ideation, attempt, and death. Then, we estimated effect sizes for anxiety symptoms (e.g., total scores on diagnosis-specific or general anxiety measures, panic attacks), excluding anxiety diagnoses, on the same suicide-related outcomes. Next, we estimated effect sizes for any type of anxiety diagnosis (i.e., adjustment disorder, agoraphobia, anxiety disorder not otherwise specified, GAD, OCD, panic disorder, PTSD, social anxiety disorder, somatic symptom disorder, specific phobia, “any anxiety diagnosis” as defined by the study authors) predicting suicide-related outcomes. Finally, we conducted diagnosis-specific analyses for the following individual diagnoses on suicide ideation, attempt, and death: adjustment disorder, agoraphobia, GAD, OCD, panic disorder, PTSD, social anxiety disorder, somatic symptom disorder, and specific phobia. Diagnosis-specific analyses were not conducted for anxiety disorder not otherwise specified because there was only one case using this particular diagnosis. A total of 20 cases used HRs only, which all predicted either attempt or death. We pooled these cases separately to estimate overall effect sizes for any anxiety construct predicting suicide attempt and then death.
Several tests were used to assess for potential publication bias in our meta-analysis. First, Orwin's fail-safe N was used to estimate the number of missing studies with ORs of 1.00 necessary to lower the magnitude of observed overall effect sizes to a negligible value; for these analyses, we set the alternative OR to 1.01. We also employed Egger's test of the intercept, which uses precision (i.e., inverse of the standard error) to predict the standardized effect (i.e., effect size divided by the standard error). In Egger's equation, the slope of the regression line indicates the size of the effect and the intercept indicates bias. Last, we used a funnel plot, which depicts the standard error of each included study on the vertical axis relative to the effect size magnitude on the horizontal axis. When studies are symmetrically dispersed around the combined mean effect size, it is likely the meta-analysis captured all relevant studies, whereas an asymmetrical distribution of studies indicates publication bias. Duval and Tweedie's Trim and Fill test was used to quantify the nature of publication bias. Specifically, this analysis identifies the number of studies missing due to publication bias, estimates the effects of these missing studies, adds the unpublished studies to the analysis, and re-estimates the overall effect size estimate. Should the initial and re-estimated ORs significantly differ, one can conclude that the effect observed in the meta-analysis is biased.
The program MetaDiSc Version 1.4 (Zamora, Muriel, & Abraira, 2014) and random-effects models were used to conduct diagnostic accuracy analyses in order to provide detail in addition to overall ORs regarding patterns of included data. Our diagnostic accuracy statistics involved generating sensitivity (true positive rate; e.g., of all individuals who attempt suicide, the percentage that we would predict will make an attempt based on the presence of an anxiety disorder) and specificity (true negative rate; e.g., of all individuals who do not attempt suicide, the percentage that we would predict will not make an attempt based on the absence of an anxiety disorder) values. We also generated receiver operating characteristic (ROC) curves, which plots the sensitivity against the false positive rate (1 — specificity) for each prediction case; areas under the curve (AUCs) and corresponding standard errors were then calculated and used as our primary indicator of diagnostic accuracy. We adhered to the following guidelines in interpreting AUCs: >.90 suggesting excellent prediction, .80–.89 good prediction, .70–.79 fair prediction, .61–.69 poor prediction, and .50–.59 extremely poor prediction (Šimundić, 2008).
To be included in diagnostic accuracy analyses, prediction cases had to provide raw data that could be converted into a 2 × 2 table with cells that indicate true positive, false positive, true negative, and false negative events. Whenever possible, raw data was obtained to maximize the number of prediction cases included in these analyses. Given the limited number of prediction cases for suicide ideation that provided sufficient information to run these analyses, diagnostic accuracy estimates were computed for outcomes of suicide attempt and death only. For suicide attempt, 39 prediction cases (spanning all anxiety constructs) were included, and for death, 26 cases (also spanning all anxiety constructs) were included in diagnostic accuracy analyses.
We used the I2 statistic to examine heterogeneity within the meta-analysis, thereby justifying our use of random-effects models, which, as previously noted, account for important methodological variations across studies. An I2 statistic >50 indicates high variance in observed effect sizes (Higgins, Thompson, Deeks, & Altman, 2003) and suggests that characteristics of individual studies should be examined as potential moderators of the observed effects of anxiety on suicide-related outcomes. The following variables were tested as potential moderators: sample type (i.e., general, clinical, history of self-injurious thoughts or behaviors [SITBs]), sample age (i.e., adult, adolescent, mixed), and length of follow-up period. For categorical variables (sample type and sample age), we examined the magnitude of effect size estimates for any anxiety construct predicting suicide ideation, attempt, and death at each level of the potential moderator. We treated length of follow-up period as a continuous variable, and employed unrestricted maximum likelihood meta-regression using a random effects model to estimate the effect of length of follow-up period on the predictive ability of anxiety. For these analyses, we used R2 as an indicator of moderator strength.
3. Results
3.1. Description of included studies
Characteristics of studies are presented in Table 1. Years of publication spanned 1982 to 2015. The 65 included articles yielded a total of 69 samples, as four publications reported data separately for males and females (i.e., Berglund & Nilsson, 1987; Lewinsohn et al.,2001; Reinherz et al.,1995; Tidemalm et al., 2014). Across all samples, there were a total of 852,159 participants. The median number of participants per study was 249 (M = 12,350, SD = 44,712, range = 26–309,861). Just over half of samples (52.2%) were classified as clinical (e.g., psychiatric patients), whereas 26.1% were drawn from the general community and 21.7% included only individuals with a history of prior SITBs. One study (Borges et al., 2008) used a combination of community-based participants and those with a SITB history. The majority of studies (71.0%) utilized adult samples; 21.7% of studies were conducted in adolescent-only samples and only 5 studies (7.2%) used mixed samples. Over half of included studies (55.1%) utilized samples from countries outside North America, most commonly in Europe.
Table 1.
Description of included studies.
| Author(s), year | Total N | Sample typea | Sample populationb | Length of follow-up (in months) | Anxiety predictor(s) | Suicide-related outcome(s) |
|---|---|---|---|---|---|---|
| Allgulander et al. (1992) | 80,790 Swedish discharged inpatients | Clinical | Adolescent and adult | 168 | Anxiety neurosisc | Death |
| Alonso et al. (2010) | 218 Spanish psychiatric patients | Clinical | Adult | 120 | OCD duration and symptoms | Attempt |
| Angst & Calyton (1998) | 62 deceased Swiss males from general community | General | Adult | 204 | Any anxiety diagnosis | Death |
| Bakken & Vaglum (2006) | 160 Norwegian patients with substance abuse | Clinical | Adult | 72 | AG, GAD, OCD, PTSD, SOC, SOM, SPEC | Attempt |
| Beautrais (2004) | 302 New Zealand patients with prior attempt | History of SITBs | Adolescent and adult | 60 | Any anxiety diagnosis | Attempt, death |
| Berglund (1984) | 1,312 Swedish inpatients with alcohol abuse | Clinical | Adult | 384 | Any anxiety diagnosis | Death |
| Berglund & Nilsson (1987) (a) | 700 Swedish female inpatients with mood disorder | Clinical | Adult | 324 | Any anxiety diagnosis | Death |
| Berglund & Nilsson (1987) (b) | 500 Swedish male inpatients with mood disorder | Clinical | Adult | 324 | Anxiety symptoms | Death |
| Blumenthal et al. (1989) | 36 German psychiatric patients | Clinical | Adult | 60 | Any anxiety diagnosis | Death |
| Bolton et al. (2010) | 5,972 general community | General | Adult | 36 | Any anxiety diagnosis, GAD, PD, PTSD, SOC, SPEC | Attempt |
| Borg & Ståhl (1982) | 68 Swedish psychiatric patients | General | Adult | 24 | Anxiety symptoms, OCD symptoms | Death |
| Borges et al. (2008) | 5,001 general community | General, History of SITBs | Adolescent and adult | 120 | Any anxiety diagnosis, AG, GAD, PD, PTSD, SOC, SPEC | Ideation, gesture, plan, attempt |
| Brådvik et al. (2010) | 85 Swedish general community | General | Adolescent and adult | 708 | ADJ, ANX-NOS, OCD, PDA, SOC, SOM | Death |
| Breslau et al. (2012) | 1,186 general community | General | Adult | 24 | Any anxiety diagnosis | Attempt |
| Britton, et al. (2012) | 381 veteran suicide descendents | History of SITBs | Adult | 1 | Anxiety symptoms | Death |
| Brown et al. (2000) | 6,891 psychiatric outpatients | Clinical | Adult | 288 | Anxiety symptoms, PD | Death |
| Bryan et al. (2014) | 176 veteran outpatients | History of SITBs | Adult | 14 | PTSD symptoms | Attempt |
| Cedereke & Öjehagen (2015) | 178 Swedish psychiatric patients | Clinical | Adult | 11 | ADJ | Attempt |
| Chan et al. (2014) | 66 inpatients with depression | Clinical | Adult | 12 | Any anxiety diagnosis | Attempt |
| Clarke et al. (2010) | 1,292 general community | General | Adult | 276 | Any anxiety diagnosis | Ideation |
| Conner et al. (2012) | 309,861 United States Air Force members | General | Adult | 72 | Any anxiety diagnosis | Death |
| Cougle et al. (2009) | 2,551 females in general community | General | Adult | 12 | PTSD | Ideation |
| Courtet et al. (2003) | 76 West European patients with prior attempt | History of SITBs | Adult | 12 | AG, GAD, PD, SOC | Attempt |
| Cullberg et al. (1988) | 163 Swedish general community with prior attempt | History of SITBs | Adult | 120 | ADJd | Death |
| Darke et al. (2005) | 495 Australian patients with substance use disorder | Clinical | Adult | 12 | PTSD | Attempt |
| Dennehy et al. (2011) | 4,360 patients with bipolar disorder | Clinical | Adult | 16 | Any anxiety diagnosis, PD | Attempt, death |
| Desai et al. (2005) | 121,933 Dept. of Veterans Affairs psychiatric patients | Clinical | Adult | 48 | PTSD | Death |
| Fawcett et al. (1990) | 954 inpatients with mood disorder | Clinical | Adult | 120 | Anxiety symptoms, OCD symptoms | Attempt |
| Flensborg-Madsen et al. (2009) | 18,146 general Danish community | General | Adult | 312 | Any anxiety diagnosis | Attempt |
| Fridell et al. (1996) | 42 Swedish inpatients with prior attempt | History of SITBs | Adult | 60 | Any anxiety diagnosis, ADJ | Attempt |
| Gallagher et al. (2014) | 144 inpatients | Clinical | Adolescent | 18 | Social anxiety symptoms | Ideation |
| Goldstein et al. (2011) | 413 patients with bipolar disorder | Clinical | Adolescent | 60 | Any anxiety diagnosis, PD | Attempt |
| Goldston et al. (2009) | 180 inpatients | Clinical | Adolescent | 168 | GAD, PD, SPEC | Attempt |
| Hayashi et al. (2012) | 106 Japanese inpatients with prior self-injury | History of SITBs | Adult | 24 | Any anxiety diagnosis | Attempt |
| Holma et al. (2010) | 249 Finnish patients with MDD | Clinical | Adult | 60 | Any anxiety diagnosis, anxiety symptoms | Attempt |
| Hung et al. (2015) | 102,454 general elderly Chinese community | General | Adult | 60 | Anxiety symptoms | Death |
| Keane et al. (1996) | 134 American Indian high school students | General | Adolescent | 6 | Anxiety symptoms | Attempt |
| Keilp et al. (2008) | 26 patients with MDD and prior attempt | History of SITBs | Adult | 24 | PTSD | Attempt |
| Kovacs et al. (1993) | 183 inpatients | Clinical | Adolescent | 144 | ADJ | Ideation, attempt |
| Laan et al. (2011) | 129,781 general Dutch community | General | Adolescent and adult | 120 | Any anxiety diagnosis | Death |
| Leadholm et al. (2013) | 34,671 patients with depression | Clinical | Adult | 204 | Any anxiety diagnosis | Death |
| Lewinsohn et al. (2001) (a) | 539 Danish females in general community | General | Adolescent | 144 | Any anxiety diagnosis | Attempt |
| Lewinsohn et al. (2001) (b) | 402 Danish males in general community | General | Adolescent | 144 | Any anxiety diagnosis | Attempt |
| Links et al. (2013) | 180 Canadian patients with BPD | Clinical | Adult | 24 | PTSD | Attempt |
| May et al. (2012) | 49 psychiatric patients with suicide ideation | History of SITBs | Adult | 120 | Any anxiety diagnosis | Attempt |
| Monnin et al. (2011) | 273 French psychiatric patients with prior attempt | History of SITBs | Adult | 24 | PTSD | Attempt |
| Nimeus et al. (2000) | 191 Swedish psychiatric patients with prior attempt | History of SITBs | Adult | 12 | ADJ | Death |
| Nordström et al. (1996) | 54 Swedish inpatients with prior attempt | History of SITBs | Adult | 72 | Anxiety symptoms | Death |
| Preuss et al. (2003) | 1,237 general community with alcohol abuse or family member with alcohol abuse | Clinical | Adult | 60 | PD | Attempt |
| Rao et al. (1993) | 281 patients with depression and/or anxiety, or controls | Clinical | Adolescent | 156 | Any anxiety diagnosis | Death |
| Reinherz et al. (1995) (a) | 193 females in general community | General | Adolescent | 168 | PTSD, SOC, SPEC, anxiety symptoms | Ideation |
| Reinherz et al. (1995) (b) | 185 males in general community | General | Adolescent | 168 | PTSD, SOC, SPEC, anxiety symptoms | Ideation |
| Ribeiro et al. (2012) | 239 psychiatric outpatients with suicidality | History of SITBs | Adult | 1 | PTSD, anxiety symptoms | Ideation, attempt |
| Riihimaki et al. (2013) | 134 Finnish patients with mood disorder | Clinical | Adult | 60 | Any anxiety diagnosis, GAD, PD, SOC, SOM, anxiety symptoms | Attempt |
| Sanchez-Gistau et al. (2013) | 82 Spanish patients with first-episode psychosis | Clinical | Adolescent | 24 | Any anxiety diagnosis | Attempt |
| Sani et al. (2011) | 4,441 Italian psychiatric patients | Clinical | Adult | 420 | GAD, OCD, PD | Death |
| Schneider et al. (2001) | 278 German patients with MDD | Clinical | Adult | 60 | Any anxiety diagnosis, PD, anxiety symptoms | Death |
| Sokero et al. (2005) | 198 Finnish patients with MDD | Clinical | Adult | 18 | Any anxiety diagnosis AG, GAD, OCD, PD, PTSD, SOC, SPEC, anxiety symptoms | Attempt |
| Tidemalm et al. (2014) (a) | 3,678 Swedish females with bipolar disorder | Clinical | Adult | 84 | Any anxiety disorder | Attempt |
| Tidemalm et al. (2014) (b) | 2,408 Swedish males with bipolar disorder | Clinical | Adult | 84 | Any anxiety disorder | Attempt |
| Tejedor et al. (1999) | 150 Spanish patients with prior attempt | History of SITBs | Adult | 120 | Any anxiety diagnosis, ADJ, anxiety symptoms | Attempt, death |
| Tuiksu et al. (2014) | 137 Finnish patients with mood disorder | Clinical | Adolescent | 84 | Anxiety symptoms | Attempt |
| Valtonen et al. (2006) | 160 Finnish patients with bipolar disorder | Clinical | Adult | 18 | Any anxiety diagnosis, anxiety symptoms | Attempt |
| Valtonen et al. (2008) | 176 Finnish patients with bipolar disorder | Clinical | Adult | 18 | Any anxiety diagnosis | Attempt |
| Wedig et al. (2012) | 231 patients with BPD | Clinical | Adult | 192 | PTSD | Attempt |
| Wenzel et al. (2011) | 297 inpatients with suicidality | History of SITBs | Adult | 360 | Any anxiety diagnosis | Death |
| Wolk, Weissman (1996) | 226 patients with depression and/or anxiety, or controls | General | Adolescent | 204 | Any anxiety diagnosis | Attempt, death |
| Yaseen et al. (2012) | 2,864 patients with past year major depressive episode | Clinical | Adult | 36 | GAD, SOC, SPEC, panic attack | Ideation, attempt |
| Yen et al. (2003) | 578 patients with personality disorder | Clinical | Adult | 24 | PD, PTSD | Attempt |
Note. ADJ=adjustment disorder;AG=agoraphobia; ANX-NOS=anxiety disorder not otherwise specified; GAD=generalized anxiety disorder; OCD=obsessive–compulsive disorder; PD=panic disorder; PDA=panic disorder with agoraphobia; PTSD=posttraumatic stress disorder; SOC=social anxiety disorder; SPEC=specific phobia; SOM=somatic symptom disorder.
General=general community; Clinical=outpatient or inpatient sample; History of SITBs=history of suicidal or nonsuicidal self-injurious thoughts and/or behaviors.
Refers to age of sample at baseline.
Although no explicit definition was provided by study authors, anxiety neuroses were distinguished from other related disorder categories (e.g., affective disorders, substance use disorders).
Defined by study authors as acute crisis reaction.
Across all included studies, the median follow-up interval was 60 months (M = 113.1, SD = 126.2, range = 1–708 months). The most common follow-up period length was also 60 months (9 studies). Only 4 included studies had a follow-up interval shorter than 12 months, whereas just under one-third (30.4%) of studies had a follow-up period of 12 years or longer. With regard to predictors, the vast majority of studies (85.5%) reported at least one case in which an anxiety diagnosis (either a specific diagnosis [e.g., GAD, PTSD] or diagnosis grouping [e.g., any anxiety disorder]) was used to predict a suicide-related outcome. Of these, 11 studies also reported one or more additional case(s) using anxiety symptoms to predict a suicide-related outcome. Only 10 studies only included symptom-level anxiety predictors. For suicide-related outcomes, most studies (60.9%) reported at least one usable suicide attempt prediction case. Death was the second most common outcome examined, with 37.7% of studies presenting one or more cases in which an anxiety predictor was used to predict suicide death. Only 13.0% of studies included a prediction case for ideation. There was an average of 2.61 usable prediction cases per study.
3.2. Overall anxiety effect sizes and publication bias
3.2.1. Suicide ideation
Overall effect sizes for any anxiety construct predicting outcomes of suicide ideation, suicide attempt, and suicide death are presented in Table 2; these (and other overall OR) findings are also presented in Fig. 2. In total, 26 prediction cases included suicide ideation as an outcome. The overall OR for any anxiety construct predicting suicide ideation was statistically significant, but small. Heterogeneity among these cases was high, suggesting significant between-study variance. We employed multiple analyses to test for publication bias among suicide ideation prediction cases. Orwin's fail-safe N value suggested that 884 cases with a mean OR of 1.00 would be necessary to lower the overall mean OR for any anxiety construct below our predefined threshold of 1.01. In addition, Egger's test demonstrated an intercept (B0) of 0.91 (95% CI: −2.02, 3.83), t(24) = 0.64, p = 0.27, which provides no clear indication of publication bias. However, the funnel plot appeared asymmetrical, with a disproportionate number of studies falling on the right side of the mean effect (see Fig. 3). Duval and Tweedie's trim and fill analysis also detected 9 missing cases, and indicated that if these were included, the overall weighted OR would be slightly smaller (OR =1.24, 95% CI: 1.01, 1.53).
Table 2.
Overall effect sizes for any anxiety construct (diagnosis and symptoms) predicting suicide-related outcomes.
| # of included OR cases | Overall OR (95% CI) | p value | z | I2 (%) | # of included HR cases | Overall HR (95% CI) | p value | z | I2 (%) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | 26 | 1.49 (1.18, 1.88) | <.01 | 3.39 | 85.57 | – | – | – | – | |
| Attempt | 80 | 1.64(1.47, 1.83) | <.001 | 8.90 | 76.97 | 10 | 1.04 (0.96, 1.11) | .36 | 0.93 | 71.20 |
| Death | 39 | 1.01 (0.87, 1.18) | .88 | 0.16 | 46.95 | 10 | 1.52 (1.28, 1.81) | b.001 | 4.79 | 92.94 |
Note. There were no HR prediction cases for suicide ideation.
Fig. 2.
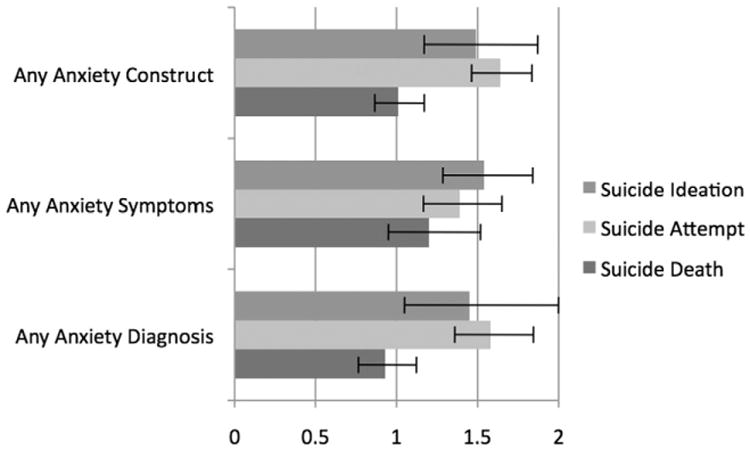
Overall odds ratios (ORs) and corresponding 95% confidence intervals for any anxiety construct, any anxiety symptoms, and any anxiety diagnosis predicting suicide ideation, suicide attempt, and suicide death. An OR must exceed 1.0 to be statistically significant.
Fig. 3.
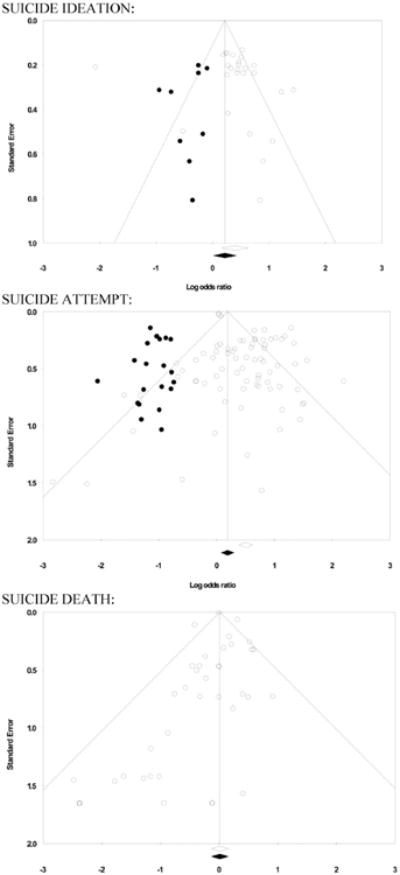
Funnel plots for anxiety constructs predicting suicide-related outcomes (ORs). Open circles indicate values captured in the meta-analysis. Shaded circles indicate imputed values missing to the left of the mean due to publication bias. Open diamonds indicate weighted mean ORs before adjusting for publication bias. Shaded diamonds indicates weighted mean ORs after adjusting for publication bias.
As previously noted, there were no HR cases for suicide ideation. We also did not examine diagnostic accuracy for suicide ideation due to an insufficient number of cases with the information required for these analyses.
3.2.2. Suicide attempt
A total of 80 prediction cases that used (or could be converted into) an OR included suicide attempt as an outcome. The overall effect size estimate for any anxiety construct also reached the level of statistical significance, but was small (Table 2, Fig. 2). Similar to suicide ideation, heterogeneity among suicide attempt prediction cases was high. With regard to publication bias, Orwin's fail-safe N indicated that 838 cases with an OR of 1.00 would be needed to bring the combined weighted OR for suicide ideation below our threshold of 1.01. Egger's regression test produced an intercept (B0) of 1.13 (95% CI: 0.66, 1.59), t(78) = 4.83, p < .0001, indicating that the less precise studies reported larger effect sizes, thereby suggesting significant publication bias. The funnel plot also appeared asymmetrical, with more studies falling to the right of the mean (see Fig. 3). Duval and Tweedie's trim and fill test indicated that 21 prediction cases were missing from our meta-analysis, and should these studies have been included, the combined mean OR for any anxiety construct predicting suicide attempt would be reduced to 1.20 (95% CI: 1.07, 1.34).
There also were 10 HR cases included in the meta-analysis that used suicide attempt as an outcome. For any anxiety construct predicting suicide attempt, the overall weighted mean HR did not reach statistical significance; these cases also evidenced high heterogeneity (Table 2).
As previously noted, there were 39 suicide attempt prediction cases with sufficient information to conduct diagnostic accuracy analyses. Overall, the accuracy of anxiety in prediction suicide attempt was poor, indicating that although anxiety may confer risk for attempt, it is only slightly better than chance. Specifically, the AUC was .56 (SE = .02), indicating extremely poor prediction (see Fig. 4). Further, sensitivity (i.e., true positive rate) was very low at .12 (95% CI: .11, .13, p < .001). Although specificity (i.e., true negative rate) was acceptable at .88 (95% CI: .87, .88, p < .001), this is likely due to a rare outcome (suicide attempt) crossed with a relatively rare predictor (e.g., anxiety disorder).
Fig. 4.
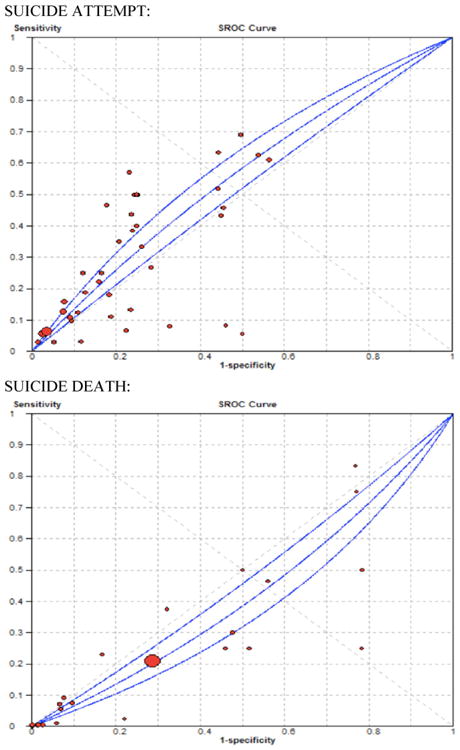
ROC curves for anxiety predicting suicide attempt and death.
3.2.3. Suicide death
There were 39 prediction cases with suicide death as an outcome included in OR analyses. The overall weighted mean OR for any anxiety construct did not reach statistical significance (Table 2, Fig. 2). Heterogeneity among these cases was lower than suicide ideation and attempt cases; indeed, the heterogeneity statistic suggests that less than half of variance was accounted for by between-study variance. Regarding tests for publication bias, Orwin's fail-safe N suggested that 14 cases with mean ORs of 1.00 would be needed to bring the overall estimated OR for suicide death under our predefined value; of note, the overall effect size was already at our predefined value for a trivial magnitude. Egger's test resulted in an intercept (B0) of —0.21 (95% CI: -0.67, 0.24), t(37) = 0.95, p = 0.18, which is not indicative of substantial publication bias. The funnel plot for suicide death cases appeared asymmetrical (see Fig. 3), with more studies on the left side of the mean, but a Duval and Tweedie's trim and fill test indicated that no prediction cases were missing.
A total of 10 HR cases included suicide death as an outcome. The overall weighted mean HR for any anxiety construct predicting suicide death was statistically significant, yet small (Table 2). There was extremely high heterogeneity among these cases, suggesting substantial between-study variance.
Diagnostic accuracy analyses were conducted using the 26 suicide death cases that provided the necessary raw data. Similar to suicide attempt, specificity (.75; 95% CI: .75, .75, p < .001) was much higher than sensitivity, which was very poor (.05; 95% CI: .04, .05, p < .001). Again, this specificity value was likely an artifact of a rare outcome (suicide death) crossed with a relatively rare predictor (e.g., anxiety disorder). Further, the AUC did not reach statistical significance (.42, SE = .02; see Fig. 4), suggesting extremely poor overall prediction.
3.3. Anxiety symptoms effect sizes
3.3.1. Suicide ideation
Results from analyses corresponding to any anxiety symptoms (i.e., excluding anxiety and related diagnoses) predicting suicide ideation, attempt, and death are presented in Table 3 and Fig. 2. Analyses showed a small, but statistically significant overall OR. Heterogeneity among these cases was relatively low.
Table 3.
Overall Odds ratios for anxiety symptoms predicting suicide-related outcomes.
| # of included cases | Overall OR (95% CI) | p value | z | I2 (%) | |
|---|---|---|---|---|---|
| Ideation | 7 | 1.54 (1.29, 1.84) | <.001 | 4.72 | 28.38 |
| Attempt | 9 | 1.39 (1.17, 1.65) | <.001 | 3.80 | 83.12 |
| Death | 12 | 1.20 (0.95, 1.52) | .13 | 1.51 | 6.40 |
3.3.2. Suicide attempt
The overall OR for anxiety symptoms predicting suicide attempt was small, but reached statistical significance, with high between-cases variance (Table 3, Fig. 2).
3.3.3. Suicide death
The estimated overall OR for anxiety symptom cases predicting suicide death did not reach the level of statistical significance. There was low heterogeneity among these cases (Table 3, Fig. 2).
3.4. Anxiety diagnosis effect sizes
3.4.1. Suicide ideation
Findings from analyses of anxiety and related diagnoses predicting suicide ideation, suicide attempt, and suicide death are presented in Table 4 and Fig. 2. First, the combined effect of any type of anxiety diagnosis significantly predicted suicide ideation; there was also high heterogeneity among cases included in this analysis. Diagnosis-specific analyses indicated that the strongest predictor of suicide ideation was PTSD; however, one PTSD case with a notably large magnitude (OR = 4.21) may have been partially driving these findings, as no other suicide ideation prediction cases exceeded an OR of 2.33. Diagnoses of GAD, specific phobia, and social anxiety disorder were also significant predictors of suicide ideation. Corresponding I2 statistics also suggest substantial heterogeneity among PTSD and GAD cases, but not specific phobia or social anxiety disorder cases (Table 4).Of note, only 4 suicide ideation prediction cases were used to generate overall ORs for PTSD, specific phobia, and social anxiety disorder, and only 2 cases were used for GAD, thereby limiting the conclusions we can draw from this set of analyses. Overall effect size estimates were not computed for adjustment disorder, agoraphobia, OCD, panic disorder, or somatic symptom disorder because there was no more than one relevant case for each of these diagnoses.
Table 4.
Overall odds ratios for anxiety diagnoses predicting suicide-related outcomes.
| # of cases | Overall OR (95% CI) | p value | z | I2 (%) | |
|---|---|---|---|---|---|
| Any type of anxiety diagnosis | |||||
| Ideation | 19 | 1.45 (1.05, 2.00) | <.05 | 2.26 | 89.00 |
| Attempt | 71 | 1.58 (1.36, 1.84) | <.001 | 5.90 | 69.77 |
| Death | 27 | 0.93 (0.77, 1.13) | .48 | −0.70 | 54.44 |
| Adjustment disorder | |||||
| Attempt | 4 | 0.33 (0.16, 0.69) | <.01 | −2.94 | 0.00 |
| Death | 5 | 0.24 (0.09, 0.67) | <.01 | −2.74 | 0.00 |
| Agoraphobia | |||||
| Attempt | 4 | 0.99 (0.55, 1.78) | .98 | −0.03 | 0.00 |
| GAD | |||||
| Ideation | 2 | 1.70 (1.18, 2.46) | <.01 | 2.84 | 53.84 |
| Attempt | 7 | 1.27 (0.78, 2.08) | .34 | 0.96 | 77.94 |
| OCD | |||||
| Attempt | 2 | 0.95 (0.28, 3.18) | .93 | −0.08 | 0.00 |
| Death | 2 | 0.23 (0.03, 1.69) | .15 | −1.44 | 0.00 |
| Panic disorder | |||||
| Attempt | 9 | 1.96 (1.38, 2.79) | <.001 | 3.76 | 41.55 |
| Death | 4 | 1.09 (0.39, 3.04) | .87 | 0.16 | 0.00 |
| PTSD | |||||
| Ideation | 4 | 2.25 (1.46, 3.47) | <.001 | 3.67 | 50.62 |
| Attempt | 10 | 2.07 (1.49, 2.88) | <.001 | 4.31 | 56.87 |
| Social anxiety disorder | |||||
| Ideation | 4 | 1.38 (1.10, 1.72) | <.01 | 2.83 | 0.00 |
| Attempt | 7 | 1.67 (1.25, 2.23) | <.01 | 3.45 | 0.00 |
| Somatic symptoms disorder | |||||
| Attempt | 2 | 1.85 (0.88, 3.90) | .11 | 1.62 | 0.00 |
| Specific phobia | |||||
| Ideation | 4 | 1.45 (1.16, 1.81) | <.01 | 3.26 | 0.39 |
| Attempt | 5 | 1.43 (0.91, 2.24) | .12 | 1.55 | 50.49 |
Note. GAD=generalized anxiety disorder; OCD=obsessive–compulsive disorder; PTSD=posttraumatic stress disorder.
3.4.2. Suicide attempt
The combined effect of any type of anxiety diagnosis on suicide attempt was also statistically significant, yet relatively small in magnitude (Table 4, Fig. 2). High heterogeneity among these cases was also observed. Diagnosis-specific analyses indicated that PTSD, panic disorder, and social anxiety disorder were significant predictors of subsequent suicide attempt; the strongest predictor of suicide attempt was PTSD followed by panic disorder. Of note, two prediction cases with ORs above 4.0 may have been driving the relatively high estimate for panic disorder, as no other cases included in any diagnosis-specific analysis for suicide attempt exceeded 3.3. Agoraphobia, GAD, OCD, somatic symptom disorder, and specific phobia did not reach the level of statistical significance. Adjustment disorder was a significant predictor of fewer suicide attempts. It is again important to consider the relatively small number of cases included in diagnosis-specific analyses for adjustment disorder, agoraphobia, OCD, somatic symptom disorder, and specific phobia (ranging from 2 to 5). Among the diagnosis-specific cases that produced statistically significant effect sizes, substantial heterogeneity was observed for PTSD, whereas relevant cases for panic disorder, social anxiety disorder, and adjustment disorder evidenced relatively low heterogeneity.
3.4.3. Suicide death
For any type of anxiety diagnosis predicting suicide death, the overall OR did not reach the level of statistical significance, and heterogeneity among these cases was present (Table 4, Fig. 2). Diagnosis-specific overall ORs for panic disorder and OCD were weak and nonsignificant, whereas adjustment disorder was shown to be a statistically significant predictor of fewer suicide deaths. I2 statistics also suggested substantial heterogeneity was present among cases included in the overall “any anxiety diagnosis” analysis, but relatively low heterogeneity across cases included in diagnosis-specific analyses. We did not generate weighted suicide death ORs for agoraphobia, GAD, PTSD, social anxiety disorder, somatic symptom disorder, or specific phobia due to the fact that there was no more than one relevant case for each diagnosis.
3.5. Moderation analyses
We examined three potential moderators of the relationship between anxiety and suicide ideation, attempt, and death: sample type (i.e., general, clinical, history of prior SITBs), sample age (i.e., adult, adolescent, mixed), and length of follow-up period.
3.5.1. Sample type
Sample type did not moderate the relationship between any anxiety construct and suicide ideation or suicide death. However, suicide attempt prediction cases drawn from studies using general samples generated a significantly stronger overall effect size (OR = 2.98, 95% CI: 2.37, 3.75, z = 9.35, p < .001) than clinical populations (OR = 1.55, 95% CI: 1.38, 1.75, z = 7.37, p < .001) and individuals with a history of SITBs (OR = 1.16, 95% CI: 0.85, 1.59, z = 0.94, p = .35).
3.5.2. Sample age
The age of the study sample also did not affect the predictive ability of anxiety for suicide ideation or death. Similar to sample type, however, there was a moderation effect of sample age on the relationship between any anxiety construct and suicide attempt. Specifically, weighted mean effect sizes from studies using samples comprised of all adults (OR = 1.79, 95% CI: 1.56, 2.06, z = 8.24, p < .001) were significantly stronger than those using mixed samples (OR = 0.83, 95% CI: 0.62, 1.11, z = −1.23, p = .22). Of note, there were no significant differences between adult-only or mixed samples in comparison to adolescent-only samples (OR = .59, 95% CI: 0.99, 2.56, z = 1.92, p = .06).
3.5.3. Length of follow-up period
Results from maximum likelihood meta-regression analyses indicated that length of follow-up period significantly moderated the relationship between anxiety and both suicide ideation and attempt (see Fig. 5), but not suicide death. For suicide ideation, there was a small (but steady) decline in magnitude of combined ORs steadily as the length of follow-up period increased (b = −0.005, SE = 0.00, 95% CI: −0.01, −0.00, z = −2.91, p < .01), with follow-up length explaining 32% of the between-study variance. The same trend was observed for suicide attempt (b = −0.004, SE = 0.00, 95% CI: −0.01, −0.00, z = −2.81, p < .01), with follow-up length explaining 5% of between-study variance. Together, these findings indicate that with longer follow-up periods, the predictive ability of anxiety disorders and symptoms for suicide ideation and attempt weakens slightly.
Fig. 5.
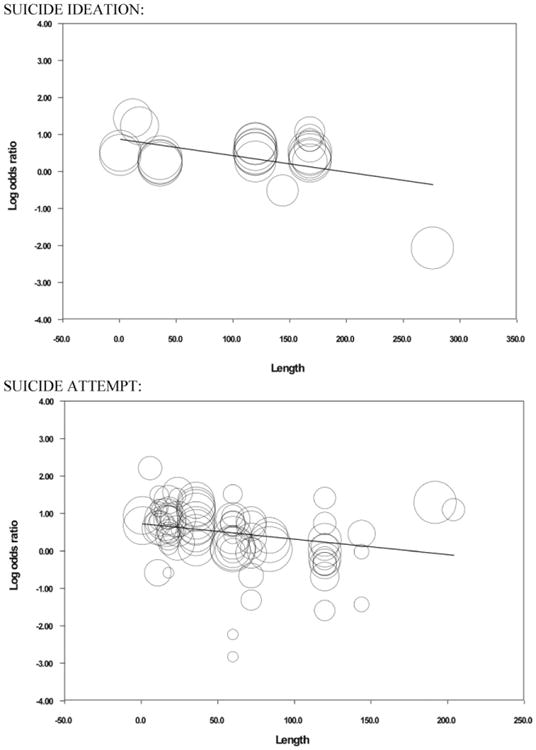
Moderation effect for length of follow-up period on suicide ideation and attempt.
4. Discussion
Suicidal thoughts and behaviors are public health problems that affect millions across the globe. Despite receiving increased empirical attention over the past 50 years, the rates of suicidal thoughts and behaviors have not abated. Identifying powerful and accurate risk factors is one promising means toward effective prevention and treatment, and thus eventual reduction, of these phenomena. Anxiety is one potential risk factor for suicidality that has been of particular interest to date. For one, anxiety is listed as a top risk factor for suicide by leading national organizations (e.g., AAS, AFSP, National Suicide Prevention Lifeline). Prominent theories of suicide (e.g., Baumeister, 1990; Joiner, 2005; Wenzel & Beck, 2008) also either directly address anxiety and/or are consistent with findings implicating the role of acute anxiety/agitation in suicidal behavior. In addition, converging evidence from large-scale longitudinal studies suggests that anxiety disorders significantly predict suicidal ideation and behaviors, even when controlling for comorbidity (e.g., Boden et al., 2007; Nock et al., 2009, 2010; Sareen et al., 2005). As such, the aim of this meta-analysis was to synthesize the existing knowledge of anxiety as a risk factor for suicidal thoughts and behaviors. Analyses indicated that anxiety and its disorders are statistically significant predictors of suicide ideation and attempts, but not deaths.1 The strength of observed relationships was weak across all categories examined.
Although overall, anxiety and its disorders showed statistically significant prospective associations with suicide ideation and attempts, these findings do not translate into high clinical utility. Across all anxiety-related predictors and suicide-related outcomes, combined effect sizes were small, and no one predictor stood out as being significantly stronger than the rest. Specifically, the largest combined OR just exceeded 2.0, and most effect sizes that reached statistical significance clustered around 1.5. Given that the absolute risk of experiencing suicidal thoughts and behaviors (and especially attempts and deaths) is low, these estimates do not translate into clinically practical information. Consider an example using PTSD, the diagnosis that produced the largest overall effect on suicide attempts in our meta-analysis. Recent data suggest that in the United States, 0.4% of adults make a suicide attempt in a given year (Borges et al., 2006). Even when these odds are multiplied by 2.25 for individuals with PTSD, as our meta-analysis would suggest, the resultant odds are still close to zero. Determining that an individual has a 0.9% probability of attempting suicide in the next year based on a PTSD diagnosis (as opposed to a 0.4% probability for individuals without PTSD) does not provide meaningful information for clinicians facing critical decisions about suicide risk. This pattern of low clinical significance also holds for adjustment disorder, the only diagnosis evidencing a statistically significant protective effect against suicidal behavior (0.1% versus 0.4% probability of attempting suicide for individuals with and without this diagnosis, respectively). The limited clinical utility of our findings is even more striking when one considers the fact that clinicians are usually tasked with determining who is at risk for suicidal behavior over the next few hours or days, rather than months or years. In short, anxiety and its disorders, at least as these constructs have been studied to date, are unlikely to serve as powerful “real-world” indicators of risk for suicidal thoughts and behaviors.
There are several potential explanations for our findings that anxiety (diagnoses or symptoms) does not significantly predict suicide deaths. The interpersonal theory of suicide (Joiner, 2005; Van Orden et al., 2010) posits that for lethal suicidal behavior to occur, individuals must develop high levels of acquired capability through repeated experiences with painful and provocative events (e.g., Ribeiro et al., 2014). Indeed, some anxiety disorders examined here (e.g., agoraphobia, GAD) may be associated with significant fear and avoidance of the experiences required to develop this suicidal capability and more frightening, lethal suicidal behavior (e.g., Silva, Ribeiro, & Joiner, 2015). Thus, consistent with Joiner's model, hallmark features of anxiety disorders may protect against the transition from ideation (and even non-lethal suicide attempts) to death by suicide. Another related explanation is that the constructs of anxiety captured in this review are not as relevant to suicide deaths as specific, more acute anxiety-related symptoms. Given findings indicating that severe, heightened arousal is often present immediately prior to suicide (e.g., Busch et al., 2003; Robins, 1981; Way, Miraglia, Sawyer, Beer, & Eddy, 2005), and facilitates lethal suicidal behavior among at-risk individuals (e.g., Ribeiro et al., 2015), there is likely an important distinction between the role of anxiety disorders and general affective states of anxiety (e.g., trait-like anxiety, future-oriented worry) versus acute symptoms of anxiety and agitation (e.g., excessive motor and mental arousal) in predicting suicide deaths specifically.
We also observed several significant moderation effects in this meta-analysis. First, general samples generated larger effect sizes for prediction of suicide attempts than those drawn from clinical settings or with a history of SITBs. This is likely due to the fact that in samples of psychiatric patients and/or with a SITB history, confounding factors (e.g., psychopathology severity, prior suicidal behavior) were more likely to be controlled for (as a function of the sample selection) in comparisons between individuals with and without anxiety. In contrast, studies of community samples did not account for these related variables, and thus were likely to produce stronger effects. We also found that adult samples produced larger effects than samples combining adolescents and adults; however, the conclusions that can be drawn here are limited given the very small number of cases included in the mixed and adolescent-only analyses, and overlapping CIs for effect sizes produced in adolescent- and adult-only samples. Finally, studies with shorter follow-up periods demonstrated larger effects than longer follow-up intervals. This suggests that anxiety and its disorders may be stronger predictors of suicidal thoughts and behaviors over shorter amounts of time.
4.1. Limitations and future directions
Overall, the current evidence suggests that anxiety and its disorders do not substantially increase risk for future suicidal thoughts and behaviors; however, this conclusion only applies to the relationship between anxiety and suicide as it has traditionally been examined. The present meta-analysis identified several methodological limitations of existing research on anxiety as a risk factor for suicidality. First, the vast majority of studies have measured anxiety in terms of specific diagnoses or broad, trait-like symptoms, rather than dynamic, acute constructs. Second, the existing literature has generally analyzed anxiety in isolation, rather than in conjunction with other known risk factors. Finally, studies have tended to employ long follow-up periods, rather than the short follow-up periods more relevant to “real-world” assessment of suicide risk. Despite the fact that almost all previous studies have used these methods, few would expect any variable (anxiety-related or otherwise), when measured as a trait-like, static construct and studied in isolation, to accurately predict suicidal thoughts and behaviors over many years.
Thus, the possibility remains that anxiety is a very important risk factor for suicide, but it has not yet been studied under the conditions necessary to detect this relationship. Future studies must focus on directly testing prominent theories and models of suicide that conceptualize suicidal thoughts and behaviors as resulting from complex combinations of risk factors (distal and proximal, trait-like and unstable) interacting to heighten risk over short periods of time. For instance, rapid elevations in specific, acute anxiety-related constructs (e.g., heightened arousal/agitation, sudden onset of severe panic-like symptoms) may substantially increase risk for suicidal behavior when such variables are combined with other potentially important factors (e.g., acquired capability, lack of social support, prior engagement in SITBs, triggering events, psychiatric comorbidities). Even in these specific contexts, these constructs may only substantially enhance risk for short periods of time.
In order to better approximate these hypotheses, a number of methodological changes are needed in future research. For one, studies must employ more dynamic (including physiological, implicit, and/or behavioral) measures of specific anxiety-related constructs hypothesized to be most pertinent to prediction of suicidal behavior as well as examine potential interactive effects with other known and more novel risk factors (e.g., implicit associations with suicide; Nock et al., 2010). It is also recommended that in future studies aiming to isolate the unique effects of a single risk factor (or specific combination of risk factors), researchers consistently adjust for factors that may influence the magnitude of their findings (e.g., gender, depression severity). Future investigations must also assess both putative risk factors and suicide-related outcomes much more frequently (rather than letting many months or years elapse between time points), and over much shorter periods of time (e.g., minutes, hours, days). It is also encouraged that researchers examine more fine-grained features of suicidal behavior (e.g., attempt frequency, lethality, intent) in order to refine our understanding of the longitudinal relationships between hypothesized risk factors and specific outcomes, including characteristics of those outcomes. Finally, very large numbers of participants must be included in these studies in order to detect a sufficient number of suicidal acts over follow-up intervals.
Previously, this type of research has not been feasible for the majority of researchers. Recent advancements in technology, however, have rendered it possible for many to conduct these studies much more easily and for relatively low cost. For example, ecological momentary assessment and other mobile technologies delivered through smart-phone or web-based methods serve as easily accessible, economically viable tools for researchers and participants alike. Future investigations that capitalize on current technological innovations have great potential for improving our understanding of effective prediction, prevention, and treatment of suicidal thoughts and behaviors, and thus reduce the impact of suicide worldwide.
5. Conclusions
This meta-analysis indicates that anxiety disorders and symptoms are statistically significant yet weak risk factors for future suicide ideation and attempts but not deaths. Given the methodological limitations of existing research in this area, however, results do not necessarily imply that anxiety plays a trivial or nonexistent role in suicide prediction. Rather, anxiety does not appear to confer meaningful risk for suicidal thoughts and behaviors under the specific conditions of how it has been examined to date. Future research must take advantage of recent technological advancements to generate potentially informative and practical knowledge about the role of anxiety-related constructs in conferring risk for suicidal thoughts and behaviors.
Highlights.
We conducted a meta-analysis of anxiety predicting suicidal thoughts and behaviors.
Anxiety was a significant risk factor for suicide ideation and attempts.
As it has traditional been studied, anxiety is a weak predictor of suicidality.
Future research must approximate current theories about risk factors for suicide.
Appendix A. References for articles included in meta-analyses
- Allgulander C, Allebeck P, Przybeck T, Rice JP. Risk of suicide by psychiatric diagnosis in Stockholm County. Euorpean Archives of Psychiatry and Clinical Neuroscience. 1992;241:323–326. doi: 10.1007/BF02195984. [DOI] [PubMed] [Google Scholar]
- Alonso P, Segalàs C, Real E, Pertusa A, Labad J, Jiménez-Murcia S, et al. Menchón JM. Suicide in patients treated for obsessive–compulsive disorder: A prospective follow-up study. Journal of Affective Disorders. 2010;124:300–308. doi: 10.1016/j.jad.2009.12.001. http://dx.doi.org/10.1016/j.jad.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Angst J, Clayton PJ. Personality, smoking, and suicide: A prospective study. Journal of Affective Disorders. 1998;51:55–62. doi: 10.1016/s0165-0327(98)00156-6. [DOI] [PubMed] [Google Scholar]
- Bakken K, Vaglum P. Predictors of suicide attempters in substance-dependent patients: A six-year prospective follow-up. Clinical Practice and Epidemiology in Mental Health. 2007;3(20) doi: 10.1186/1745-0179-3-20. http://dx.doi.org/10.1186/1745-0179-3-20 http://dx.doi.org/10.1186/1745-0179-3-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beautrais AL. Further suicidal behavior among medically serious suicide attempters. Suicide and Life-Threatening Behavior. 2004;34(1):1–11. doi: 10.1521/suli.34.1.1.27772. [DOI] [PubMed] [Google Scholar]
- Berglund M. Suicide in alcoholism: A prospective study of 88 suicides: The multidimensional diagnosis at first admission. Archives of General Psychiatry. 1984;41:888–891. doi: 10.1001/archpsyc.1984.01790200070009. [DOI] [PubMed] [Google Scholar]
- Berglund M, Nilsson K. Mortality in severe depression: A prospective study including 103 suicides. Acta Psychiatrica Scandinavica. 1987;76:372–380. doi: 10.1111/j.1600-0447.1987.tb05621.x. [DOI] [PubMed] [Google Scholar]
- Blumenthal S. Mortality and rate of suicide of first admission psychiatric patients. Psychopathology. 1989;22(1):50–56. doi: 10.1159/000284579. http://dx.doi.org/10.1111/add.12381. [DOI] [PubMed] [Google Scholar]
- Bolton JM, Pagura J, Enns MW, Grant B, Sareen J. A population-based longitudinal study of risk factors for suicide attempts in major depressive disorder. Journal of Psychiatric Research. 2010;44(13):817–826. doi: 10.1016/j.jpsychires.2010.01.003. http://dx.doi.org/10.1016/j.jpsychires.2010.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borg SE, Ståhl M. Prediction of suicide: A prospective study of suicides and controls among psychiatric patients. Acta Psychiatrica Scandinavica. 1982;65:221–232. doi: 10.1111/j.1600-0447.1982.tb00842.x. [DOI] [PubMed] [Google Scholar]
- Borges G, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: A 10-year follow-up study using the National Comorbidity Surveys. Journal of Affective Disorders. 2008;105:25–33. doi: 10.1016/j.jad.2007.01.036. http://dx.doi.org/10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brådvik L, Mattisson C, Bogren M, Nettelbladt P. Mental disorders in suicide and undetermined death in the Lundby Study. The contribution of severe depression and alcohol dependence. Archives of Suicide Research. 2010;14(3):266–275. doi: 10.1080/13811118.2010.494146. http://dx.doi.org/10.1080/13811118.2010.494146. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz L, Lipton R, Peterson E, Welch KMA. Migraine headaches and suicide attempt. Headache: The Journal of Head and Face Pain. 2012;52(5):723–731. doi: 10.1111/j.1526-4610.2012.02117.x. http://10.10.1111/j.1526-4610.2012.02117.x. [DOI] [PubMed] [Google Scholar]
- Britton PC, Ilgen MA, Valenstein M, Knox K, Claassen CA, Conner KR. Differences between veteran suicides with and without psychiatric symptoms. American Journal of Public Health. 2012;102(S1):S125–S130. doi: 10.2105/AJPH.2011.300415. http://dx.doi.org/10.2105/AJPH.2011.300415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown GK, Beck AT, Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: A 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68(3):371–377. http://dx.doi.org/10.1037/0022-006X.68.3.371 http://dx.doi.org/10.1037/0022-006X.68.3.371. [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E, Young-McCaughon, Peterson A. Nonsuicidal self-injury as a prospective predictor of suicide attempts in a clinical sample of military personnel. Comprehensive Psychiatry. 2015;59:1–7. doi: 10.1016/j.comppsych.2014.07.009. http://dx.doi.org/10.1016/j.comppsych.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Cedereke M, Öjehagen A. Prediction of repeated parasuicide after 1–12 months. European Psychiatry. 2005;20(2):101–109. doi: 10.1016/j.eurpsy.2004.09.008. http://dx.doi.org/10.1016/j.eurpsy.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Chan LF, Shamsul AS, Maniam T. Are predictors of future suicide attempts and the transition from suicidal ideation to suicide attempts shared or distinct: A 12-month prospective study among patients with depressive disorders. Psychiatry research. 2014;220(3):867–873. doi: 10.1016/j.psychres.2014.08.055. [DOI] [PubMed] [Google Scholar]
- Clarke DE, Eaton WW, Petronis KR, Ko JY, Chatterjee A, Anthony JC. Increased risk of suicide ideation in smokers and former smokers compared to never smokers: Evidence from the Baltimore ECA follow-up study. Suicide and Life-Threatening Behavior. 2010;40(4):307–318. doi: 10.1521/suli.2010.40.4.307. http://dx.doi.org/10.1521/suli.2010.40.4.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner KR, McCarthy MD, Bajorska A, Caine ED, Tu XM, Knox KL. Mood, anxiety, and substance-use disorders and suicide risk in a military population cohort. Suicide and Life-Threatening Behavior. 2012;42(6):699–708. doi: 10.1111/j.1943-278X.2012.00125.x. http://dx.doi.org/10.1111/j.1943-278X.2012.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. PTSD, depression, and their comorbidity in relation to suicidality: Cross-sectional and prospective analyses of a national probability sample of women. Depression and Anxiety. 2009;26(12):1151–1157. doi: 10.1002/da.20621. http://dx.doi.org/10.1002/da.20621. [DOI] [PubMed] [Google Scholar]
- Courtet P, Picot MC, Bellivier F, Torres S, Jollant F, Michelon C, et al. Malafosse A. Serotonin transporter gene may be involved in short-term risk of subsequent suicide attempts. Biological Psychiatry. 2004;55:46–51. doi: 10.1016/j.biopsych.2003.07.004. http://dx.doi.org/10.1016/j.biopsych.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Cullberg J, Wasserman D, Stefansson CG. Who commits suicide after a suicide attempt?: An 8 to 10 year follow up in suburban catchment area. Acta Psychiatrica Scandinavica. 1988;77(5):598–603. doi: 10.1111/j.1600-0447.1988.tb05173.x. [DOI] [PubMed] [Google Scholar]
- Darke S, Williamson A, Ross J, Teesson M. Attempted suicide among heroin users: 12-month outcomes from the Australian Treatment Outcome Study (ATOS) Drug and Alcohol Cependence. 2005;78(2):177–186. doi: 10.1016/j.drugalcdep.2004.10.009. http://dx.doi.org/10.1016/j.drugalcdep.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Dennehy EB, Marangell LB, Allen MH, Chessick C, Wisniewski SR, Thase ME. Suicide and suicide attempts in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Journal of Affective Disorders. 2011;133(3):423–427. doi: 10.1016/j.jad.2011.04.036. http://dx.doi.org/10.1016/j.jad.2011.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desai RA, Dausey DJ, Rosenheck RA. Mental health service delivery and suicide risk: The role of individual patient and facility factors. The American Journal of Psychiatry. 2005;162(2):311–318. doi: 10.1176/appi.ajp.162.2.311. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DC, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. The American Journal of Psychiatry. 1990;147(9):1189–1194. doi: 10.1176/ajp.147.9.1189. http://dx.doi.org/10.1159/000327754. [DOI] [PubMed] [Google Scholar]
- Flensborg-Madsen T, Knop J, Mortensen EL, Becker U, Sher L, Grønbæk M. Alcohol use disorders increase the risk of completed suicide—Irrespective of other psychiatric disorders. A longitudinal cohort study. Psychiatry Research. 2009;167:123–130. doi: 10.1016/j.psychres.2008.01.008. http://dx.doi.org/10.1016/j.j.psychres.2008.01.008. [DOI] [PubMed] [Google Scholar]
- Fridell EJ, Öjehagen A, Träskman-Bendz I. A 5-year follow-up study of suicide attempts. Acta Psychiatrica Scandinavica. 1996;93(3):151–157. doi: 10.1111/j.1600-0447.1996.tb10622.x. [DOI] [PubMed] [Google Scholar]
- Gallagher M, Prinstein MJ, Simon V, Spirito A. Social anxiety symptoms and suicidal ideation in a clinical sample of early adolescents: Examining loneliness and social support as longitudinal mediators. Journal of Abnormal Child Psychology. 2014;42:871–883. doi: 10.1007/s10802-013-9844-7. http://dx.doi.org/10.1007/s10802-013-9844-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein TR, Ha W, Axelson DA, Goldstein BI, Liao F, Gill MK, Birmaher B. Predictors of prospectively examined suicide attempts among youth with bipolar disorder. Archives of General Psychiatry. 2012;69(11):1113–1122. doi: 10.1001/archgenpsychiatry.2012.650. http://dx.doi.org/10.1001/archgenpsychiatry.2012.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB, Daniel SS, Erkanli A, Reboussin BA, Mayfield A, Frazier PH, Treadway SL. Psychiatric diagnoses as contemporaneous risk factors for suicide attempts among adolescents and young adults: Developmental changes. Journal of Consulting and Clinical Psychology. 2009;77(2):281–290. doi: 10.1037/a0014732. http://dx.doi.org/10.1037/a0014732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayashi N, Igarashi M, Imai A, Yoshizawa Y, Utsumi K, Ishikawa Y, et al. Okazaki Y. Post-hospitalization course and predictive signs of suicidal behavior of suicidal patients admitted to a psychiatric hospital: A 2-year prospective follow-up study. BMC Psychiatry. 2012;12 doi: 10.1186/1471-244X-12-186. http://dx.doi.org/10.1186/1471-244X-12-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holma KM, Melartin TK, Haukka J, Holma IAK, Sokero TP, Isometsä ET. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: A five-year prospective study. The American Journal of Psychiatry. 2010;167(7):801–808. doi: 10.1176/appi.ajp.2010.09050627. [DOI] [PubMed] [Google Scholar]
- Hung GC, Kwok C, Yip PS, Gunnell D, Chen Y. Predicting suicide in older adults – a community-based cohort study in Tapei City, Taiwan. Journal of Affective Disorders. 2014;172:165–170. doi: 10.1016/j.jad.2014.09.037. http://dx.doi.org/10.1016/j.jad.2014.09.037. [DOI] [PubMed] [Google Scholar]
- Keane EM, Dick RW, Bechtold DW, Manson SM. Predictive and concurrent validity of the Suicide ideation Questionnaire among American Indian adolescents. Journal of Abnormal Child Psychology. 1996;24(6):735–747. doi: 10.1007/BF01664737. http://dx.doi.org/10.1007/BF01664737. [DOI] [PubMed] [Google Scholar]
- Keilp JG, Oquendo MA, Stanley BH, Burke AK, Cooper TB, Malone KM, Mann JJ. Future suicide attempt and responses to serotonergic challenge. Neuropsychopharmacology. 2010;35(5):1063–1072. doi: 10.1038/npp.2008.28. http://dx.doi.org/10.1038/npp.2008.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M, Goldston D, Gatsonis C. Suicidal behaviors and childhood-onset depressive disorders: A longitudinal investigation. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(1):8–20. doi: 10.1097/00004583-199301000-00003. http://dx.doi.org/10.1097/00004583-199301000-00003. [DOI] [PubMed] [Google Scholar]
- Laan W, Termorshuizen F, Smeets HM, Boks MPM, de Wit NJ, Geerlings MI. Acomorbid anxiety disorder does not result in an excess risk of death among patients with a depressive disorder. Journal of Affective Disorders. 2011;135(1-3):284–291. doi: 10.1016/j.jad.2011.08.026. http://dx.doi.org/10.1016/j.jad.2011.08.026. [DOI] [PubMed] [Google Scholar]
- Leadholm AKK, Rothschild AJ, Nielsen J, ech P, Østergaard SD. Risk factors for suicide among 34,671 patients with psychotic and non-psychotic severe depression. Journal of Affective Disorders. 2014;156:119–125. doi: 10.1016/j.jad.2013.12.003. http://dx.doi.org/10.1016/j.jad.2013.12.003. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- Links PS, Kolla NJ, Guimond T, McMain S. Prospective risk factors for suicide attempts in a treated sample of patients with borderline personality disorder. Canadian Journal of Psychiatry. 2013;58(2):99–106. doi: 10.1177/070674371305800207. [DOI] [PubMed] [Google Scholar]
- May AM, Klonsky ED, Klein DN. Predicting future suicide attempts among depressed suicide ideators: a 10-year longitudinal study. Journal of Psychiatric Research. 2012;46(7):946–952. doi: 10.1016/j.jpsychires.2012.04.009. http://dx.doi.org/10.1016/j.jpsychires.2012.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monnin J, Thiemard E, Vandel P, Nicolier M, Tio G, Courtet P, et al. Haffen E. Sociodemographic and psychopathological risk factors in repeated suicide attempts: gender differences in a prospective study. Journal of Affective Disorders. 2012;136(1):35–43. doi: 10.1016/j.jad.2011.09.001. http://dx.doi.org/10.1016/j.jad.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Nimeus A, Alsen M, Träskman-Bendz L. The suicide assessment scale: an instrument assessing suicide risk of suicide attempters. European Psychiatry. 2000;15(7):416–423. doi: 10.1016/s0924-9338(00)00512-5. [DOI] [PubMed] [Google Scholar]
- Nordström P, Gustavsson P, Edman G, Åsberg M. Temperamental vulnerability and suicide risk after attempted suicide. Suicide and Life-Threatening Behavior. 1996;26(4):380–394. [PubMed] [Google Scholar]
- Preuss UW, Schuckit MA, Smith TL, Danko GP, Bucholz KK, Hesselbrock MN, et al. Kramer JR. Predictors and correlates of suicide attempts over 5 years in 1,237 alcohol-dependent men and women. American Journal of Psychiatry. 2003;160(1):56–63. doi: 10.1176/appi.ajp.160.1.56. [DOI] [PubMed] [Google Scholar]
- Rao U, Weissman MM, Martin JA, Hammond RW. Childhood depression and risk of suicide: a preliminary report of a longitudinal study. Journal of the American Academy of Child & Adolescent Psychiatry. 1993;32(1):21–27. doi: 10.1097/00004583-199301000-00004. [DOI] [PubMed] [Google Scholar]
- Reinherz HZ, Giaconia RM, Silverman AB, Friedman A, Pakiz B, Frost AK, Cohen E. Early psychosocial risks for adolescent suicide ideation and attempts. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(5):599–611. doi: 10.1097/00004583-199505000-00012. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Pease JL, Gutierrez PM, Silva C, Bernert RA, Rudd MD, Joiner TE. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicide ideation and behavior in young adults in the military. Journal of Affective Disorders. 2012;136(3):743–750. doi: 10.1016/j.jad.2011.09.049. http://dx.doi.org/10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- Riihimäki K, Vuorilehto M, Melartin T, Haukka J, Isometsä E. Incidence and predictors of suicide attempts among primary-care patients with depressive disorders: a 5-year prospective study. Psychological Medicine. 2014;44(02):291–302. doi: 10.1017/S0033291713000706. http://dx.doi.org/10.1017/S0033291713000706. [DOI] [PubMed] [Google Scholar]
- Sanchez-Gistau V, Baeza I, Arango C, Gonzalez-Pinto A, de la Serna E, Parellada M, et al. Castro-Fornieles J. Predictors of suicide attempt in early-onset, first-episode psychoses: a longitudinal 24-month follow-up study. The Journal of Clinical Psychiatry. 2013;74(1):59–66. doi: 10.4088/JCP.12m07632. http://dx.doi.org/10.4088/JCP.12m07632. [DOI] [PubMed] [Google Scholar]
- Sani G, Tondo L, Koukopoulos A, Reginaldi D, Kotzalidis GD, Koukopoulos AE, et al. Tatarelli R. Suicide in a large population of former psychiatric inpatients. Psychiatry and Clinical Neurosciences. 2011;65(3):286–295. doi: 10.1111/j.1440-1819.2011.02205.x. http://dx.doi.org/10.1111/j.1440-1819.2011.02205.x. [DOI] [PubMed] [Google Scholar]
- Schneider B, Philipp M, Müller MJ. Psychopathological predictors of suicide in patients with major depression during a 5-year follow-up. European Psychiatry. 2001;16(5):283–288. doi: 10.1016/s0924-9338(01)00579-x. [DOI] [PubMed] [Google Scholar]
- Sokero TP, Melartin TK, Rytsälä HJ, Leskelä US, Lestelä-Mielonen PS, Isometsä ET. Prospective study of risk factors for attempted suicide among patients with DSM–IV major depressive disorder. The British Journal of Psychiatry. 2005;186(4):314–318. doi: 10.1192/bjp.186.4.314. [DOI] [PubMed] [Google Scholar]
- Tejedor MC, Diaz A, Castillon JJ, Pericay JM. Attempted suicide: repetition and survival findings of a follow-up study. Acta Psychiatrica Scandinavica. 1999;100(3):205–211. doi: 10.1111/j.1600-0447.1999.tb10847.x. http://dx.doi.org/10.1097/chi.0b013e318149e66f. [DOI] [PubMed] [Google Scholar]
- Tidemalm D, Haglund A, Karanti A, Landen M, Runeson B. Attempted suicide in bipolar disorder: Risk factors in a cohort of 6086 patients. PLoS ONE. 2014;9(4):e94097. doi: 10.1371/journal.pone.0094097. http://dx.doi.org/10.1371/journal.pone.0094097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tuisku V, Kiviruusu O, Pelkonen M, Karlsson L, Strandholm T, Marttunen M. Depressed adolescents as young adults–Predictors of suicide attempt and non-suicidal self-injury during an 8-year follow-up. Journal of Affective Disorders. 2013 doi: 10.1016/j.jad.2013.09.031. http://dx.doi.org/10.1016/j.jad.2013.09.031. [DOI] [PubMed]
- Valtonen HM, Suominen K, Mantere O, Leppämäki S, Arvilommi P, Isometsä ET. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disorders. 2006;8:576–585. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Haukka J, Mantere O, Leppämäki S, Arvilommi P, Isometsä ET. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disorders. 2008;10(5):588–596. doi: 10.1111/j.1399-5618.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- Wedig MM, Silverman MH, Frankenburg FR, Reich DB, Fitzmaurice G, Zanarini MC. Predictors of suicide attempts in patients with borderline personality disorder over 16 years of prospective follow-up. Psychological Medicine. 2012;42(11):2395–2404. doi: 10.1017/S0033291712000517. http://dx.doi.org/10.1017/S0033291712000517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel A, Berchick ER, Tenhave T, Halberstadt S, Brown GK, Beck AT. Predictors of suicide relative to other deaths in patients with suicide attempts and suicide ideation: a 30-year prospective study. Journal of Affective Disorders. 2011;132(3):375–382. doi: 10.1016/j.jad.2011.03.006. http://dx.doi.org/10.1016/j.jad.2011.03.006. [DOI] [PubMed] [Google Scholar]
- Wolk SI, Weissman MM, Puig J. Suicidal Behavior in Depressed Children Grown. Psychiatric Annals. 1996;26(6) http://dx.doi.org/10.1097/chi.0b013e318149e66f. [Google Scholar]
- Yaseen ZS, Chartrand H, Mojtabai R, Bolton J, Galynker II. Fear of yding in panic attacks predicts suicide attempt in comorbid depressive illness: Prospective evidence from the national epidemiological survey on alcohol and related conditions. Depression and Anxiety. 2013;30(10):930–939. doi: 10.1002/da.22039. http://dx.doi.org/10.1002/da.22039. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea T, Pagano M, Sanislow CA, Grilo CM, McGlashan TH, et al. Morey LC. Axis I and axis II disorders as predictors of prospective suicide attempts: findings from the collaborative longitudinal personality disorders study. Journal of Abnormal Psychology. 2003;112(3):375. doi: 10.1037/0021-843x.112.3.375. http://dx.doi.org/10.1037/0021-843X.112.3375. [DOI] [PMC free article] [PubMed] [Google Scholar]
Footnotes
This refers to findings from weighted mean OR analyses, which were based on 80 and 39 cases (respectively), given that HR analyses for attempt and death were based on only 10 prediction cases each, and thus less reliable.
References
- American Association of Suicidology. Warning Signs & Risk Factors [online] [Accessed October 16, 2015];2015 http://www.suicidology.org/ncpys/warning-signs-risk-factors.
- American Foundation for Suicide Prevention. Suicide Risk factors [online] [Accessed October 16, 2015];2015 https://www.afsp.org/understanding-suicide/suicide-risk-factors.
- Amir M, Kaplan Z, Efroni R, Kotler M. Suicide risk and coping styles in posttraumatic stress disorder patients. Psychotherapy and Psychosomatics. 1999;68(2):76–81. doi: 10.1159/000012316. [DOI] [PubMed] [Google Scholar]
- Barlow DH, Sauer-Zavala S, Carl JR, Bullis JR, Ellard KK. The nature, diagnosis, and treatment of neuroticism: Back to the future. Clinical Psychological Science. 2014;2(3):344–365. [Google Scholar]
- Baumeister R. Suicide as escape from self. Psychological Review. 1990;97:90–113. doi: 10.1037/0033-295x.97.1.90. http://dx.doi.org/10.1037/0033-295X.97.1.90. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Boden JM, Fergusson DM, Horwood LJ. Anxiety disorders and suicidal behaviours in adolescence and young adulthood: Findings from a longitudinal study. Psychological Medicine. 2007;37:431–440. doi: 10.1017/S0033291706009147. [DOI] [PubMed] [Google Scholar]
- Boergers J, Spirito A, Donaldson D. Reasons for adolescent suicide attempts: Associations with psychological functioning. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(12):1287–1293. doi: 10.1097/00004583-199812000-00012. [DOI] [PubMed] [Google Scholar]
- Bolton JM, Cox BJ, Afifi TO, Enns MW, Bienvenu OJ, Sareen J. Anxiety disorders and risk for suicide attempts: Findings from the Baltimore epidemiologic catchment area follow-up study. Depression and Anxiety. 2008;25:477–481. doi: 10.1002/da.20314. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive meta-analysis version 2. Englewood, New Jersey: Biostat; 2005. [Google Scholar]
- Borges G, Angst J, Nock MK, Ruscio AM, Kessler RC. Risk factors for the incidence and persistence of suicide-related outcomes: A 10-year follow-up study using the National Comorbidity Surveys. Journal of Affective Disorders. 2008a;105:25–33. doi: 10.1016/j.jad.2007.01.036. http://dx.doi.org/10.1016/j.jad.2007.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Angst J, Nock MK, Ruscio AM, Walters EE, Kessler RC. A risk index for 12-month suicide attempts in the National Comorbidity Survey Replication (NCS-R) Psychological Medicine. 2006;36(12):1747–1757. doi: 10.1017/S0033291706008786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borges G, Nock MK, Haro Abad JM, Hwang I, Sampson NA, Alonso J, et al. Kessler RC. Twelve month prevalence of and risk factors for suicide attempts in the WHO Mental Health Surveys. Journal of Clinical Psychiatry. 2010;71(12):1617–1628. doi: 10.4088/JCP.08m04967blu. http://dx.doi.org/10.4088/JCP.08m04967blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Hodges M, Godbout N. Traumatic stress, affect dysregulation, and dysfunctional avoidance: A structural equation model. Journal of Traumatic Stress. 2010;23:767–774. doi: 10.1002/jts.20578. [DOI] [PubMed] [Google Scholar]
- Britton PC, Ilgen MA, Rudd MD, Conner KR. Warning signs for suicide within a week of healthcare contact in Veteran decedents. Psychiatry Research. 2012;200:395–399. doi: 10.1016/j.psychres.2012.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E. Reasons for suicide attempts in a clinical sample of active duty soldiers. Journal of Affective Disorders. 2013;144:148–152. doi: 10.1016/j.jad.2012.06.030. [DOI] [PubMed] [Google Scholar]
- Busch KA, Fawcett J, Jacobs DG. Clinical correlates of inpatient suicide. Journal of Clinical Psychiatry. 2003 doi: 10.4088/jcp.v64n0105. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Web-based Injury Statistics Query and Reporting System (WISQARS) [online] 2011 Retrieved from www.cdc.gov/injury/wisqars/index.html.
- Conrad AK, Jacoby AM, Jobes DA, Lineberry TW, Shea CE, Arnold Ewing TD, et al. Kung S. A psychometric investigation of the Suicide Status Form II with a psychiatric inpatient sample. Suicide and Life-threatening Behavior. 2009;39(3):307–320. doi: 10.1521/suli.2009.39.3.307. [DOI] [PubMed] [Google Scholar]
- Fawcett J. Treating impulsivity and anxiety in the suicidal patient. Annals of the New York Academy of Sciences. 2001;932:94–102. doi: 10.1111/j.1749-6632.2001.tb05800.x. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Busch KA, Jacobs D, Kravitz HM, Fogg L. Suicide: A four-pathway clinical-biochemical model. Annals of the New York Academy of Sciences. 1997;836:288–301. doi: 10.1111/j.1749-6632.1997.tb52366.x. [DOI] [PubMed] [Google Scholar]
- Fawcett J, Scheftner WA, Fogg L, Clark DV, Young MA, Hedeker D, Gibbons R. Time-related predictors of suicide in major affective disorder. American Journal of Psychiatry. 1990b;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Field AP. Meta-analysis of correlation coefficients: A Monte Carlo comparison of fixed- and random-effects methods. Psychological Methods. 2001;6:161–180. doi: 10.1037/1082-989x.6.2.161. http://dx.doi.org/10.1037/1082-989X.6.2.161. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS. The Yale-Brown obsessive compulsive scale. II. Validity. Archives of General Psychiatry. 1989;46(11):1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Gradus JL, Qin P, Lincoln AK, Miller M, Lawler E, Sorensen, Lash TL. Post-traumatic stress disorder and completed suicide. American Journal of Epidemiology. 2010;171(6):721–727. doi: 10.1093/aje/kwp456. [DOI] [PubMed] [Google Scholar]
- Hall R, Platt D, Hall R. Suicide risk assessment: A review of risk factors for suicide in 100 patients who made severe suicide attempts. Psychosomatics. 1999;40:18–27. doi: 10.1016/S0033-3182(99)71267-3. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- Hedges LV, Vevea JL. Fixed- and random effects models in meta-analysis. Psychological Methods. 1998;3:486–504. http://dx.doi.org/10.1037/1082-989X.3.4.486. [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. British Medical Journal. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. http://dx.doi.org/10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornig CD, McNally RJ. Panic disorder and suicide attempts: A reanalysis of data from the epidemiologic catchment area study. British Journal of Psychiatry. 1995;167:76–79. doi: 10.1192/bjp.167.1.76. [DOI] [PubMed] [Google Scholar]
- Joiner TE. Why people die by suicide. Cambridge, MA, US: Harvard University Press; 2005. [Google Scholar]
- Kanwar A, Malik S, Prokop LJ, Sim LA, Feldstein D, Wang Z, Murad MH. The association between anxiety disorders and suicidal behaviors: A systematic review and meta-analysis. Depression and Anxiety. 2013;30(10):917–929. doi: 10.1002/da.22074. http://dx.doi.org/10.1002/da.22074. [DOI] [PubMed] [Google Scholar]
- Kaplan MS, McFarland BH, Huguet N, Newsom JT. Physical illness, functional limitations, and suicide risk: A population-based study. American Journal of Orthopsychiatry. 2007;77(1):56–60. doi: 10.1037/0002-9432.77.1.56. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Kazdin AE, Offord DR, Kessler RC, Jensen PS, Kupfer DJ. Coming to terms with the terms of risk. Archives of General Psychiatry. 1997;54:337–344. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- National Suicide Prevention Lifeline. Suicide Risk Factors [online] [Accessed October 16, 2015];2015 http://www.suicidepreventionlifeline.org/learn/riskfactors.aspx.
- Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. American Journal of Psychiatry. 1993;150(4):600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine. 2006;3(11):e442. doi: 10.1371/journal.pmed.0030442. http://dx.doi.org/10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. http://dx.doi.org/10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Nepon J, Belik SL, Bolton J, Sareen J. The relationship between anxiety disorders and suicide attempts: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Depression and Anxiety. 2010;27(9):791–798. doi: 10.1002/da.20674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK. Self-injury. Annual Review of Clinical Psychology. 2010;6:339–363. doi: 10.1146/annurev.clinpsy.121208.131258. [DOI] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the national comorbidity survey replication. Molecular Psychiatry. 2010a;15(8):868–876. doi: 10.1038/mp.2009.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiologic Reviews. 2008;30(1):133–154. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Hwang I, Sampson N, Kessler RC, Angermeyer M, Beautrais A, et al. Williams DR. Cross-national analysis of the associations among mental disorders and suicidal behavior: Findings from the WHO world mental health surveys. PLoS Medicine. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Ursano RJ, Heeringa SG, Stein MB, Jain S, Raman R, et al. Kessler RC. Mental disorders, comorbidity, and pre-enlistment suicidal behavior among new soldiers in the U.S. Army: Results from the Army Study to Assess Risk and Resilience in Servicemembers (ARMY STARRS) Suicide and Life-threatening Behavior. 2015 doi: 10.1111/sltb.12153. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noyes R. Suicide and panic disorder: A review. Journal of Affective Disorders. 1991;22:1–11. doi: 10.1016/0165-0327(91)90077-6. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review. 2007;27(5):572–581. doi: 10.1016/j.cpr.2007.01.015. http://dx.doi.org/10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Rector NA, Kamkar K, Riskind JH. Misappraisal of time perspective and suicide in the anxiety disordres: The multiplier effect of looming illusions. International Journal of Cognitive Therapy. 2008;1(1):69–79. [Google Scholar]
- Ribeiro JD, Silva C, Joiner TE. Overarousal interacts with a sense of fearlessness about death to predict suicide risk in a sample of clinical outpatients. Psychiatry Research. 2014a;218(1–2):106–112. doi: 10.1016/j.psychres.2014.03.036. [DOI] [PubMed] [Google Scholar]
- Ribeiro JD, Bender TW, Buchman JM, Nock MK, Rudd MD, Bryan CJ, et al. Joiner TE. An investigation of the interactive effects of the capability for suicide and acute agitation on suicidality in a military sample. Depression and Anxiety. 2015 doi: 10.1002/da.22240. [DOI] [PubMed] [Google Scholar]
- Riskind JH. Looming vulnerability to threat: A cognitive paradigm for anxiety. Behaviour Research and Therapy. 1997;35:685–702. doi: 10.1016/s0005-7967(97)00011-9. [DOI] [PubMed] [Google Scholar]
- Riskind JH, Long DG, Williams NL, White J. Desperate acts for desperate times: Looming vulnerability and suicide. In: Joiner T, editor. Suicide science. New York: Plenum Press; 2000. pp. 105–115. [Google Scholar]
- Robins E. The final months: A study of the lives of 134 persons who committed suicide. New York, NY: Oxford University Press; 1981. [Google Scholar]
- Rudd MD, Berman AL, Joiner TE, Nock MK, Silverman MM, Mandrusiak M, et al. Witte T. Warning signs for suicide: Theory, research, and clinical applications. Suicide and Life-threatening Behavior. 2006;36:255–265. doi: 10.1521/suli.2006.36.3.255. [DOI] [PubMed] [Google Scholar]
- Sareen J. Anxiety disorders and risk for suicide: Why such controversy? Depression and Anxiety. 2011;28(11):941–945. doi: 10.1002/da.20906. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Afifi TO, de Graaf R, Asmundson GJ, ten Have M, Stein MB. Anxiety disorders and risk for suicide ideation and suicide attempts: A population-based longitudinal study of adults. Archives of General Psychiatry. 2005;62(11):1249–1257. doi: 10.1001/archpsyc.62.11.1249. [DOI] [PubMed] [Google Scholar]
- Shneidman ES. Suicide as psychache: A clinical approach to self-destructive behavior. Northvale, NJ: Jason Aronson; 1993. [Google Scholar]
- Silva C, Ribeiro JD, Joiner TE. Mental disorders and thwarted belongingness, perceived burdensomeness, and acquired capability for suicide. Psychiatry Research. 2015;226:316–327. doi: 10.1016/j.psychres.2015.01.008. [DOI] [PubMed] [Google Scholar]
- Šimundić AM. Measures of diagnostic accuracy: Basic definitions. Medical & Biological Sciences. 2008;22(4):61–65. [PMC free article] [PubMed] [Google Scholar]
- Thibodeau MA, Welch PG, Sareen J, Asmundson GJ. Anxiety disorders are independently associated with suicide ideation and attempts: Propensity score matching in two epidemiological samples. Depression and Anxiety. 2013;30(10):947–954. doi: 10.1002/da.22203. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite S, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychological Review. 2010;117(2):575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warshaw MG, Massion AO, Peterson LG, Pratt LA, Keller MB. Suicidal behavior in patients with panic disorder: Retrospective and prospective data. Journal of Affective Disorders. 1995;34(3):235–247. doi: 10.1016/0165-0327(95)00022-f. [DOI] [PubMed] [Google Scholar]
- Way B, Miraglia R, Sawyer D, Beer R, Eddy J. Factors related to suicide in New York state prisons. International Journal of Law and Psychiatry. 2005;28:207–221. doi: 10.1016/j.ijlp.2004.09.003. http://dx.doi.org/10.1016/j.ijlp.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicide ideation and suicide attempts in panic disorder and attacks. New England Journal of Medicine. 1989;321:1209–1214. doi: 10.1056/NEJM198911023211801. [DOI] [PubMed] [Google Scholar]
- Wenzel A, Beck AT. A cognitive model of suicidal behavior: Theory and treatment. Applied and Preventive Psychology. 2008;12:189–201. http://dx.doi.org/10.1016/j.appsy.2008.05.001. [Google Scholar]
- Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: Scientific and clinical applications. Washington, DC: APA Books; 2008. in press. [Google Scholar]
- Wilcox HC, Storr CL, Breslau N. Posttraumatic stress disorder and suicide attempts in a community sample of urban American young adults. Archives of General Psychiatry. 2009;66:305–311. doi: 10.1001/archgenpsychiatry.2008.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Public health action for the prevention of suicide: A framework. Geneva, Switzerland: WHO Press; 2012. [Google Scholar]
- Zamora J, Muriel A, Abraira V. Meta-DiSc: Meta-analysis of diagnostic and screening tests, version 1.4. Madrid, Spain: 2014. [Google Scholar]


