Abstract
Chondromyxoid fibroma (CF) is a benign bone tumor of cartilaginous origin and is considered the least common of cartilage-derived neoplasms. The lesion's most frequent location is in long bones, while involvement of craniofacial skeleton is extremely unusual. It generally appears in the second and third decade of life and most frequent in men. We present the case of a 68-year-old female with a CF of the zygomatic region. The resection of the tumor and reconstruction of the defect is described.
Keywords: Bone neoplasms, chondromyxoid fibroma, zygoma
INTRODUCTION
In 1948, Jaffe reported a bone tumor similar to chondrosarcoma but its clinical behavior was benign, he classified it as chondromyxoid fibroma (CF).[1]
According to the World Health Organization, CF is a bone tumor of cartilaginous origin that appears in long bones, the most affected of which are the proximal tibia and the distal femur. Cases have been reported in other bones of the body and only 2% of the cases involved bones in the craniofacial skeleton. In this article, we report a very rare case of a 68-year-old woman with an CF in the zygoma.[2,3]
CASE REPORT
We present the case of a healthy 68-year-old female patient with no history of surgery who was referred to the maxillofacial surgery and traumatology unit of the University of Chile Hospital after being diagnosed with odontogenic myxoma of the left zygomatic arch. The patient reported having consulted with the maxillofacial surgery service in another city because of a slight increase in the volume in the left zygomatic region, which caused intermittent, intense and lacerating pain that irradiated to the ipsilateral temporal region with an intensity of eight on the visual analog scale and which was not relieved with common analgesics [Figures 1 and 2]. That service undertook an incisional biopsy with an intraoral approach and diagnosed an odontogenic myxoma. After a physical examination of the patient, a slight increase in volume with diffuse borders and a firm consistency was detected.
Figure 1.

Extraoral view of patient
Figure 2.

Profile view of patient
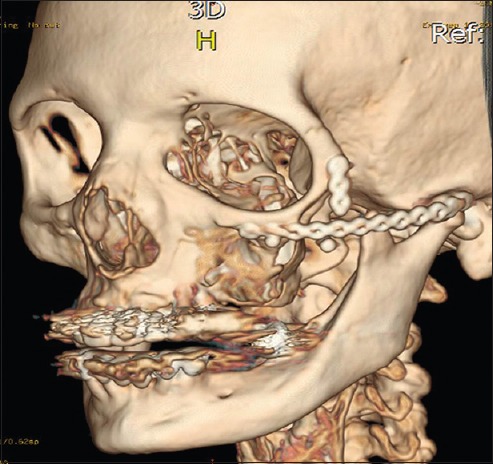
Computer tomography (CT) was requested, revealing a lesion of 3 cm × 3 cm with clear boundaries and mixed density, which was compromising the body of the left malar bone and was spreading to the zygomatic arch [Figures 3-5].
Figure 3.
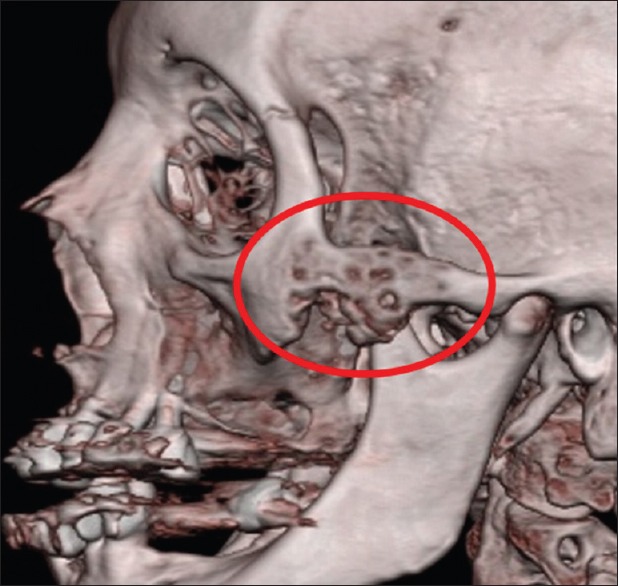
Three-dimensional reconstruction of computed tomography, revealed a lesion in the body of the left zygoma (red circle)
Figure 5.
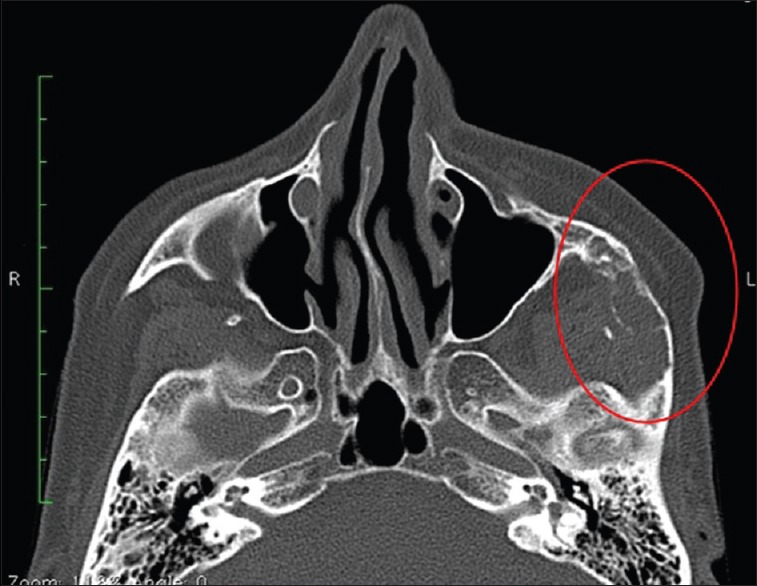
Axial view of computed tomography, showing involvement of the body of the left zygoma and internal cortical erosion of the bone
Figure 4.
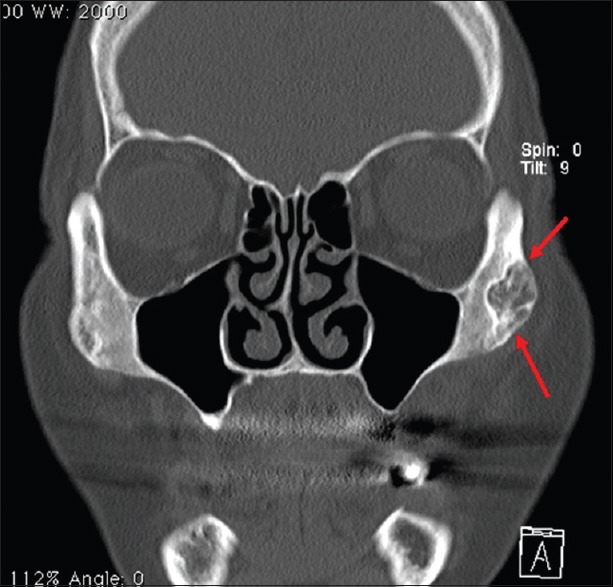
Coronal view of computed tomography, revealed a lesion of mixed density in the left zygoma (red arrow)
According to the patient's clinical history, the imaging and biopsy diagnosis a tumor resection was planned with a safety margin appropriate to the initial diagnosis, accessing the lesion with a coronal approach. The tumor was resected with a reciprocating saw, leaving macroscopic margins in the healthy bone [Figures 6 and 7]. The facial architecture was reconstructed in the same surgical event, using a 2.0 mm titanium osteosynthesis plate to restore the facial arch that had been lost, in addition to a biocompatible porous high-density polyethylene alloplastic graft to restore the contour [Figures 8 and 9].
Figure 6.
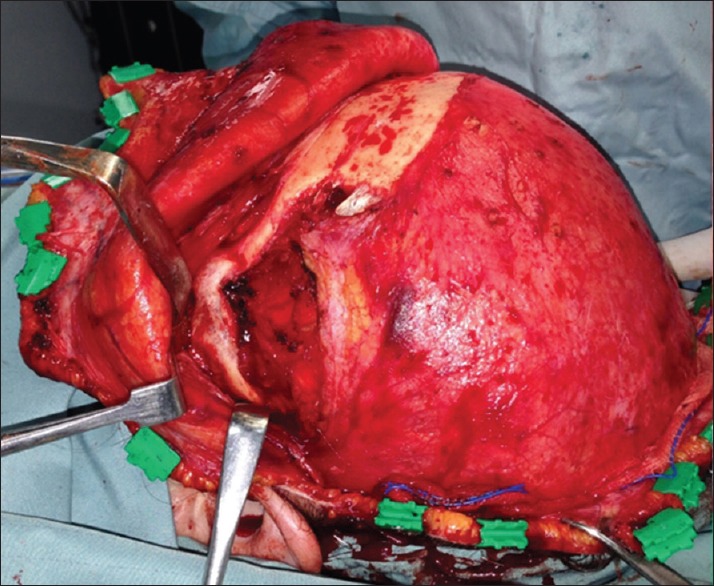
Coronal approach to the left zygoma and exposure of the lesion
Figure 7.
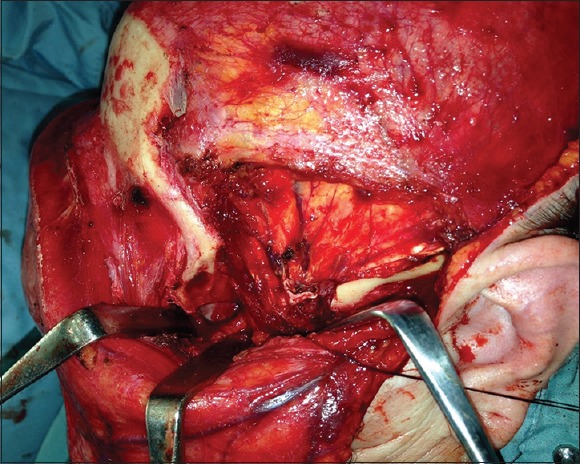
Intraoperative view showing defect after resection of the lesion
Figure 8.
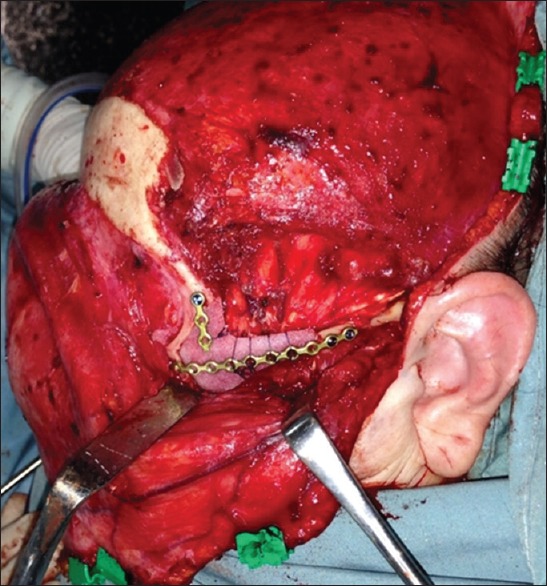
Reconstruction of the defect with a 2.0 mm titanium osteosynthesis plate and a high-density polyethylene alloplastic graft
Figure 9.
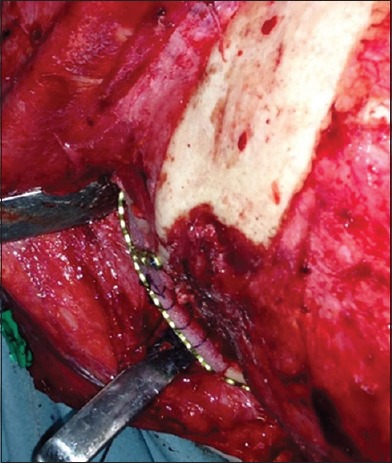
Intraoperative view showing good contour of the reconstruction
A surgical specimen of 3 cm × 4 cm was obtained, mainly consisting of intact bone with some areas where the lesion had been exteriorized to the cortical bone. This specimen was sent for biopsy to obtain a definitive diagnosis, which was CF [Figure 10].
Figure 10.
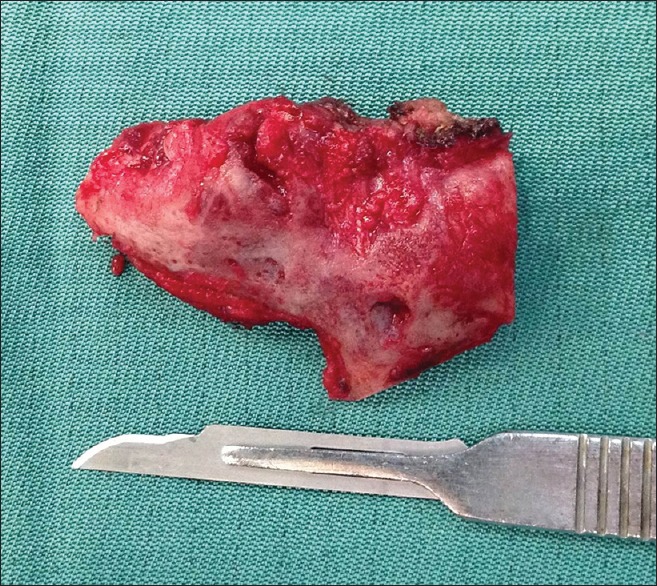
Surgical specimen of 3 cm × 4 cm obtained after resection of the lesion
The patient evolved positively with the pain symptoms completely resolved and the biopsy confirmation that the lesion had been completely eliminated, in addition to restoring her facial esthetics. Six months postoperative a CT was taken showing excellent contour and continuity of zygomatic arch [Figure 11].
Figure 11.
Postoperative three-dimensional reconstruction showing good contour and continuity of zygomatic arch
The histopathological study showed lobules with areas of myxomatous connective tissue, with islands of epithelioid cells, near muscle tissue (lower border of figure). The cells were epithelioid with central nuclei, pink cytoplasms. The myxomatous areas showed spindle and stellate cells and small blood vessels. Well-formed hyaline cartilage was not found [Figures 12 and 13].
Figure 12.
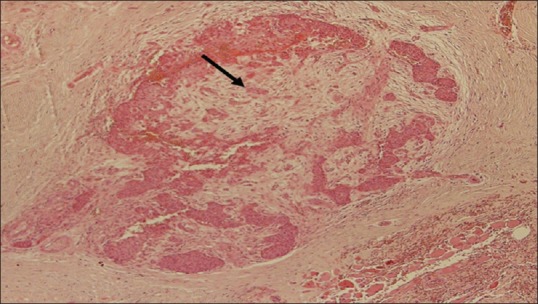
Microphotography of the specimen Hematoxylin and Eosin staining 10X magnification. Showed lobules with areas of myxomatous connective tissue, with islands of epithelioid cells (black arrow). The myxomatous areas showed spindle and stellate cells and small blood vessels
Figure 13.
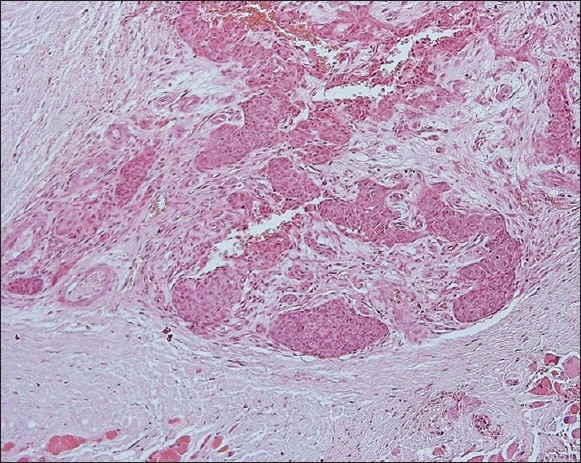
Microphotography of the specimen Hematoxylin and Eosin staining 40X magnification
DISCUSSION
CF is rare and represents <1% of all bone tumors. It generally appears in the second and third decade of life and most frequent in men. The lesion's most frequent location is in the proximal tibia and the distal femur, and it is rarely seen in the maxillofacial region, in the jaws, the neoplasm typically occurs in the mandible. Only three cases involving the zygomatic bone have been reported.[2,4,5] However, we have presented the case of a 68-year-old patient, considerably older than what is established in the literature.
It is clinically characterized by an insidious pain and increased volume in the affected region, as was the case with our patient, where the pain was the main symptom and the increased volume was not very significant. On occasions, the tumor can by asymptomatic and discovered in routine X-rays. Pathological fractures are very rare. The radiographic description is that of a radiolucent lobulated lesion from 1 to 10 cm diameter and an average of 3 cm, with scalloped and defined edges. Some 10% of CF have interior calcification, and there is rarely destruction of cortical bone or an infiltration of neighboring soft tissue.[3]
Microscopically, a great amount of variability in presentation might be seen. Classically it presents itself as a lobular tissue with stellated or spindle-shaped cells in a myxoid or chondroid tissue. The lesion's lobules have a hypocellular center, a hypercellular periphery, and abundant blood vessels.[6,7] Frank hyaline cartilage foci are rare, only a few tumors show calcification or mineralization and only 19% of the cases of FC have hyaline cartilage.[3,4] In this case, the lesion did not have any hyaline cartilage.
The ideal treatment for this tumor is total surgical removal of the lesion and, given that in this case it was located in a facial bone, reconstruction must be undertaken in the same surgical act. For this same reason, many authors recommend just a curettage and strict follow-up of patients to avoid the esthetic side effects of total tumor removal. However, the literature describes a 25% recurrence rate with this treatment, meaning that the ideal treatment is the total resection of the lesion and the subsequent reconstruction of the defect.[2]
The zygomatic bone is a fundamental part of the facial architecture. Its anatomy is directly related to the width of the face, with an adequate anteroposterior projection of the middle third, meaning that surgical resection of this bone, due to a tumor or trauma, can end in considerable esthetic and functional side effects if it is not properly reconstructed. The literature offers different alternatives for zygomatic reconstruction, such as gold prosthetics, hydroxyapatite rib grafts, iliac crest grafts and calvarial bone grafts.[8,9] The latter of these is very widely used due to the ease with which they can be harvested, but they also have high levels or reabsorption that could compromise the esthetic result. In this case, we preferred to use osteosynthesis plates for reconstruction to restore bone continuity and an alloplastic biocompatible porous high-density polyethylene alloplast to restore the malar anatomy.
The patient's initial consultation was with a diagnosis of odontogenic myxoma, and we believe that this confusion in the histopathological diagnosis could be due to the existence of myxomatous tissue and a cell morphology consistent with myxoma, as in both lesions the cells can be spindle-shaped in a myxoid stroma. Odontogenic myxoma originates in the dental papillae, the dental follicle or the periodontal ligament and, therefore, it is a tumor that is exclusive of the maxillary bones, which immediately ruled out that possibility.[10]
We identified chondrosarcoma and chondroblastoma as differential diagnoses of the lesion. It is important to distinguish it from these lesions, as 22–28% of CF cases correspond to a mistaken diagnosis.[4] Some of CF's traits like its radiographic presentation and the lesion's histology help us to differentiate it from a chondrosarcoma. Radiographically, chondrosarcoma presents itself as a radiolucent area with several radiopaque regions with pointed forms or in ring shapes. There is usually cortical erosion or destruction. Histologically, CF is comprised of lobules separated by fibrous tissue and has a defined border between the tumor and the healthy tissue, in contrast to chondrosarcoma, which has irregular lobules that can be separated by fibrous bands or impregnate the bone trabeculae.[3] Chondroma and chondroblastoma are also differential diagnoses that can be considered in this case and they can be distinguished from CF with immunohistochemistry studies.
CF is a benign cartilaginous tumor that is generally located in long bones and rarely in the maxillofacial region. Only three cases of CF in the zygomatic region have been previously reported in the literature. This lesion should be considered one of differential diagnosis in the case of craniofacial bone tumors, despite the fact that it is an uncommon lesion. It is important that an adequate diagnosis is made, as there is a need to differentiate it from a malign tumor-like chondrosarcoma, which has a totally different prognosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Dr. Benjamín Martínez, Professor in Oral and Maxillofacial Pathology, for his selfless support on the diagnosis and histopathological aspect of this particular case.
REFERENCES
- 1.Hammad HM, Hammond HL, Kurago ZB, Frank JA. Chondromyxoid fibroma of the jaws. Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;85:293–300. doi: 10.1016/s1079-2104(98)90011-7. [DOI] [PubMed] [Google Scholar]
- 2.Bucci T, Dell’Aversana Orabona G, Insabato L, Califano L. Chondromyxoid fibroma of the zygoma: A case report. Int J Oral Maxillofac Surg. 2006;35:569–71. doi: 10.1016/j.ijom.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 3.Fletcher CD, Unni KK, Mertens F. World Health Organization Classification of Tumors. Lyon, France: IARC Press; 2002. pp. 243–7. [Google Scholar]
- 4.Sudhakara M, Bavle RM, Srinath N, Paremala K. Chondromyxoid fibroma of zygoma: A rare case report. J Oral Maxillofac Pathol. 2014;18:93–6. doi: 10.4103/0973-029X.131924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carr NJ, Rosenberg AE, Yaremchuk MJ. Chondromyxoid fibroma of the zygoma. J Craniofac Surg. 1992;3:217–22. doi: 10.1097/00001665-199212000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Budny AM, Ismail A, Osher L. Chondromyxoid fibroma. J Foot Ankle Surg. 2008;47:153–9. doi: 10.1053/j.jfas.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Fomete B, Adeosun OO, Awelimobor DI, Olayemi L. Chondromyxoid fibroma of the mandible: Case report and review of the literature. Ann Maxillofac Surg. 2014;4:78–80. doi: 10.4103/2231-0746.133072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Khayat B, Eley KA, Shah KA, Watt-Smith SR. Ewings sarcoma of the zygoma reconstructed with a gold prosthesis: A rare tumor and unique reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e5–e10. doi: 10.1016/j.tripleo.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Hirano S, Shoji K, Kojima H, Omori K. Use of hydroxyapatite for reconstruction after surgical removal of intraosseous hemangioma in the zygomatic bone. Plast Reconstr Surg. 1997;100:86–90. doi: 10.1097/00006534-199707000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Limdiwala P, Shah J. Odontogenic myxoma of maxilla: A review discussion with two case reports. Contemp Clin Dent. 2015;6:131–6. doi: 10.4103/0976-237X.149310. [DOI] [PMC free article] [PubMed] [Google Scholar]


