Abstract
Leiomyosarcoma (LMS) of the larynx is a very rare malignancy that originates from blood vessel, smooth muscle or from the heterotopic mesenchymal tissue in the larynx. The histological diagnosis of LMS depends on the immunohistochemical investigation. The case is here presented of an 82-year-old man with shortness of breath and hoarseness. Indirect laryngoscopy showed a pedunculated large glottic lesion causing airway obstruction. Direct laryngoscopy was performed and biopsies were taken. From the pathological examination, the diagnosis of LMS was made. This case is presented of laryngeal LMS with the clinical, radiological, and histological findings.
Keywords: Glottis, laryngoscopy, larynx, leiomyosarcoma
INTRODUCTION
Laryngeal carcinoma (LC) constitutes 50% of all head and neck cancers. Squamous cell carcinoma accounts for 95–98% of LC.[1] Sarcomas form a very small proportion of laryngeal malignancies with similar clinical findings.[2] Less than 1% of LCs are sarcomas.[3] Leiomyosarcoma (LMS) originates from smooth muscle and represents 5–6% of all soft-tissue sarcomas.[1] Laryngeal LMS (LLMS) is extremely rare.[2] The challenging histological diagnosis of LLMS depends on immunohistochemical investigation. A rare case of LLMS is presented here with clinical and histological findings.
CASE REPORT
An 82-year-old male presented to our clinic with complaints of shortness of breath and hoarseness which had been ongoing for 2 weeks. The patient had a medical history of ischemic heart disease and coronary angiography but no previous surgery. Indirect laryngoscopy showed a pedinculated large glottic lesion in the left vocal cord causing airway obstruction and an elective tracheotomy and direct laryngoscopy was recommended for the patient [Figure 1a]. There was no palpable lymphadenopathy in the neck examination. The patient did not accept the procedure. After 1 day, he presented again with a piece of tissue that had exported with a severe cough. The pathological examination of the exported tissue revealed the diagnosis of suspected LMS of the larynx. A new indirect laryngoscopy showed a glottic lesion that was holding the left vocal cord length-wise without the pedunculated part [Figure 1b]. Computed tomography (CT) showed an oval-shaped hypodense lesion extending into the rima glottis from the left vocal cord [Figure 2].
Figure 1.
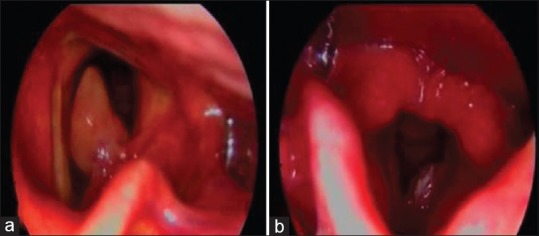
(a) Indirect laryngoscopy showed a pedunculated large glottic lesion in the left vocal cord causing airway obstruction. (b) A glottic lesion holding the left vocal cord length-wise without the pedunculated part
Figure 2.
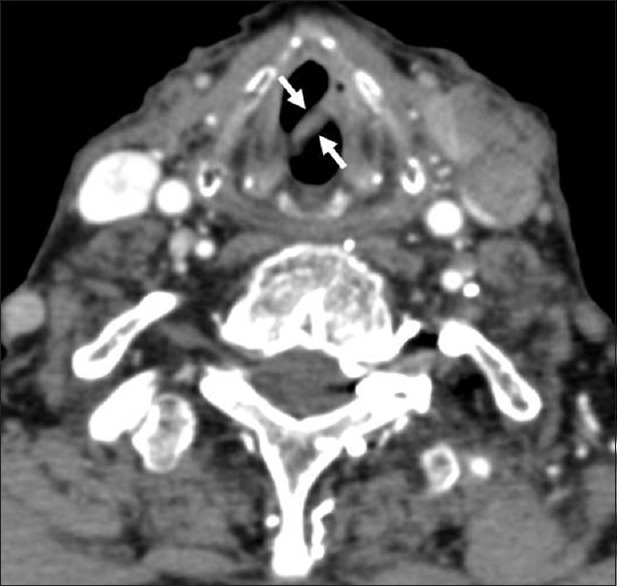
Oval-shaped hypodense lesion of the left vocal cord extending to the lumen shown in axial computed tomography sections
Direct laryngoscopy and stripping was performed without tracheostomy. In the pathological examination, a polypoid lesion covered with a mucous membrane surface of 1.5 cm × 1 cm × 1 cm in size was observed macroscopically. The cut surface showed a pale white. An intersecting bundle of long elongated spindle cells with blunt-ended nuclei and a focal necrosis area with a common surface ulcer of the epithelium were observed microscopically. Mild pleomorphism was seen and 22 mitosis were counted in 10 HPF. The case was commissioned by immunohistochemistry for vimentin-positive, smooth muscle paint (SMA) strongly positive, desmin focally positive, S-100 negative, CD31 negative, weak positive for anaplastic lymphoma kinase, pankeratin negative, epithelial membrane antigen negative, and the Ki-67 proliferation index was 18–20% [Figure 3]. From the results of the immunohistochemical staining together with the histopathological findings, the case was evaluated as low-grade LMS. The patient did not approve any further treatment. Informed consent was obtained from the patient for this case presentation.
Figure 3.
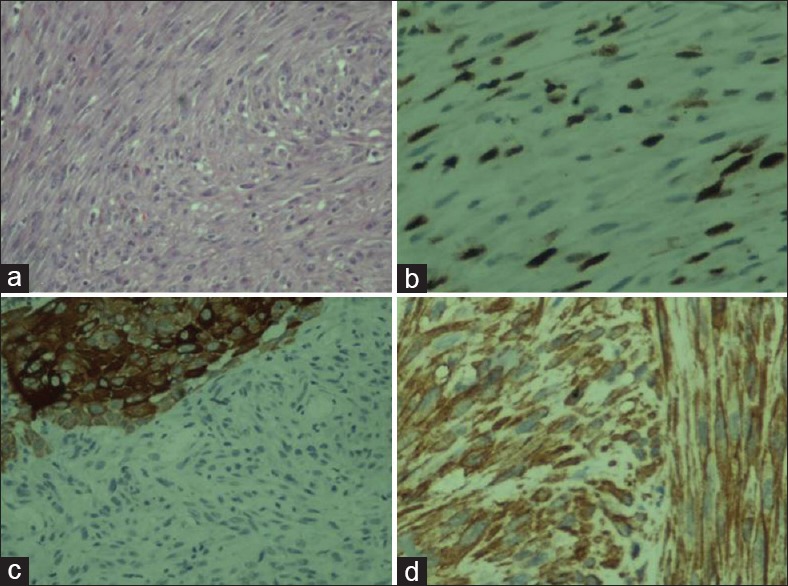
(a) Overall appearance of the tumor. H and E, ×20, (b) Panck, ×10. The remaining squamous epithelium covering the surface of the tumor stained Panck positive, tumor Panck negative. (c) Smooth muscle paint, ×4, smooth muscle paint stained leiomyosarcoma and not stained squamous epithelium. pedunculated, shows positive cytoplasmic staining (d) Ki-67, ×40, proliferation index and large number of nuclear staining is seen in large magnification
DISCUSSION
LC is the most frequently seen carcinoma of the head and neck carcinomas. Squamous cell carcinomas are the majority of these tumors. Sarcomas account for <1% of all head and neck malignancies.[3] LMS mostly originates in regions such as the uterus, the gastrointestinal tract and the retroperitoneum where there is a predominance of smooth muscle.
Head and neck LMS account for 3% of all LMSs.[2] The most common head and neck regions are the oral cavity, the sinonasal region, the scalp, the neck, the orbit and the cervical esophagus.[1,2] Sarcomas form a very small proportion of laryngeal malignancies, accounting for 1% of all head and neck tumors.[2] Sarcomas of the larynx include fibrosarcomas, chondrosarcomas, rhabdomyosarcomas, osteosarcomas, LMS, and hemangiosarcomas.[4] Chondrosarcoma is the most common sarcoma of the larynx.[1]
LLMS is a very rare entity. Since the first LLMS case was reported in 1939, fewer than 50 cases have been published.[2,5]
Sarcomas mostly occur in the fifth decade in the head and neck region.[6] Although LLMS may appear even in childhood, the peak incidence is in the fifth decade.[7] Previously, the ratio of males to females has been reported as 4:1.[5] The current case was an 82-year-old male.
There are some predisposing factors for the presence of sarcomas such as radiation exposure, surgery, tuberous sclerosis, neurofibromatosis, Werner syndrome, Gardner syndrome, retinoblastoma, multiple basal cell carcinoma syndrome, Turcot syndrome, and Epstein–Barr virus infection in immunosuppressed patients.[3,8,9] The current patient did not have any known predisposing factor for the development of LLMS.
LLMS originates mostly in the supraglottic or glottic area. In a previous study of 31 patients, LLMS presence in the larynx was reported as glottis (48%), supraglottis (32%), and supraglottis-glottis (6.5%).[10] Similarly, the current case had a pedunculated large glottic lesion in the left vocal cord causing airway obstruction.
The diagnosis of LLMS is difficult clinically as these lesions are clinically indistinguishable from other LCs.[2] The clinical presentation of LLMS is like other laryngeal tumors with progressive hoarseness, dyspnea, and dysphagia.[1] The reported duration of the symptoms may vary from weeks to years.[6] In the current case, the symptoms of shortness of breath and hoarseness had been present for 2 weeks before the initial diagnosis. LLMS can present with obstructive features that may require an emergency laryngectomy or emergency tracheostomy.[2,11] The patient presented here also had a pedinculated large glottic lesion in the left vocal cord causing obstructive complaints, which were revealed after a severe cough.
The histological type, the grade of the sarcoma and the presence of metastasis affect prognosis and the treatment.[6] Head and neck LMS s rarely metastasize to the lymph nodes.[2] The current patient did not have metastasis to the lymph nodes. Metastases are usually not seen initially. The most common metastatic sites are the lung, liver, bone, brain, and skin.[6] As the current patient refused any further treatment or investigation of the disease, there is no information available about metastasis.
CT and magnetic resonance imaging, provide adjunctive information as they show the local extent and the size of the tumor as well as giving information regarding the lymph node status and the vascular component of the lesion.[5] In this case, CT was used for the initial evaluation.
Differential diagnosis of LLMS may be difficult with small biopsies.[9] An accurate histological diagnosis depends on electron microscopy and immunohistochemical tests. Generally, it contains 5 or more mitotic figures in 10 HPF. Necrosis is usually seen. Leiomyocytes express SMA, desmin, and vimentin and S-100 are usually negative. Spindle cell tumors such as rhabdomyosarcoma, melanoma, schwannoma, malignant fibrous histiocytoma and sarcomatoid carcinoma are in the list of differential diagnosis.[2]
Surgery is the primary choice of treatment for LLMS.[5] Surgery performed with wide surgical margins and with tumor-free margins provides the best prognosis.[12,13] In the current case, surgery was also used for the diagnosis with stripping applied to the glottic lesion that was held length-wise on the left vocal cord. The patient did not accept any further treatment. Neck dissection is not routinely performed for sarcomas of the head and neck.[6] Radiotherapy is an adjuvant therapeutic modality that may have a role in recurrence or in residual disease but is less effective as a primary treatment modality and chemotherapy also has a limited role.[2]
CONCLUSION
LLMS is a very rare malignancy that can clinically mimic squamous cell carcinoma. This case is interesting as a part of a pedinculated large glottic that was exported with a severe cough. Aspiration could be a risk for these patients. Due to the risk of recurrence, a long period of follow-up is mandatory after treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Skoulakis CE, Stavroulaki P, Moschotzopoulos P, Paxinos M, Fericean A, Valagiannis DE. Laryngeal leiomyosarcoma: A case report and review of the literature. Eur Arch Otorhinolaryngol. 2006;263:929–34. doi: 10.1007/s00405-006-0092-0. [DOI] [PubMed] [Google Scholar]
- 2.Khadivi E, Taziky MH, Jafarian AH, Nasseri Sadr M. Laryngeal leiomyosarcoma, a case report and review of articles. Iran J Otorhinolaryngol. 2013;25:253–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Eeles RA, Fisher C, A’Hern RP, Robinson M, Rhys-Evans P, Henk JM, et al. Head and neck sarcomas: Prognostic factors and implications for treatment. Br J Cancer. 1993;68:201–7. doi: 10.1038/bjc.1993.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tran LM, Mark R, Meier R, Calcaterra TC, Parker RG. Sarcomas of the head and neck. Prognostic factors and treatment strategies. Cancer. 1992;70:169–77. doi: 10.1002/1097-0142(19920701)70:1<169::aid-cncr2820700127>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 5.Morera Serna E, Pérez Fernández CA, de la Fuente Jambrina C, Razquin Muñoz J, Pérez Gil MA. Laryngeal leiomyosarcoma. Acta Otorrinolaringol Esp. 2007;58:445–8. [PubMed] [Google Scholar]
- 6.Helmberger RC, Croker BP, Mancuso AA. Leiomyosarcoma of the larynx presenting as a laryngopyocele. AJNR Am J Neuroradiol. 1996;17:1112–4. [PMC free article] [PubMed] [Google Scholar]
- 7.Timmons CF, Dawson DB, Richards CS, Andrews WS, Katz JA. Epstein-Barr virus-associated leiomyosarcomas in liver transplantation recipients. Origin from either donor or recipient tissue. Cancer. 1995;76:1481–9. doi: 10.1002/1097-0142(19951015)76:8<1481::aid-cncr2820760828>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 8.Dijkstra MD, Balm AJ, Gregor RT, Hilgers FJ, Loftus BM. Soft tissue sarcomas of the head and neck associated with surgical trauma. J Laryngol Otol. 1995;109:126–9. doi: 10.1017/s0022215100129457. [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Loh KS, Petersson F. Epstein-barr virus-associated smooth muscle tumor of the larynx: Report of a rare case mimicking leiomyosarcoma. Head Neck Pathol. 2010;4:300–4. doi: 10.1007/s12105-010-0201-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marioni G, Bertino G, Mariuzzi L, Bergamin-Bracale AM, Lombardo M, Beltrami CA. Laryngeal leiomyosarcoma. J Laryngol Otol. 2000;114:398–401. doi: 10.1258/0022215001905698. [DOI] [PubMed] [Google Scholar]
- 11.Tewary AK, Pahor AL. Leiomyosarcoma of the larynx: Emergency laryngectomy. J Laryngol Otol. 1991;105:134–6. doi: 10.1017/s0022215100115166. [DOI] [PubMed] [Google Scholar]
- 12.Abbas A, Ikram M, Yaqoob N. Leiomyosarcoma of the larynx: A case report. Ear Nose Throat J. 2005;84:435–6. [PubMed] [Google Scholar]
- 13.Darouassi Y, Bouaity B, Zalagh M, Rimani M, Abrouq A, Azendour B. Laryngeal leiomyosarcoma. B-ENT. 2005;1:145–9. [PubMed] [Google Scholar]


