Abstract
Introduction:
Ludwig's angina (LA) still presents regularly at our tertiary academic hospital. Various etiologies and comorbid diseases are documented worldwide, but the South African population has not been studied.
Aim:
To establish whether LA cases presenting to the department are different from international reports regarding etiology and comorbidities.
Settings and Design:
Retrospective analysis of patients presenting with LA to a tertiary hospital.
Materials and Methods:
93 patients were included over a 5-year period. Archived files were analyzed for data including age, gender, comorbid diseases, etiology, airway management, and season on admission.
Statistical Analysis:
Descriptive statistics with the inclusion of frequency distributions.
Results:
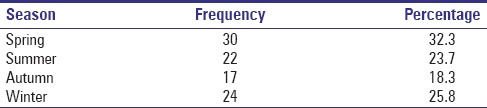
93 patients were included; 65 (69.9%) male and 28 (30.1%) female; age - minimum 20 years, maximum 75 years, mean 40.366. Etiology: 68 (73.1%) odontogenic, 13 (14%) nonodontogenic, and 12 (12.9%) unknown cause. Comorbid diseases: 21 (22.6%) diabetes mellitus (DM), 19 (20.4%) hypertension, and 18 (19.4%) human immunodeficiency virus (HIV). Airway management: 61 (65.6%) tracheostomy and 32 (34.4%) nonsurgical. Complications: 11 (11.8%) deaths, 8 (8.60%) descending mediastinitis, and 7 (7.53%) necrotizing fasciitis. Seasonal occurrence: 30 (32.3%) spring, 24 (25.8%) winter, 22 (23.7%) summer, and 17 (18.3%) autumn.
Conclusion:
A 2.32:1 ratio male: female presentation mirrors previous statistics. DM patients had increased risks of complications, which resulted in multiple deaths. HIV patients showed increased risks for complications with more intense, longer hospital stays, but lower percentages of deaths compared to patients with DM and complications who died. There was no statistically significant finding regarding seasonal tendency.
Keywords: Airway management, comorbid diseases, complications, etiology, Ludwig's angina
INTRODUCTION
Despite modern medicine and improved oral hygiene programs, Ludwig's angina (LA) presents regularly at our tertiary academic institution. Various etiologies and comorbid diseases have been documented in patients worldwide, but the South African population has not been studied.
Etiologies worldwide are divided into odontogenic and nonodontogenic groups. Diabetes mellitus (DM) has been well-documented as a comorbid disease in patients presenting with LA internationally.
To date, only one study has been conducted in South Africa, which focussed on the microbiology of the disease. The comorbid disease burden in South Africa is great and as such could be expected to play a role in disease progression and presentation.
MATERIALS AND METHODS
This study was conducted on cases over a 5-year period, using patient files that were archived in the department. All relevant data required for the research were personally retrieved by the researcher. The following data were required upon admission: Age, gender, date of admission, etiology of infection, comorbid diseases of the patient, and airway management technique required upon surgical treatment of the infection. If any comorbid diseases were diagnosed during the period of hospitalization, this too was counted in the analysis. All patients were counseled about undergoing human immunodeficiency virus (HIV) testing that was done only once consent was signed.
Patient/research object selection
Inclusion criteria
A diagnosis of LA, as per the definition proposed by Grodinsky in 1939
Signed informed consent (for treatment and research).
Exclusion criteria
Fascial space infection not conforming to the definition of LA
No signed informed consent
Patient file missing/incomplete
Minors/pediatric patients (patients below the age of 16).
Data analysis and interpretation
The data consisted of a sample size total n = 93, and proportionate numbers of cases that had odontogenic/nonodontogenic causes, and/or comorbidities expressed and defined as descriptive statistics with inclusion of frequency distributions. Data were also collected with regard to seasonal tendencies, airway management technique required during the initial treatment of the patients, and complications/deaths that arose during management of these patients.
Ethics
This was an analysis of clinical records and files of patients admitted for LA to the academic institution. The files have a disclaimer, which patients are made aware of, stating that all information listed on the questionnaire may be used by researchers under a blanket of confidentiality. Before any treatment was initiated on any patient, informed consent concerning the procedures required and risks involved was obtained from the patient. Each patient was assigned a number. None of the patients’ personal details (names, file number, etc.) was revealed, and the files never left the premises of the maxillofacial and oral surgery archives. Consent to use the files and database was requested from the HOD and Dean of the faculty. Ethical clearance was obtained from Ethics Committee as per the Helsinki Declaration.
RESULTS
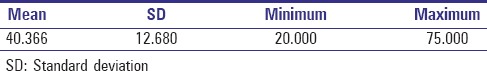
Age distribution
The oldest patient was aged 75 years and despite several minors presenting whom were excluded from the study as per study criteria, the youngest was 20 years old. The mean age was 40.366 years [Table 1].
Table 1.
Age of patients with Ludwig's angina
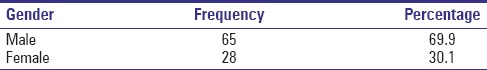
Gender
There was a marked male predominance in patients presenting with LA, with the ratio of female to male was 1:2.32 [Graph 1 and Table 2].
Graph 1.
Graphic presentation of gender differences
Table 2.
Gender differences
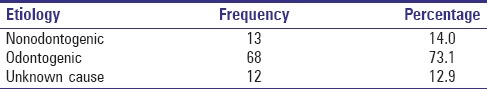
Etiology
The large majority of LA cases presenting to the department were of odontogenic origin. Nonodontogenic causes included sialadenitis, floor of mouth injury during violent assault, peritonsillar abscess (five cases), lymphadenitis, infected mandibular fracture, infected insect bite to the chin, infected shaving injury, infected ranula, and an infected sebaceous cyst on the chin [Table 3].
Table 3.
Etiology of Ludwig's angina
Comorbid diseases
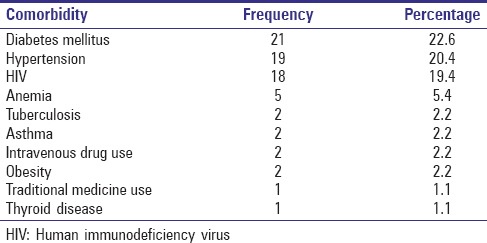
DM was present in n = 21, 22.6% of the patients. Hypertension was present in n = 19, 20.4%, and HIV presented in n = 18, 19.4% of patients. However, there were several patients who refused consent for HIV testing, thus the result possibly may not be a true reflection of actual cases present, considering the high burden of HIV infection in RSA [Table 4].
Table 4.
Comorbid diseases of patients with Ludwig's angina
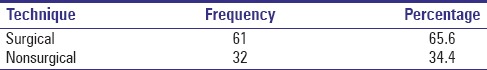
Airway management
Surgical airways accounted for n = 61, 65.6 % of the cases, while normal endotracheal intubation accounted for n = 32, 34.4 % of the cases [Table 5].
Table 5.
Airway management required
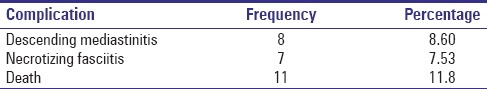
Complications
A total of n = 11 patients died during or after intervention either due to acute airway compromise and cardiac arrest, or septic shock with multiple organ failure. There were n = 8 patients with diagnosed descending mediastinitis and n = 7 with necrotizing fasciitis of the neck and/or anterior chest [Table 6].
Table 6.
Complications encountered after admission
Seasonal spread/tendency
The weather bureau of South Africa divides the seasons as per Table 7. There were no significant statistical differences between the four seasons in terms of predominance. Spring had the highest presentation of cases and autumn had the least [Table 8].
Table 7.
South African seasonal spread
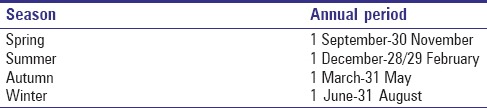
Table 8.
Seasonal presentation of Ludwig's angina
DISCUSSION
LA, previously known as “angina maligna” and “morbus strangularis,” is a potentially fatal, rapidly expanding and progressive infection of bilateral submandibular, sublingual, and submental facial spaces.[1] In 1836, a German surgeon, Wilhelm Friedrich von Ludwig was the first to diagnose five patients with rapidly expanding submandibular infections, which he noticed progressed to involve tissues from the floor of the mouth down to and including the larynx.[1,2]
In 1939, Dr. Manuel Grodinsky suggested four criteria in making the diagnosis of LA, namely: (1) Bilateral infection involving more than one “peri-mandibular” facial space; (2) producing a gangrenous, serosanguinous, putrid infiltration often associated with little or no pus formation initially; (3) involving connective tissue, fascia, and muscle but rarely/never glandular tissue; (4) spreading via continuous planes in fascial spaces and not via lymphatics or hematogenous routes [Figure 1].[3]
Figure 1.

Typical bilateral submandibular and submental swelling
Spread of infection is facilitated by synergism between aerobic and anaerobic organisms, and the resultant virulence of these.[4] More often than not, the microbiological etiology of LA is polymicrobial, which is representative of the oral mucosal microflora.[5] Organisms isolated worldwide are Enterococcus, Escherichia coli, Fusobacterium, Klebsiella pneumoniae, Streptococcus spp., Staphylococcus aureus, Pseudomonas, and Actinomyces spp.[6] Important to remember when dealing with LA is that antibiotic cover alone will not manage the infection, and the prognosis only improves with combined surgical and pharmacological management.[7]
Several life-threatening complications are associated with LA, namely: Acute airway obstruction, upper respiratory airway infection, acute respiratory distress syndrome, descending mediastinitis, necrotizing fasciitis, pleural empyema, pericarditis, epidural abscess, jugular vein thrombosis, carotid artery rupture, septic embolus, systemic sepsis, and disseminated intravascular coagulopathy.[8,9] Deaths are usually the result of long-standing or significant sepsis followed by multiorgan failure [Figures 2-6].[10]
Figure 2.

Another patient intubated before surgical intervention
Figure 6.

Healing wound bed pre-split thickness skin graft
Figure 3.

Same patient with surgical drains and tracheostomy tube in situ
Figure 4.

Same patient who developed necrotizing fasciitis 4 days postdrainage
Figure 5.

Postradical debridement
Four principles form the cornerstones in treating LA. First and foremost is urgent skillful management of a patent, safe airway. Airway compromise due to LA usually originates from parapharyngeal or retropharyngeal edema giving rise to supraglottic obstruction.[11] There are major concerns about the mass effect of the infection, which either compresses the airway or could lead to aspiration of saliva, or of pus if the abscess ruptures.[12] Airway management options include blind nasotracheal intubation, retrograde intubation, GlideScope, fiberoptic intubation, and surgical airway or tracheostomy.[13] However, Sakamoto et al. advocated that tracheostomy should be avoided where possible due to a connection between the fascial spaces which may lead to the pretracheal space being involved with possible spread of infection further inferiorly into the chest.[8] Second, aerobic and anaerobic antibiotics cover should be initiated as early as possible at aggressive dosages. Third, thorough incision and drainage of the facial spaces involved should be carried out to decompress the involved areas and should include treating the cause as well.[8] Finally, patients require stringent control of their fluid management and adequate nutritional support, usually via a nasogastric feeding tube, in their postoperative recovery phase.[14] This all translates into substantial resource utilization during hospitalization and intensive manpower input and time.[15]
Over a 5-year period, 93 patients presented to our facility. 65 of those were males (69.9%), and 28 were females (30.1%), a ratio of 2.32:1, which is similar to worldwide studies also showing a male predominance in presentation, citing a 2:1 ratio. The largest study to reciprocate this finding was by Allareddy et al.[16] A possible explanation for this in our setting is that males are often the sole breadwinners of the family, and as such time constraints limit the time they have to seek medical/dental aid. The other reason is that males generally seek aid a lot later than females do, which means they often present with progressed disease requiring aggressive intervention. Some culturally based beliefs also view men as weak if they seek medical help for a disease/infection.
The mean age of presentation was 40.366 years. Patients in this age group again are mostly part of the working force of the community, and as such time constraints apply. This age group also presents with increased rates of comorbid disease, either newly diagnosed or advanced disease. Again the reason for this may be due to poor checkup history due to time constraints.
Odontogenic origin of infection is in accordance with worldwide reports, making up 73.1% of the cases. Unknown origin is documented as being present in a high percentage of pediatric cases worldwide, yet it made up 12.9% of the adult cases presenting to our facility. Nonodontogenic causes comprised 14.0% of cases.
The top 3 presenting comorbid diseases were DM (22.6%), hypertension (20.4%), and HIV (19.4%). DM is well-documented as a cause of compromised immunity, poor wound healing, and increased risk of both infection and prolonged hospital stays due to increased severity of infection. Four of the 21 patients with DM (19.05%) developed serious life-threatening complications, and significantly all those patients died (100%). This is in accordance with the study by Miller and Dodson, who found diabetic patients to be more at risk of developing bacteremias, pneumonia, and necrotizing fasciitis.[17] It also reflects the need for close monitoring of these patients, with strict control of their blood glucose levels, and early aggressive management of the initial infection or subsequent complications as reciprocated in the study by Chen et al.[9]
Unfortunately, there were several patients who refused consent for HIV testing; thus, this may be a limitation in this study, as it may not reflect the true incidence of HIV considering the high documented infection rate in South Africa. Nonetheless, HIV percentages in our facility were significantly higher than documented results from worldwide studies. Significantly, 7 of the 18 patients with HIV (38.89%) developed serious life-threatening complications, and 4 of those 7 (57.14%) died due to complications. These findings are similar to findings by Carey and Dodson,[18] in that HIV patients in our facility had a more complicated and longer hospital stay and had a greater percentage of complications and death associated with the infection.
Due to late presentation and advanced disease at the time of presentation, the majority of our patients already had airway compromise. This required surgical management of the airway by way of a tracheostomy. Surgical airways accounted for n = 61, 65.6% of the cases, while normal endotracheal intubation accounted for n = 32, 34.4% of the cases.
Deaths related to acute airway compromise or infection-related consequences comprised 11.8% (n = 11) of the study population. Early reports of LA had deaths reported at 60%, but the statistics have changed to between 4% and 10% in recent studies. The possible explanation for the 11.8% in our study was that the majority of our patients presented late in the progression of the infection and were severely compromised already at the time of presentation. Thus, their surgical intervention and/or postoperative course was compromised. The reasons for late presentation are multiple, but worryingly, clinical ignorance seems to be a growing concern with doctors/dentists managing patients with oral antibiotics for several days before finally referring the patient to us for correct management, often in a very compromised condition by that stage. Added to this is the problem with transportation of the patients between the referring facility and our facility where management is carried out. Often there are time delays that compromise the situation and management again. Causes of death included mediastinitis/pericarditis (n = 5), hypoxic cardiac arrest (n = 2), and multiple organ failure (n = 4). The cases of hypoxic cardiac arrest occurred as a result of acute airway compromise, hypoxic obtundation/confusion/aggression, with resultant inability to secure an airway.
We found no significant statistical differences in seasonal presentation of LA. However, spring showed a statistically insignificant increase in occurrences (n = 30, 32.3%) compared to the other seasons.
Our management of patients follows more or less the following protocol:
Full examination with relevant standard facial X-rays, permitting no acute airway compromise is present. If this is the case, the patient is immediately sent for admission for emergency surgery
Blood is drawn for full blood count, electrolytes, C-reactive protein, and HIV test if consented to
Consent for surgical drainage and debridement of all fascial spaces involved, with removal of any offending or suspicious teeth
Anesthetic consult with plan for airway management
Intravenous fluids and antibiotics initiated
Emergency surgery with admission for postoperative care and management
The empiric antibiotics initiated are amoxicillin/clavulanic acid 1.2 g and metronidazole 500 mg intravenous, until such time as we know the patients’ renal status or the microscopy, culture and sensitivity tests are available, whereupon we may escalate with gentamycin 240 mg daily. Patients managed comprehensively with referral to other specialties (e.g., internal medicine) should the need arise.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scully C, Langdon J, Evans J. Marathon of eponyms: 12 Ludwig angina. Oral Dis. 2010;16:496–7. doi: 10.1111/j.1601-0825.2009.01544.x. [DOI] [PubMed] [Google Scholar]
- 2.Kavarodi AM. Necrotizing fasciitis in association with Ludwig's angina – A case report. Saudi Dent J. 2011;23:157–60. doi: 10.1016/j.sdentj.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcus BJ, Kaplan J, Collins KA. A case of Ludwig angina: A case report and review of the literature. Am J Forensic Med Pathol. 2008;29:255–9. doi: 10.1097/PAF.0b013e31817efb24. [DOI] [PubMed] [Google Scholar]
- 4.Opitz D, Camerer C, Camerer DM, Raguse JD, Menneking H, Hoffmeister B, et al. Incidence and management of severe odontogenic infections – A retrospective analysis from 2004 to 2011. J Craniomaxillofac Surg. 2015;43:285–9. doi: 10.1016/j.jcms.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Chang CM, Lu FH, Guo HR, Ko WC. Klebsiella pneumoniae fascial space infections of the head and neck in Taiwan: Emphasis on diabetic patients and repetitive infections. J Infect. 2005;50:34–40. doi: 10.1016/j.jinf.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Rao DD, Desai A, Kulkarni RD, Gopalkrishnan K, Rao CB. Comparison of maxillofacial space infection in diabetic and nondiabetic patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:e7–12. doi: 10.1016/j.tripleo.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Walia IS, Borle RM, Mehendiratta D, Yadav AO. Microbiology and antibiotic sensitivity of head and neck space infections of odontogenic origin. J Maxillofac Oral Surg. 2014;13:16–21. doi: 10.1007/s12663-012-0455-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caccamese JF, Jr, Coletti DP. Deep neck infections: Clinical considerations in aggressive disease. Oral Maxillofac Surg Clin North Am. 2008;20:367–80. doi: 10.1016/j.coms.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Chen MK, Wen YS, Chang CC, Lee HS, Huang MT, Hsiao HC. Deep neck infections in diabetic patients. Am J Otolaryngol. 2000;21:169–73. doi: 10.1016/s0196-0709(00)85019-x. [DOI] [PubMed] [Google Scholar]
- 10.Yadav S, Verma A, Sachdeva A. Facial necrotizing fasciitis from an odontogenic infection. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:e1–4. doi: 10.1016/j.tripleo.2011.06.010. [DOI] [PubMed] [Google Scholar]
- 11.Flavell EM, Stacey MR, Hall JE. The clinical management of airway obstruction. Curr Anaesth Crit Care. 2009;20:102–12. [Google Scholar]
- 12.Ryan P, McMahon G. Severe dental infections in the emergency department. Eur J Emerg Med. 2012;19:208–13. doi: 10.1097/MEJ.0b013e32834ddb68. [DOI] [PubMed] [Google Scholar]
- 13.Wolfe MM, Davis JW, Parks SN. Is surgical airway necessary for airway management in deep neck infections and Ludwig angina? J Crit Care. 2011;26:11–4. doi: 10.1016/j.jcrc.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 14.Chou YK, Lee CY, Chao HH. An upper airway obstruction emergency: Ludwig angina. Pediatr Emerg Care. 2007;23:892–6. doi: 10.1097/pec.0b013e31815c9d4a. [DOI] [PubMed] [Google Scholar]
- 15.Kim MK, Allareddy V, Nalliah RP, Kim JE, Allareddy V. Burden of facial cellulitis: Estimates from the nationwide emergency department sample. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:312–7. doi: 10.1016/j.tripleo.2011.07.043. [DOI] [PubMed] [Google Scholar]
- 16.Allareddy V, Rampa S, Nallaih RP, Allareddy V. Longitudinal discharge trends and outcomes after hospitalization for mouth cellulitis and Ludwig angina. Anesth Analg. 2014;100:524–31. doi: 10.1016/j.oooo.2014.06.003. [DOI] [PubMed] [Google Scholar]
- 17.Miller EJ, Jr, Dodson TB. The risk of serious odontogenic infections in HIV-positive patients: A pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:406–9. doi: 10.1016/s1079-2104(98)90364-x. [DOI] [PubMed] [Google Scholar]
- 18.Carey JW, Dodson TB. Hospital course of HIV-positive patients with odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91:23–7. doi: 10.1067/moe.2001.111410. [DOI] [PubMed] [Google Scholar]


