Abstract
Background:
Previous authors have suggested that intra-articular morphine and clonidine injections after knee arthroscopy have demonstrated equivocal analgesic effect in comparison with bupivacaine while circumventing the issue of chondrotoxicity. There have been no studies evaluating the effect of intra-articular morphine after hip arthroscopy.
Purpose:
To evaluate the efficacy of intra-articular morphine in combination with clonidine on postoperative pain and narcotic consumption after hip arthroscopy surgery for femoroacetabular impingement.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A retrospective chart review was performed on 43 patients that underwent hip arthroscopy for femoroacetabular impingement at a single institution between September 2014 and May 2015. All patients received preoperative celecoxib and acetaminophen, and 22 patients received an additional intra-articular injection of 10 mg morphine and 100 μg of clonidine at the conclusion of the procedure. Narcotic consumption, duration of anesthesia recovery, and perioperative pain scores were compared between the 2 groups.
Results:
Patients who received intra-articular morphine and clonidine used significantly less opioid analgesic (mEq) in the postanesthesia recovery (median difference, 17 mEq [95% CI, –32 to –2 mEq]; P = .02) compared with the control group. There were no differences in time spent in recovery before hospital discharge or in visual analog pain scores recorded immediately postoperatively and at 1 hour after surgery.
Conclusion:
Intraoperative intra-articular injection of morphine and clonidine significantly reduced the narcotic requirement during the postsurgical recovery period after hip arthroscopy. The reduction in postsurgical opioids may decrease adverse effects, improve overall pain management, and lead to better quality of recovery and improved patient satisfaction.
Keywords: hip arthroscopy, femoroacetabular impingement intra-articular injection, pain management
Hip arthroscopy has become increasingly more prevalent as a safe and effective means for treating a variety of conditions such as labral tears and femoroacetabular impingement (FAI).1 There was a 365% increase in the rate of hip arthroscopy from 2004 to 2009, with the majority of cases being performed for patients aged 20 to 39 years.18 The majority of these procedures are performed in an outpatient surgery setting. While improvements in imaging technology and surgical instrumentation have accelerated the implementation of arthroscopic hip surgery, literature is lacking with regard to a gold standard for postoperative pain management, especially when compared with knee and shoulder arthroscopy. The use of a nerve block after shoulder or knee arthroscopy is relatively common place; however, given the complex anatomy and innervation of the hip joint, it is uncommon to use nerve blocks in the perioperative period after hip arthroscopy. There are numerous studies demonstrating successful outcomes with decreased morbidity and postoperative complications compared with open procedures; however, pain remains one of the major causes of patient dissatisfaction after arthroscopic hip surgery in the immediate perioperative period.26 The overall goals to improve postoperative pain include improved patient comfort, earlier mobilization of the hip joint, and decreased opioid consumption with the possibility of overall reduction in cost of care.19
The use of intra-articular (IA) morphine injections for postoperative pain is controversial; however, it has been utilized in patients undergoing knee arthroscopy for over 2 decades.20,25,27 Morphine is known to act on the μ-opioid receptors in the central nervous system as well as the gastrointestinal tract. There are more recent studies to suggest that there are opioid receptors within chondrocytes located in various joints peripherally within the body, explaining the potential efficacy of IA morphine injections.7 Additionally, the use of clonidine, an α2 agonist, has been shown to potentiate the anti-nociceptive effects of morphine for pain control.11 Recent studies have also demonstrated the chondrotoxic properties of traditional anesthetics such as bupivacaine and lidocaine, favoring the use of safer alternatives, such as morphine.2,5,22 Despite its utilization in orthopaedic surgery, a recent systematic review raised questions about the efficacy of IA morphine when used for analgesia after arthroscopy.9 To our knowledge, there is no literature investigating the use of IA injections of morphine with clonidine for postoperative analgesia in arthroscopic hip surgery.12 The purpose of this study was to evaluate the efficacy of IA morphine in combination with clonidine on perioperative pain and narcotic consumption after hip arthroscopy surgery for FAI. We hypothesized that patients who received an IA injection of morphine and clonidine would have lower pain scores and reduced opioid consumption in the perioperative recovery period.
Methods
After approval from our institutional review board, we retrospectively reviewed the 88 patients who had undergone primary unilateral hip arthroscopy for FAI between September 2014 and May 2015 by a single surgeon at our institution. While all patients underwent labral debridement and repair along with acetabular osteoplasty, some of these patients underwent additional concomitant procedures (eg, chondroplasty, iliotibial band windowing, iliopsoas lengthening) (Table 1). All concomitant procedures were performed arthroscopically after central compartment work with the aid of an extracapsular fourth portal located at the distal anterolateral position.
TABLE 1.
Patient Demographics and Characteristics of Surgery and Discharge Timesa
| Control Group (n = 21) | IA Group (n = 22) | P | |
|---|---|---|---|
| Age, y | 34 (23-43) | 38 (32-45) | .25 |
| Sex, n (%) | |||
| Male | 6 (27) | 7 (33) | .75 |
| Female | 16 (73) | 14 (67) | .86 |
| Smoker, n (%) | |||
| No | 20 (91) | 18 (86) | .9 |
| Yes | 2 (9) | 3 (14) | .64 |
| Height, in | 170 (165-173) | 175 (165-178) | .24 |
| Weight, lbs | 65 (59-80) | 73 (63-85) | .10 |
| Surgical duration, min | 31 (27-40) | 36 (34-47) | .08 |
| Concomitant procedure, nb | |||
| Iliopsoas lengthening | 5 | 7 | .56 |
| Iliotibial band windowing/trochanteric bursectomy | 5 | 4 | .65 |
| Chondroplasty | 4 | 4 | .94 |
| Loose body removal | 2 | 0 | .14 |
| No additional procedure | 5 | 7 | .56 |
| Time from operating room discharge, min | |||
| To ready for discharge from hospital | 133 (108-160) | 134 (123-169) | .56 |
| To actual discharge from hospital | 172 (143-183) | 161 (138-189) | .83 |
aData are presented as median (interquartile range) unless otherwise indicated. IA, intra-articular.
bPatients could have undergone >1 procedure.
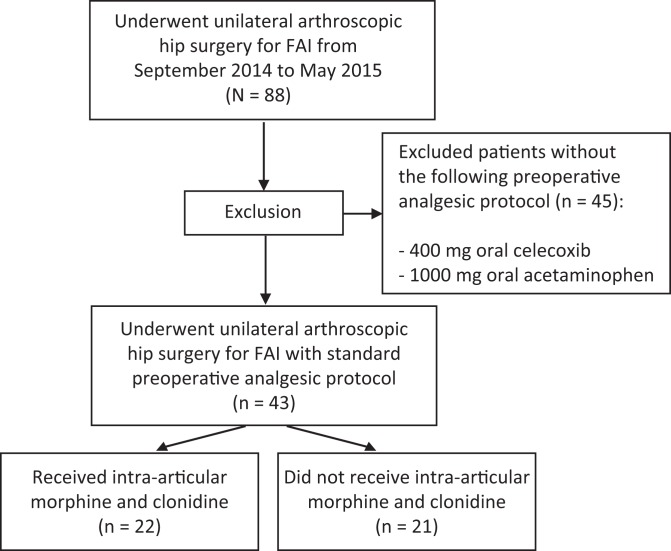
The cohort of 88 patients was screened to consist of only patients undergoing a standard preoperative pain treatment protocol. The standard preoperative pain regimen consisted of 400 mg celecoxib and 1000 mg acetaminophen, both orally, which is given to all patients 1 hour before their scheduled time of surgery. After screening, 43 patients remained (Figure 1). The control group of 21 patients received no additional intervention beyond the standard of care. In addition to the standard of care, the study group of 22 patients received an intraoperative IA injection of 10 mg morphine and 100 μg clonidine under visualization through the anterior portal at the conclusion of the arthroscopic procedure but before removing the hip from traction to ensure precise placement within the hip joint. The dosage of 10 mg morphine and 100 μg clonidine was chosen based on previous literature demonstrating the effectiveness of such doses for postoperative pain management in arthroscopic knee surgery while also considering the larger size of the hip joint as compared with the knee.3,6,8
Figure 1.
Subject selection criteria. FAI, femoroacetabular impingement.
The IA injection of morphine and clonidine was instituted in December 2014. All patients after December 2014 were eligible for the IA injection if they had no contraindications or enrollment in another study that prohibited a change in standard anesthesia protocol (ie, IA injection). Patients after December 2014 not eligible for the injection were still eligible for the control group. As part of the standard anesthesia protocol, all patients received 4 mg intravenous ondansetron intraoperatively as antinausea prophylaxis. The treatment protocols between the control and study groups were identical with the exception of the intraoperative IA injection.
Postoperative pain control protocols were the same between both groups and consisted of intravenous medication (fentanyl, hydromorphone, meperidine) as needed for breakthrough pain as well as oral opioids for longer term relief (hydromorphone, hydrocodone/acetaminophen). All postoperative medications were administered on an as-needed basis. Opioid consumption during the postoperative period was measured in terms of morphine equivalents, which were calculated using the analgesic-specific conversion factor from http://www.globalrph.com/narcotic.cgi.16 For example, a nontolerant subject taking 1 tablet orally of 10 mg hydrocodone would be equivalent to 10 oral morphine equivalents (mEq) (50 μg fentanyl = 15 mEq; 5 mg oxycodone = 7.5 mEq). Pain levels were recorded by the nursing staff using a visual analog scale (VAS) ranging from 0 to 10 (0 = no pain, 10 = worst pain possible). Pain scores were recorded before surgery, entering the postanesthesia recovery area, and 1 hour postsurgery.
The primary outcome variable was opioid consumption in the postsurgical recovery period and was compared between groups using the Mann-Whitney U test, which compares median values. Data are reported as point estimates and interquartile ranges (IQRs). Interval data (age, VAS pain scores, time out of the operating room to ready for discharge from hospital, time out of the operating room to actual discharge from hospital) were compared using the Mann-Whitney U test. Categorical data (sex, smoker) was evaluated using the Pearson chi-square test. Median difference and 95% CI of the difference were calculated using 10,000 bootstrap samples. Statistical analysis was performed using STATA version 11.2 (STATA Corp). All tests were 2-sided, and a P < .05 was required to reject the null hypothesis.
Results
The demographic characteristics were similar in the 2 groups (Table 1). All patients underwent labral repair with acetabular osteoplasty as a primary procedure, and there was no difference between groups in the types of concomitant procedures for FAI. The senior surgeon (M.A.T.) did not perform interportal capsulotomies or T-capsulotomies, as osteoplasty only focused on the central compartment. Additionally, no femoral-sided or cam-lesion decompression was performed for any of the patients. The median difference in surgery duration between the control and study groups was 5 minutes (95% CI, –14 to 2.5 minutes; P = .08).
Median analgesic consumption during the intraoperative period was 61 mEq (IQR, 52-69 mEq) in the patients who received an IA injection and 50 mEq (IQR, 48-72 mEq) in patients who did not (difference, 11 mEq [95% CI, –10.5 to 17 mEq]; P = .32). During the postoperative period, patients who received IA injection of morphine and clonidine used significantly lower amounts of opioids in the postanesthesia recovery area (23 mEq; range, 16-38 mEq) compared with the patients in the control group (40 mEq; range, 28-60 mEq) (median difference, –17 mEq [95% CI, –32 to –2 mEq]; P = .02) (Table 2).
TABLE 2.
Opioid Consumption and Pain Scores During the Perioperative Perioda
| Control Group (n = 21) | IA Group (n = 22) | P | |
|---|---|---|---|
| Opioid use, mEq | |||
| Intraoperative | 50 (48-72) | 61 (52-69) | .32 |
| Postsurgical recovery | 40 (28-60) | 23 (16-38) | .02 |
| Perioperative painb | |||
| Preoperative | 0 (0-3) | 2 (0-3) | .43 |
| Entering postsurgical care unit | 6 (2-8) | 5 (2-7) | .71 |
| 1 hour postsurgery | 5 (4-6) | 4 (4-7) | .25 |
aData are presented as median (interquartile range). IA, intra-articular.
bMeasured using visual analog scale score (range, 0-10).
The median VAS score reported during the preoperative period was 2 (range, 0-3) in patients who received the IA injection compared with 0 (range, 0-3) in the control group (median difference, 2 [95% CI, –1 to 2]; P = .43). On entering the postsurgical recovery area, patients in the IA group had a median VAS pain rating score of 5 (range, 2-7) versus patients in the control group with a score of 6 (range, 2-8) (median difference, –1 [95% CI, –4 to 3]; P = .71). One hour postsurgery, patients in the IA group had a VAS pain rating score of 4 (range, 4-7) as compared with the control group with a score of 5 (range, 4-6) (median difference, 1 [95% CI, 0-2]; P = .25).
The median (IQR) duration from operating room discharge until time ready for hospital discharge was 134 minutes (range, 112-163 minutes) and was not different between those who received IA morphine and clonidine with those who did not (median difference, –1 [95% CI, –35 to 24]; P = .56). The median time until actual discharge was 161 minutes (range, 138-189 minutes) in the injection group and 172 minutes (range, 143-183 minutes) in the control group (median difference, –11 [95% CI, –18 to 40]; P = .83).
Discussion
Hip arthroscopy is mostly performed in the outpatient setting, and thus, there has been a greater focus on perioperative pain management with efforts to reduce pain in the acute postoperative period. Increased pain and narcotic consumption can affect patient satisfaction, quality of recovery, and time to discharge from outpatient surgery centers.4 In this study, we found that an IA injection of morphine and clonidine significantly reduced the amount of opioid required for patients recovering in the postanesthesia recovery area after outpatient hip arthroscopy. The difference of 17 mEq translates to a minimum of two 10-mg hydrocodone tablets or one 1-mg hydromorphone tablet. This is very important in that decreasing the amount of opioid consumption may result in less postoperative side effects (eg, nausea, vomiting, drowsiness, confusion) and will improve postoperative recovery. It has previously been demonstrated that surgical patients who consumed less opioids reported better postoperative quality of recovery.4
Despite the advancement of hip arthroscopy techniques in the past decade, postoperative pain control remains a considerable challenge.14,26 A study of 10,000 consecutive outpatient surgeries demonstrated that orthopaedic surgery procedures had the highest incidence of postoperative pain among surgical subspecialties.23 Previous studies have evaluated multimodal pain management in an effort to improve pain management and to reduce opioid consumption. Nonsteroidal anti-inflammatories such as celecoxib have been studied in the setting of hip arthroscopy surgery and been found to be effective in reducing narcotic consumption in the outpatient setting.26
Intra-articular injection of morphine, clonidine, and ketorolac has been shown to improve postoperative analgesia and reduce opioid consumption after knee arthroscopy. Stein et al21 demonstrated that IA morphine results in substantial lower plasma levels compared with intravenous injection, which may explain the enhanced postoperative analgesia without an increase in systemic side effects. Elkousy et al6 found that 10 mg of morphine injected after knee arthroscopy was as effective as bupivacaine while circumventing the concerns of chondrotoxicity from bupivacaine. Although many studies have found that IA morphine is beneficial after knee arthroscopy, a systematic review has raised questions about the overall efficacy of morphine when used in combination with arthroscopy.9,24 No study has examined the effect of IA morphine and clonidine after hip arthroscopy.
Morphine is known to act on the μ-opioid receptor with high sensitivities in the brain and gastrointestinal tract; however, newer studies suggest that there are opioid receptors within chondrocytes located in the various joints peripherally within the body.10 Mouse models have also shown us that clonidine potentiates morphine antinociceptive activity 5-fold, and thus, has been utilized in conjunction with IA morphine in multiple studies involving knee arthroscopy.11
Although the group that received IA morphine and clonidine had decreased opioid requirements in the postsurgical recovery period, there was very little difference in time spent in recovery after discharge. No significant difference was seen between groups with regard to time until actual discharge or time until the patient was ready for discharge. The lack of difference in recovery room time is not that surprising as the study was a retrospective evaluation of clinical practice, and discharge criteria are often dependent on institutional practices.
The discrepancy between reduced opioid consumption in the study group despite similar VAS pain scores may be a result of the subjective nature of patient pain measurements in a clinical setting.17 There was also no statistically significant difference between immediate postoperative and 1-hour postoperative VAS scores for patients in either the control or the study group. This may also be due to the subjectivity and variability of pain tolerance among patients. Whereas VAS scores measure a subjective representation of patient-perceived pain, narcotic consumption measures the objective intervention for pain management as sought by the patient and assessed by a nurse or anesthesiologist. Our data do support further investigation of the role of IA morphine and clonidine in multimodal pain and recovery management after hip arthroscopy.
The lack of opioid-related side effects after IA injection was notable. The systemic administration of opioids to patients for pain relief is limited by adverse effects such as nausea, vomiting, pruritus, and respiratory depression. No intraoperative or postoperative complications directly related to the IA injection in the study group were observed. There were no intraoperative or postoperative complications of any sort in the control group. One patient in the study group with a previous history of chronic back pain and narcotic use (hydrocodone) was admitted to the hospital for postoperative pain.
There are many potential benefits to use of IA morphine and clonidine for hip arthroscopy. Similar to findings of local opioid receptors within the synovial lining of the knee,10,15 activation of the local opioid receptors within the hip joint may be providing effective analgesia while circumventing the issue of systemic opioid toxicity. Recent studies have shown that the risk of respiratory depression due to postoperative systemic opioid administration ranges from 0.1% to 37%, and decreasing systemic opioid exposure will help decrease such postoperative complications.13 Longer term follow-up is still needed to determine patient recovery and narcotic usage in the days to weeks after surgery.
Limitations
Our study should only be interpreted with respect to its limitations. The study design was retrospective, our study population is relatively small, and follow-up assessments were not based on specific criteria. Because of the retrospective study design, selection of subjects to receive the IA injection was not by random allocation, and staff were not blinded to the treatment received by each patient. Opioid analgesia consumption and VAS scores were only collected during the immediate postoperative period, and collection of this information over a longer period of time would allow for an evaluation of the benefit beyond the immediate postsurgical period. Therefore, the scope of this study is limited only to the impact of the morphine and clonidine injection on decreasing opioid medication usage in the immediate postoperative period. With regard to VAS measurement, we were limited to collecting only preoperative, postoperative, and 1-hour postoperative scores because VAS scores were collected irregularly based on nurse availability and variable recovery times for patients. We utilized a single combination of morphine and clonidine, so the optimal dose of the agents either alone or in combination cannot be ascertained. Our data support the need for a prospective study to support a more conclusive analysis.
Conclusion
Intraoperative intra-articular injection of morphine and clonidine significantly reduced the narcotic requirement during the postsurgical recovery period after hip arthroscopy. The reduction in postsurgical opioids may decrease adverse effects, improve overall pain management, and lead to better quality of recovery and improved patient satisfaction.
References
- 1. Baker J, Byrne D, Hunter K, Mulhall K. Post-operative opiate requirements after hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2010;19:1399–1402. [DOI] [PubMed] [Google Scholar]
- 2. Baker J, McGuire C, Byrne D, Hunter K, Eustace N, Mulhall K. Analgesic control after hip arthroscopy: a randomised, double-blinded trial comparing portal with intra-articular infiltration of bupivacaine. Hip Int. 2011;21:373–377. [DOI] [PubMed] [Google Scholar]
- 3. Cepeda MS, Uribe C, Betancourt J, et al. Pain relief after knee arthroscopy: intra-articular morphine, intra-articular bupivacaine, or subcutaneous morphine? Reg Anesth. 1997;22:233–238. [DOI] [PubMed] [Google Scholar]
- 4. De Oliveira GS, Fitzgerald P, Streicher LF, Marcus RJ, McCarthy RJ. Systemic lidocaine to improve postoperative quality of recovery after ambulatory laparoscopic surgery. Anesth Analg. 2012;115:262–267. [DOI] [PubMed] [Google Scholar]
- 5. Dragoo J, Braun H, Kim H, Phan H, Golish S. The in vitro chondrotoxicity of single-dose local anesthetics. Am J Sports Med. 2012;40:794–799. [DOI] [PubMed] [Google Scholar]
- 6. Elkousy H, Kannan V, Calder CT, Zumwalt J, O’Connor DP, Woods GW. Intra-articular morphine versus bupivicaine for postoperative pain management. Orthopedics. 2013;36:1121–1127. [DOI] [PubMed] [Google Scholar]
- 7. Elvenes J, Andjelkov N, Figenschau Y, Seternes T, Bjørkøy G, Johansen O. Expression of functional mu-opioid receptors in human osteoarthritic cartilage and chondrocytes. Biochem Biophys Res Commun. 2003;311:202–207. [DOI] [PubMed] [Google Scholar]
- 8. Gentili M, Enel D, Szymskiewicz O, Mansour F, Bonnet F. Postoperative analgesia by intraarticular clonidine and neostigmine in patients undergoing knee arthroscopy. Reg Anesth Pain Med. 2001;26:342–347. [DOI] [PubMed] [Google Scholar]
- 9. Gupta A, Bodin L, Holmström B, Berggren L. A systematic review of the peripheral analgesic effects of intraarticular morphine. Anesth Analg. 2001;93:761–770. [DOI] [PubMed] [Google Scholar]
- 10. Jaureguito J, Wilcox J, Thisted R, Phillips C, Cunningham B, Reider B. The effects of morphine on human articular cartilage of the knee: an in vitro study. Arthroscopy. 2002;18:631–636. [DOI] [PubMed] [Google Scholar]
- 11. Joshi W, Reuben S, Kilaru P, Sklar J, Maciolek H. Postoperative analgesia for outpatient arthroscopic knee surgery with intraarticular clonidine and/or morphine. Anesth Analg. 2000;90:1102–1106. [DOI] [PubMed] [Google Scholar]
- 12. Lavelle W, Lavelle E, Lavelle L. Intra-articular injections. Anesthesiol Clin. 2007;25:853–862. [DOI] [PubMed] [Google Scholar]
- 13. Lee L, Caplan R, Stephens L, et al. Postoperative opioid-induced respiratory depression. Anesthesiology. 2015;122:659–665. [DOI] [PubMed] [Google Scholar]
- 14. Lee E, Murphy K, Ben-David B. Postoperative analgesia for hip arthroscopy: combined L1 and L2 paravertebral blocks. J Clin Anesth. 2008;20:462–465. [DOI] [PubMed] [Google Scholar]
- 15. Marchal JM, Delgado-Martinez AD, Poncela M, Valenzuela J, de Dios Luna J. Does the type of arthroscopic surgery modify the analgesic effect of intraarticular morphine and bupivacaine? A preliminary study. Clin J Pain. 2003;19:240–246. [DOI] [PubMed] [Google Scholar]
- 16. McAuley D. Clinicians ultimate guide to drug therapy. Globalrph.com. 2015. http://globalrph.com. Accessed June 8, 2015.
- 17. McCarthy RJ, De Oliveira GS. The trouble with using provider assessments for rating clinical performance: it’s a matter of bias. Anesth Analg. 2015;120:714–716. [DOI] [PubMed] [Google Scholar]
- 18. Montgomery S, Ngo S, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29:661–665. [DOI] [PubMed] [Google Scholar]
- 19. Ramsay MA. Acute postoperative pain management. Proc (Bayl Univ Med Cent). 2000;13:244–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Stein C, Comisel K, Haimerl E, et al. Analgesic effect of intraarticular morphine after arthroscopic knee surgery. N Engl J Med. 1991;16:1123–1126. [DOI] [PubMed] [Google Scholar]
- 21. Stein A, Yassouridis A, Szopko C, Helmke K, Stein C. Intraarticular morphine versus dexamethasone in chronic arthritis. Pain. 1999;83:525–532. [DOI] [PubMed] [Google Scholar]
- 22. Stueber T, Karsten J, Stoetzer C, Leffler A. Differential cytotoxic properties of drugs used for intra-articular injection on human chondrocytes: an experimental in-vitro study. Eur J Anaesthesiol. 2014;31:640–645. [DOI] [PubMed] [Google Scholar]
- 23. Ward J, Albert D, Altman R, Goldstein R, Cuff G, Youm T. Are femoral nerve blocks effective for early postoperative pain management after hip arthroscopy? Arthroscopy. 2012;28:1064–1069. [DOI] [PubMed] [Google Scholar]
- 24. Wei J, Lei GH, Gao SG, et al. Single-dose intra-articular bupivacaine versus morphine after arthroscopic knee surgery: a meta-analysis of randomized-controlled studies. Clin J Pain. 2014;30:630–638. [DOI] [PubMed] [Google Scholar]
- 25. Yari M, Saeb M, Golfam P, Makhloogh Z. Analgesic efficacy of intra-articular morphine after arthroscopic knee surgery in sport injury patients. J Inj Violence Res. 2013;5:84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Zhang Z, Zhu W, Zhu L, Du Y. Efficacy of celecoxib for pain management after arthroscopic surgery of hip: a prospective randomized placebo-controlled study. Eur J Orthop Surg Traumatol. 2013;24:919–923. [DOI] [PubMed] [Google Scholar]
- 27. Zeng C, Gao SG, Cheng L, et al. Single-dose intra-articular morphine after arthroscopic knee surgery: a meta-analysis of randomized placebo-controlled studies. Arthroscopy. 2013;29:1450–1458.e2. [DOI] [PubMed] [Google Scholar]