Abstract
Background
Return to work following acute myocardial infarction (AMI) is an important outcome and is particularly relevant to young patients. Women may be at a greater risk for not returning to work given evidence of their worse recovery after AMI than similarly aged men. However, sex differences in return to work after AMI has not been studied extensively in a young population (≤55 years).
Methods and Results
We analyzed data from 1680 AMI patients aged 18–55 years (57% women) participating in the VIRGO study (Variation in Recovery: Role of Gender on Outcomes of Young AMI patients) who were working full time (≥35 hours) prior to the event. Data were obtained by medical record abstraction and patient interviews. We conducted multivariable regression analyses to examine sex differences in return to work at 12 months after AMI, and the association of patient characteristics with return to work. Compared to young men, young women were less likely to return to work (89% vs. 85%, P=0.018); however this sex difference was not significant after adjusting for patient socio-demographic characteristics, psychosocial factors, and health measures. Being married, engaging in a professional or clerical type of work, having more favorable physical health, and having no prior coronary disease or hypertension were significantly associated with a higher likelihood of return to work at 12 months.
Conclusion
Among a young population, women are less likely to return to work after AMI than men. This disadvantage is explained by differences in demographic, occupational and health characteristics.
Keywords: acute myocardial infarction, women, young, recovery, gender differences
Subject Terms: Myocardial infarction, Women, Health services, Quality and outcomes
Return to work following acute myocardial infarction (AMI) represents an important indicator of recovery from illness and return to a degree of ‘normality’.1 Return to work also has important economic significance and implications for subsequent health.1 Employment is reflective of superior health and wellbeing,2 whereas being out of work often has negative consequences on physical and mental health.3 Unemployed individuals have higher rates of premature death, a greater risk of coronary heart disease, high rates of depression/anxiety, as well as loss of income and financial hardship.2, 4
Return to work may be particularly important for young patients who are likely to be employed at the time of their AMI and who may not have contemplated and/or are not prepared for loss of employment. Young women may be especially vulnerable for leaving the workforce given that they tend to have worse health outcomes following AMI than their male counterparts.5 Previous studies that have examined return to work post-AMI in young and middle aged adults only included sex as a covariate rather than explicitly addressing sex differences as a primary objective.6, 7 Moreover, they were mostly based on outdated data, limited by small sample sizes,1, 8–10 and focused only on conventional clinical factors without detailed patient-reported health and psychosocial measures. As the social context for women has changed dramatically over the past few decades in terms of women’s participation in the labor force,11 a comprehensive assessment of sex differences in return to work after AMI using recent data is warranted.
To address this gap in knowledge, we utilized data from the VIRGO study (Variation in Recovery: Role of Gender on Outcomes of Young Acute Myocardial Infarction Patients), the largest sample of young working-age patients with AMI,12 to examine sex differences in the likelihood of return to work at 12 months after an AMI, and to identify other patient characteristics that may help explain any observed sex difference in return to work.
Understanding return to work in male and female patients, including the contribution of detailed patient characteristics may help to develop tailored interventions for young female and male patients after an AMI.
METHODS
Study Design and Sample
Our study utilizes data gathered from the VIRGO study.12 Between August 2008 and January 2012, 3,572 patients hospitalized with AMI were enrolled from 103 United States (US), 24 Spanish, and 3 Australian hospitals. The VIRGO study was designed to investigate factors associated with higher mortality in young women with AMI,12 and used a 2:1 female to male enrollment ratio to enrich the study’s inclusion of young women. The VIRGO methodology and design have been previously described.12 In brief, participants were 18–55 years old, and AMI was confirmed by increased cardiac biomarkers within 24 hours of admission, and at least either additional evidence of myocardial ischemia or electrocardiographic changes. Included patients presented directly to the enrolling site or were transferred within the first 24 hours of presentation to ensure that primary clinical decision making occurred at the enrolling site. Exclusion criteria included (a) non-English or non-Spanish speaking patients’, (b) inability to provide informed consent or be contacted for follow-up, (c) incarceration, and (d) those patients who developed elevated cardiac markers because of elective coronary revascularization, or had an AMI as the result of physical trauma.
We collected patients’ baseline characteristics from medical chart abstraction and standardized in-person interviews administered by trained personnel during the index AMI admission. Patient interviews were also conducted by telephone at 12 months post-AMI.12 Institutional Review Board approval was obtained at each participating institution, and patients provided informed consent for their study participation. Our analysis included 1680 subjects (962 women, 719 men) who were working for pay full time (defined as working for pay and working at least 35 hours per week) at baseline (i.e. prior to their AMI). This was determined based on each patient’s response to questions whether they “currently work for pay” and if so, how many hours per week they usually worked.
Measures
Return to Work
Return to work was defined as a dichotomous measure indicating whether a patient was currently working for pay at 12 months after AMI, regardless of hours worked. We did not distinguish part-time versus full-time working at the 12 month time period as few patients who returned to work had less than 35 work hours per week (i.e. 3.9% at 12 months).
Socio-demographic Characteristics and Health Measures
Socio-demographic variables collected at the baseline hospitalization for AMI included information on age, race, marital status, number of children living in the household (0, 1–2, >3), education, and insurance status. Baseline health measures included hypertension, diabetes, dyslipidemia, Short-form 12 (SF-12)13 physical component summary (PCS) score, smoking status, prior coronary artery disease (CAD, including AMI, percutaneous coronary intervention [PCI], coronary artery bypass grafting [CABG]), obesity (body mass index [BMI] ≥30kg/m2), ST-elevation myocardial infarction (STEMI), ejection fraction <40%, and length of stay for baseline admission. The SF-12 PCS score ranges from 0–100, with higher scores indicating greater functioning. A score of 50 represents the US population average, with a standard deviation of 10 points.14, 15 In addition, the VIRGO study also collects information on whether patients received cardiac rehabilitation during the 12 months after AMI.
Occupational Characteristics
For patients who indicated “currently work for pay”, the VIRGO study asked their detailed employment status including whether the patient had changed jobs in the past year, working hours per week and type of their primary/main job (professional, business, clerical, skilled labor, general labor, self-employed, homemaker, farmer, police/military, receiving disability/social security, health profession and other). We used these variables to measure patients’ baseline occupational characteristics. Similar to previous studies,8, 16 we classified these occupations into one of four categories: (1) manual worker (general labor), (2) professional and clerical (professional, business, clerical, health profession), (3) Semi-skilled professional (policy/military, farmer, skilled labor), and (4) other ( self-employed, homemaker, other).8, 16 In regards to the homemaker category, these were patients who identified as currently working for pay and working at least 35 hours a week, but indicated their primary/main job as “homemakers”. The VIRGO study also ascertains reasons why patients stopped working at 12 months, including: (1) fired/lost job, (2) prefer not to work, and (3) no longer able to work.
Psychosocial Factors
Measures of psychosocial factors included depression, social support, stress and financial strain measured at baseline. Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9),17 a standardized and validated instrument that has been widely used among cardiac populations.18 The PHQ quantifies the frequency of depressive symptoms experienced in the past 2 weeks based on the 9 Diagnostic and Statistical Manual of Mental Disorders (4th edition) criteria for a major depressive disorder.19 A PHQ-9 score ≥10 was used as indicating depression.20 Perceived social support was measured using the ENRICHD Social Support Inventory (ESSI).21 This scale is a reliable and valid assessment of social support in cardiac populations22 and has been used by several studies to evaluate social support after AMI.23 For this study, social support was defined as low versus high social support.
Perceived stress was measured using the 14-item Perceived Stress Scale (PSS-14),24 which has been previously used in AMI populations.24, 25 This item enquires about patients feelings over the past month, with examples such as “In the last month, how often have you been upset because of something that happened unexpectedly.” Each items was scored as 0 for never and 4 for very often, with the overall score ranging from 0 to 56. Higher scores refer to greater stress levels. Stress in this study was coded as low, medium and high based on tertiles of the overall score. Financial strain was defined as having “just enough to make ends meet” or “not enough to make ends meet” (versus having some money left over) based on patients’ response to question “in general, how do your finances usually work out at the end of the month? Do you usually end up with: some money left over, just enough to make ends meet, not enough to make ends meet.”
Statistical Analysis
Bivariate analyses were used to compare differences in baseline characteristics between women and men. In addition, we compared patient characteristics between those who returned to work at 12 months post-AMI and those who did not. Statistical differences between groups were determined using chi-squared test or Fisher’s exact test for categorical variables and student’s t-test or Wilcoxon Rank Sum test for continuous variables. In addition to the 12 month interview, the VIRGO study also asked whether a patient returned to work within 1 week, 2 weeks, 1 month, 3 months or 6 months after discharge. Drawing on this information, we also plotted the percentage of patients who returned to work at these various time points over the 12 months follow up period by sex.
We developed a multivariable logistic regression model to assess sex difference in the likelihood of return to work at 12 months post-AMI, while adjusting for other patient socio-demographic characteristics, psychosocial factors, and health status.10 These covariates were selected based on consideration of their clinical relevance. As there was no evidence for significant interaction effect between sex and country, we included country as a control variable in the model. As a sensitivity analysis, we estimated an additional multivariable logistic regression model only including covariates that achieved statistical significance in univariate testing.
We also compared characteristics of patients who had missing data on the outcome variable (i.e., status of return to work at 12 month post-AMI) (n=258 patients had missing data at 12 months) with those who had complete data (Supplemental Table 1). Due to observed differences in patient characteristics between these patients, we conducted a sensitivity analysis using multiple imputation method to address the missing data. As the results from analysis with multiple imputation were similar to those using complete case analysis, we reported results from the complete case analysis. In addition, intra-hospital correlation was minimal with a between hospital variation of 0.04, therefore, we did not adjust for site clustering. For all analyses, a p-value less than 0.05 was considered statistically significant. All analyses were conducted using SAS 9.3 (SAS Institute Inc., Cary, NC) and VIRGO data version 1.0.
RESULTS
Baseline Characteristics
Baseline characteristics of the sample by sex are shown in Table 1 (see country-stratified data in Supplemental Tables 2–3). Women and men were of a similar age. However, compared with men, women were more likely to be black, to be unmarried, to have more than a high school education, and had fewer and/or no children living in the household. In terms of occupational characteristics, women worked fewer hours per week, and were more likely to work in professional or clerical roles. Women were also more likely to have diabetes and poorer physical health, but were less likely to have STEMI and had a lower ejection fraction than men. Regarding psychosocial factors, women were more likely than men to be depressed, perceive greater stress, and experience greater financial strain at baseline (Table 1).
Table 1.
Comparison of baseline characteristics of AMI patients between men and women.
| Men (N=718) | Women (N=962) | P Value* | |
|---|---|---|---|
| Socio-demographics (%) | |||
| Age (Median, IQR) | 48.0 (8.0) | 48.0 (8.0) | 0.070 |
| Country | 0.153 | ||
| US | 82.5 | 85.6 | |
| Spain | 15.4 | 13.2 | |
| Australia | 2.1 | 1.2 | |
| Race | <0.001 | ||
| White | 85.4 | 78.7 | |
| Black | 7.9 | 14.7 | |
| Other | 6.7 | 6.7 | |
| Married | 67.6 | 49.9 | <0.001 |
| Number of children living in household | <0.001 | ||
| 0 | 4.9 | 6.8 | |
| 1–2 | 77.0 | 78.2 | |
| ≥ 3 | 18.1 | 15.0 | |
| Education | 0.027 | ||
| Less than high school | 3.1 | 4.1 | |
| Some high school | 36.5 | 30.4 | |
| More than high school | 60.4 | 65.5 | |
| Insurance status | 88.3 | 90.0 | 0.277 |
| Changed jobs in last year | 11.6 | 11.2 | 0.766 |
| Work hours (Mean, SD) | 48.7 (11.3) | 43.9 (8.6) | <0.001 |
| Work classification/type of work | <0.001 | ||
| Manual worker | 12.0 | 10.1 | |
| Professional/clerical | 42.1 | 65.9 | |
| Semi-skilled | 26.6 | 8.2 | |
| Other | 19.4 | 15.8 | |
|
| |||
| Health measures (%) | |||
| Hypertension | 57.9 | 57.6 | 0.886 |
| Diabetes | 16.4 | 26.3 | <0.001 |
| Dyslipidemia | 70.6 | 62.4 | <0.001 |
| Current smoking | 54.6 | 53.9 | 0.756 |
| Prior CAD | 16.3 | 12.9 | 0.049 |
| Obesity (BMI ≥30kg/m2 ) | 44.6 | 48.1 | 0.154 |
| Physical health (SF-12 PCS) (Mean, SD) | 48.9 (9.6) | 47.4 (10.2) | 0.004 |
| STEMI | 61.4 | 50.6 | <0.001 |
| EF <40% | 11.1 | 8.0 | 0.035 |
| Cardiac rehabilitation | 42.2 | 41.3 | 0.743 |
| LOS during admission (Mean, SD) | 4.1 (3.4) | 4.4 (3.9) | 0.177 |
|
| |||
| Psychosocial factors | |||
| Depression (PHQ-9) | 16.6 | 27.7 | <0.001 |
| Stress (PSS-14) | <0.001 | ||
| Low stress level | 40.4 | 29.6 | |
| Median stress level | 34.4 | 33.4 | |
| High stress level | 25.3 | 37.0 | |
| Low Social support (ESSI) | 18.8 | 17.0 | 0.330 |
| Financial strain† (%) | 48.5 | 60.8 | <0.001 |
Student’s t-test for continuous variables that were normally distributed and Wilcoxon Rank-Sum test for continuous variable that were not normally distributed. Chi-Square or Fisher’s exact Test for categorical variables.
Financial strain defined as composite of ‘just enough to make ends meet’ and ‘not enough to make ends meet’.
Abbreviations: AMI= acute myocardial infarction, CAD= coronary artery disease, STEMI= ST-elevation myocardial infarction, EF= ejection fraction, LOS=length of stay, PHQ-9= Patient Health Questionnaire-9, PSS-14= 14-item Perceived Stress Scale, ESSI= ENRICHD Social Support Inventory.
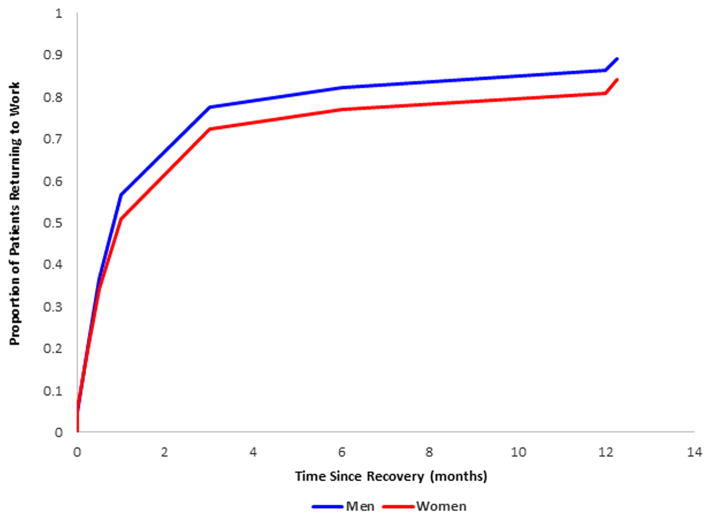
Return to Work at 12 Months
At 12 months follow-up, 86% of patients returned to work. However, women were slightly less likely to return to work, in comparison to men (85% women vs. 89% men, p=0.02). Figure 1 is a descriptive representation of the proportion of women and men who returned to work at various time points after AMI. For example, the rate of return to work at 1 month was 92% and deceased to 86% at 12 months post AMI.
Figure 1.
Percentage of patients (%) who returned to work in months (red=women, blue=men).
Table 2 compares the baseline characteristics of AMI patients between those who returned to work and those who did not return to work at 12 months. Patients who returned to work at 12 months were more likely to be married, to have more than a high school education, have private insurance, were less likely to have changed jobs in the past year, worked more hours, reported being in more professional/clerical roles, had fewer risk factors and had less depression, less stress, more social support and less financial strain (Table 2).
Table 2.
Comparison of baseline characteristics of AMI patients between those who were and were not working at 12 months.
| 12 months post-AMI (N=1422) | |||
|---|---|---|---|
| RTW (N=1229) | Not RTW (N=193) | P Value | |
| Socio-demographics (%) | |||
| Age (Median, IQR) | 48.0 (8.0) | 48.0 (9.0) | 0.678 |
| Race | 0.353 | ||
| White | 84.1 | 80.3 | |
| Black | 10.2 | 13.5 | |
| Other | 5.7 | 6.2 | |
| Married | 62.1 | 43.5 | <0.001 |
| Number of children living in household | 0.083 | ||
| 0 | 6.7 | 2.9 | |
| 1–2 | 76.2 | 85.7 | |
| ≥3 | 17.1 | 11.4 | |
| Education | <0.001 | ||
| Less than high school | 3.0 | 7.0 | |
| High school | 30.8 | 40.1 | |
| More than high school | 66.2 | 52.9 | |
| Insurance status | 91.7 | 78.7 | <0.001 |
| Changed jobs in last year | 10.6 | 16.1 | 0.025 |
| Work hours per week (Mean, SD) | 46.3 (10.1) | 44.7 (10.1) | 0.044 |
| Work classification | <0.001 | ||
| Manual worker | 8.9 | 20.7 | |
| Professional/clerical | 59.6 | 42.0 | |
| Semi-skilled | 16.0 | 13.5 | |
| Other | 15.5 | 23.8 | |
|
| |||
| Health measures (%) | |||
| Hypertension | 56.8 | 60.1 | 0.388 |
| Diabetes | 20.5 | 28.0 | 0.019 |
| Dyslipidemia | 65.2 | 68.9 | 0.309 |
| Current smoking | 51.0 | 63.7 | 0.001 |
| Prior CAD | 12.6 | 19.7 | 0.008 |
| Prior Stroke/TIA | 1.5 | 3.1 | 0.124 |
| Obesity (BMI ≥30kg/m2 ) | 47.0 | 45.8 | 0.766 |
| Physical health (SF-12 PCS) (Mean, SD) | 48.6 | 44.7 | <0.001 |
| STEMI | 55.7 | 48.7 | 0.071 |
| EF <40% | 8.4 | 13.5 | 0.024 |
| Cardiac rehabilitation | 43.1 | 32.6 | 0.007 |
| LOS during admission (Mean, SD) | 4.1 (3.4) | 5.7 (5.2) | <0.001 |
|
| |||
| Psychosocial factors | |||
| Depression (PHQ-9) | 21.2 | 36.8 | <0.001 |
| Stress (PSS-14) | <0.001 | ||
| Low stress level | 35.9 | 27.6 | |
| Medium stress level | 34.0 | 27.6 | |
| High stress level | 30.1 | 44.8 | |
| Low social support (ESSI) | 16.5 | 20.9 | 0.131 |
| Financial strain† (%) | 51.1 | 70.8 | <0.001 |
Student’s t-test for continuous variables that were normally distributed; Wilcoxon Rank-Sum test for continuous variables that were not normally distributed. Chi-Square or Fisher’s exact Test for categorical variables.
Financial strain defined as composite of ‘just enough to make ends meet’ and ‘not enough to make ends meet’.
Abbreviations: AMI= acute myocardial infarction, RTW= return to work, CAD= coronary artery disease, STEMI= ST-elevation myocardial infarction, EF= ejection fraction, LOS=length of stay, PHQ-9= Patient Health Questionnaire-9, PSS-14= 14-item Perceived Stress Scale, ESSI= ENRICHD Social Support Inventory.
Among patients who did not return to work at 12 months post-AMI (N=193), women and men cited reasons for not returning that were not significantly different (P=0.90) (Table 3). Six percent of women and 3% of men preferred not to work, whereas 32% of women and 33% of men reported that they were fired and/or lost their job. The rest reported no longer able to work.
Table 3.
Reasons for not returning to work at 12 months
| 12 Month | ||||
|---|---|---|---|---|
| No Return (N=193) | ||||
| Overall sample (N=193) | Men (N=66) | Women (N=127) | P Value | |
| No longer able to work (%) | 62.9 | 63.9 | 62.5 | |
| Fired/lost job (%) | 32.4 | 33.3 | 31.9 | 0.90 |
| Prefer not to work (%) | 4.7 | 2.8 | 5.6 | |
Adjusted Sex Difference in Return to Work at 12 months
To assess the independent association of sex with return to work at 12 months post-AMI after adjusting for potential confounders, multivariable logistic regression analysis was undertaken. The unadjusted and adjusted associations between sex and return to work are presented in Table 4.
Table 4.
The unadjusted and adjusted association between sex and return to work at 12 months
| Before Adjustment for Patient Characteristics | After Adjustment for Patient Characteristics | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95% CI | OR | 95% CI | |||
| Sex (reference is male) | 0.68 | 0.50 | 0.94 | 0.53 | 0.27 | 1.05 |
| Age (5-year as a unit) | 1.04 | 0.81 | 1.33 | |||
| Other race (reference is Black)* | 1.26 | 0.34 | 4.67 | |||
| White (reference is Black) | 1.52 | 0.69 | 3.34 | |||
| Marital status (reference is non-married) | 2.79 | 1.51 | 5.16 | |||
| Country (reference is Spain) | 0.93 | 0.36 | 2.46 | |||
| Children group (No child vs more than 2) | 3.43 | 0.57 | 20.59 | |||
| Children group (1–2 vs more than 2 children) | 0.90 | 0.40 | 2.02 | |||
| Education (high school vs less high school) | 1.16 | 0.32 | 4.18 | |||
| Education (more vs. less than high school) | 1.40 | 0.37 | 5.27 | |||
| Insurance (reference is no insurance) | 2.18 | 0.98 | 4.86 | |||
| Changed jobs (reference is changed jobs) | 1.14 | 0.51 | 2.53 | |||
| Weekly working hours (10-hour as a unit) | 0.99 | 0.76 | 1.29 | |||
| Work type (Professional vs Manual worker) | 5.22 | 2.31 | 11.82 | |||
| Work type (Semi-skilled vs Manual worker) | 2.14 | 0.85 | 5.41 | |||
| Work type (Others vs Manual worker) | 2.11 | 0.84 | 5.30 | |||
| Depression (reference is Yes) | 1.53 | 0.76 | 3.10 | |||
| Stress (low vs high) | 0.89 | 0.42 | 1.90 | |||
| Stress (medium vs high) | 1.95 | 0.93 | 4.09 | |||
| Social support (reference is low social support) | 1.15 | 0.57 | 2.33 | |||
| Financial Strain (reference is financial strain) | 1.57 | 0.83 | 3.00 | |||
| Physical health | 1.04 | 1.01 | 1.07 | |||
| Hypertension (reference is Yes) | 0.38 | 0.20 | 0.69 | |||
| Diabetes (reference is Yes) | 1.05 | 0.52 | 2.11 | |||
| Dyslipidemia (reference is Yes) | 1.13 | 0.59 | 2.16 | |||
| Smoking (reference is Yes) | 1.04 | 0.57 | 1.88 | |||
| Prior CAD (reference is Yes) | 2.25 | 1.04 | 4.90 | |||
| Obesity (reference is Yes) | 0.64 | 0.35 | 1.16 | |||
| STEMI (reference is NSTEMI) | 1.10 | 0.63 | 1.91 | |||
| EF<40% (reference is Yes) | 1.94 | 0.87 | 4.33 | |||
| Cardiac rehabilitation (reference is Yes) | 1.47 | 0.79 | 2.72 | |||
| Length of Stay | 0.93 | 0.88 | 1.00 | |||
Other race = American Indian, Asian, Other, unknown (compared with black race).
Abbreviations: OR = odds ratio, CI = confidence interval, CAD = coronary artery disease, EF = ejection fraction.
Before adjusting for other patient characteristics, women had lower likelihood of return to work compared with men (unadjusted odds ratio [OR] = 0.68, 95% confidence interval [CI]: 0.50, 0.94). However, following adjustment for all factors shown in Table 4 (i.e. including patient socio-demographics, health status and psychosocial factors), there was no statistically significant difference between women and men in their likelihood of return to work (OR= 0.53, 95% CI: 0.27, 1.05). Several factors were associated with increased rates of return to work at 12 months, such as being married (OR= 2.79, 95% CI: 1.51, 5.16), engaging in professional or clerical type of work (versus manual work) (OR 5.22, 95% CI: 2.31, 11.82), having more favorable physical health (OR 1.04, 95% CI: 1.01, 1.07), and no prior CAD (OR=2.25, 95% CI: 1.04, 4.90). In addition, patients with no history of hypertension (OR=0.38, 95% CI: 0.20, 0.69) had decreased odds of returning to work (Table 4).
In the sensitivity analysis of only including covariates that achieved statistical significance in univariate testing (p<0.05), we found that the adjusted OR for sex was 0.72 (95% CI: 0.47, 1.09). Covariates showing statistical significance in univariate testing included marital status, country, education, insurance status, changed jobs in the last year, weekly working hours, depression, perceived stress, financial strain, physical health, diabetes, smoking, prior CAD, EF <40%, cardiac rehabilitation, and length of stay.
DISCUSSION
We observed that, in a young population (≤55 years), women were less likely to return to work than men. We also found that their increased risk was largely explained by socio-demographic, occupational, and health factors. Further, our study demonstrates that several patient level and occupational characteristics are significantly associated with a patient’s likelihood of returning to work. As 14% of our population did not return to work following an AMI, these factors may provide worthwhile targets for future interventions to improving AMI patients’ resumption to work and may promote effective communication between physicians and patients. For example, more support may be required for patients in manual or semi-skilled labor roles (which may require intense physical activity)26, 27 and/or these patients may not have the education or training to seek alterative work in clerical or professional roles.28 In addition, cardiac rehabilitation or home healthcare which seeks to improve the quality of life of patients, including providing more social supports, may be worthwhile targets for intervention as 63% of those not retuning to work following AMI reported that they were no longer able to work, perhaps due to deteriorating health.1
Our study extends the literature in several important ways. First, this is the largest and most contemporary study to investigate factors associated with work-related outcomes in young patients, particularly young women, following AMI. Younger women are an important subgroup to investigate as they have been shown to experience more adverse outcomes following AMI compared with young men.5 Second, we were able to include detailed clinical and patient psychosocial measures (e.g., depression) in our study,1, 29–33 which were mostly not included in previous sex-based research but have been shown to be more prominent in young women following AMI.34–36
Our study also enriches the literature by demonstrating a relatively high rate of return to work following AMI in this unique younger patient population. Previous estimates of return to work after an AMI varied widely across studies, ranging from 37% to 85% at 12 months, however these studies did not focus on younger patients.1, 37, 38 Our study showed that 85% women and 89% men returned to work at 12 months, which is consistent with the upper range reported in previous studies. The relatively high rates in our sample may be due to the younger age group and improvements in cardiac management over the past decade, as prior studies tended to have older patients and were based on data from the 1970–90’s.1, 9, 39 It is also likely that some of the discrepancies in resumption rates observed in our study, relative to other studies, may be due to differences in study design (i.e. enrollment selection, follow up duration after AMI, age of patient population, and definition of return to work), and contextual differences between countries (e.g., differences in society and patients attitudes, insurance support for workers, social welfare systems, sickness benefits, and employment protection laws).
Moreover, we found a sex difference in crude return to work rates at 12 months after AMI, which were explained by other patient characteristics between women and men. After adjusting for these characteristics, the difference in likelihood of return to work between women and men was no longer significant. Based on our prior work, we hypothesize that women may be less likely to return to work due to a mixture of unfavorable psychosocial risk profiles than men, which may hinder their recovery over the full year. For example, women may have a higher burden of stress, poorer health status and/or quality of life, more depression, and fewer social supports following AMI.34–36 In addition, women have more caregiving demands (i.e. caring for children and elderly parents), as well as a greater burden of household duties than men, which may impact on their likelihood of resuming work following AMI.40, 41 These factors may explain the loss of statistical significance in sex difference after our model adjusted for a comprehensive set of patient demographic, health and psychosocial characteristics.
Although previous research generally demonstrated no sex differences in the rates of return to work in patients following AMI,8, 9, 42,9, 43–45 some studies found a lower rate of return to work in women.6, 7, 45, 46 By using more up-to-date data and larger sample sizes, our study provided additional evidence supporting a small crude sex difference in rates of returning to work in younger patients after AMI, which was accounted for by a range of patient level and occupational factors. Women and men, however, differed in some key characteristics. For example, being married was strongly associated with a patient’s likelihood of return to work at 12 months, and having a professional/clerical job was associated higher likelihood of return to work at 12 months. As a larger proportion of women were not married whereas a higher proportion of men held non-professional or non-clerical jobs, efforts to promote return to work for women and men may be tailored to target different populations - which may be at particularly higher risk. It is also important to note that similar to other young AMI patients,47 over 50% of our sample smoked and 48% were obese. These high-risk populations may provide future targets for intervention; since we demonstrated that current smokers were less likely to return to work and obesity has been shown in other studies as negatively affect recovery after AMI.48 This study should be interpreted in the context of several limitations. First, we lacked detailed information on psychosocial aspects of the work environment (i.e. workplace stress, workplace social support, job satisfaction, motivation to resume work), which are critical issues in understanding the duration of sickness absence and health risks associated with return to work.49 Second, the finding that psychosocial factors were not associated with return to work in our study was surprising, as they were shown to be more important than conventional clinical factors in previous studies.1 This difference in findings may be due to the fact that we used baseline psychosocial factors to predict 1-year outcomes. As patients’ psychosocial status may change substantially over the 12 month period, future research assessing the influence of these factors as time-varying variables may provide additional insights. Third, we had missing data on return to work at 12 months; however, this limitation does not seem to have biased our results as patients with missing data were similar to those without missing data in regards to socio-demographics, psychosocial factors and health measures at each time point (Supplemental Table 1). In general, our VIRGO sample is directly comparable to similarly aged AMI patients observed in several other contemporary studies,50 supporting the generalizability of our study findings. Fourth, among patients who did not return to work at 12 months, 64% men and 63% women indicated that they were “no longer able to work”, yet we lacked more detailed information regarding the exact reasons they were not able to work. Such information would be useful for guiding future design of intervention and warrants close attention in subsequent research. In addition, we also lacked details regarding the exact reasons why a low proportion of young AMI patients did not attend cardiac rehabilitation programs (i.e. 40–42% of women and men in our sample), which can be essential for informing ways to improve cardiac rehabilitation in younger patients post AMI..
CONCLUSION
In conclusion, we have demonstrated that in a young population of patients (18–55 years), women are less likely to return to work 12 months following AMI compared with similarly aged men. We show that women’s increased risk is largely explained by adjustment for patient demographic, occupational, psychosocial and health factors. In addition, our results also suggest several patient characteristics that were significantly associated with a patient’s likelihood of return to work. Interventions targeting these factors may be particularly helpful in improving AMI patients’ resumption to work.
Supplementary Material
WHAT IS KNOWN
Return to work following acute myocardial infarction (AMI) represents an important indicator of recovery from illness and is particularly relevant to young patients (18–55 years) who are likely to be employed at the time of their AMI.
Younger women in particular, may be at greater risk for not returning to work given evidence of their worse recovery after AMI than similarly aged men.
WHAT THE STUDY ADDS
This is the largest and most contemporary study to investigate factors associated with work-related outcomes in young patients, particularly young women, following AMI.
We demonstrate that young women are less likely to return to work 12 months following AMI compared with similarly aged men. This increased risk is explained by differences in demographic, occupational and health characteristics.
In addition to understanding sex differences, this study has identified several patient level and occupational characteristics that are significantly associated with a patient’s likelihood of returning to work. These factors may provide worthwhile targets for future interventions to improving AMI patients’ resumption to work and may promote effective communication between physicians and patients.
Acknowledgments
Sources of Funding
The VIRGO study was supported by a 4-year National Heart, Lung, and Blood Institute grant [number 5R01HL081153). IMJOVEN was supported in Spain by grant PI 081614 from the Fondo de Investigaciones Sanitarias del Instituto Carlos III, Ministry of Science and Technology, and additional funds from the Centro Nacional de Investigaciones Cardiovasculares (CNIC). Dr. Krumholz is supported by grant U01 HL105270-05 (Center for Cardiovascular Outcomes Research at Yale University) from the National Heart, Lung, and Blood Institute. Dr Bueno was supported in part by grant BA08/90010 from the Fondo de Investigación Sanitaria del Instituto de Salud Carlos III, Spain.
Footnotes
Disclosures
Drs. Krumholz and Xu work under contract with the Centers for Medicare & Medicaid Services to develop and maintain performance measures. Dr. Krumholz is chair of a cardiac scientific advisory board for UnitedHealth and is the recipient of research agreements from Medtronic, Inc. and Johnson and Johnson through Yale University to develop methods of clinical trial data sharing. In addition, Dr. Spertus is supported by grants from Gilead, Genentech, Lilly, Amorcyte, and EvaHeart, and has a patent Seattle Angina Questionnaire with royalties paid. Dr Bueno has received advisory/consulting fees from AstraZeneca, Bayer, Daichii-Sankyo, Eli-Lilly, Menarini, Novartis, Sanofi and Servier, and research grants from AstraZeneca. The other authors report no conflicts.
References
- 1.Perk J. Returning to work after myocardial infarction. Cardiovascular prevention and rehabilitation. 2007:317–323. [Google Scholar]
- 2.Waddell G, Burton K, Aylward M. Work and common health problems. J Insur Med. 2007;39:109–120. [PubMed] [Google Scholar]
- 3.Artazcoz L, Benach J, Borrell C, Cortes I. Unemployment and mental health: Understanding the interactions among gender, family roles, and social class. Am J Public Health. 2004;94:82–88. doi: 10.2105/ajph.94.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mital A, Desai A, Mital A. Return to work after a coronary event. J Cardiopulm Rehabil. 2004;24:365–373. doi: 10.1097/00008483-200411000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National registry of myocardial infarction 2 participants. N Engl J Med. 1999;341:217–225. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 6.Biering K, Nielsen TT, Rasmussen K, Niemann T, Hjollund NH. Return to work after percutaneous coronary intervention: The predictive value of self-reported health compared to clinical measures. PLoS One. 2012;7:e49268. doi: 10.1371/journal.pone.0049268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jackson L, Leclerc J, Erskine Y, Linden W. Getting the most out of cardiac rehabilitation: A review of referral and adherence predictors. Heart. 2005;91:10–14. doi: 10.1136/hrt.2004.045559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Attarchi MRA, Mirzamohammadi E, Mohammadi S. Assessment of the main factors influencing return to work following myocardial infarction: A longitudinal study. International Journal of Collaborative Research on Internal Medi. 2012;4:1305. [Google Scholar]
- 9.Bhattacharyya MR, Perkins-Porras L, Whitehead DL, Steptoe A. Psychological and clinical predictors of return to work after acute coronary syndrome. Eur Heart J. 2007;28:160–165. doi: 10.1093/eurheartj/ehl440. [DOI] [PubMed] [Google Scholar]
- 10.Abbas AE, Brodie B, Stone G, Cox D, Berman A, Brewington S, Dixon S, O'Neill WW, Grines CL. Frequency of returning to work one and six months following percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2004;94:1403–1405. doi: 10.1016/j.amjcard.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 11.Williams K, Kurina LM. The social structure, stress, and women's health. Clin Obstet Gynecol. 2002;45:1099–1118. doi: 10.1097/00003081-200212000-00018. [DOI] [PubMed] [Google Scholar]
- 12.Lichtman JH, Lorenze NP, D'Onofrio G, Spertus JA, Lindau ST, Morgan TM, Herrin J, Bueno H, Mattera JA, Ridker PM, Krumholz HM. Variation in recovery: Role of gender on outcomes of young ami patients (virgo) study design. Circ Cardiovasc Qual Outcomes. 2010;3:684–693. doi: 10.1161/CIRCOUTCOMES.109.928713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Wyrwich KW, Bullinger M, Aaronson N, Hays RD, Patrick DL, Symonds T. Estimating clinically significant differences in quality of life outcomes. Qual Life Res. 2005;14:285–295. doi: 10.1007/s11136-004-0705-2. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Kosinski M, Keller SD, Lincoln RI. SF-12: How to score the sf-12 physical and mental health summary scales. 3. Boston MA: Quality Metric Inc; 1998. [Google Scholar]
- 16.Lin S, Wang Z, Wang M. Work ability of workers in western china: Reference data. Occup Med (Lond) 2006;56:89–93. doi: 10.1093/occmed/kqi195. [DOI] [PubMed] [Google Scholar]
- 17.Kroenke K, Spitzer RL, Williams JB. The phq-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mallik S, Spertus JA, Reid KJ, Krumholz HM, Rumsfeld JS, Weintraub WS, Agarwal P, Santra M, Bidyasar S, Lichtman JH, Wenger NK, Vaccarino V. Depressive symptoms after acute myocardial infarction: Evidence for highest rates in younger women. Arch Intern Med. 2006;166:876–883. doi: 10.1001/archinte.166.8.876. [DOI] [PubMed] [Google Scholar]
- 19.American psychiatric association. Diagnostic and statistical manual of mental disorders, fourth edition (dsm-iv) Washington, DC: American Psychiatric Publishing; 1994. [Google Scholar]
- 20.Kroenke K, Spitzer RL. The phq-9: A new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–521. [Google Scholar]
- 21.The enrichd investigators. Enhancing recovery in coronary heart disease patients (enrichd): Study design and methods. The enrichd investigators. Am Heart J. 2000;139:1–9. doi: 10.1016/s0002-8703(00)90301-6. [DOI] [PubMed] [Google Scholar]
- 22.Vaglio J, Jr, Conard M, Poston WS, O'Keefe J, Haddock CK, House J, Spertus JA. Testing the performance of the enrichd social support instrument in cardiac patients. Health Qual Life Outcomes. 2004;2:24. doi: 10.1186/1477-7525-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell PH, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, Froelicher ES, Czajkowski S, Youngblood M, Huber M, Berkman LF. A short social support measure for patients recovering from myocardial infarction: The enrichd social support inventory. J Cardiopulm Rehabil. 2003;23:398–403. doi: 10.1097/00008483-200311000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 25.Rosengren A, Hawken S, Ounpuu S, Sliwa K, Zubaid M, Almahmeed WA, Blackett KN, Sitthiamorn C, Sato H, Yusuf S. Association of psychosocial risk factors with risk of acute myocardial infarction in 11119 cases and 13648 controls from 52 countries (the interheart study): Case-control study. Lancet. 2004;364:953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 26.Mirmohammadi SJ, Sadr-Bafghi SM, Mehrparvar AH, Gharavi M, Davari MH, Bahaloo M, Mostaghaci M, Sadr-Bafghi SA, Shokouh P. Evaluation of the return to work and its duration after myocardial infarction. ARYA Atheroscler. 2014;10:137–140. [PMC free article] [PubMed] [Google Scholar]
- 27.Fiabane E, Giorgi I, Candura SM, Argentero P. Return to work after coronary revascularization procedures and a patient's job satisfaction: A prospective study. Int J Occup Med Environ Health. 2014 doi: 10.2478/s13382-014-0313-5. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 28.Gelfand R, Flanders B, Haywood LJ. Return to work after myocardial infarction in a lower socioeconomic population. J Natl Med Assoc. 1981;73:855–857. [PMC free article] [PubMed] [Google Scholar]
- 29.Maeland JG, Havik OE. Return to work after a myocardial infarction: The influence of background factors, work characteristics and illness severity. Scand J Soc Med. 1986;14:183–195. doi: 10.1177/140349488601400404. [DOI] [PubMed] [Google Scholar]
- 30.Maeland JG, Havik OE. Psychological predictors for return to work after a myocardial infarction. J Psychosom Res. 1987;31:471–481. doi: 10.1016/0022-3999(87)90005-5. [DOI] [PubMed] [Google Scholar]
- 31.Petrie KJ, Weinman J, Sharpe N, Buckley J. Role of patients' view of their illness in predicting return to work and functioning after myocardial infarction: Longitudinal study. BMJ. 1996;312:1191–1194. doi: 10.1136/bmj.312.7040.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Soejima Y, Steptoe A, Nozoe S, Tei C. Psychosocial and clinical factors predicting resumption of work following acute myocardial infarction in japanese men. Int J Cardiol. 1999;72:39–47. doi: 10.1016/s0167-5273(99)00157-6. [DOI] [PubMed] [Google Scholar]
- 33.Waszkowska M, Szymczak W. Return to work after myocardial infarction: A retrospective study. Int J Occup Med Environ Health. 2009;22:373–381. doi: 10.2478/v10001-009-0033-4. [DOI] [PubMed] [Google Scholar]
- 34.Dreyer RP, Wang Y, Strait KM, Lorenze NP, D'Onofrio G, Bueno H, Lichtman JH, Spertus JA, Krumholz HM. Gender differences in the trajectory of recovery in health status among young patients with acute myocardial infarction: Results from the variation in recovery: Role of gender on outcomes of young ami patients (virgo) study. Circulation. 2015;131:1971–1980. doi: 10.1161/CIRCULATIONAHA.114.014503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Smolderen KG, Strait KM, Dreyer RP, D'Onofrio G, Zhou S, Lichtman JH, Geda M, Bueno H, Beltrame J, Safdar B, Krumholz HM, Spertus JA. Depressive symptoms in younger women and men with acute myocardial infarction: Insights from the virgo study. J Am Heart Assoc. 2015;4:e0001424. doi: 10.1161/JAHA.114.001424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Xu X, Bao H, Strait K, Spertus JA, Lichtman JH, D'Onofrio G, Spatz E, Bucholz EM, Geda M, Lorenze NP, Bueno H, Beltrame JF, Krumholz HM. Sex differences in perceived stress and early recovery in young and middle-aged patients with acute myocardial infarction. Circulation. 2015;131:614–23. doi: 10.1161/CIRCULATIONAHA.114.012826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Herlitz J, Karlson BW, Sjolin M, Ekvall HE, Hjalmarson A. Prognosis during one year of follow-up after acute myocardial infarction with emphasis on morbidity. Clin Cardiol. 1994;17:15–20. doi: 10.1002/clc.4960170104. [DOI] [PubMed] [Google Scholar]
- 38.Boudrez H, De Backer G, Comhaire B. Return to work after myocardial infarction: Results of a longitudinal population based study. Eur Heart J. 1994;15:32–36. doi: 10.1093/oxfordjournals.eurheartj.a060376. [DOI] [PubMed] [Google Scholar]
- 39.Kaul P, Newby LK, Fu Y, Mark DB, Califf RM, Topol EJ, Aylward P, Granger CB, Van de Werf F, Armstrong PW. International differences in evolution of early discharge after acute myocardial infarction. Lancet. 2004;363:511–517. doi: 10.1016/S0140-6736(04)15536-0. [DOI] [PubMed] [Google Scholar]
- 40.Kristofferzon ML, Lofmark R, Carlsson M. Myocardial infarction: Gender differences in coping and social support. J Adv Nurs. 2003;44:360–374. doi: 10.1046/j.0309-2402.2003.02815.x. [DOI] [PubMed] [Google Scholar]
- 41.King KB. Emotional and functional outcomes in women with coronary heart disease. J Cardiovasc Nurs. 2001;15:54–70. doi: 10.1097/00005082-200104000-00005. [DOI] [PubMed] [Google Scholar]
- 42.Hodgson TA, Cohen AJ. Medical care expenditures for selected circulatory diseases: Opportunities for reducing national health expenditures. Med Care. 1999;37:994–1012. doi: 10.1097/00005650-199910000-00004. [DOI] [PubMed] [Google Scholar]
- 43.Brink E, Brandstrom Y, Cliffordsson C, Herlitz J, Karlson BW. Illness consequences after myocardial infarction: Problems with physical functioning and return to work. J Adv Nurs. 2008;64:587–594. doi: 10.1111/j.1365-2648.2008.04820.x. [DOI] [PubMed] [Google Scholar]
- 44.Isaaz K, Coudrot M, Sabry MH, Cerisier A, Lamaud M, Robin C, Richard L, Da Costa A, Khamis H, Abd-Alaziz A, Gerenton C. Return to work after acute st-segment elevation myocardial infarction in the modern era of reperfusion by direct percutaneous coronary intervention. Arch Cardiovasc Dis. 2010;103:310–316. doi: 10.1016/j.acvd.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 45.Drory Y, Kravetz S, Koren-Morag N, Goldbourt U Israel Study Group on First Acute Myocardial I. Resumption and maintenance of employment after a first acute myocardial infarction: Sociodemographic, vocational and medical predictors. Cardiology. 2005;103:37–43. doi: 10.1159/000081850. [DOI] [PubMed] [Google Scholar]
- 46.Mark DB, Lam LC, Lee KL, Clapp-Channing NE, Williams RB, Pryor DB, Califf RM, Hlatky MA. Identification of patients with coronary disease at high risk for loss of employment. A prospective validation study. Circulation. 1992;86:1485–1494. doi: 10.1161/01.cir.86.5.1485. [DOI] [PubMed] [Google Scholar]
- 47.Egiziano G, Akhtari S, Pilote L, Daskalopoulou SS. Sex differences in young patients with acute myocardial infarction. Diabet Med. 2013;30:e108–14. doi: 10.1111/dme.12084. [DOI] [PubMed] [Google Scholar]
- 48.Coutinho T, Goel K, Correa de Sa D, Kragelund C, Kanaya AM, Zeller M, Park JS, Kober L, Torp-Pedersen C, Cottin Y, Lorgis L, Lee SH, Kim YJ, Thomas R, Roger VL, Somers VK, Lopez-Jimenez F. Central obesity and survival in subjects with coronary artery disease: A systematic review of the literature and collaborative analysis with individual subject data. J Am Coll Cardiol. 2011;57:1877–1886. doi: 10.1016/j.jacc.2010.11.058. [DOI] [PubMed] [Google Scholar]
- 49.Fiabane EOO, Argentero P, Massimo Candura S, Giorgi I. Return to work after an acute cardiac event: The role of psychosocial factors. Prevention and research. 2014;3:137–141. [Google Scholar]
- 50.Pilote L, Karp I. Genesis-praxy (gender and sex determinants of cardiovascular disease: From bench to beyond-premature acute coronary syndrome) Am Heart J. 2012;163:741–746. e742. doi: 10.1016/j.ahj.2012.01.022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.