Abstract
Married couples might be an appropriate target for obesity prevention interventions. In the present study, we aimed to evaluate whether an individual's risk of obesity is associated with spousal risk of obesity and whether an individual's change in body mass index (BMI; weight in kilograms divided by height in meters squared) is associated with spousal BMI change. We analyzed data from 3,889 spouse pairs in the Atherosclerosis Risk in Communities Study cohort who were sampled at ages 45–65 years from 1986 to 1989 and followed for up to 25 years. We estimated hazard ratios for incident obesity by whether spouses remained nonobese, became obese, remained obese, or became nonobese. We estimated the association of participants' BMI changes with concurrent spousal BMI changes using linear mixed models. Analyses were stratified by sex. At baseline, 22.6% of men and 24.7% of women were obese. Nonobese participants whose spouses became obese were more likely to become obese themselves (for men, hazard ratio = 1.78, 95% confidence interval: 1.30, 2.43; for women, hazard ratio = 1.89, 95% confidence interval: 1.39, 2.57). With each 1-unit increase in spousal BMI change, women's BMI change increased by 0.15 (95% confidence interval: 0.13, 0.18) and men's BMI change increased by 0.10 (95% confidence interval: 0.09, 0.12). Having a spouse become obese nearly doubles one's risk of becoming obese. Future research should consider exploring the efficacy of obesity prevention interventions in couples.
Keywords: change, cohort study, obesity, spouses
Almost 50% of US adults are married (1), but little public health research has been done in which couples were considered as a unit. Studies have shown that spouses are likely to share both health outcomes (2) and health behaviors (3). Further, the behavior of one spouse might influence the behavior of the other (4, 5), which suggests that the pair may be a natural unit of intervention.
Obesity is a major public health problem in the United States that affects 35% of adults (6) and is responsible for more than 100,000 deaths annually (7). The obesity epidemic is thought by many to be partly due to changes in the human environment that make it easier to eat more and exercise less (8); the impact of individual interventions has been modest at best (9).
A largely cross-sectional body of literature has shown that body mass indices (BMIs) in spouses are positively correlated and that obese individuals are more likely to have obese spouses (10–12). One reason for similar BMIs within couples is the propensity, particularly among the obese, to marry people of a similar size (13). Limited longitudinal evidence has shown positive associations between BMI changes in spouses (14–16) and between changes in weight status in spouses (17), which suggests that spousal similarities might also be driven by the impact of living in a shared obesogenic environment and by the influence of one spouse on the other. In fact, couples who cohabitate for longer periods of time are more likely to show concordance in behaviors related to obesity, such as low levels of physical activity and high levels of sedentary behavior (18). There is also mixed longitudinal evidence for the association of weight status changes among peers (17, 19). However, longitudinal studies in spouses to date have been focused largely on white populations and have had limited follow-up or small sample sizes (14, 16, 17). Further, previous studies have not accounted for potential confounding by individual and spousal characteristics nor evaluated potential modification by behavioral factors such as dietary intake, physical activity level, and smoking status (20).
Using data from 3,889 spouse pairs who enrolled in the Atherosclerosis Risk in Communities (ARIC) Study and followed for up to 25 years, we examined associations between BMI and obesity status change among spouse pairs. We hypothesized 1) that individuals whose spouses became obese would be more likely to become obese themselves and 2) that a BMI change in an individual would be associated with a concurrent BMI change in their spouse. Furthermore, this association would be symmetrical by sex and possibly stronger at older ages and among white spouse pairs and those who shared behaviors known to affect weight (diet, physical activity level, smoking status). Finally, we hypothesized that controlling for potential risk factors for obesity would lessen the association of BMI changes between spouses.
METHODS
Study population
The ARIC Study, a population-based cohort study, recruited 15,792 individuals from 4 communities in the United States (Minneapolis, Minnesota; Washington County, Maryland; Jackson, Mississippi; and Forsyth County, North Carolina) between 1987 and 1989. After the baseline visit (visit 1), there were 3 initial follow-up visits (visits 2–4) that occurred approximately 3 years apart. A fifth visit was conducted between 2011 and 2013 (12 years after visit 4). Study details have been published previously (21).
Identification of spouse pairs in the ARIC Study has been previously described (2). Either participants identified another ARIC Study participant in their household as their spouse during the initial interview or (less commonly) exactly 2 married adult ARIC Study participants lived in the household, for a total 4,505 spouse pairs at baseline. Data on ARIC Study spouse pairs were limited to married couples. We excluded participants of ethnicities other than black or white because of their small sample sizes (n = 24 pairs). If either member of the couple reported being divorced or separated after baseline, the pair was excluded from that time forward (n = 120 pairs). We included pairs for a specific visit only if both members attended and had complete data (see Appendix Table 1 for data on attrition). Analyses of BMI change were limited to 3,889 spouse pairs (n = 7,778 participants) with measured BMI available for at least 2 visits. Analyses of incident obesity in men were limited to the 2,990 men who were not obese at baseline and their spouses; in women, they were limited to the 2,913 women who were not obese at baseline and their spouses.
Exposures, outcomes, and risk factors
BMI was calculated at each visit by dividing measured weight (in kilograms) by measured height (in meters) squared. For the analyses of BMI change, the main outcome of interest was a participant's BMI change from one visit to the next. The main exposure was his or her spouse's concurrent BMI change. For the analyses of incident obesity, an event was defined as a nonobese participant becoming obese between one visit and the next. Obesity was chosen as the event of interest because it is a clinically important outcome. The main exposure was the concurrent change in spousal obesity status: spouse remained nonobese, spouse became obese, spouse remained obese, or spouse became nonobese. Participants with a BMI ≥ 30 were considered obese.
Age, race, educational level, and BMI at 25 years of age were self-reported at baseline and were not time-varying. All other covariates were time-varying. Variables were updated at each visit unless specified below. For variables that were not measured at a particular visit, values were carried forward from a previous visit.
Employment status was reported at visits 1–4 and then dichotomized into employed versus not employed. At visit 5 (by which time all participants were 70 years of age or older), participants were assumed to be retired. Smoking status was self-reported and categorized into current smoker or nonsmoker. Alcohol intake (grams per week) was estimated from the number of glasses of wine, beer, and hard liquor consumed per week. Diet and physical activity level were assessed at visits 1 and 3. Total daily caloric intake was estimated using a modified 61-question Willet food frequency questionnaire (22). We calculated diet scores based on American Heart Association guidelines. We gave each participant 1 point each for ≥4.5 servings per day of fruits and vegetables; ≥2 servings (3–5 ounces) per week of fish; ≥3 servings per day of whole grains; <1,500 mg sodium per day; and <4 servings per week of sugar-sweetened beverages. Participants with scores of 0 or 1 were considered to have a poor diet (23). Baecke questionnaires were used measure physical activity level; from the results, we calculated scores from 1 to 5 for sports/exercise and leisure time physical activity (24) and an estimate of whether participants met physical activity guidelines of either ≥150 minutes/week of moderate or ≥75 minutes/week of vigorous physical activity (23).
Participants who self-reported having diabetes, took diabetes medications, had a fasting glucose level of 126 mg/dL or higher, or had a nonfasting glucose level of 200 mg/dL or higher were classified as having diabetes. Hypertension was defined as having a mean systolic blood pressure of 140 mm Hg or higher, having a mean diastolic blood pressure of 90 mm Hg or higher, or taking antihypertension medication. Prevalent lung disease and cancer were self-reported; information on cancer was unavailable at visit 5. Prevalent coronary heart disease was self-reported at baseline and based on a combination of baseline self-report and adjudicated events (myocardial infarction, silent myocardial infarction detected by electrocardiogram, and cardiac procedures) at subsequent visits. Because of the large number of people for whom self-reported coronary heart disease at baseline was missing, we included a missing indicator for this variable.
Statistical analysis
We calculated descriptive statistics for key baseline characteristics to understand spousal similarities across exposures, outcomes, and covariates. For continuous variables, we calculated mean values by sex and Pearson correlation coefficients within pairs. For categorical variables, we calculated marginal frequencies by sex and concordance within spouse pairs. We also calculated odds ratios to determine whether having a spouse with the characteristic made an individual more likely to have the characteristic.
To determine the association between incident obesity in a participant and obesity status change in her or his spouse, we calculated the hazard ratio of becoming obese by comparing subjects whose spouse became obese, remained obese, or became nonobese to a reference group of participants whose spouses remained nonobese. We used complementary log-log regression rather than traditional Cox proportional hazards models to take into account interval censoring. Analyses were conducted separately for men and women; analyses for men excluded couples in which the man was obese at baseline and vice versa for women.
We compared 2 models in which we controlled for individual and spousal demographic characteristics, behaviors, risk factors, and illnesses related to BMI, weight, or weight change. Model 1 was adjusted only for baseline BMI. Model 2 was additionally adjusted for the following individual and spousal characteristics: age, race, educational level, current smoking, calorie intake, sport and leisure physical activity indices, alcohol intake, diet score, illnesses that could cause weight change, and risk factors that might change behavior, including hypertension, diabetes, lung disease, cancer, and coronary heart disease. We conducted a sensitivity analysis using lagged rather than concurrent spousal obesity status change as the exposure, that is, using the spouse's change in obesity status from visit 1 to visit 2 as the exposure and the individual's change from visit 2 to 3 as the outcome. In a second sensitivity analysis, we assessed the association between change in spousal obesity and incident nonobesity (BMI dropping below 30) in already obese individuals.
To determine the relationship between a participant's BMI change from one visit to the next and his or her spouse's concurrent BMI change, we used linear mixed models with a random intercept for the pair. We tested BMI changes in men as a function of those in their wives and then BMI changes in women as a function of those in their husbands. The models were the same as those described above except that they were adjusted for time between visits but not baseline BMI. Finally, we tested for interactions between spousal BMI change and the following baseline characteristics: age, race, concordance of obesity status (both obese, neither obese, discordant on obesity), and concordance of key behavioral predictors of obesity (poor diet, meeting physical activity guidelines, and smoking status). We conducted stratified analyses when the P value for interaction was <0.1. All analyses were conducted using Stata software, version 12 (StataCorp LP, College Station, Texas).
RESULTS
Descriptive statistics and cross-sectional analyses
At baseline, the mean age was 55 years in men and 53 years in women. Age was highly correlated between husbands and wives (r = 0.80). In general, participants whose spouses had a characteristic at baseline were more likely to have that same characteristic. The strongest associations were with race (only 4 couples out of our sample of 3,889 were interracial), educational level (odds ratio = 8.55, 95% confidence interval (CI): 7.03, 10.39), and current smoking (odds ratio = 3.57, 95% CI: 3.01, 4.23), such that being a current smoker was associated with a 3-fold higher odds of being married to a current smoker (Table 1).
Table 1.
Baseline Characteristics, Correlation of Continuous Variables, and Concordance of Categorical Variables Within 3,889 Spouse Pairs, Atherosclerosis Risk in Communities Study, 1987–1989
| Characteristic | Individual |
Paired Concordancea |
Correlationb | ORc | 95% CI | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Men |
Women |
H+ W+, % | H− W−, % | H+ W−, % | H− W+, % | ||||||
| Mean (SD) | % | Mean (SD) | % | ||||||||
| Continuous baseline characteristics | |||||||||||
| Age, years | 55.4 (5.4) | 53.0 (5.2) | 0.80 | ||||||||
| BMId | 27.5 (4.0) | 26.9 (5.5) | 0.18 | ||||||||
| Self-reported BMI at 25 years of age | 24.2 (3.4) | 21.9 (3.2) | 0.05 | ||||||||
| Alcohol intake, g/week | 64.3 (108.6) | 21.4 (47.8) | 0.39 | ||||||||
| Calorie intake, kcal/day | 1,767 (634) | 1,503 (519) | 0.13 | ||||||||
| Categorical baseline characteristics | |||||||||||
| White race | 86.6 | 86.7 | 83.5 | 12.8 | 0.0 | 0.1 | ∞e | ||||
| Less than a high school education | 19.5 | 14.5 | 8.2 | 74.2 | 11.3 | 6.3 | 8.55 | 7.03, 10.39 | |||
| Employed | 82.6 | 64.4 | 56.6 | 9.5 | 26.0 | 0.8 | 2.60 | 2.19, 3.07 | |||
| Obese (BMI ≥30d) | 22.6 | 24.7 | 8.1 | 60.8 | 14.6 | 16.6 | 2.03 | 1.72, 2.39 | |||
| Obese at 25 years of age (BMI ≥30d) | 5.92 | 2.69 | 0.3 | 91.7 | 5.6 | 2.3 | 2.36 | 1.30, 4.30 | |||
| Current smoker | 22.6 | 19.6 | 8.5 | 66.3 | 14.2 | 11.1 | 3.57 | 3.01, 4.23 | |||
| Does not meet physical activity guidelines | 55.5 | 67.4 | 40.3 | 17.5 | 15.1 | 27.1 | 1.72 | 1.50, 1.97 | |||
| Poor diet scoref (<2) | 33.2 | 19.8 | 9.1 | 56.0 | 24.2 | 10.7 | 1.95 | 1.66, 2.29 | |||
| Diabetes | 10.6 | 8.1 | 1.4 | 82.6 | 9.3 | 6.7 | 1.82 | 1.33, 2.49 | |||
| History of coronary heart disease | 8.4 | 1.6 | 0.3 | 90.3 | 8.1 | 1.3 | 2.79 | 1.47, 5.31 | |||
| Hypertension | 32.0 | 28.1 | 11.4 | 51.3 | 20.5 | 16.8 | 1.71 | 1.47, 1.97 | |||
| History of lung disease | 4.3 | 4.4 | 0.4 | 91.6 | 4.0 | 4.0 | 2.24 | 1.29, 3.89 | |||
| History of cancer | 4.3 | 6.4 | 0.5 | 89.8 | 3.8 | 5.9 | 2.18 | 1.35, 3.50 | |||
Abbreviations: BMI, body mass index; CI, confidence interval; H, husband; OR, odds ratio; SD, standard deviation; W, wife.
a H+W+ indicates couples in which both the husband and wife have the characteristic; H−W−, couples in which neither have it. H+W− and H−W+ indicate discordant pairs.
b The Pearson correlation coefficient within spouse pairs is shown for continuous variables.
c ORs within spouse pairs represent one's odds of having the characteristic if his or her spouse has the characteristic or the odds of having the characteristic if his or her spouse does not have the characteristic. OR = (H+W+ × H−W−)/(H+W− × H−W+).
d Weight (kg)/height (m2).
e Only 4 pairs were not concordant on race.
f Calculated based on American Heart Association guidelines.
Mean BMI was 27.5 at baseline in men and increased over time to 28.5 at visit 5. Mean baseline BMI in women was 26.9; BMI in women peaked at 28.5 at visit 4 and then declined slightly by visit 5. BMIs in husbands and wives were correlated (r = 0.18 at baseline and similar at visits 2–4, dropping to 0.13 at visit 5). The correlation between self-reported BMI at 25 years of age was lower (r = 0.05). At baseline, a total of 8.1% of couples had 2 obese members; in 60.8% of couples, neither spouse was obese. Obese adults were more likely to have an obese spouse than were normal-weight adults (odds ratio = 2.03, 95% CI: 1.72, 2.39). Similarly, those who reported being obese at 25 years of age were more likely to have a spouse who reported being obese at 25 years of age (odds ratio = 2.36, 95% CI: 1.30, 4.30) (Table 1).
Incident obesity analysis
Nonobese men whose wives became obese between visits were 1.78 times (95% CI: 1.30, 2.43; model 2) more likely to become obese themselves during that period than they would have been if their wives had remained nonobese. However, having a wife who became nonobese or who remained obese was not significantly associated with the chances of a man becoming obese. Results did not vary appreciably after adjustment for factors associated with obesity (Table 2). Results in women were similar: Having their husband become obese was associated with a higher risk of obesity (hazard ratio (HR) = 1.89; 95% CI: 1.39, 2.57; Table 3, model 2). In the sensitivity analysis in which we used lagged spousal obesity status change as the exposure, the results showed a similar trend but did not reach statistical significance (for men, HR = 1.29, 95% CI: 0.83, 2.01; for women HR = 1.17, 95% CI: 0.72, 1.89; model 2). In our sensitivity analysis in which becoming nonobese was the outcome, we found a significant association between a spouse becoming nonobese and an individual becoming nonobese (for men, HR = 1.79, 95% CI: 1.11, 2.88; for women, HR = 1.79, 95% CI: 1.12, 2.86).
Table 2.
Hazard Ratios for Incident Obesity Among 2,990 Men Who Were Not Obese at Baselinea, by Change in Wife's Obesity Status, Atherosclerosis Risk in Communities Study, 1987–2013
| Model | Wife's Obesity Status |
|||||||
|---|---|---|---|---|---|---|---|---|
| Stable Nonobese (n = 5,744)b |
Nonobese to Obese (n = 407) |
Obese to Nonobese (n = 171) |
Stable Obese (n = 1,415) |
|||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| 1c | 1.00 | Referent | 1.78 | 1.32, 2.41 | 1.18 | 0.69, 2.02 | 1.07 | 0.87, 1.31 |
| 2d | 1.00 | Referent | 1.78 | 1.30, 2.43 | 1.17 | 0.67, 2.02 | 1.07 | 0.86, 1.34 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
a A total of 562 men became obese by visit 5.
b The n values represent the number of observations, that is, the changes (or lack of change) in wives’ obesity statuses between 2 visits. Because spouse pairs were usually included for more than 2 visits, the total number of observations (7,737) is greater than the number of spouse pairs in the analysis (2,990). The percent of observations for each category is 74.2% for stable nonobese, 5.3% for nonobese to obese, 2.2% for obese to nonobese, and 18.3% for stable obese.
c Model 1 includes baseline body mass index.
d Model 2 includes baseline body mass index, race, study site, employment, educational level, smoking status, calorie intake, cardiovascular diet score, alcohol intake, leisure and sport physical activity scores, coronary heart disease, hypertension, diabetes, cancer, and lung disease for both the individual and his spouse.
Table 3.
Hazard Ratios for Incident Obesity Among 2,913 Women Who Were Not Obese at Baselinea, by Change in Husband's Obesity Status, 1987–2013
| Model | Husband's Obesity Status |
|||||||
|---|---|---|---|---|---|---|---|---|
| Stable Nonobese (n = 5,720)b |
Nonobese to Obese (n = 466) |
Obese to Nonobese (n = 218) |
Stable Obese (n = 1,233) |
|||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| 1c | 1.00 | Referent | 1.84 | 1.35, 2.44 | 0.88 | 0.59, 1.47 | 1.16 | 0.93, 1.43 |
| 2d | 1.00 | Referent | 1.89 | 1.39, 2.57 | 0.83 | 0.49, 1.40 | 1.13 | 0.90, 1.42 |
Abbreviations: CI, confidence interval; HR, hazard ratio.
a A total of 518 women became obese by visit 5.
b The n values represent the number of observations, that is, the change (or lack of change) in husbands' obesity statuses between 2 visits. Because spouse pairs were usually included for more than 2 visits, the total number of observations (7,637) is greater than the number of spouse pairs in the analysis (2,913). The percent of observations for each category is 74.9% for stable nonobese, 6.1% for nonobese to obese, 2.9% for obese to nonobese, 16.6% and for stable obese.
c Model 1 includes baseline body mass index.
d Model 2 includes baseline body mass index, race, study site, employment, educational level, smoking status, calorie intake, cardiovascular diet score, alcohol intake, leisure and sport physical activity scores, coronary heart disease, hypertension, diabetes, cancer, and lung disease for both the individual and her spouse.
BMI change analysis
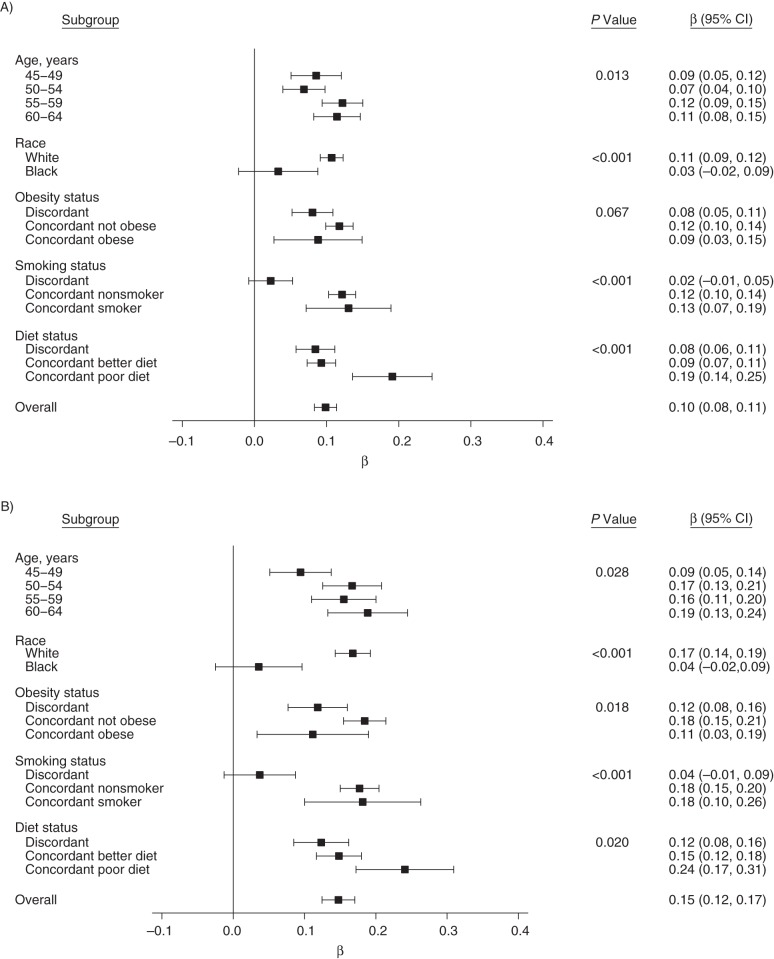
In models in which we used concurrent linear spousal BMI change as the exposure, a 1-unit increase in wives' BMI changes was associated with a 0.10 increase in men's BMI changes (95% CI: 0.09, 0.12) (Figure 1A). This association was not altered by adjustment. A stronger association was seen for women: A 1-unit increase in husbands' BMI change was associated with a 0.15-unit increase in women's BMI change (95% CI: 0.13, 0.18) (Figure 1B).
Figure 1.
Linear associations between changes in participants’ body mass indices and concurrent changes in spousal body mass indices, Atherosclerosis Risk in Communities Study, 1987–2013. Analyses are shown for men (A) and women (B), overall and by subgroup. β coefficients represent the change in body mass index associated with a 1-unit increase in a spouse's body mass index change. P values are for the interaction between each baseline characteristic and change in spousal body mass index. Models were adjusted for the following time-varying individual characteristics and spousal behaviors: age, time between visits, race, study site, employment, educational level, smoking status, calorie intake, cardiovascular diet score, alcohol intake, leisure and sport physical activity level, coronary heart disease, hypertension, diabetes, cancer, and lung disease. The models were not adjusted for the stratification variables.
We found significant (P < 0.1) interactions between spousal BMI change and baseline age, race, obesity concordance, poor diet concordance, and smoking status concordance (concordance in meeting physical activity recommendations did not significantly modify associations between BMI changes in spouses). Figure 1 shows analyses of associations of spousal BMI changes within groups defined by these factors. Of note, we found no evidence of an association between participants' BMI changes and those of their spouses among black couples (for men, β = 0.03, 95% CI: −0.02, 0.09; for women β = 0.04, 95% CI: −0.02, 0.10) or couples who were discordant on baseline smoking status (for men, β = 0.02, 95% CI: −0.01, 0.05; for women β = 0.04, 95% CI: −0.01, 0.09). In couples in which both spouses had a poor diet score at baseline, men's BMI changes were more strongly associated with their wives' BMI changes than in couples with discordant diet quality or where neither spouse had a poor diet (β = 0.19, 95% CI: 0.14, 0.25; β = 0.08, 95% CI: 0.06, 0.11; and β = 0.09, 95% CI: 0.07, 0.11, respectively). Results for women followed a similar pattern.
DISCUSSION
We found that as their spouses' BMIs increased, men's and women's BMIs also increased. Patterns of BMI change in the ARIC Study were similar to those found in other cohorts (25). Our findings confirm and extend the results of studies in which investigators have found positive longitudinal associations between unadjusted 2-year, 7-year, and 12-year changes in BMIs in spouses (14–16). Further, we found that these associations differed depending on whether spouses shared similar behavioral characteristics. We found no association between BMI changes in spouses who were discordant on smoking status at baseline, potentially because of the effect of smoking on BMI and or because spouses who were discordant on smoking shared few health behaviors. Further, we found that the association between BMI changes in couples who shared a poorer diet was stronger than that in either discordant couples or those who shared a healthier diet. Our results were robust to adjustment for individual and spousal characteristics known to be associated with obesity, possibly because spousal risk factors were only weakly associated with an individual's BMI.
To our knowledge, this is the first study in which the association between concurrent spousal obesity status change and incident obesity has been examined. We found that having a spouse become obese increased the likelihood of the participant becoming obese; however, most participants were stable obese or stable nonobese over the study period. In a previous study, Christakis and Fowler (17) found that one's spouse becoming obese in a previous period was associated with a 37% increased likelihood of the subject then developing obesity. In a sensitivity analysis using lagged spousal obesity status change, we found a similar, although nonsignificant, trend. This difference may be because of the loss of power from having one less visit and because lagged spousal change may not fully capture the association that is due to a shared environment. Further, the minimum of 3 years between ARIC Study visits might be too long to capture the true influence of a spouse's prior obesity status change.
Prior research documented that spousal selection plays a small role in the correlation of BMIs across spouses, but it appears to have a larger role among obese individuals (13). Although we do not know at what age ARIC Study participants married, self-reported obesity status at 25 years of age likely represents weight status before marriage or during early marriage. We found that obese subjects were more likely to have obese spouses at both 25 years of age and middle age. However, spouses' BMIs were more strongly correlated at study baseline when participants were between the ages of 45 and 64 years (r = 0.18) than when they were 25 years of age (r = 0.06). The stronger association at baseline suggests that elements of the social and physical environmental within marriage might be as important as spousal selection with regard to obesity.
Among spouses who were not obese at baseline, we found that having a spouse become obese almost doubled the likelihood of becoming obese oneself during that same period. The United States Preventive Services Task Force recommends individually counseling obese adults on weight loss, yet suggests only selectively counseling patients on lifestyle changes that might prevent weight gain, such as eating a healthful diet and increasing physical activity levels, based on professional judgment and patient preferences (26). Our findings suggest that future research should explore whether obesity prevention interventions that target couples at risk of obesity are effective. Having couples adopt healthy behaviors together may be a promising approach, particularly when weight gain is not a consequence of medications or comorbid conditions. Such interventions might focus on nutrition, because we found a stronger association between BMI changes in couples who both had poor diet quality at baseline.
Having a spouse reverse her or his obesity occurred infrequently (8% of participants). Although this was associated with an increased likelihood of an obese individual becoming nonobese, it did not reduce the risk of a nonobese individual becoming obese. Additionally, we found no added risk of becoming obese among those whose spouses remained obese across visits. Based on our effect modification analysis, it is possible that couples who are discordant on obesity are less likely to influence each other than couples in which both members are of similar obesity status.
In prior studies, investigators have found differential effects of marital status on weight by sex; women tend to gain more weight after marriage than do men (27, 28). We found a stronger association between husbands' BMI changes and women's BMI changes than vice versa. These findings are similar to those for smoking cessation among ARIC Study spouse pairs, in which husbands again had a greater influence on wives (4). Previous longitudinal studies of BMI have not found this asymmetry (15, 17), nor did we find it in our obesity status change analysis. One potential explanation for this asymmetry is that power dynamics within marriages may lead to women's weight-related behaviors being more influenced by their husbands' than vice versa (29, 30). However, we should interpret these results cautiously, because they might be influenced by the fact that women in our sample gained more weight on average than did men.
To date, most studies have been conducted among predominantly white populations (14, 16, 17), and we believe that the present study is the first in which spousal associations of BMI change in a black population have been examined. In contrast to our overall findings, results in blacks were nonsignificant. This may be due to the fact that blacks (particularly black women) in our study started with higher BMIs at baseline or to the fact that they were more likely to report being in poor or fair health. Further, previous research has found that the ideal body size for black women is larger than that for white women, which might affect BMI trajectories and their relationships across spouses (31). Although our sample size among black participants was limited (just over 500 pairs), this suggests the need to investigate spousal BMI and obesity status change in diverse populations. Relationships among white Americans might not be generalizable to other groups.
The present study has several strengths. We were able to examine BMI changes in 3,889 spouse pairs and obesity status changes in 2,990 pairs over 25 years. Additionally, we used time-varying covariates; BMI and many associated risk factors were rigorously measured at each visit. Study weaknesses include the long gap between visits 4 and 5 and the large rate of attrition (mostly due to death) by visit 5. Further, measurement error in some key effect modifiers, such as physical activity level, might have biased the assessment of interactions toward the null. Although we were able to account for changes in some individual factors, we were not able to control for changes in environmental or social factors that can impact obesity. Finally, spouse pairs in the ARIC Study are all heterosexual married couples, reflecting norms at the time of recruitment in 1987–1989 and possibly limiting the generalizability of our study.
In conclusion, both obesity status and BMI changes among spouses are associated over time. These associations are driven to a certain extent by the fact that spouses share similar behaviors, such as diet. Previous studies have suggested that individuals' behaviors are not only likely to be concordant with those of their spouses but may also influence their spouses' behavior. Given our overall failure to reverse the obesity epidemic, new approaches may be needed. In the absence of comprehensive policies that can change the environment for both spouses, clinicians and public health professionals may want to explore targeting obesity prevention messages at the couple rather than at an individual.
ACKNOWLEDGMENTS
Author affiliations: Welch Center for Prevention, Epidemiology and Clinical Research, Johns Hopkins University, Baltimore, Maryland (Laura K. Cobb, Mara A. McAdams-DeMarco, Kimberly A. Gudzune, Mark Woodward, Elizabeth Selvin, Josef Coresh); Department of Epidemiology, Bloomberg School of Public Health, Johns Hopkins University, Baltimore, Maryland (Laura K. Cobb, Mara A. McAdams-DeMarco, Cheryl A. M. Anderson, Mark Woodward, Elizabeth Selvin, Josef Coresh); Division of General Internal Medicine, School of Medicine, Johns Hopkins University, Baltimore, Maryland (Kimberly A. Gudzune); Department of Family and Preventive Medicine, School of Medicine, University of California, San Diego, San Diego, California (Cheryl A. M. Anderson); Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, Minnesota (Ellen Demerath); The George Institute for Global Health, University of Sydney, Sydney, Australia (Mark Woodward); and Nuffield Department of Population Health, University of Oxford, Oxford, United Kingdom (Mark Woodward).
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C. L.K.C. was supported in part by the National Heart, Lung, and Blood Institute Cardiovascular Epidemiology Training Grant (T32HL007024) and the National Institute of Diabetes and Digestive Kidney Diseases Diabetes and Endocrinology Training Grant (2T32DK062707-11A1). K.A.G. is supported by a career development award from NHLBI (K23HL116601). M.A.M.-D. is supported by a career development award from the National Institute on Aging (K01AG043501).
We thank the staff of the Atherosclerosis Risk in Communities Study for their important contributions.
Conflict of interest: none declared.
Appendix Table 1.
Retention in Spouse Pairs, Atherosclerosis Risk in Communities Study, 1987–2013
| Spouse Pair Retention | Visit (Years) |
Total No. | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 (1987–1989) |
2 (1990–1992) |
3 (1993–1995) |
4 (1993–1995) |
5 (2011–2013) |
||||||
| No. | No. | % | No. | % | No. | % | No. | % | ||
| Retention summary | ||||||||||
| Total cohort | 15,792 | 14,348 | 91 | 12,887 | 82 | 11,656 | 74 | 6,538 | 41 | |
| ≥1 spouse | 4,505 | 4,346 | 96 | 4,111 | 91 | 3,860 | 86 | 2,644 | 59 | |
| Both spouses | 4,505 | 4,042 | 90 | 3,537 | 79 | 3,111 | 69 | 1,406 | 31 | |
| Both spouses, married | 4,505 | 3,985 | 88 | 3,467 | 77 | 3,030 | 67 | 1,357 | 30 | |
| Reason for drop out among spouse pairs | ||||||||||
| Deaths (≥1) | 284 | 14 | 344 | 17 | 335 | 17 | 1,059 | 52 | 2,022 | |
| Drop out (both)a | 86 | 8 | 98 | 9 | 119 | 11 | 701 | 66 | 1,062 | |
| Divorce/separationb | 61 | 51 | 30 | 25 | 18 | 15 | 13 | 11 | 120 | |
| Reason for drop out among full cohort | ||||||||||
| Death | 720 | 15 | 804 | 16 | 820 | 17 | 2,566 | 52 | 4,910 | |
| Drop outa | 358 | 8 | 424 | 10 | 577 | 13 | 2,985 | 69 | 4,344 | |
a Pairs/individuals who failed to attend a visit but were seen in subsequent visits were not included in this row (246 pairs and 1,022 individuals).
b Pairs classified as leaving because of drop out might also have had at least 1 partner die before the end of follow-up (n = 46). However, 1 spouse dropped out before death, and therefore the pair was classified as lost to drop out rather than death.
REFERENCES
- 1.United States Census Bureau. Selected Social Characteristics in the United States: 2008–2012 American Community Survey 5-year Estimates. http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_12_5YR_DP02&prodType=table Updated 2014. Accessed March 26, 2014.
- 2.McAdams DeMarco M, Coresh J, Woodward M et al. Hypertension status, treatment, and control among spousal pairs in a middle-aged adult cohort. Am J Epidemiol. 2011;1747:790–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sutton GC. Do men grow to resemble their wives, or vice versa? J Biosoc Sci. 1993;251:25–29. [DOI] [PubMed] [Google Scholar]
- 4.Cobb LK, McAdams-DeMarco MA, Huxley RR et al. The association of spousal smoking status with the ability to quit smoking: the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2014;17910:1182–1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Falba TA, Sindelar JL. Spousal concordance in health behavior change. Health Serv Res. 2008;43(1 Pt 1):96–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogden CL, Carroll MD, Kit BK et al. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA. 2014;3118:806–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Flegal KM, Graubard BI, Williamson DF et al. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;29315:1861–1867. [DOI] [PubMed] [Google Scholar]
- 8.Jeffery RW, Utter J. The changing environment and population obesity in the United States. Obes Res. 2003;11(suppl):12S–22S. [DOI] [PubMed] [Google Scholar]
- 9.Svetkey LP, Stevens VJ, Brantley PJ et al. Comparison of strategies for sustaining weight loss: the weight loss maintenance randomized controlled trial. JAMA. 2008;29910:1139–1148. [DOI] [PubMed] [Google Scholar]
- 10.Katzmarzyk PT, Hebebrand J, Bouchard C. Spousal resemblance in the Canadian population: implications for the obesity epidemic. Int J Obes Relat Metab Disord. 2002;262:241–246. [DOI] [PubMed] [Google Scholar]
- 11.Bloch KV, Klein CH, de Souza e Silva NA et al. Socioeconomic aspects of spousal concordance for hypertension, obesity, and smoking in a community of Rio de Janeiro, Brazil. Arq Bras Cardiol. 2003;802:179–186. [DOI] [PubMed] [Google Scholar]
- 12.Di Castelnuovo A, Quacquaruccio G, Donati MB et al. Spousal concordance for major coronary risk factors: a systematic review and meta-analysis. Am J Epidemiol. 2009;1691:1–8. [DOI] [PubMed] [Google Scholar]
- 13.Ajslev TA, Angquist L, Silventoinen K et al. Assortative marriages by body mass index have increased simultaneously with the obesity epidemic. Front Genet. 2012;3:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Katzmarzyk PT, Pérusse L, Rao DC et al. Spousal resemblance and risk of 7-year increases in obesity and central adiposity in the Canadian population. Obes Res. 1999;76:545–551. [DOI] [PubMed] [Google Scholar]
- 15.Jeffery RW, Rick AM. Cross-sectional and longitudinal associations between body mass index and marriage-related factors. Obes Res. 2002;108:809–815. [DOI] [PubMed] [Google Scholar]
- 16.Rice T, Pérusse L, Bouchard C et al. Familial aggregation of body mass index and subcutaneous fat measures in the longitudinal Québec Family Study. Genet Epidemiol. 1999;163:316–334. [DOI] [PubMed] [Google Scholar]
- 17.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;3574:370–379. [DOI] [PubMed] [Google Scholar]
- 18.The NS, Gordon-Larsen P. Entry into romantic partnership is associated with obesity. Obesity (Silver Spring). 2009;177:1441–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cohen-Cole E, Fletcher JM. Is obesity contagious? Social networks vs. environmental factors in the obesity epidemic. J Health Econ. 2008;275:1382–1387. [DOI] [PubMed] [Google Scholar]
- 20.Mozaffarian D, Hao T, Rimm EB et al. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;36425:2392–2404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Atherosclerosis Risk in Communities (ARIC) Study: design and objectives. The ARIC investigators. Am J Epidemiol. 1989;1294:687–702. [PubMed] [Google Scholar]
- 22.Willett WC, Sampson L, Stampfer MJ et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;1221:51–65. [DOI] [PubMed] [Google Scholar]
- 23.Folsom AR, Yatsuya H, Nettleton JA et al. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;5716:1690–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;365:936–942. [DOI] [PubMed] [Google Scholar]
- 25.Kimokoti RW, Newby PK, Gona P et al. Patterns of weight change and progression to overweight and obesity differ in men and women: implications for research and interventions. Public Health Nutr. 2013;168:1463–1475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moyer VA; U.S. Preventive Services Task Force. Screening for and management of obesity in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;1575:373–378. [DOI] [PubMed] [Google Scholar]
- 27.Sobal J, Rauschenbach B, Frongillo EA. Marital status changes and body weight changes: a US longitudinal analysis. Soc Sci Med. 2003;567:1543–1555. [DOI] [PubMed] [Google Scholar]
- 28.Rauschenbach B, Sobal J, Frongillo EA Jr. The influence of change in marital status on weight change over one year. Obes Res. 1995;34:319–327. [DOI] [PubMed] [Google Scholar]
- 29.Brown JL, Miller D. Couples’ gender role preferences and management of family food preferences. J Nutr Educ Behav. 2002;344:215–223. [DOI] [PubMed] [Google Scholar]
- 30.Sprecher S, Felmlee D. The balance of power in romantic heterosexual couples over time from “his” and “her” perspectives. Sex Roles. 1997;37(5/6):361–379. [Google Scholar]
- 31.Padgett J, Biro FM. Different shapes in different cultures: body dissatisfaction, overweight, and obesity in African-American and Caucasian females. J Pediatr Adolesc Gynecol. 2003;166:349–354. [DOI] [PubMed] [Google Scholar]