Abstract
Background
We describe a novel algorithm for identifying transgender people and determining their male-to-female (MTF) or female-to-male (FTM) identity in electronic medical records (EMR) of an integrated health system.
Methods
A SAS program scanned Kaiser Permanente Georgia EMR from January 2006 through December 2014 for relevant diagnostic codes, and presence of specific keywords (e.g., “transgender” or “transsexual”) in clinical notes. Eligibility was verified by review of de-identified text strings containing targeted keywords, and if needed, by an additional in-depth review of records. Once transgender status was confirmed, FTM or MTF identity was assessed using a second SAS program and another round of text string reviews.
Results
Of 813,737 members, 271 were identified as possibly transgender: 137 through keywords only, 25 through diagnostic codes only, and 109 through both codes and keywords. Of these individuals, 185 (68%, 95% confidence interval [CI]: 62-74%) were confirmed as definitely transgender. The proportions (95% CIs) of definite transgender status among persons identified via keywords, diagnostic codes, and both were 45% (37-54%), 56% (35-75%), and 100% (96-100%), respectively. Of the 185 definitely transgender people, 99 (54%, 95% CI: 46-61%) were MTF, 84 (45%, 95% CI: 38-53%) were FTM. For two persons, gender identity remained unknown. Prevalence of transgender people (per 100,000 members) was 4.4 (95% CI: 2.6-7.4) in 2006 and 38.7 (95% CI: 32.4-46.2) in 2014.
Conclusions
The proposed method of identifying candidates for transgender health studies is low cost and relatively efficient. It can be applied in other similar health care systems.
Keywords: transgender, electronic medical records, algorithm, prevalence
INTRODUCTION
Transgender people are a heterogeneous group of individuals who transcend normative cultural definitions and categories of sex and gender. Sex is assigned at birth based on primary sexual characteristics [1]. A person’s gender refers to one’s sense of maleness, femaleness, neither, or both [1, 2]. Transgender people are those whose gender identity or expression differs from the sex originally assigned to them at birth [3]. While self-identification of transgender people may not fit binary definitions [4], a person whose gender identity differs from a male sex assignment at birth is often referred to as male-to-female (MTF) and a person whose gender identity differs from a female sex assignment at birth is often referred to as a female-to-male (FTM) [5]. Transgender people may experience gender dysphoria, which is a diagnostic term that describes “a discomfort or distress that is caused by a discrepancy between a person’s gender identity and that person’s sex assigned at birth” [6]. In some cases gender dysphoria requires gender affirmation, which may include hormonal or surgical treatment, or both [7].
The 2011 Institute of Medicine report on the health of sexual and gender minorities specifically emphasized the need for more information about people who are transgender [8]. Even basic information, such as the proportion of transgender people in the general population, is not known with certainty because most available studies are based on convenience samples without an identifiable population denominator [9].
Electronic medical records (EMR) provide diagnostic codes that offer opportunities for the identification of hard-to-reach subgroups in large well-defined populations. However, for transgender people, reliance on the diagnostic codes for gender dysphoria or related diagnoses is inadequate because many transgender people experience no gender dysphoria and have no need for gender affirmation therapy. In addition, transgender people who are already receiving or wish to receive hormonal or surgical gender affirmation may not have transgender-specific diagnoses documented in the EMR [10]. An alternative option to identify transgender people in medical records could be through natural language processing (NLP) methods. Many NLP methods are complex and require specialized software, substantial expertise, time, and cost to build a reliable computerized algorithm [11, 12]. Relatively simple algorithms that use standard software may be more practical.
In this communication, we describe a method for creating and validating a cohort of transgender people using a simple algorithm that combines diagnostic codes and text string-based NLP. We also show how following confirmation of transgender status, the algorithm is useful for identifying each person’s MTF or FTM status. We then apply this algorithm to estimate proportion of transgender people among members of an integrated health care system.
METHODS
Study Setting
This study took place at Kaiser Permanente Georgia (KPGA), an integrated care delivery system that provided health services to approximately 813,000 enrollees between 2006 and 2015. The study was conducted in cooperation with the Emory University School of Public Health. All activities described in this manuscript were reviewed and approved by the Institutional Review Boards (IRB) of both institutions. KPGA is a member of several research consortia including the Health Care Systems Research Network (formerly known as the HMO Research Network [13] and the Mental Health Research Network) [14]. The 19 health care systems comprising these networks have over 20 million enrollees, use similar EMR systems, and have comparably organized databases with identical variables names, formats, and specifications across sites. [15].
Algorithm
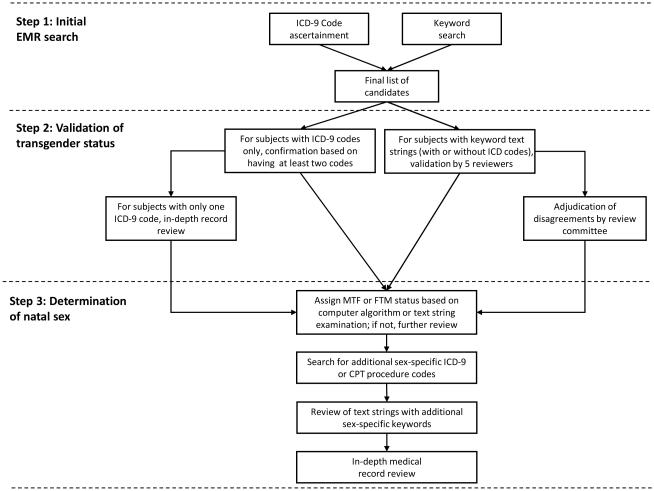
A flow diagram describing the 3-step algorithm used in this study is presented in Figure 1. In Step 1, a SAS program (SAS institute, Cary, NC) examined EMR pertaining to 813,737 Kaiser Permanente Georgia (KPGA) members of all ages enrolled between January 1, 2006 and December 31, 2014 to identify two types of evidence supporting transgender status: 1) relevant International Classification of Diseases Ninth edition (ICD-9) codes; and 2) presence of relevant specific keywords in free-text notes.
Figure 1.
Flow diagram of assessing transgender status and natal sex among KPGA members
The diagnostic ICD-9 codes suggestive of transgender status were selected based on methodology described in earlier studies [16, 17]. These codes included: 302.5 (“Transsexualism”); 302.50 (“Transsexualism with unspecified sexual history, a.k.a. transsexualism not otherwise specified”); 302.51 “Ttranssexualism with asexual history”); 302.52 (“Transsexualism with homosexual history”); 302.53 (“Transsexualism with heterosexual history”); 302.85 (“Gender identity disorder in adolescents or adults”); 302.6 (“Gender identity disorder in children”); and 302.3 (“Transvestic fetishism”). We also used ICD-9 V codes which are used for supplementary classification of factors influencing health status [18]. V codes identify circumstances for patient visits that are for reasons other than a disease or injury and are used to report problems or factors that may influence present or future care [19]. As V codes may cover several conditions, we used them in conjunction with internal KPGA codes to ensure specificity. For example, a combination of ICD-9 code V49.89 and KPGA code 121141596 means “Other conditions influencing health: transgender.” Additional code combinations used for selection of study participants were V45.77 +121141596 (“Acquired absence of genital organs: history of sex reassignment surgery”); V07.8 + 12124952 (“Other specified prophylactic measure: male-to-female hormone supplementation”); and V07.8 + 12124310 “(Other specified prophylactic measure: female-to-male hormone supplementation”).
As many transgender people do not receive any of the above diagnostic codes, the second method of transgender ascertainment used a SAS program that identified the following keywords in digitized free-text clinical notes: “transgender”, “transsexual” “transvestite,” “gender identity” “gender dysphoria,” and “gender reassignment” (these keywords were not case-sensitive). This list of keywords was created in consultation with the Stakeholder Advisory Group, which included health care providers specializing in transgender care and representatives of the transgender community [20]. The process started with an expanded list of keywords provided by the stakeholders. The expanded list was gradually shortened after step-wise removal of keywords that did not contribute additional cases. The resulting list of six keywords provided a complete cohort ascertainment with the shortest program running time. Improving efficiency was necessary because the program is designed to be applicable in health care systems that are much larger than KPGA. A separate SAS program then extracted short strings of text that included 100 characters before and 50 characters after the keyword of interest.
In the second step of the algorithm, we verified transgender status of potential cohort candidates identified via keywords of interest, ICD-9 codes, or both (Figure 1). For members whose clinical notes contained the keywords of interest (with or without an ICD-9 code), validation was done by five trained reviewers who read each extracted text sting to confirm “definitely transgender” status. Prior to review, all patient names, addresses and other identifiers were deleted. Disagreements among reviewers were adjudicated by a review committee. Members who had no keywords in their records, but had more than one ICD-9 code of interest, were considered definitely transgender and did not require further verification. For those members who had only one relevant ICD-9 code and no keyword, and for persons whose text string review was inconclusive, transgender status was verified by an in-depth review of the EMR. The in-depth review was conducted by a KPGA project manager with authorized and IRB-approved access to medical records. The project manager identified notes associated with the visit that had the ICD code of interest and then presented de-identified text to the committee members who made final determination of eligibility.
Step 3 of the algorithm was used to identify each eligible subject’s MTF or FTM status. This was done because a preliminary review of the KPGA administrative records revealed that the data sometimes reflected natal (assigned at birth) sex and at other times current gender identity. The study participants were categorized as MTF or FTM using several methods. First, a SAS program searched all text strings and ICD-9 codes extracted for Step 1 to identify additional words such as “male-to-female,” “female-to-male”, and gender affirmation V codes (V07.8 +12124952 and V07.8 +12124310). Next, during the text string validation, the reviewers were instructed to categorize each eligible person as MTF, FTM, or unclear. For persons whose natal sex was unclear, additional examination of the EMR involved: 1) identification of ICD-9 or Current Procedure Terminology (CPT) codes for sex-specific diagnoses (e.g., prostate cancer) and procedures (e.g., hysterectomy); 2) review of additional text strings that included sex-specific keywords (e.g., “testes” or “ovaries”); and 3) an in-depth review of records.
Analysis
The proportions of KPGA members designated as definitely transgender were computed for each of the three modes of identifying potential cohort candidates: keywords only, ICD-9 codes only, and both ICD-9 codes and keywords. Each proportion was accompanied by a 95% confidence interval (CI) calculated based on Fleiss quadratic correction using OpenEpi statistical calculator [21].
The prevalence of definitely transgender status was then calculated. For each eligible person, the date of the first visit associated with the keyword or ICD-9 code of interest was considered the index date. To be included in the prevalence numerator for a given year, a person had to be enrolled in KPGA at any time during that year, and to have an index date during or before that year. The denominator comprised all KPGA members for the same year. All prevalence estimates and the corresponding 95% CIs were expressed per 100,000 persons.
RESULTS
Using our methodology, 271 persons were identified as possibly transgender. Of these, 51% (N=137) were identified through keywords only, 9% (N=25) through ICD-9 codes only, and 40% (109) by both ICD-9 codes and keywords (Table 1). Among these individuals, 185 (68%; 95% CI: 62-74%) were confirmed as definitely transgender (Table 1). Based on validation results, the positive predictive values (95% CIs) for keywords, diagnostic codes, and both were 45% (37-54%), 56% (35-75%), and 100% (96-100%), respectively. The leading reason for non-eligibility was the use of a keyword in the EMR note that was not related to the patient. Only 3% (9 of 271) had “uncertain” status.
Table 1.
Results of eligibility validation for alternative modes of cohort ascertainment
| Mode of Ascertainment |
Number of Patients |
Determination of Cohort Eligibility; N, row percentages (95% CI)* |
||
|---|---|---|---|---|
| Definitely transgender |
Definitely not transgender |
Possibly transgender** |
||
| Progress note keyword(s) only |
137 | 62 45% (37-54%) |
73 53% (45-62%) |
2 1% (0-6%) |
| ICD-9 code(s) only | 25 | 14 56% (35-75%) |
4 16% (5-37%) |
7 28% (13-50%) |
| Both keyword(s) and ICD-9 code(s) |
109 | 109 100% (96-100%) |
0 (0%; 0-4%) |
0 0% (0-4%) |
| Total | 271 | 185 68% (62-74%) |
77 28% (23-34%) |
9 3% (2-6%) |
may not add up to 100% due to rounding
Includes persons whose text strings and/or in depth records reviews were inconclusive
Among the 246 of the 271 persons identified using keyword searches, agreement among all five reviewers was 85% (Table 2). After adjudication of the remaining 15%, transgender status of only two persons remained unresolved by review of text strings. The additional in-depth review of records for these two individuals did not allow a more definitive ascertainment of transgender status.
Table 2.
Agreement among five reviewers in assessing cohort eligibility*
| Outcome of text string reviews | Conclusion; N | Percentage of total (95% CI)** |
|---|---|---|
| Complete agreement among all 5 reviewers | Eligible; N=149 Not Eligible; N=61 Uncertain; N=0 |
61% (54-67%) 25% (20-31%) 0% (0-2%) |
| 4:1 disagreement; adjudicated | Eligible; N=14 Not Eligible; N=5 Uncertain; N=0 |
6% (3-10%) 2% (1-5%) 0% (0-2%) |
| 3:2 disagreement; adjudicated | Eligible; N=8 Not Eligible; N=7 Uncertain; N=0 |
3% (2-7%) 3% (1-6%) 0% (0-2%) |
| 3:2 disagreement; remained uncertain after adjudication | Eligible; N=0 Not Eligible; N=0 Uncertain; N=2 |
0% (0-2%) 0% (0-2%) 1% (0-3%) |
Limited to 246 subjects with at least one text string available
Does not add up to 100% because of rounding
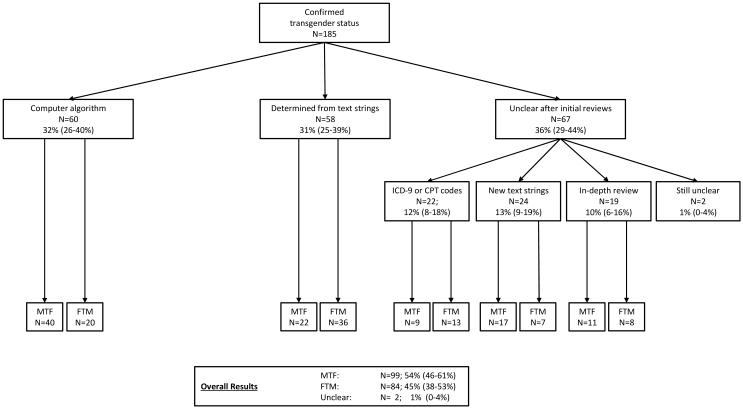
Natal sex for the 185 definitely transgender people was ascertained by computer algorithm or initial text string review for 32% (N=60), and 31% (N=58), respectively (Figure 2). The remaining 67 subjects underwent additional evaluation using ICD and CPT codes, sex-specific keywords or further in-depth review of records. As a result, natal gender was successfully determined for 99% (183 of 185) of definitely transgender study participants: 54% (99 of 185, 95% CI: 46-61%) were MTF and 45% (84 of 185, 95% CI: 38-53%) were FTM.
Figure 2.
Natal sex ascertainment among confirmed transgender KPGA members
Table 3 displays prevalence estimates over time and by natal sex. For the entire study interval (2006-2014), the estimated prevalence of transgender (per 100,000 KPGA members) was 22.7 (95% CI: 19.6-26.3). This number varied by year: 4.4 (95% CI: 2.6-7.4) in 2006, and 38.7 (95% CI: 32.4-46.2) in 2014. The 2006-2014 prevalence estimates (95% CI) for MTF and FTM were 25.6 (20.9-31.3) and 19.7 (15.8-24.5) per 100,000 natal males and females, respectively.
Table 3.
Prevalence of “Definitely Transgender” by natal sex among KPGA members 2006-2014
| Year | All transgender persons |
All HMO members |
Prevalence estimate (95% CI)* |
FTM** | Total natal females** |
Prevalence estimate (95% CI)* |
MTF** | Total natal males** |
Prevalence estimate (95% CI)* |
|---|---|---|---|---|---|---|---|---|---|
| 2006 | 15 | 340,909 | 4.4 (2.6-7.4) | 3 | 179,921 | 1.7 (0.4-5.3) | 11 | 160,988 | 6.8 (3.6-12.6) |
| 2007 | 21 | 332,482 | 6.3 (4.0-9.8) | 7 | 175,480 | 4.0 (1.7-8.6) | 14 | 157,002 | 8.9 (5.1-15.4) |
| 2008 | 38 | 323,116 | 11.8 (8.4-16.3) | 16 | 171,452 | 9.3 (5.5-15.5) | 21 | 151,664 | 13.8 (8.8-21.6) |
| 2009 | 41 | 310,488 | 13.2 (9.6-18.1) | 15 | 165,061 | 9.1 (5.3-15.4) | 26 | 145,427 | 17.9 (11.9-26.6) |
| 2010 | 46 | 270,730 | 17.0 (12.6-22.9) | 15 | 142,482 | 10.5 (6.1-17.8) | 31 | 128,248 | 24.2 (16.7-34.8) |
| 2011 | 63 | 295,371 | 21.3 (16.5-27.5) | 28 | 155,684 | 18.0 (12.2-26.4) | 35 | 139,687 | 25.1 (17.7-35.3) |
| 2012 | 74 | 293,966 | 25.2 (19.9 -31.8) | 29 | 154,521 | 18.8 (12.8-27.3) | 45 | 139,445 | 32.3 (23.8-43.6) |
| 2013 | 91 | 300,481 | 30.3 (24.5-37.4) | 41 | 157,490 | 26.0 (18.9-35.7) | 50 | 142,972 | 35.0 (26.2-46.5) |
| 2014 | 128 | 330,727 | 38.7 (32.4-46.2) | 58 | 173,411 | 33.4 (25.6-43.6) | 70 | 157,285 | 44.5 (35.0-56.6) |
|
| |||||||||
| 2006-2014 | 185 | 813,737 | 22.7 (19.6-26.3) | 84 | 426,440 | 19.7 (15.8-24.5) | 99 | 387,251 | 25.6 (20.9-31.3) |
per 100,000 population
Excludes 2 persons in the numerator and 46 persons in the denominator with unknown natal sex
DISCUSSION
In this study, we demonstrate that by using a relatively simple SAS algorithm -- based on standard codes and supplemented with analysis of digitized provider notes -- it is possible to more completely identify transgender status of individuals than would be possible using codes alone. The use of keyword-containing text strings clearly enhanced cohort ascertainment relative to ICD code-based approaches. On the other hand, reliance on keywords without text string validation would have erroneously included a substantial number of persons who are not transgender. Additional review of records was necessary to confirm transgender status and identify false-positives. Most commonly, this occurred when a keyword of interest (e.g., “transgender”) was referring not to the patient but to the patient’s close relative, or partner. In other false-positive situations the keywords of interest were used as part of standard text, such as when listing indications for hormone use.
Previous studies that have estimated proportions of transgender people using medical records fall into two categories: those that have focused on receipt of surgical or hormonal gender affirmation therapy and those that defined the numerator based on transgender-related diagnoses. Most reported prevalence estimates based on these two methods have ranged from 1 to 10 per 100,000 individuals [22-26]. Our results are outside of this range, a discrepancy that may have several explanations. First, approximately one-third of eligible participants in our study would have been missed if the cohort selection methods were limited to standard code-based methods. Second, as our analysis was based on comparatively recent data, the higher prevalence in our study may reflect the secular trend of an increasing proportion of people who acknowledge their transgender status. Third, the majority of previous studies quantified the numerator (usually by canvassing specialized clinics in a given area) and then used an approximated population size to arrive at a prevalence estimate. In our study, the availability of EMR data and a more complete ascertainment of both the numerator and the denominator likely produced a more accurate result.
Our findings are consistent with two US-based studies that used the Veterans Health Administration (VHA) data [27, 28]. The more recent of the two papers reported prevalence of transgender-related diagnoses of 3.5 per 100,000 in 2006 and 32.9 per 100,000 in 2013 [28]. It is notable that the numerator in the VHA study was defined based on ICD-9 codes only, and for this reason, the true prevalence of transgender status among veterans may be higher. It is also important to keep in mind that the VHA analyses did not distinguish between MTF and FTM, and the denominator in the prevalence calculations included mostly natal males.
In recent months the U.S. Department of Health and Human Services issued a directive that instructs that EMR systems to find a way to record a patient’s sexual orientation and gender identity in a structured way with standardized data. It may take some time before gender identity data become widely available because the directive specifically “does not require that a provider collect this information”, but it requires only that the EMR “enable the provider to do so” [29].
The main advantages of our method are the use of a simple SAS program for initial cohort selection, and the relatively low cost and efficiency of validation procedures. No costly specialized NLP software or extensive informatics expertise was required. The use of five reviewers for each text string validation was guided by the need to train research staff members who will perform similar tasks at much larger sites. In the future, two reviews of each case, with adjudication of disagreements, should be sufficient and will lower the cost of cohort validation. Only a small proportion of cohort candidates required detailed EMR review.
In summary, our method of identifying candidates for transgender health studies is relatively low-cost, rapid and capable of identifying persons who would have been missed by traditional approaches. The SAS programs and the validation algorithms developed for this study can be applied in other health care systems that use similar EMR data structure.
ACKNOWLEDGMENTS
This research was supported by the Contract AD-12-11-4532 from the Patient Centered Outcome Research Institute and by the Grant R21HD076387 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Lombardi E. Enhancing transgender health care. Am J Public Health. 2001;91:869–872. doi: 10.2105/ajph.91.6.869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bockting W, Coleman E, De Cuypere G. Care of transsexual persons. N Engl J Med. 2011;364:2559–2560. doi: 10.1056/NEJMc1104884. [DOI] [PubMed] [Google Scholar]
- 3.Gardner IH, Safer JD. Progress on the road to better medical care for transgender patients. Curr Opin Endocrinol Diabetes Obes. 2013;20:553–558. doi: 10.1097/01.med.0000436188.95351.4d. [DOI] [PubMed] [Google Scholar]
- 4.Bockting W. From construction to context: Gender through the eyes of the transgendered. Siecus Report. 1999;28:3–7. [Google Scholar]
- 5.Giami A, Beaubatie E. Gender identification and sex reassignment surgery in the trans population: a survey study in France. Arch Sex Behav. 2014;43:1491–1501. doi: 10.1007/s10508-014-0382-3. [DOI] [PubMed] [Google Scholar]
- 6.Knudson G, De Cuypere G, Bockting W. Recommendations for revision of the DSM diagnoses of gender identity disorders: Consensus statement of the World Professional Association for Transgender Health. Int J Transgenderism. 2010;12:115–118. [Google Scholar]
- 7.Gooren LJ. Clinical practice. Care of transsexual persons. N Engl J Med. 2011;364:1251–1257. doi: 10.1056/NEJMcp1008161. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine . The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. The National Academies Press; Washington, DC: 2011. [PubMed] [Google Scholar]
- 9.Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: A systematic review. Lancet. 2015 doi: 10.1016/S0140-6736(16)00684-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deutsch MB, Buchholz D. Electronic health records and transgender patients--practical recommendations for the collection of gender identity data. J Gen Intern Med. 2015;30:843–847. doi: 10.1007/s11606-014-3148-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iyer SV, Harpaz R, LePendu P, et al. Mining clinical text for signals of adverse drug-drug interactions. J Am Med Inform Assoc. 2014;21:353–362. doi: 10.1136/amiajnl-2013-001612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGarvey PB, Suzek BE, Baraniuk JN, et al. In silico analysis of autoimmune diseases and genetic relationships to vaccination against infectious diseases. BMC Immunol. 2014;15:61. doi: 10.1186/s12865-014-0061-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lieu TA, Hinrichsen VL, Moreira A, Platt R. Collaborations in population-based health research: the 17th annual HMO Research Network Conference, March 23-25, 2011, Boston, Massachusetts, USA. Clin Med Res. 2011;9:137–140. doi: 10.3121/cmr.2011.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Simon GE, Stewart C, Beck A, et al. National prevalence of receipt of antidepressant prescriptions by persons without a psychiatric diagnosis. Psychiatr Serv. 2014;65:944–946. doi: 10.1176/appi.ps.201300371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goodman M, Fletcher RH, Doria-Rose VP, et al. Observational methods to assess the effectiveness of screening colonoscopy in reducing right colon cancer mortality risk: SCOLAR. J Comp Eff Res. 2015:1–11. doi: 10.2217/cer.15.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown GR, Jones KT. Racial health disparities in a cohort of 5,135 transgender veterans. J Racial Ethnic Health Disparities. 2014;1:257–266. [Google Scholar]
- 17.Brown GR, Jones KT. Incidence of breast cancer in a cohort of 5,135 transgender veterans. Breast Cancer Res Treat. 2015;149:191–198. doi: 10.1007/s10549-014-3213-2. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organisation . International Statistical Classification of Diseases and Related Health Problems, 9th Revision. WHO; Geneva: 1978. [Google Scholar]
- 19.Maguire N. search of the "V" codes (ICD-9-CM) J Med Pract Manage. 2012;28:56–57. [PubMed] [Google Scholar]
- 20.Quinn V, Becerra T, Gillespie T, et al. Embedding patients, providers, and community stakeholders in research to improve transgender health. J Patient-Centered Res Rev. 2015;2:114–115. [Google Scholar]
- 21.Sullivan KM, Dean A, Soe MM. OpenEpi: a web-based epidemiologic and statistical calculator for public health. Public Health Rep. 2009;124:471–474. doi: 10.1177/003335490912400320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bakker A, van Kesteren PJ, Gooren LJ, Bezemer PD. The prevalence of transsexualism in The Netherlands. Acta Psychiatr Scand. 1993;87:237–238. doi: 10.1111/j.1600-0447.1993.tb03364.x. [DOI] [PubMed] [Google Scholar]
- 23.Judge C, O'Donovan C, Callaghan G, et al. Gender dysphoria -prevalence and co-morbidities in an irish adult population. Front Endocrinol (Lausanne) 2014;5:87. doi: 10.3389/fendo.2014.00087. 10.3389/fendo.2014.00087. eCollection 02014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baba T, Endo T, Ikeda K, et al. Distinctive features of female-to-male transsexualism and prevalence of gender identity disorder in Japan. J Sex Med. 2011;8:1686–1693. doi: 10.1111/j.1743-6109.2011.02252.x. [DOI] [PubMed] [Google Scholar]
- 25.O'Gorman EC. A retrospective study of epidemiological and clinical aspects of 28 transsexual patients. Arch Sex Behav. 1982;11:231–236. doi: 10.1007/BF01544991. [DOI] [PubMed] [Google Scholar]
- 26.Caldarera A, Pfäfflin F. Transsexualism and sex reassignment surgery in Italy. Int J Transgender. 2011;13:26–36. [Google Scholar]
- 27.Blosnich JR, Brown GR, Shipherd JC, Phd, et al. Prevalence of gender identity disorder and suicide risk among transgender veterans utilizing veterans health administration care. Am J Public Health. 2013;103:e27–32. doi: 10.2105/AJPH.2013.301507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kauth MR, Shipherd JC, Lindsay J, et al. Access to care for transgender veterans in the Veterans Health Administration: 2006-2013. Am J Public Health. 2014;104(Suppl 4):S532–534. doi: 10.2105/AJPH.2014.302086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services . Department of Health and Human Services; Rockville, MD: 2015. Medicare and Medicaid Programs; Electronic Health Record Incentive Program—Stage 3 and Modifications to Meaningful Use in 2015 through 2017. [Google Scholar]