Abstract
Killian polyp is predominantly found in children and any sinonasal tumor in elderly presenting with epistaxis and pain usually indicates malignant growth until proved otherwise. We present an unusual case of Killian polyp in an elderly patient that behaved as a malignant tumor. This case report reminded us that paranasal sinuses are still dark hollow mysterious cavities, and we should take utmost clinical acumen in managing such cases.
Keywords: Antrochoanal polyp, cancer, endoscopy, maxilla, polyp
INTRODUCTION
Inflammatory or allergic nasal polyps are commonly encountered in ENT, and diagnosis is easily achieved on clinical history and examination. High-resolution computed tomography (CT) scan is mandatory for endoscopic sinus surgery and shows homogenous soft tissue in sinus, nasal cavity, and/or nasopharynx. The bony landmarks are well preserved, and any erosion indicates fungal or malignant growth. However, this case report contradicts this statement where polyp represented as malignant growth both clinically and radiologically.
CASE REPORT
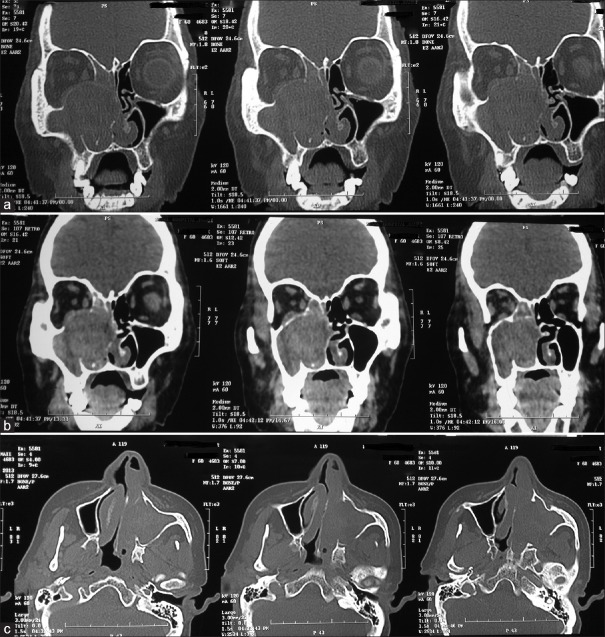
A 60-year-old female was referred to us by an ENT specialist with provisional diagnosis of malignant maxillary tumor. The patient had progressive nasal obstruction and discharge from left nostril for the last 6 months. There were occasional episodes of epistaxis from left nostril. She also had mild left facial pain and headache with no other relevant history. Anterior rhinoscopy found deviated nasal septum and a grayish-white mass in the left middle meatus area that appeared to be arising from lateral wall. The mass was painless but bled on probing. Oral cavity, posterior rhinoscopy, eye, and neck were found normal. The patient had been subjected to CT scan by the specialist [Figure 1a-c] that showed a large well-defined, mildly enhancing heterogeneous lesion in the left maxillary antrum, with minimal extensions into the infratemporal fossa. The tumor had eroded and destroyed medial, posterior, and superior walls of the maxilla. It was also extending into the orbit and abutting the inferior rectus muscle. Hematological and biochemical investigations were normal. CT scan review by radiology department of our hospital endorsed the possibility of malignant maxillary tumor kept initially.
Figure 1.
(a-c) Coronal and axial sections of computed tomography scan showing heterogeneous tumor in left maxillary sinus extending beyond medial, posterior, and superior walls
We took punch biopsy of nasal mass under local anesthesia. Histopathological examination found benign respiratory epithelium-lined fibrocollagenous tissue. It was densely infiltrated by lymphocytes, plasma cell, and contained seromucinous glands with duct lining epithelium showing squamous metaplasia [Figure 2a-d]. However, studied specimen showed no evidence of malignancy. Due to strong possibility of malignant tumor, a repeat endoscopic biopsy was performed under general anesthesia. The procedure encountered hemorrhagic, friable tumor that was removed almost completely from the antrum, so as to provide maximum tissue to pathologist. In postoperative period, we started counseling and preparing the patient for total maxillectomy. However, surprisingly, histopathology had features of inflammatory polyp with squamous metaplasia. There was no evidence of malignancy in the excised specimen. Based on this report, the patient was advised for repeat endoscopic examination and CT scan after 6 weeks. Follow-up endoscopic examination found wide open ostium showing healthy antral mucosa and intact walls. CT scan [Figure 3] showed normal intact maxillary sinus with no evidence of extra-antral tissue as compared to initial scan. The patient was followed-up for 6 months and remained asymptomatic.
Figure 2.
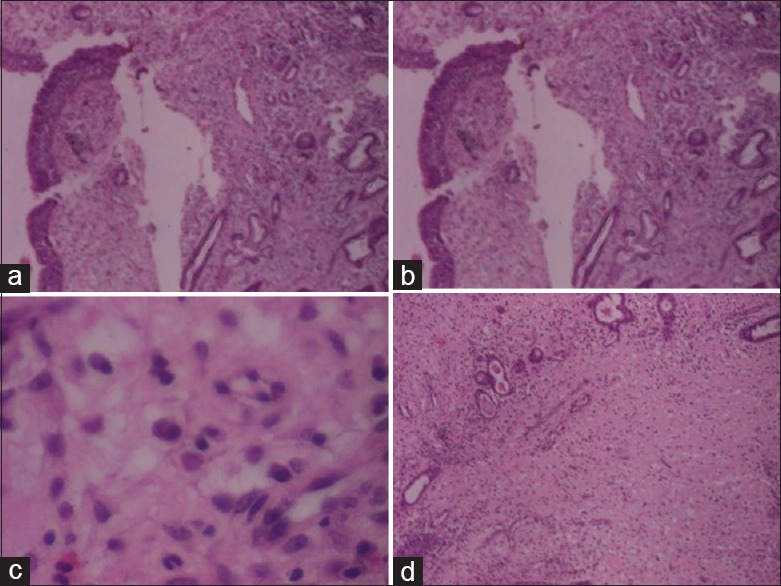
(a-d) Microphotograph of histopathology showing respiratory epithelium with squamous metaplasia in duct epithelium (a,b,d: H and E, X10), (c: H and E, X40)
Figure 3.
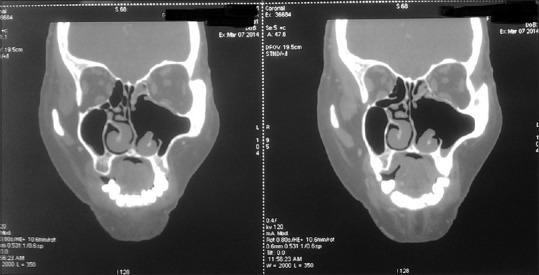
Postoperative computed tomography scan showing wide open ostium with normal maxillary sinus and surrounding structures
DISCUSSION
Sinonasal carcinoma can present as polyp but polyp presenting as carcinoma is rare.[1,2] Sinonasal malignant tumors are uncommon. They usually present with nasal obstruction, epistaxis, losing of teeth, facial heaviness, and headache. Hyposmia, otalgia, visual disturbance, and neck node are late features of such tumors. Clinical examination shows painless, hemorrhagic tumor in nasal cavity, facial fullness, proptosis, or neck node. Latest radiological investigations easily depict hallmark findings of malignant tumors.
Killian's (antrochoanal) polyp is usually unilateral and found in children suffering with long-standing rhinosinusitis. It is painless (unless infective), sessile mass found in nasal cavity and/or nasopharynx. Epistaxis is rare and usually due to superadded infection. A polyp is confined to antrum, and polyp shows widened ostiomeatal complex without bony erosion is a hallmark finding on CT scan. These polyps can cause thinning and remodeling of sinus walls. We found mild enhanced heterogeneous soft tissue in maxilla with bony erosions and extension beyond sinus. In our opinion, extensive thinning and remodeling of bony walls lead to loss of bony attenuation on CT scan that mislead radiologist in favor of malignant tumor, and hence, magnetic resonance imaging should have been the investigation of choice in this dilemma. Inflammatory pseudotumor is a rare sinonasal tumor that mimic malignant tumor as it has propensity to erode bony walls.[3,4,5,6,7] Histopathologically, it is a myofibroblastic tumor that has numerous inflammatory cells. It treated by corticosteroids, but refractory cases require surgical excision.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Tritt S, McMains KC, Kountakis SE. Unilateral nasal polyposis: Clinical presentation and pathology. Am J Otolaryngol. 2008;29:230–2. doi: 10.1016/j.amjoto.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 2.Minhas RS, Thakur JS, Sharma DR. Primary schwannoma of maxillary sinus masquerading as malignant tumour. BMJ Case Rep 2013. 2013 doi: 10.1136/bcr-2013-009267. pii: Bcr2013009267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karakök M, Ozer E, Sari I, Mumbuç S, Aydin A, Kanlikama M, et al. Inflammatory myofibroblastic tumor (inflammatory pseudotumor) of the maxillary sinus mimicking malignancy: A case report of an unusual location (is that a true neoplasm?) Auris Nasus Larynx. 2002;29:383–6. doi: 10.1016/s0385-8146(02)00024-x. [DOI] [PubMed] [Google Scholar]
- 4.Thomas L, Uppal HS, Kaur S, David VC. Inflammatory pseudotumour of the maxillary sinus presenting as a sino-nasal malignancy. Eur Arch Otorhinolaryngol. 2005;262:61–3. doi: 10.1007/s00405-004-0750-z. [DOI] [PubMed] [Google Scholar]
- 5.Amin M, Ali R, Kennedy S, Timon C. Inflammatory myofibroblastic tumor of the nose and paranasal sinuses masquerading as a malignancy. Ear Nose Throat J. 2012;91:E1–3. doi: 10.1177/014556131209100513. [DOI] [PubMed] [Google Scholar]
- 6.Chong S, Teh C, Shashinder S, Mun KS, Viswaraja S. Aggressive inflammatory pseudotumor of the maxillary sinus and orbit. Ear Nose Throat J. 2014;93:108–11. [PubMed] [Google Scholar]
- 7.Segawa Y, Yasumatsu R, Shiratsuchi H, Tamae A, Noda T, Yamamoto H, et al. Inflammatory pseudotumor in head and neck. Auris Nasus Larynx. 2014;41:321–4. doi: 10.1016/j.anl.2013.11.002. [DOI] [PubMed] [Google Scholar]