Abstract
Objective
An International Classification of Diseases code-based case definition for non-fatal abusive head trauma (AHT) in children <5 years of age was developed in March 2008 by an expert panel convened at the Centers for Disease Control and Prevention (CDC). This study presents an application of the CDC recommended operational case definition of AHT to US hospital inpatient data to characterise the AHT hospitalisation rate for children <5 years of age.
Methods
Nationwide Inpatient Sample (NIS) data from the Healthcare Cost and Utilisation Project from 2003 to 2008 were examined.
Results
Inspection of the NIS data resulted in the identification of an estimated 10 555 non-fatal AHT hospitalisations with 9595 classified as definite/presumptive AHT and 960 classified as probable AHT. The non-fatal AHT rate was highest among children aged <1 year (32.3 per 100 000) with a peak in hospitalisations between 1 and 3 months of age. Non-fatal AHT hospitalisation rates for children <2 years of age were higher for boys (21.9 per 100 000) than girls (15.3 per 100 000). The non-fatal AHT hospitalisation rate showed little variation across seasons.
Conclusions
To reduce the burden of AHT in the USA, a preventable public health problem, concerted prevention efforts targeting populations at risk should be implemented. This report demonstrates a model procedure for using the new CDC definition for public health surveillance and research purposes. Such findings can be used to inform parents and providers about AHT (eg, dangers of shaking, strategies for managing infant crying) as well as to monitor better the impact of prevention strategies over time.
INTRODUCTION
Abusive head trauma (AHT) is a serious injury resulting from assaults (ie, violent shaking and/or blunt impact) on infants or young children leading to injuries to the head or brain. This condition is known by many names depending upon the discipline and setting, including shaken baby or shaken infant syndrome, shaken impact syndrome, infant whiplash-shake injury syndrome, inflicted traumatic brain injury and inflicted, non-accidental or intentional head injury. Depending upon the term used and how it is operationalised, the corresponding measures of incidence, prevalence and clinical picture can be quite different. For example, when surveillance of shaken baby syndrome is conducted using the common triad of clinical symptoms (subdural haematoma, retinal haemorrhage and cerebral oedema), cases of head trauma that may result from other mechanisms can be excluded. Thus, in April 2009 the American Academy of Pediatrics (AAP) officially recommended using ‘abusive head trauma’ to describe any assault-related injury inflicted to the head and its contents among children.1
The range and severity of the health consequences for victims compound the public health significance of AHT. This condition is one of the leading causes of child maltreatment-related fatalities.2,3 It is estimated that between 50% and 80% of head trauma-related deaths in infants and children <2 years old in the USA result from abuse.4,5 Previous estimates of the population-based rate for serious inflicted head injury in children <2 years of age fall between 14 and 19 hospitalisations per 100 000 person years.5–8 While injuries consistent with AHT have been found in children as old as 5 years of age, the majority of victims are <2 years of age and peak incidence is typically found at 3 months.4,9,10
Although most victims do survive, the mortality rate in clinical studies has ranged from 13% to 35%.11–14 The majority of AHT survivors suffer from significant physical disabilities and neurological impairment, while only 10–15% have little to no impairment or disability.15–18 Common adverse outcomes include numerous cognitive and neurological sequelae including motor and visual deficits, epilepsy and speech, language and behavioural problems.16,19,20
Despite the numerous studies that have been published on the epidemiology, clinical manifestations and sequelae of AHT, routine surveillance (eg, measuring incidence, examining temporal trends and demographic patterns) has been limited by the lack of a standard case definition. To address this limitation, the Centers for Disease Control and Prevention (CDC) convened a panel of pediatricians, child maltreatment experts, abusive head trauma experts, International Classification of Diseases (ICD) coding experts and experienced state health department personnel in March 2008 to develop ICD code-based case definitions for both non-fatal AHT (applicable primarily to ICD 9th Revision, Clinical Modification (ICD-9-CM) coded administrative/billing medical records) and fatal AHT (applicable primarily to death certificate data) in children <5 years of age. The panel developed broad and narrow operational case definitions, with the former emphasising greater sensitivity of case ascertainment and recommended for general population-based surveillance and the latter emphasising specificity and recommended for more focused assessments (eg, individual-level case study).21 We recently published the operational case definition for fatal AHT applied to national vital statistics data22 which characterised the incidence of fatal AHT in children under <5 years old. This analysis applies the panel’s broad operational case definition for non-fatal AHT to the Nationwide Inpatient Sample (NIS) database from the Healthcare Cost and Utilisation Project (HCUP) to characterise the incidence of non-fatal AHT in children <5 years old and to characterise the epidemiological and clinical characteristics of the subpopulations at highest risk.
METHODS
This study was based on a retrospective analysis of 6 years (2003–8) of hospitalisation data using the HCUP-NIS database which is compiled and maintained by the United States Agency for Healthcare Research and Quality (AHRQ).23 The NIS is a stratified probability sample of hospitals from the states that submit data to HCUP, and is weighted to support national estimates. It is the largest inpatient care database that is publicly available in the USA, containing data on 5–8 million hospital stays per year from about 1000 hospitals sampled to approximate a 20% stratified sample of US community hospitals. NIS data represent hospital discharges and not individual persons, so patients with multiple hospitalisations can be counted a number of times.
For non-fatal AHT, the CDC panel’s broad operational case definition is based on ICD-9-CM clinical diagnosis and cause-of-injury codes.24 The recommended set of ICD-9-CM codes for the broad case definition and the division of hospitalisations into two categories of non-fatal AHTare shown in table 1. Column 2 is a list of ICD-9-CM codes that must be present in one of the 15 clinical diagnosis fields listed in each hospitalisation billing record in NIS (see Appendix 1 in online supplement for a description of clinical diagnosis codes). Column 3 includes External cause-of-injury codes (E-codes) and abuse codes. For each hospital billing record there must be either one of the listed E-codes in one of the four external cause-of-injury fields or one of the listed abuse codes in one of the 15 diagnosis fields (see Appendix 2 in online supplement for a description of E-codes).
Table 1.
CDC’s recommended operational case definition based on ICD-9-CM† diagnoses and external cause-of-injury codes for defining non-fatal abusive head trauma in children aged <5 years
| Clinical diagnosis code | External cause-of-injury or abuse code | |
|---|---|---|
| Definite or presumptive abusive head trauma | 781.0–781.4, 781.8, 800, 801, 803, 804.1–804.4, 804.6–804.9, 850, 851, 852.0–852.5, 853.0, 853.1, 854.0, 854.1, 925.1, 950.0–950.3, 959.01, 995.55‡ | E960.0, E967, E968.1, E968.2, E968.8, E968.9, 995.50*, 995.54, 995.59* |
| Probable abusive head trauma | All of those above (except 995.55) | E987, E988.8, E988.9 |
| Non-abusive head trauma | 781.0–781.4, 781.8, 800, 801, 803, 804, 850, 851, 852, 853, 854.0, 854.1, 925.1, 950.0–950.3, 959.01 | Excluding all those above |
Excludes cases in the presence of a fall or unintentional injury code: E800eE807, E810-E838, E840eE848, E880eE888 and E890eE928.
International Classification of Diseases, Ninth Revision, Clinical Modification.
Does not require an external cause or abusive code.
Patients aged 0–4 years with head trauma were classified into one of three categories listed in table 1: definite or presumptive AHT, probable AHT and non-AHT. Each patient was assigned to a single category in the classification scheme if they had at least one of the ICD-9-CM clinical diagnosis codes (column 2) and one of the external cause-of-injury or abuse codes (column 3) listed for that category. Patients with ICD-9-CM clinical diagnoses code 995.55 (shaken infant syndrome) were directly defined as definite or presumptive AHT without an accompanying E-code or abuse clinical diagnosis code.
Several exclusions were applied to the data. Unless accompanied by the ICD-9-CM code 995.55 or other abuse clinical diagnosis codes, hospitalisations with missing E-codes were excluded. E-codes were missing for 9.9% of children aged <5 years and 9.8% of children aged <2 years. Patients with abuse clinical diagnosis codes 995.50 and 995.59 were also excluded if they occurred with an unintentional fall-related injury or other unintentional injury code including ICD-9-CM E-codes E800–E807, E810–E838, E840–E848, E880–E888 and E890–E928 (see Appendix 3 in online supplement for a description of excluded E-codes). Other excluded conditions and injury mechanisms which can be mistaken for AHT (but were not accompanied by indications of abuse) were birth trauma (967), congenital anomalies (740.0–759.9), coagulation defects (286), motor vehicle incidents (E810–E819) and unintentional gun-related injuries (E922). Patients who died while in hospital were also excluded from the study. An application of the CDC operational definition for fatal AHT to US vital statistics data has been previously published.22
Population-based hospitalisation rates for patients with nonfatal AHT were determined by year, age and sex. Rates, ORs, p values and 95% CIs were calculated using SAS PROC SURVEYFREQ to account for the sample weights and complex sample design and to calculate the variances of the estimates. The ORs estimate the odds of a case of a given variable category (eg, male, summer) being classified as AHT as opposed to non-AHT, relative to the reference category. All statistical analyses were performed using SAS Systems for Windows V.9.2.
RESULTS
Using the CDC recommended definition for AHT, there were an estimated 74 233 head trauma-related hospitalisations among children aged <5 years in the USA during 2003–8. Of these, 10 555 hospitalisations met the broad CDC operational case definition for AHT (average of 1759 per year; table 2). Owing to missing E-codes, 8130 potential AHT hospitalisations were unexplained. Among the AHT hospitalisations, 9595 (90.9%) were definite or presumptive AHT and 960 (9.1%) were probable AHT. Among all AHT hospitalisations (both definitive/presumptive and probable), 76.6% (n=1348) occurred among children <1 year of age compared with 39.3% (n=4167 per year) of non-AHT hospitalisations (table 2). Among children aged <1 year, the majority of hospitalisations (66.3%) were at 1–5 months of age with a peak rate of AHT at 2 months of age (182 hospitalisations per year). In contrast, non-AHT among children aged <1 year peaked at 0 months of age (416 hospitalisations per year), predominantly due to falls (81.2%), and progressively declined with age (figure 1).
Table 2.
Estimated annual numbers and rates of non-fatal abusive head trauma (AHT) and non-AHT hospitalisations by age per 100 000 population based on the CDC expert panel’s operational AHT definition, USA, 2003–8
| <1 year
|
1 year
|
2 years
|
3 years
|
4 years
|
Total
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | |
| Definite/presumptive AHT | 1224 | 29.3 | 24.3 to 34.3 | 186 | 4.5 | 3.4 to 5.6 | 121 | 2.9 | 2.1 to 3.7 | 39 | 1.0 | 0.7 to 1.3 | 30 | 0.7 | 0.4 to 1.0 | 1599 | 7.8 | 6.5 to 9.1 |
| Probable AHT | 125 | 3.0 | 2.2 to 3.8 | 18 | 0.4 | 0.2 to 0.6 | 13 | 0.3 | 0.1 to 0.5 | 2 | 0.0 | 0.0 to 0.1 | 3 | 0.1 | 0.0 to 0.2 | 160 | 0.8 | 0.6 to 1.0 |
| Total AHT | 1348 | 32.3 | 27.0 to 37.6 | 204 | 4.9 | 3.7 to 6.1 | 134 | 3.3 | 2.5 to 4.1 | 40 | 1.0 | 0.6 to 1.4 | 33 | 0.8 | 0.5 to 1.1 | 1759 | 8.6 | 7.2 to 10.0 |
| Total non-AHT | 4167 | 99.9 | 86.4 to 113.4 | 1634 | 39.5 | 33.9 to 45.1 | 2428 | 59 | 49.4 to 68.6 | 1301 | 31.8 | 27.3 to 36.3 | 1084 | 26.8 | 22.8 to 30.8 | 10613 | 51.6 | 45.1 to 58.1 |
Figure 1.
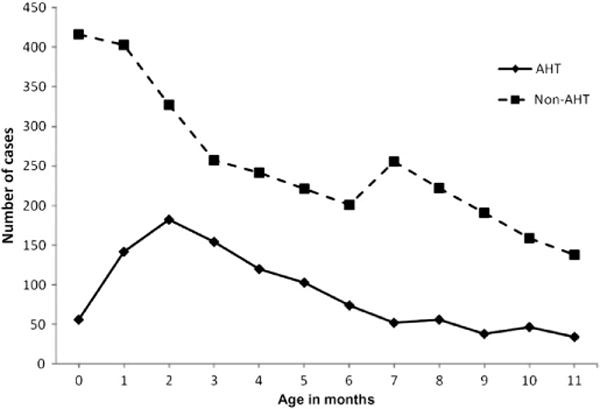
Estimated annual number of cases of non-fatal abusive head trauma (AHT) and non-AHT hospitalisations by month of age, USA, 2003–8.
Because both our study and previous research show that most hospitalisations for non-fatal AHT occur in children <2 years of age (table 2 and figure 2), additional analyses were restricted to that population. Among children <2 years of age, the hospitalisation rate for both AHTand non-AHT peaked in 2005 (22.0 per 100 000 (95% CI 14.2 to 29.8) and 85.9 per 100 000 (95% CI 59.3 to 112.5), respectively; figure 3). Following that peak the annual rate of head trauma among children <2 years of age declined slightly, although the decline appeared to have been more rapid for the non-AHT population (85.9–61.2 per 100 000 (95% CI 44.1 to 78.3)) than for the AHT population (22.0–17.1 per 100 000 (95% CI 11.1 to 23.1)).
Figure 2.
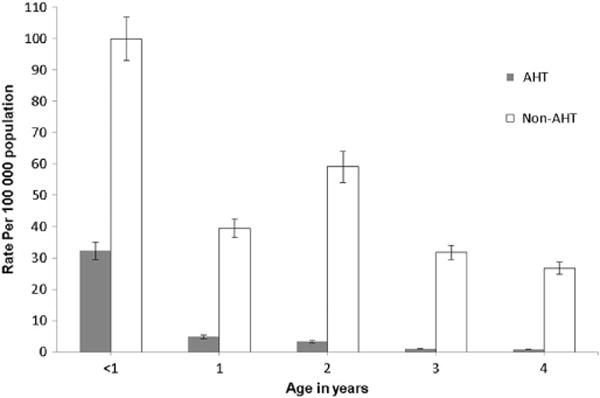
Estimated annual rates of non-fatal abusive head trauma (AHT) and non-AHT hospitalisations by age based on the CDC expert panel’s operational AHT definition, USA, 2003–8. Error bars represent ±SD for each rate.
Figure 3.
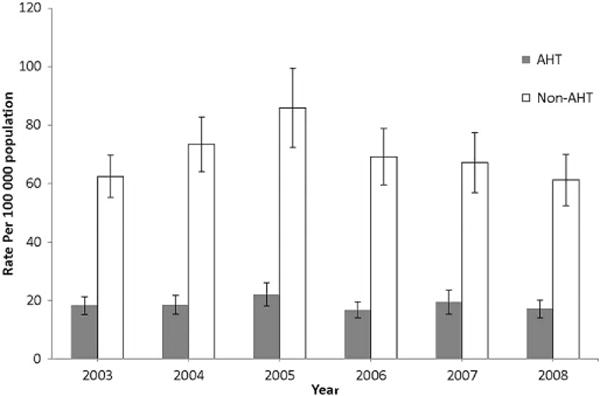
Estimated rates of non-fatal abusive head trauma (AHT) and non-AHT hospitalisations by year for children aged <2 years, USA, 2003–8. Error bars represent ±SD for each rate.
Overall, for children <2 years of age, slightly more hospitalisations for AHT (60.0%) and non-AHT (57.6%) were in boys (table 3). Because of the large amount of missing data, we were unable to calculate rates by race/ethnicity. Among children <2 years of age, hospitalisations occurred in all calendar months without any clear seasonality for AHT or non-AHT (table 3). Compared with non-AHT hospitalisations, the odds of AHT during summer and autumn (fall) were 0.8 times the odds of AHT during winter months (p<0.005).
Table 3.
Estimated annual numbers and rates of non-fatal abusive head trauma (AHT) and non-AHT hospitalisations by selected demographic and admission characteristics for children aged <2 years, USA, 2003–8
| Definite/presumptive AHT
|
Probable AHT
|
Total AHT
|
Non-AHT
|
OR (95% CI) | p Value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | No. | Rate | 95% CI | |||
| Total | 1409 | 17.0 | 14.2 to 19.8 | 143 | 1.7 | 1.2 to 2.2 | 1552 | 18.7 | 15.6 to 21.8 | 5801 | 69.8 | 60.8 to 78.8 | ||
| Sex | ||||||||||||||
| Female | 569 | 14.0 | 11.4 to 16.6 | 51 | 1.3 | 0.9 to 1.7 | 620 | 15.3 | 12.5 to 18.1 | 2434 | 59.9 | 52.0 to 67.8 | 1.0 (reference) | |
| Male | 839 | 19.7 | 16.4 to 23.0 | 92 | 2.2 | 1.5 to 2.9 | 931 | 21.9 | 18.3 to 25.5 | 3343 | 78.6 | 68.3 to 88.9 | 1.092 (0.981 to 1.216) | 0.1084 |
| Unknown | 1 | 0 | 1 | 25 | ||||||||||
| Race* † | ||||||||||||||
| White | 478 | 45 | 523 | 2182 | ||||||||||
| Black | 199 | 28 | 227 | 672 | ||||||||||
| Native American | 5 | 1 | 6 | 32 | ||||||||||
| Asian/PI | 14 | 1 | 15 | 145 | ||||||||||
| Hispanic | 194 | 32 | 225 | 999 | ||||||||||
| Other/unknown | 518 | 37 | 555 | 1772 | ||||||||||
| Month of admission | ||||||||||||||
| Winter (December–February) | 327 | 3.9 | 3.2 to 4.6 | 30 | 0.4 | 0.3 to 0.5 | 357 | 4.3 | 3.6 to 5.0 | 1115 | 13.4 | 11.5 to 15.3 | 1.0 (reference) | |
| Spring (March–May) | 349 | 4.2 | 3.3 to 5.1 | 31 | 0.4 | 0.3 to 0.5 | 380 | 4.6 | 3.7 to 5.5 | 1327 | 16.0 | 13.7 to 18.3 | 0.896 (0.771 to 1.040) | 0.1486 |
| Summer (June–August) | 328 | 3.9 | 3.1 to 4.7 | 36 | 0.4 | 0.2 to 0.6 | 364 | 4.4 | 3.5 to 5.3 | 1475 | 17.7 | 15.0 to 20.4 | 0.771 (0.660 to 0.900) | 0.0011 |
| Fall (September–November) | 314 | 3.8 | 3.1 to 4.5 | 33 | 0.4 | 0.2 to 0.6 | 347 | 4.2 | 3.4 to 5.0 | 1320 | 15.9 | 13.6 to 18.2 | 0.821 (0.718 to 0.940) | 0.0047 |
| Unknown | 92 | 1.1 | 0.5 to 1.7 | 13 | 0.2 | 0.1 to 0.3 | 104 | 1.3 | 0.6 to 2.0 | 565 | 6.8 | 3.3 to 10.3 | ||
White, white; non-Hispanic, black; Black, non-Hispanic; AI/AN, American Indian/Alaska Native; A/PI, Asian/Pacific Islander.
Due to the large percentage of missing data the rates for race/ethnicity could not be calculated.
In post hoc analyses we found that, among the 9311 AHT hospitalisations of children <2 years of age over the study period, the most frequent injuries were subdural haemorrhage following injury without mention of an open intracranial wound (42.5%), retinal haemorrhage (41.2%), fractures of the vault of the skull (27.2%) and closed fractures of the vault of the skull with subarachnoid, subdural and extradural haemorrhage (14.0%). Abuse-related codes (995.54 ‘Child Physical Abuse’ and 995.55 ‘Shaken Infant Syndrome’) were reported in 36.1% and 35.6% of hospitalisations, respectively. Among the 34 807 non-AHT hospitalisations in children aged <2 years, 8.0% reported having a subdural haematoma and 1.9% a retinal haemorrhage. In the non-AHT group the most frequent injuries were fractures of the vault of the skull (40.7%) or fractures of the base of the skull (14.6%). Most injuries in these two categories were closed head injury without mention of intracranial injury (800.0, 801.0).
DISCUSSION
This is the first study to apply the CDC’s ICD-based operational case definition for AHT morbidity to a national dataset. The application of this consensus AHT definition to data from NIS, a large nationally representative sample, demonstrates a model procedure for using the definition to track and study AHT, a relatively rare condition with serious and lifelong consequences.
The CDC recommended that standard non-fatal AHT case definition can help identify population subgroups at higher risk for AHT requiring hospitalisation by age, sex, race/ethnicity and seasonality. Our findings indicate that rates of AHT hospitalisations were highest in children aged 1–5 months and boys.
We observed a slight but statistically non-significant peak in 2005 and fluctuating rates from 2006 to 2008. Despite several post hoc analyses exploring the peak hospitalisation rate for both AHT and non-AHT in 2005, we were unable to identify any factors that could have precipitated a rise and fall in incidence in that period. Overlap in the CIs around the annual rates (not shown) suggests the fluctuation may have been due to chance. The overall non-fatal AHT-related hospitalisation rate among children aged <2 years (18.7 per 100 000) was higher than previous studies in which the incidence among this population ranged from 14.0 to 17.0 per 100 000.5,25 Both previous studies were conducted using state population data and slightly different case inclusion/exclusion criteria (eg, case definitions contained a less inclusive list of ICD-9-CM clinical diagnoses and E-codes than the CDC AHT definition). Similar to that found in the current study, the peak hospitalisation rate for AHT in previous studies has occurred at 1–4 months.6,26
Consistent with several other studies, we found that both AHT (60.0%) and non-AHT (57.6%) were more common among boys, with a frequency of 58.4% in a study of AHT using Pennsylvania child abuse registry data,8 57.2% in a North Carolina review of hospital medical records,27 58% in a study of California hospital inpatient data and 67.2% in an analyses of North Carolina traumatic brain injury registry data.28
Our analyses did not reveal a notable peak in AHT during any season. Findings regarding seasonality of AHT have been mixed. One study found that children aged <2 years were less likely to suffer AHT during April and more likely to be injured during August and October.29 Others have shown a peak hospitalisation rate for AHT during the Thanksgiving/Christmas holiday months (October–December), especially among children aged <3 years8 or during the summer months among children aged 0–4 years.30 Two of these studies used state trauma registry data8,29 and the third30 used data collected prospectively in paediatric intensive care units in the UK. We found a slightly higher hospitalisation rate for non-AHT among children aged <2 years during the summer months. In post hoc analyses we found that the hospitalisation rate for autumn (fall) and motor vehicle-related injuries peak during the summer months were possibly due to higher rates of outdoor recreation and vacation-related travel.
Because ICD-9-CM clinical diagnosis and E-codes are used primarily for administrative/billing purposes, the validity and reliability of the CDC operational AHT morbidity case definition needed to be studied. This study demonstrated a suggested procedure for using the CDC operational case definition for surveillance purposes. Future studies which assess and demonstrate the validity and reliability of the definition will help to advance the case for its utilisation.
This study was subject to several limitations. First, because NIS data represent hospital discharges and not individual persons, patients with multiple hospitalisations could be counted a number of times. Second, the NIS underestimates the total number of AHT discharges because it does not include AHTs that are treated in federal hospitals and outpatient settings or those that do not present for medical care. Third, for those children aged <1 year, age in days is set to missing in records for a number of hospitalisations (22.4%) so the number of AHT hospitalisations by month of age for children aged <1 year could also be underestimated.
A fourth potential limitation is that some AHT hospitalisations may not be identifiable due to lack of sufficient information to confirm child maltreatment. Furthermore, given the similarity in the epidemiology of AHT and assault-related non-AHT (traumatic head injuries that did not have a qualifying AHT clinical diagnosis code but had an assault-related external cause of injury or abuse code), it is possible that some hospitalisations in the latter category are misclassified due to incorrect coding of information in the medical record. Due to missing E-codes, 8130 potential AHT hospitalisations were unexplained. This potential under-reporting of maltreatment codes has been demonstrated in several previous studies.31,32
If the upcoming transition for ICD-9-CM to ICD-10-CM excludes the ‘shaken infant syndrome’ clinical diagnosis code, additional hospitalisations may be lost in future analyses. In ICD-10-CM the code T74.4 (shaken infant syndrome) will not be a billable ICD-10-CM clinical diagnosis code and will not be used to indicate a medical diagnosis. Instead, three sub-codes below T74.4 will be used to describe this diagnosis in greater detail. In the current study ‘shaken infant syndrome’ (995.55) was listed in 601 of 1599 (37.6%) definitive AHT records among children <5 years of age, an average annual hospitalisation rate of 2.9 per 100 000 population. Of the 601 records where shaken infant syndrome was listed, 229 (38.1%) would be reclassified as probable AHT (n=4), non-AHT (n=70) or completely lost (n=155) as head trauma hospitalisations without 995.55. In summary, 225 of 1759 hospitalisations (12.8%) could be lost as AHT hospitalisations without clinicians being able to use 995.55 for abusive head trauma. It will be important to address the new structure of the shaken infant codes in training and planning activities until and after they go into effect on 1 October 2013.
The degree of variation in rates of AHT hospitalisations across previous studies depending upon the age of the study population, case definitions and data source point to the need for some level of standardisation. This study presents results that, with continued application of the new CDC definition for non-fatal AHT, will help strengthen the degree of confidence in our understanding of the epidemiology of AHT. Examination of cases along the spectrum of severity is needed to obtain the most complete picture of groups at highest risk for morbidity and mortality from AHT. Thus, as a companion to the application of the standard AHT morbidity definition presented here, similar descriptive analyses of AHT fatalities identified using the new CDC definition for fatal AHT were conducted and recently published.22
As demonstrated in these analyses and in previous studies, peak AHT hospitalisation rates occur during the first 3–4 months of life. The previous analyses of AHT fatalities also indicated a peak in rates in the first 2 months of life.22 This is also the period during which infants are most physically vulnerable to inflicted injuries. Prolonged, inconsolable and unpredictable episodes of infant crying are known to coincide with peak hospitalisation rate for AHT.33,34 Thus, prevention efforts currently aim to address educating parents about the dangers of shaking, strategies for managing infant crying and the benefits of sharing of preventive information with peers. Prominent examples of these types of educational programs include the Period of PURPLE Crying and the Upstate New York Shaken Baby Syndrome Education Program.35,36 Both programs are currently being evaluated in North Carolina and Pennsylvania, respectively, with funding support from CDC. Guidance on preventing AHT has been fully described elsewhere.37 It is important to note that most (if not all) AHT prevention efforts are implemented at the regional or state level. The new operational case definition can be a useful tool for standardising the process of targeting and possibly evaluating such efforts.
This study also demonstrates significant differences in the epidemiology of non-fatal AHT-related hospitalisation versus non-AHT-related hospitalisation that could help to inform paediatricians, public health practitioners and child protective services better and promote better and comparable research.
This report shows the utility of CDC’S standard AHT definition for public health surveillance activities. Furthermore, the large number of unknown external causes underscores the need for better accuracy and specificity and more complete E-coding and reliable use of child maltreatment codes by healthcare providers and data coders. Together, these elements stand to greatly improve research, surveillance and ultimately prevention of AHT among young children.
Supplementary Material
What is already known on the subject.
-
►
AHT is the leading cause of physical child maltreatment fatalities. Good outcomes with little to no impairment or disability are only seen in 10–15% of survivors.
-
►
Surveillance (eg, measuring incidence, examining temporal trends and demographic patterns) of abusive head trauma has been limited by the lack of standard case definitions.
What this study adds.
-
►
The code-based case definitions for non-fatal AHT in children <5 years of age which were developed by a Centers for Disease Control and Prevention-convened expert panel has been successfully operationalised and applied to US death data.
-
►
The proposed definition for non-fatal AHT can be a useful tool for standardising future public health surveillance activities related to head trauma in young children.
Acknowledgments
The authors would like to thank Dr Joseph L Annest and Dr Scott Kegler who provided thorough reviews and constructive suggestions during the development of this manuscript.
Funding This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Additional appendices 1–3 are published online only. To view these files please visit the journal online (http://dx.doi.org/10.1136/injuryprev-2011-040234).
Contributors All authors participated in the development of this manuscript and all agree to take public responsibility for the appropriate portions of the content.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The data used in this study are publicly available from the United States Agency for Healthcare Research and Quality.
References
- 1.Christian CW, Block R. Abusive head trauma in infants and children. Pediatrics. 2009;123:1409–11. doi: 10.1542/peds.2009-0408. [DOI] [PubMed] [Google Scholar]
- 2.Administration for Children and Families. Child Abuse and Neglect Fatalities 2009: Statistics and Interventions. http://www.childwelfare.gov/pubs/factsheets/fatality.cfm (accessed 28 Apr 2011)
- 3.National MCH Center for Child Death Review. Child Abuse and Neglect: Fact Sheet. http://www.childdeathreview.org/causesCAN.htm (accessed 28 Apr 2011)
- 4.Bruce DA, Zimmerman RA. Shaken impact syndrome. Pediatr Ann. 1989;18:482–4. 486–9, 492–4. doi: 10.3928/0090-4481-19890801-07. [DOI] [PubMed] [Google Scholar]
- 5.Keenan HT, Runyan DK, Marshall SW, et al. A population-based study of inflicted traumatic brain injury in young children. JAMA. 2003;290:621–6. doi: 10.1001/jama.290.5.621. [DOI] [PubMed] [Google Scholar]
- 6.Barlow KM, Minns RA. Annual incidence of shaken impact syndrome in young children. Lancet. 2000;356:1571–2. doi: 10.1016/S0140-6736(00)03130-5. [DOI] [PubMed] [Google Scholar]
- 7.Dias MS, Smith K, DeGuehery K, et al. Preventing abusive head trauma among infants and young children: a hospital-based, parent education program. Pediatrics. 2005;115:e470–7. doi: 10.1542/peds.2004-1896. [DOI] [PubMed] [Google Scholar]
- 8.Kesler H, Dias MS, Shaffer M, et al. Demographics of abusive head trauma in the commonwealth of Pennsylvania. J Neurosurg Pediatr. 2008;1:351–6. doi: 10.3171/PED/2008/1/5/351. [DOI] [PubMed] [Google Scholar]
- 9.Pounder DJ. Shaken adult syndrome. Am J Forensic Med Pathol. 1997;18:321–4. doi: 10.1097/00000433-199712000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ludwig S, Warman M. Shaken baby syndrome: a review of 20 cases. Ann Emerg Med. 1984;13:104–7. doi: 10.1016/s0196-0644(84)80571-5. [DOI] [PubMed] [Google Scholar]
- 11.Dias MS, Backstrom J, Falk M, et al. Serial radiography in the infant shaken impact syndrome. Pediatr Neurosurg. 1998;29:77–85. doi: 10.1159/000028694. [DOI] [PubMed] [Google Scholar]
- 12.Hadley MN, Sonntag VK, Rekate HL, et al. The infant whiplash-shake injury syndrome: a clinical and pathological study. Neurosurgery. 1989;24:536–40. doi: 10.1227/00006123-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Sinal SH, Ball MR. Head trauma due to child abuse: serial computerized tomography in diagnosis and management. South Med J. 1987;80:1505–12. doi: 10.1097/00007611-198712000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Zimmerman RA, Bilaniuk LT, Gennarelli T, et al. Cranial computed tomography in diagnosis and management of acute head trauma. AJR Am J Roentgenol. 1978;131:27–34. doi: 10.2214/ajr.131.1.27. [DOI] [PubMed] [Google Scholar]
- 15.Ewing-Cobbs L, Kramer L, Prasad M, et al. Neuroimaging, physical, and developmental findings after inflicted and noninflicted traumatic brain injury in young children. Pediatrics. 1998;102:300–7. doi: 10.1542/peds.102.2.300. [DOI] [PubMed] [Google Scholar]
- 16.Goldstein B, Kelly MM, Bruton D, et al. Inflicted versus accidental head injury in critically injured children. Crit Care Med. 1993;21:1328–32. doi: 10.1097/00003246-199309000-00016. [DOI] [PubMed] [Google Scholar]
- 17.Kivlin JD, Simons KB, Lazoritz S, et al. Shaken baby syndrome. Ophthalmology. 2000;107:1246–54. doi: 10.1016/s0161-6420(00)00161-5. [DOI] [PubMed] [Google Scholar]
- 18.Starling SP, Holden JR, Jenny C. Abusive head trauma: the relationship of perpetrators to their victims. Pediatrics. 1995;95:259–62. [PubMed] [Google Scholar]
- 19.Barlow KM, Thomson E, Johnson D, et al. Late neurologic and cognitive sequelae of inflicted traumatic brain injury in infancy. Pediatrics. 2005;116:e174–85. doi: 10.1542/peds.2004-2739. [DOI] [PubMed] [Google Scholar]
- 20.Duhaime AC, Christian C, Moss E, et al. Long-term outcome in infants with the shaking-impact syndrome. Pediatr Neurosurg. 1996;24:292–8. doi: 10.1159/000121058. [DOI] [PubMed] [Google Scholar]
- 21.Parks SE, Annest JL, Hill HA, et al. Pediatric Abusive Head Trauma: Recommended Definitions for Public Health Surveillance and Research. Atlanta (GA): Centers for Disease Control and Prevention; 2012. [Google Scholar]
- 22.Parks SE, Kegler SR, Annest JL, et al. Characteristics of fatal abusive head trauma among children in the USA: 2003–2007 an application of the CDC operational case definition to national vital statistics data. Inj Prev. 2011 Oct 20; doi: 10.1136/injuryprev-2011-040128. Published Online First: [DOI] [PubMed] [Google Scholar]
- 23.Agency for Healthcare Research and Quality. HCUP NIS Database Documentation. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 24.Anon. Clinical modification Hospital edition 9th Revision. Los Angeles, GA: Practice Management Information Corporation (PMIC); 2005. International Classification of Diseases. [Google Scholar]
- 25.Wirtz SJ, Trent RB. Passive surveillance of shaken baby syndrome using hospital inpatient data. Am J Prev Med. 2008;34(4 Suppl):S134–9. doi: 10.1016/j.amepre.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 26.Barr R, Trent RB, Cross J. Age-related incidence curve of hospitalized shaken baby syndrome cases: convergent evidence for crying as a trigger to shaking. Child Abuse Negl. 2006;30:7–16. doi: 10.1016/j.chiabu.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 27.Keenan HT, Runyan DK, Marshall SW, et al. A population-based comparison of clinical and outcome characteristics of young children with serious inflicted and noninflicted traumatic brain injury. Pediatrics. 2004;114:633–9. doi: 10.1542/peds.2003-1020-L. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keenan HT. Practical aspects of conducting a prospective statewide incidence study: the incidence of serious inflicted traumatic brain injury in North Carolina. Am J Prev Med. 2008;34(4 Suppl):S120–5. doi: 10.1016/j.amepre.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thomas NJ, Shaffer ML, Rzucidlo S, et al. Temporal factors and the incidence of physical abuse in young children: decreased nonaccidental trauma during child abuse prevention month. J Pediatr Surg. 2007;42:1735–9. doi: 10.1016/j.jpedsurg.2007.05.032. [DOI] [PubMed] [Google Scholar]
- 30.Parslow RC, Morris KP, Tasker RC, et al. Epidemiology of traumatic brain injury in children receiving intensive care in the UK. Arch Dis Child. 2005;90:1182–7. doi: 10.1136/adc.2005.072405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Winn DG, Agran PF, Anderson CL. Sensitivity of hospitals’ E-coded data in identifying causes of children’s violence-related injuries. Public Health Rep. 1995;110:277–81. [PMC free article] [PubMed] [Google Scholar]
- 32.O’Donnell M, Nassar N, Leonard H, et al. Monitoring child abuse and neglect at a population level: patterns of hospital admissions for maltreatment and assault. Child Abuse Negl. 2010;34:823–32. doi: 10.1016/j.chiabu.2010.04.003. [DOI] [PubMed] [Google Scholar]
- 33.Barr R, Barr M, Fujiwara T, et al. Do educational materials change knowledge and behavior about crying and shaken baby syndrome? A randomized controlled trial CMAJ. 2009;180:727–33. doi: 10.1503/cmaj.081419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Catherine N, Ko JJ, Barr RG. Getting the word out: advice on crying and colic in popular parenting magazines. J Dev Behav Pediatr. 2008;29:508–11. doi: 10.1097/DBP.0b013e31818d0c0c. [DOI] [PubMed] [Google Scholar]
- 35.Committee on Child Abuse and Neglect of the American Academy of Pediatrics. Shaken baby syndrome: rotational cranial injuries: technical report. Pediatrics. 2001;108:206–10. doi: 10.1542/peds.108.1.206. [DOI] [PubMed] [Google Scholar]
- 36.Klevens J. Prevention of inflicted neurotrauma: what we know, what we don’t know, and what we need to know. In: Reece RM, Nicholson CE, editors. Inflicted Childhood Neurotrauma. Elk Grove Village, Illinois, USA: American Academy of Pediatrics; 2003. pp. 269–79. [Google Scholar]
- 37.Centers for Disease Control and Prevention. Preventing Shaken Baby Syndrome: a Guide for Health Departments and Community-Based Organizations. 2011 http://www.cdc.gov/Concussion/pdf/Preventing_SBS_508-a.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


