Abstract
This study applies qualitative research methods to explore perspectives on cessation among smokers/former smokers recruited from an area of Northern Appalachia. Six focus groups, stratified by age group (18–39 years old and 40 years and older), were conducted among participants (n=54) recruited from community settings. Participants described varied interest in and challenges with quitting smoking. Smokers 40 years and older more readily endorsed the health risks of smoking and had greater interest in quitting assistance. Participants expressed frustration with the U.S. government for allowing a harmful product (e.g., cigarettes) to be promoted with minimal regulation. Use of social media was robust among both age groups; participants expressed limited interest in various social media/technology platforms for promoting smoking cessation. Findings from this understudied area of northern Appalachia reflect the heterogeneity of this region and contribute novel information about the beliefs, attitudes, and experiences of current and formers smokers with regard to cessation.
Keywords: smoking cessation, Appalachia, adults, rural population, qualitative
Introduction
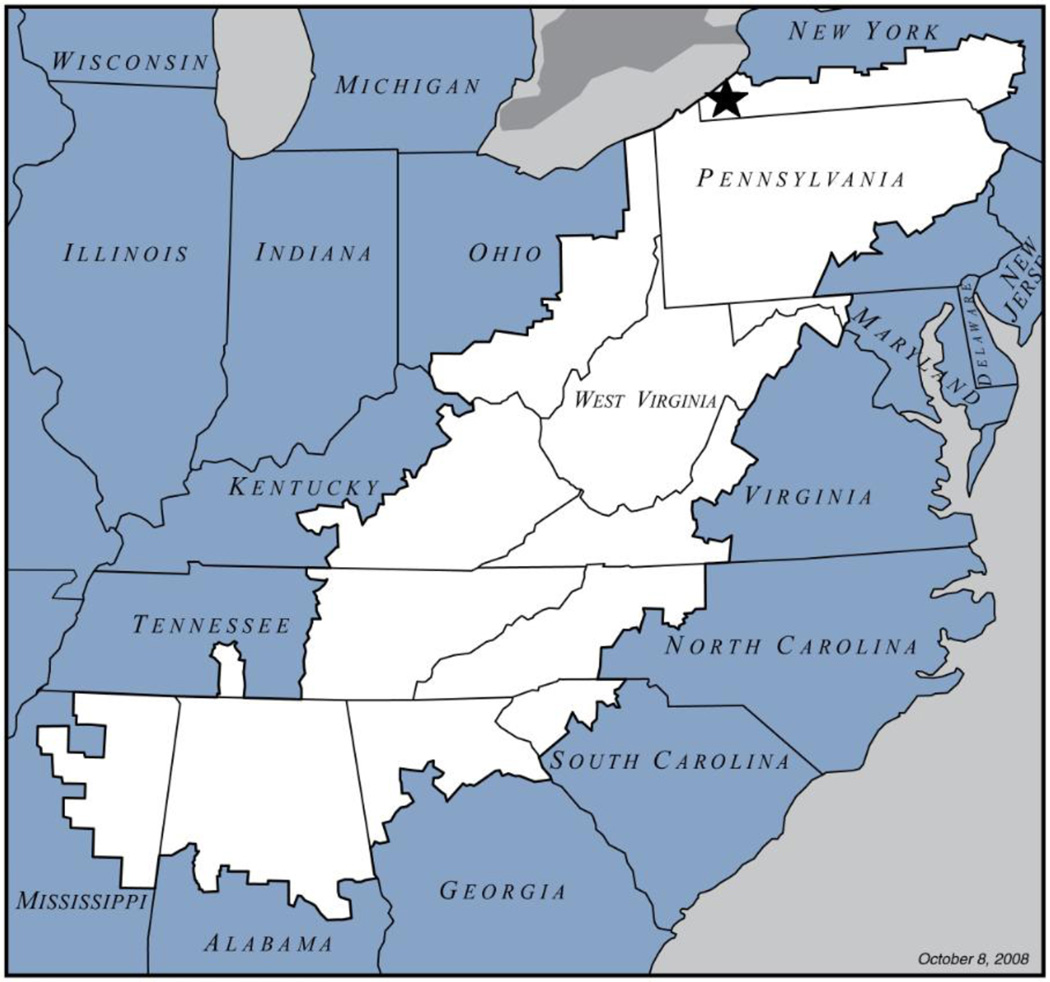
Tobacco use ranks as a major health concern for rural communities, along with higher rates of obesity, heart and lung diseases, alcoholism and substance abuse (Hutcheson, et al, 2008). The Appalachian region in the United States (U.S.) has a population of over 25 million people and over 42 percent of the population is located in rural areas (Northridge, et al, 2008, Division, Appalachian Regional Commission Regional Planning and Research, 2011). The Appalachian region includes parts of several states including southern New York (Northern Appalachian region). Smoking rates in the Appalachia region of the U.S. are 24.2 percent compared to 21.9 percent in non-Appalachia regions (Meyer, et al, 2008). The Appalachian population confronts increased health risks - especially those linked to tobacco- as compared to many of their national counterparts; therefore, it is essential to focus efforts on preventive health care programs with an emphasis on tobacco control and smoking cessation. Even with higher tobacco use prevalence rates, the published research on the topic of tobacco cessation among rural populations is somewhat limited, particularly studies specific to the Northern Appalachian region in New York state (NYS) (see Figure 1).
Figure 1.
Map of Appalachian Region
Source: Appalachian Regional Commission
Appalachia as a whole not only embodies an economically depressed/challenged area but also represents a region in the U.S. that has pockets of extremely low Healthcare Cost, Coverage and Access (HCCA) scores by county (PDA, Inc., and the Cecil B. Sheps Center for Health Services Research, 2012). An ideal HCCA score is at or above the 80th percentile; however, the majority of Appalachian states & counties are well below the 80th percentile. The low HCCA scores in the Appalachian counties are reflective of lower than average healthcare resources, insurance coverage, and reimbursement compared to the nation as a whole (PDA, Inc., and the Cecil B. Sheps Center for Health Services Research, 2012). Another important facet of healthcare access is infrastructure and personnel available to provide primary care. Regional designation as a Health Professional Shortage Area (HPSA) is another metric directly relating to challenges with access. According to the U.S. census bureau at least one-fifth of the population, or 51 million persons, reside in non-metropolitan areas and of these, 20 million live in federally designated HPSAs. The northern region of Appalachia within NYS is designated as a medically underserved area with four HPSA designations (i.e., two primary care, one dental, and one mental health) (Chautauqua County Health Network, 2014).
The majority of published studies on smoking cessation efforts in Appalachia represent communities located in Kentucky (Schoenberg, et al, 2014, Butler, et al, 2012, Kruger, et al, 2012) and the central and southern regions (Northridge, et al, 2008). Relatively little is known about the effectiveness of population-based interventions to reach smokers in Northern Appalachia. Counties bordering the southwestern edge of New York State (NYS) represent the most northern regions of Appalachia (see Figure 1). While NYS has the highest cigarette tax rate in the country, (Orzechowski and Walker, 2008) it ranks eighth among the states with respect to prevalence of cigarette smoking among adults at 18.1% in 2011, (Centers for Disease Control and Prevention (CDC) and Centers for Disease Control and Prevention (CDC), 2011) and among youth who smoke cigarettes (12.5% in 2011), NYS ranks fourth among 44 states (Eaton, et al, 2012). Considering the high prevalence of cigarette smoking among adults and youth in NYS despite having the highest tax rate on cigarettes there are opportunities to better understand effective strategies for smoking cessation especially among those populations most affected.
The goal of this research was to understand the perspectives and experiences with smoking cessation among current and former smokers recruited from community settings in this largely understudied New York State area within northern Appalachia. This formative research was done as part of a larger study to test the effectiveness of using advanced communication technologies to deliver tobacco cessation messaging. In trying to address health disparities within areas of Appalachia, and more specifically efforts related to smoking cessation interventions, there needs to be careful consideration of community impressions, access to resources in the community and the level of capacity required from existing resources to facilitate such an intervention in a high need and low resource setting.
Methods
Population studied
Geographic and demographic characteristics
Appalachian New York includes 14 counties with a population of 1,064,968 and represents just over 5% of the state’s total population within a land area of 11,681 square miles (about 25% of the land area within New York State) (U.S. Census Bureau, 2012). The populations studied were recruited from three small towns within Chautauqua County, which covers about 1,060 square miles with approximately 127 persons per square mile (US Census Bureau, 2014). Located within southwestern New York State, this county includes a population of 133,539: 94.2 percent White, 2.7 percent African American and 6.5 percent Hispanic/Latino (U.S. Census Bureau, 2012). The smoking rate in Chautauqua County is 25.3 percent which is higher than NYS and the average Appalachian county smoking rate of 24.31 (Dino, et al, 2012, New York State Department of Health, 2009).
Recruitment and Participants
We applied a community-based participatory research (CBPR) approach to engage in a collaborative research partnership which included academic investigators from the regional comprehensive cancer center and State University, with community partners from three primary care medical offices organized in a health network in Chautauqua County, NY. Practice sites were selected based upon their location in predominately medically underserved and rural communities of Chautauqua County. We employed a variety of recruitment strategies including community canvassing at retail store locations and posting flyers in medical office waiting rooms, the local health department, and additional surrounding community venues. A total of six focus groups (n=54 total participants) were conducted between August 2012 through October 2012, stratified by age group (persons 18–39 years old and 40+ years because of the expected differences in use of social media and technology) to explore potential age-related differences in perceptions/experiences regarding tobacco cessation and the use of information and communication technologies.
Data collection
Focus group participants included current or former smokers who were at least 18 years of age. The focus groups were facilitated by two experienced research staff and conducted at community venues within each of the three respective communities. Each focus group was audio recorded and lasted on average 60 minutes. The study was approved by the cancer center institutional review board. All participants reviewed an informational sheet explaining the study and granted oral consent prior to their participation and permission to record the sessions for subsequent analysis; all data was collected anonymously. Participants each received a $30 gift card to a local grocery store.
At the start of each focus group we collected demographic information and participants’ current smoking status using an Audience Response System (ARS) program. The ARS allows program facilitators to read the questions aloud and participants responded anonymously by using a wireless keypad. This technology represents an effective research and education tool for compiling data among low-literacy populations (Sudarsan, et al, 2011). A semi-structured guide was used to facilitate group discussion topics which included tobacco use, decisions related to cessation, quit attempts and resources that may enhance cessation. As this formative study was part of a larger study to incorporate appropriate messaging into a telephone-based cessation program, we included specific questions related to perceptions and experiences with automated call technology, preferences for tobacco cessation messaging and access/use of technology and social media.
Data analysis
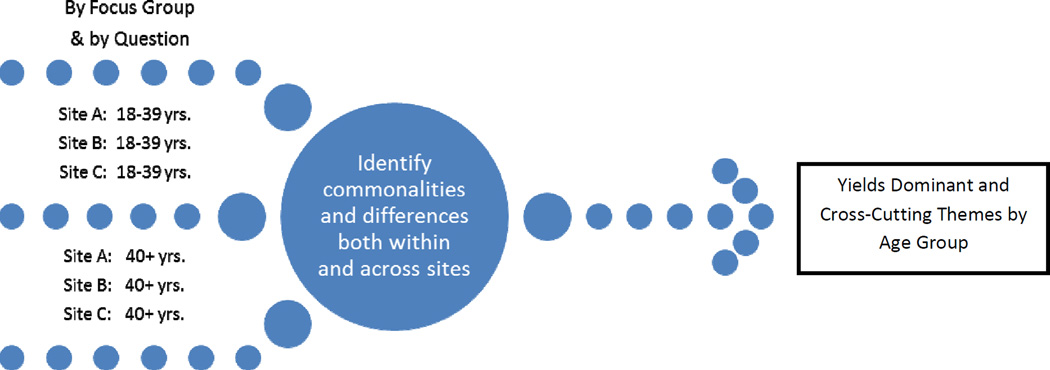
The first author created an analysis framework (Figure 2) that took into consideration the stratified design and participant responses to the focus group questions across the three sites (i.e., Sites A, B, C). All authors agreed on the analysis framework and two of the authors (EMR and AMT) analyzed the transcripts. Focus group recordings were transcribed and entered into QSR NVivo 8 qualitative software (QSR International, Victoria, Australia). The project data manager checked the transcripts for consistency with the audio recording and the two group facilitators who conducted the sessions verified the transcripts for accuracy. Each coder created a summary of themes/topics by focus group and then met to compare their individual analyses to verify agreement and detect any differences. Upon discussion and review of the findings, dominant and cross-cutting themes were identified and agreed upon by the co-authors. Quantitative data collected using the ARS was transferred into SPSS (Version 16.0, SPSS Inc., Chicago, IL) and sociodemographic information was summarized using descriptive statistics; final results are reported in Table 1. No individual identifiers were collected from any of the participants.
Figure 2.
Analytic Framework for Focus Group Data
Table 1.
Rural Focus Group Participant Demographics and Smoking Status, by age category.
| Variables | Focus Group | Total | p-value | ||
|---|---|---|---|---|---|
| Age 18–39 years n (%) |
Age 40+ years n (%) |
||||
| Attendees | Site A | 4 (14%) | 5 (20%) | 9 (17%) | 0.789 |
| Site B | 19 (66%) | 16 (64%) | 35 (65%) | ||
| Site C | 6 (21%) | 4 (16%) | 10 (19%) | ||
| Gender | Male | 17 (59%) | 11 (44%) | 28 (52%) | 0.212 |
| Female | 12 (41%) | 14 (56%) | 26 (48%) | ||
| Race/Ethnicity | White | 15 (52%) | 18 (72%) | 33 (61%) | 0.246 |
| African-American | 5 (17%) | 1 (4%) | 6 (11%) | ||
| Hispanic | 2 (7%) | 3 (12%) | 5 (9%) | ||
| Mixed/Other | 7 (24%) | 2 (8%) | 9 (17%) | ||
| Not collected | . | 1 (4%) | 1 (2%) | ||
| Age | 18–30 years | 18 (62%) | . | 18 (33%) | <0.001 |
| 31–39 years | 11 (38%) | . | 11 (20%) | ||
| 40–50 years | . | 15 (60%) | 15 (28%) | ||
| 51–60 years | . | 9 (36%) | 9 (17%) | ||
| 61–69 years | . | 1 (4%) | 1 (2%) | ||
| Marital Status | Married/Partnered | 10 (35%) | 7 (28%) | 17 (32%) | 0.083 |
| Divorced | 4 (14%) | 5 (20%) | 9 (17%) | ||
| Widowed | . | 2 (8%) | 2 (4%) | ||
| Separated | 1 (3%) | 5 (20%) | 6 (11%) | ||
| Never Married | 14 (48%) | 6 (24%) | 20 (37%) | ||
| Education | Less than high school | 10 (34%) | 2 (8%) | 12 (22%) | 0.096 |
| High School | 10 (35%) | 5 (20%) | 15 (28%) | ||
| graduate/GED | 2 (7%) | 6 (24%) | 8 (15%) | ||
| Some college/technical | 5 (17%) | 8 (32%) | 13 (24%) | ||
| College graduate | 2 (7%) | 3 (12%) | 5 (9%) | ||
| Graduate School | |||||
| Health Insurance | Medicare | 3 (10%) | 3 (12%) | 6 (11%) | 0.283 |
| Medicaid/Managed Care | 10 (35%) | 11 (44%) | 21 (39%) | ||
| Private | 4 (14%) | 7 (28%) | 11 (20%) | ||
| No insurance | 7 (24%) | 1 (4%) | 8 (15%) | ||
| Family Health Plus | 1 (3%) | . | 1 (2%) | ||
| Other | 4 (14%) | 3 (12%) | 7 (13%) | ||
| Household Income | Less than $5,000 | 8 (29%) | 5 (20%) | 13 (24%) | 0.487 |
| $5,000–$15,000 | 12 (43%) | 9 (36%) | 21 (39%) | ||
| $15,001–$30,000 | 4 (14%) | 7 (28%) | 11 (20%) | ||
| $30,001–$45,000 | . | 2 (8%) | 2 (3%) | ||
| $45,001–$60,000 | 2 (7%) | 1 (4%) | 3 (6%) | ||
| More than $60,000 | 2 (7%) | 1 (4%) | 3 (6%) | ||
| Not Collected | 1 (3%) | . | 1 (2%) | ||
| Employment | Full-time | 7 (24%) | 8 (32%) | 15 (28%) | 0.008 |
| Part-time | 2 (7%) | 1 (4%) | 3 (6%) | ||
| Looking for work | 11 (28%) | 4 (16%) | 15 (28%) | ||
| Unable to work/Disability | 2 (7%) | 11 (44%) | 13 (24%) | ||
| Attending school | 6 (21%) | . | 6 (11%) | ||
| Full-time homemaker | 1 (3%) | 1 (4%) | 2 (4%) | ||
| Smoker | Current | 26 (90%) | 19 (76%) | 45 (83%) | 0.165 |
| Former | 3 (10%) | 6 (24%) | 9 (17%) | ||
Results
Focus group participant characteristics
Six focus groups were conducted with a total of (n=54) community participants at least 18+ years of age and who also self-identified as a current or former smoker. Saturation of responses was achieved in both age groups across the three sites. The younger age group of 18–39 year olds accounted for about 54% (n=29) of the total number of participants. Nearly 60% of participants in the 18–39 year age group were male, while 56% were female in the 40+ years age group (p=0.21). As shown in Table 1, the majority of participants self-identified as White (61%); 50% had less than a high school education or had completed a high school diploma/GED, 39% were Medicaid recipients, and more than 60% reported a household income of $15,000 or less. These demographic parameters mirror the demographics of the county as it relates to race/ethnicity, educational attainment and socioeconomic status. Overall, 83% (n=45) of focus group participants reported being a current smoker; smoking status did not differ by age group (p=0.165). A summary of dominant focus group themes and findings by age group are listed in Table 2.
Table 2.
Dominant Focus Group Themes and Findings by Age Category
| Ages 18–39 years old | Ages 40+ years old | |
|---|---|---|
| Theme: | ||
| Quitting Smoking | • Cessation on their own “terms” -- “if I’m ready, I’ll quit” – little discussion of addiction; more about personal choice. | • We need help, no longer a personal choice --addictive properties/ illegal drug comparison; lack of control/influence on tobacco industry |
| Media/PSAs | • Impact of media & anti-smoking commercials; familiar with images, distastefulness of smoking | • Theme not expressed |
| Social Media/Internet | • Facebook, Twitter, YouTube; access- mobile phones & laptops; texting; not used for health-related purposes | • Facebook; access- mobile phones & laptops; limited texting; not used for health-related purposes |
| Automated call messaging for Quitting | • Limited experiences; familiar with automated calls from health provider and experience from political campaigns | • Limited experiences and interested in automated call, but not every day; not familiar with automated calls from health provider; but experiences from political campaigns |
| Perceptions of Tobacco Companies | •“Robbing you” and “trying to kill us”; profiting from destroying smokers’ health | • Tobacco companies and government are working together; government should protect us by regulating tobacco as a drug. |
Viewpoints on quitting smoking
The majority of participants in both the 18–39 (90%) and 40+ year old (76%) age groups identified as current smokers. The negative health outcomes associated with tobacco use were well-recognized and participants cited examples of personal experiences with tobacco-related symptoms or health problems. In particular, one person stated that: “A couple of members of my family have had lung cancer so I keep that in the back of my mind if I want a cigarette.” (18–39 years) Quitting smoking on their own terms was clearly expressed among the 18–39 year olds at all three sites. This was especially reflected in the following comments: “If people don’t want to quit, they’re not gonna quit” (18–39 years); and “I don’t want to hear it. If I’m ready to quit, I’ll quit.” (18–39 years) The former smokers, who represented 17% (n=9) of the total participant sample (n=54), discussed various aides for quitting; there were no differences by age group in the aides they discussed using to quit smoking. Former smokers discussed using hard candy, tooth picks, chewing gum, recreational drugs (i.e., marijuana, alcohol), and cessation pharmacotherapy (i.e., nicotine lozenges/patches, bupropion/Wellbutrin®, and varenicline/Chantix®) to help them quit smoking. Former smokers also discussed speaking to friends and family for support and “going cold turkey” as strategies to quit smoking, and noted that health issues (i.e., pregnancy, taking birth control, open heart surgery, at high risk for stroke) served to motivate or influence them to quit smoking. Several former smokers who tried the patch and/or varenicline/Chantix® noted experiencing uncomfortable side-effects and therefore did not find these agents to be helpful in quitting.
Addiction to nicotine and the need for support to quit smoking resonated among the 40+ year old age groups across the three sites. One participant stated that, “Heroin is easier to quit.” (40+ years) Another participant at the same site concurred and further stated that, “Nicotine is a drug that you get addicted to like you get addicted to pot or any other drug…it’s a drug so if you ban it just like meth or heroin then there you go.” Participants commented on the legality of nicotine in cigarettes versus other addictive drugs mentioned above that are considered illegal substances. The lack of community-based support groups for tobacco dependence and the perspective that tobacco was not treated the same as other drugs of dependence- specifically because of the influence of the tobacco industry were also cited by participants in the 40+ year old age groups: “You got the surgeon general out there and since they got us addicted, they should pay us to get off it.” (40+years)
In general, participants in the 40+ year old age groups discussed tobacco in terms of drug addiction and the difficulty of quitting smoking as a result of addiction to nicotine and the lack of resources to assist in quitting. Many felt that because tobacco is legal to obtain, despite the highly addictive properties of nicotine as compared to other addictive illegal drugs, resources for treating tobacco dependence are less effective, since the tobacco industry is ultimately a legal distributor of the product.
The tobacco companies’ role in smoking
Although we did not probe on topics specific to tobacco manufacturing companies the topic came up several times at site B during sessions with both age groups, which were held independently of each other. The 18–39 year olds at this site felt very strongly about quitting smoking on their own terms; however, they also felt the tobacco companies played a role in their smoking behaviors. The following statements pertain to this perspective: “How the big tobacco companies are robbing you of your money and they’re living in big mansions”; and “They’re trying to kill us.” While the participant made it clear that the decision to quit was their personal issue, they also perceived the tobacco companies as profiting from their habit and recognized smoking as something that could be detrimental to their health.
Participants in the 40+ year age group at site B discussed the tobacco companies as having government ties and felt that the government should protect citizens from tobacco. This group also discussed nicotine as highly addictive and compared it to other illicit substances that are illegal (i.e., heroin) and blamed the government for not protecting them from big tobacco companies or addiction. Some suggested banning tobacco; however, others mentioned access to cheaper price cigarettes on the “Indian Reservation.” A participant from the 40+ year age group shared, “I would go to the government and ask them why they put this out here. Other drugs people are in prison for, but you ain’t in prison for putting this poison out here. Out of everything I ever tried to quit this has been the hardest thing to get off.”
Attitudes and reactions to media and public service announcements on promoting cessation
Among the 18–39 year olds across the three sites there was consensus around having seen commercials for the NY State Smokers’ Quit Line (NYSSQ). Comments from participants on their reactions to the commercials included: “Yeah, it makes me not want to smoke again,” and, “The commercials are very disturbing.” Some discussed a specific commercial scene and their reaction to it as described here, “One that I can’t stand the most is the guy with the lung cancer breathing. I have to change the channel.” Other comments focused on the feeling a commercial elicited from them, such as, “Makes me feel guilty. I want to change the channel and finish my cigarette.” While participants in the younger age groups were generally familiar with the media campaigns and were able to share their reactions to them, the same was not found among the 40+ year olds. Identical questions were asked of both age groups at all three sites; however, there was no discussion or commentary from the older age groups on media and quit line commercials.
Behaviors and practices on the use of social media and internet
The use of the internet to access the social media site known as Facebook was common across both age groups at all three sites. In addition, accessing the internet for shopping and job hunting was also reported across all of the focus groups. The younger age groups did report use of Twitter and YouTube as well which was not mentioned among the 40+ year olds. All focus groups reported their primary modes of accessing the internet were through cell phones and laptops. The 18–39 year olds across the three sites reported greater use of texting, “Text every day and often throughout the day.” However, the frequency of texting among the 40+ year olds was described as: “Text occasionally on a sometimes daily basis.” Neither of the age groups discussed the use of the internet for health-related purposes, or in terms of accessing health information and resources.
Attitudes on use of automated calling with messages on quitting smoking
In general, the majority of participants in both age groups expressed limited receptivity to receiving automated calls with tips on quitting smoking; however, comments included: “I’m gonna listen to what they say and then hang up”; “I don’t want to hear it. If I’m ready to quit, I’ll quit.” There were some differences seen across the sites by age group, for instance there was consensus among all participants at site A with respect to a lack of interest in automated calls with messages on smoking cessation. In addition, 18–39 year olds at site B also shared this lack of interest; however, this was not the case for the 40+ year olds at that site. Comments from interested participants in the 40+ year old group at site B included: “I think it would be nice.”; “They give you a little tip in the morning like ‘don’t smoke’. I think that’s good encouragement to start the day off.” The 40+ year olds at site C expressed a non-receptive attitude toward automated calls on smoking cessation but the younger age groups at that site were receptive to the receiving the calls with a caveat regarding the frequency of calls: “It wouldn’t bother me really, I guess, just not every day.” None of the participants had previous experience with receiving automated calls for a health intervention but were familiar with automated calls from the pharmacy for filling prescriptions or during elections from political parties and candidates running for an office.
Discussion
This study reinforces many of the challenges with regard to meeting the needs of smokers living in rural as well as urban areas to achieve cessation (Mahoney, et al, 2014). There was significant variability in perceptions by age group of focus group participants which corresponds to earlier studies by this team in urban areas of New York State (Mahoney, et al, 2014). Responses from these three rural sites suggest that younger smokers (<40 years of age) continue to report less worry and less cognizance of the difficulty of “just quitting.” Possibly because they have little current interest in cessation, these smokers <40 years old have made few, if any, attempts to quit, and they do not report frustration or desire for assistance with tobacco cessation. Younger smokers reported no desire to be approached about their tobacco use within the framework of an addictive health problem which requires assistance and guidance. Rather, their responses indicated that when they are “ready,” that they plan to simply quit of their own volition (Hutcheson, et al, 2008). Conversely, the over 40 year old participants more readily recognized what Tresza and colleagues (2008) (Hutcheson, et al, 2008) characterize as the “intrinsic factors” of tobacco such as the negative health consequences and the enormous challenges of the addiction process related to tobacco use. Likewise, the smokers 40 years and older were more likely to discuss their needs for greater support and resources to quit as demonstrated in another study in Appalachian Kentucky (Kruger, et al, 2012).
This study also provided unique perspectives from current/former smokers about the perceived roles of government and “Big Tobacco” which have not been reported in other rural or Appalachian studies or expressed by participants of focus groups in urban areas of western New York State (Mahoney, et al, 2014). It is unclear why this would differ between urban and rural residents of the same state. Unlike other Appalachian residents, rural New Yorkers do not rely upon tobacco production or growing as a primary agricultural industry as other Appalachian states (e.g., Kentucky), so they may be more likely to feel victimized by these large corporations from which they receive no direct financial benefit. This may also be different for tribal members from sovereign nations in New York State who are actively involved in the promotion and sale of tobacco products in retail shops on territory which are untaxed by NYS. These particular nuances are less understood and provide an opportunity for future research.
Many of the comments from one particular location focused on participants’ perception that the government is in collusion with the tobacco industry as evidenced by the fact that companies can still promote cigarettes and addiction to nicotine while other addictive drugs remain illegal. Moreover, if businesses are actively involved in promoting nicotine as a “drug” and are not held accountable by the government (i.e., lack of regulation by the FDA) similar to laws prohibiting use of other addictive drugs (e.g., heroin), participants argued that the government should at least provide expanded resources and support for cessation. There was consensus between younger and older participants related to concerns about lack of accountability by the tobacco industry. This perspective suggests that some smokers may be more receptive to enhanced cessation resources – an important trait also identified in the Kentucky smokers (Kruger, et al, 2012) —and, like these Appalachia neighbors, may also be experiencing a similar transition from a formally pro-tobacco culture to a less tobacco-friendly environment seen in rural Appalachian regions. These signs of changing perspectives also may be an opportunity to initiate more cessation messages (Kruger, et al, 2012) focused on the exploitative role of “Big Tobacco.”
As identified by previous research, “In years past the tobacco industry used frontier images to convey the image of a ‘real’ man, who worked the land and smoked cigarettes.” It is suggested that this cultural targeting has helped to maintain the social and cultural norms of tobacco use within rural communities and significantly influencing the high rates of smoking (Behringer, et al, 2007). In rural NYS, a potential external influence with respect to increasing access to tobacco through proximity and lower cost is the availability of tax-free, 33% less expensive tobacco products on the tribal territories in Appalachian NYS. The relationship between access to low cost tobacco products from tribal territories as an external influencer for promoting or enabling higher rural smoking rates in these geographic areas is also unclear. The findings from this study demonstrate frustration and anger toward the corporate role of Big Tobacco in tobacco addiction. In addition, the consequent lack of government control of tobacco products suggest that the impact of state and national policy, as well as legislative changes accompanied by widespread media about the role of the tobacco industry in promoting a practice that was known to have negative health effects may be changing the social norms regarding tobacco use and attitudes toward cessation. The positive attitudes reported by participants (especially for older smokers, 40+ yrs.) toward assistance for cessation from multiple sources suggest the potential for interventions in the form of telephone counseling, internet or e-mail based programs (Hutcheson, et al, 2008).
The findings from this qualitative study may not be generalizable to all current and former smokers residing in rural and non-rural Appalachian communities. For example, residents who participated in these focus groups from this rural region of northern Appalachia live within close proximity to a tribal territory that markets and sells various tobacco products free of state taxes at much lower prices compared to other areas within Appalachia, possibly limiting generalizability.
The findings from this study add both novel and important information about the beliefs, attitudes, and experiences of current and formers smokers residing in an understudied area of northern Appalachia. Current and former smokers from different age groups described distinct interest in and challenges with quitting smoking, and reported their experiences with, access to, and receptivity to various forms of social media and technology as related to smoking cessation intervention approaches. Future studies should further explore the application of innovative smoking cessation interventions within Appalachian communities that make use of social media and other novel technologies. By better understanding the perspectives of current and former smokers in this region of Appalachia, we hope to improve access to relevant and feasible cessation interventions which can help to achieve an improved health status among this underserved and at-risk population.
Acknowledgements
The authors acknowledge the assistance of Susan Lindner in transcribing the audiotapes from these focus group sessions and support from our community partners and focus group participants in the Southern Tier region of New York State.
Financial Support: This study was supported in part by the Western New York Cancer Coalition (WNYC2) Center to Reduce Disparities grant: NIH/NCI/CRCHD U54CA153598-01.
Footnotes
Portions of this data were presented as a poster at the September 2013 International Cancer Education Conference for the American Association for Cancer Education (AACE) in Seattle, WA.
Conflict of Interest:
The authors declare that they have no conflict of interest.
Contributor Information
Elisa M. Rodriguez, Email: Elisa.rodriguez@roswellpark.org, Epidemiology and Prevention, Roswell Park Cancer Institute, Cancer Prevention and Population Sciences, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-5953, Fax: 716-845-8487.
Annamaria Masucci Twarozek, Roswell Park Cancer Institute, Department of Health Behavior, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-4969.
Deborah Erwin, Office of Cancer Health Disparities Research, Roswell Park Cancer Institute, Cancer Prevention and Population Sciences, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-2927.
Christy Widman, Roswell Park Cancer Institute, Cancer Prevention and Population Sciences, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-5814.
Frances G. Saad-Harfouche, Roswell Park Cancer Institute, Cancer Prevention and Population Sciences, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-4887.
Chester H. Fox, Family Medicine, State University of New York at Buffalo, Department of Family Medicine, 240 Goodell Street, Buffalo, New York 14208, Phone: 716-816-7282.
Willie Underwood, Roswell Park Cancer Institute, Cancer Prevention and Population Sciences, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-4050.
Martin C. Mahoney, Oncology, Roswell Park Cancer Institute, Department of Health Behavior, Elm & Carlton Streets, Buffalo, New York 14263, Phone: 716-845-3597.
References
- Behringer B, Friedell GH, Dorgan KA, Hutson SP, Naney C, Phillips A, Krishnan K, Cantrell ES. Understanding the challenges of reducing cancer in Appalachia: addressing a place-based health disparity population. Californian Journal of Health Promotion. 2007;5:40–49. [Google Scholar]
- Butler KM, Hedgecock S, Record RA, Derifield S, McGinn C, Murray D, Hahn EJ. An evidence-based cessation strategy using rural smokers’ experiences with tobacco. 2012;47:31–43. doi: 10.1016/j.cnur.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), Centers for Disease Control and Prevention (CDC) Atlanta, Georgia: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2011. Behavioral Risk Factor Surveillance System Survey. BRFSS. [Google Scholar]
- Chautauqua County Health Network. Health care workforce development. 2014 [Google Scholar]
- Dino GA, Pignataro RM, Horn KA, Anesetti-Rothermel A. Tobacco use in rural populations. In: Crosby RA, Wendel ML, Vanderpool RC, Casey BR, editors. Rural Population and Health: Determinants, Disparities, and Solutions. Jossey-Bass; 2012. pp. 357–376. [Google Scholar]
- Division, Appalachian Regional Commission Regional Planning and Research. Economic Overview of Appalachia. 2011 [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Flint KH, Hawkins J, Harris WA, Lowry R, McManus T, Chyen D, Whittle L, Lim C, Wechsler H Centers for Disease Control and Prevention (CDC) Morbidity and mortality weekly report. Surveillance summaries. Vol. 61. Washington, D.C.: 2012. Youth risk behavior surveillance - United States, 2011; pp. 1–162. 2002 doi: ss6104a1 [pii]. [PubMed] [Google Scholar]
- Hutcheson TD, Greiner KA, Ellerbeck EF, Jeffries SK, Mussulman LM, Casey GN. Understanding smoking cessation in rural communities. 2008;24:116–124. doi: 10.1111/j.1748-0361.2008.00147.x. [DOI] [PubMed] [Google Scholar]
- Kruger TM, Howell BM, Haney A, Davis RE, Fields N, Schoenberg NE. Perceptions of smoking cessation programs in rural Appalachia. 2012;36:373. doi: 10.5993/AJHB.36.3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney MC, Erwin DO, Widman C, Masucci Twarozek A, Saad-Harfouche FG, Underwood W, 3rd, Fox CH. Formative evaluation of a practice-based smoking cessation program for diverse populations. Health education & behavior : the official publication of the Society for Public Health Education. 2014;41:186–196. doi: 10.1177/1090198113504415. [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer MG, Toborg MA, Denham SA, Mande MJ. Cultural perspectives concerning adolescent use of tobacco and alcohol in the Appalachian mountain region. The Journal of Rural Health. 2008;24:67–74. doi: 10.1111/j.1748-0361.2008.00139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York State Department of Health. New york state expanded behavioral risk factor surveillance system. 2009 [Google Scholar]
- Northridge ME, Vallone D, Xiao H, Green M, Blackwood JW, Kemper SE, Duke J, Watson KA, Burrus B, Treadwell HM. The importance of location for tobacco cessation: Rural-urban disparities in quit success in underserved West Virginia counties. 2008;24:106–115. doi: 10.1111/j.1748-0361.2008.00146.x. [DOI] [PubMed] [Google Scholar]
- Orzechowski W, Walker R. The tax burden on tobacco. Historical compilation 39. PDA, Inc., and the Cecil B. Sheps Center for Health Services Research, 2012. Health care costs and access disparities in appalachia. 2008 [Google Scholar]
- Schoenberg NE, Bundy HE, Bispo JAB, Studts CR, Shelton BJ, Fields N. A Rural Appalachian Faith-Placed Smoking Cessation Intervention. Journal of religion and health. 2014:1–14. doi: 10.1007/s10943-014-9858-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sudarsan NR, Jandorf L, Erwin DO. Multi-site implementation of health education programs for Latinas. Journal of Community Health. 2011;36:193. doi: 10.1007/s10900-010-9297-7. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau. 2008–2012 American community survey 5-year estimates. 2012 [Google Scholar]
- US Census Bureau. State and county quick facts: American community survey, census population and housing estimates, county business patterns, nonemployer statistics, economic census, survey of business owners, building permits. 2014 [Google Scholar]