Abstract
The knowledge of both normal and abnormal anatomy of the veins of the neck is important for clinicians performing catheterization and surgeons operating in the region of the neck. The presence of such anomalous communications may also be important for radiologists performing angiographic and sonographic studies. This study presents three cases of variant anatomy in posterior branching and abnormal branching of internal jugular vein found during our routine neck dissection.
Keywords: Common carotid artery, internal jugular vein, modified radical neck dissection, selective neck dissection
INTRODUCTION
Variation in the vascular system from its usual pattern is a common feature and is more commonly observed in veins than arteries.[1] Internal jugular vein being the principle vein supplying to the head and neck area, descends from the posterior portion of the jugular foramen having a superior and inferior bulb in the base skull and neck region. From the base of the skull to the neck, it lies lateral to the internal carotid and common carotid artery, between these two structures hypoglossal and spinal accessory nerve pass and continue to descend downward to join the subclavian vein. The left jugular vein is usually smaller than the right side vein.
This vein receives in its course the inferior petrosal sinus, the common facial, lingual, pharyngeal, superior, and middle thyroid veins and sometimes the occipital vein. The thoracic duct on the left side and the right lymphatic duct on the right side open into the angle of union of the internal jugular and subclavian veins.[2] All these arise from the anterior surface in the neck and most of the times it does not gives the posterior branches, this is the important finding which makes neck dissection in the posterior triangle easier; however, in some cases, it gives out posterior branches and may have duplication of the vein. We present our three cases with posterior branching, trifurcation of vein at its superior end, and bifurcation of vein with common carotid artery in between the bifurcation.
CASE REPORTS
Three female patients in the age group of 35-50 years with squamous cell carcinoma of the oral cavity, tumour size of T3-T4 were planned for selective neck dissection (level-I to level-III node removal) as a staging procedure and modified radical neck dissection for carcinoma of tongue.
For selective neck dissection, a utility flap was designed to elevate the subplatysmal flap over the neck to expose the intended operating field. Greater auricular nerve running over sternocleidomastoid was preserved; superficial layer of deep cervical fascia was dissected to expose sternocleidomastoid muscle and retracted laterally to expose the internal jugular vein and level-II and III nodes. Level I-III nodes were removed. External jugular vein and spinal accessory nerve were preserved in all the cases.
In case of modified radical neck dissection, sternocleidomastoid muscle was removed along with lymph node clearance from level I-V. Spinal accessory nerve and internal jugular vein were preserved.
Case 1
A 45-year-old female reported to the department with non healing ulcer over the left lower gingivobuccal sulcus, measuring around 2-3 cm and there were no palpable nodes. Patient was not having any systemic complications; case was posted for elective neck dissection with hemimandibulectomy as the tumor was involving the mandible on radiograph.
A subplatysmal flap was elevated, anterior border of sternocleidomastoid muscle dissected and retracted laterally to expose internal jugular vein and level III node above the level of omohyoid muscle. On removal of the fascia over internal jugular vein, there was branching of internal jugular vein above the level of omohyoid muscle, the anterior branch was giving superior and middle thyroid vein and forming common facial vein as shown in [Figure 1] and the posterior branch passing bellow the posterior belly of digastrics muscle.
Figure 1.
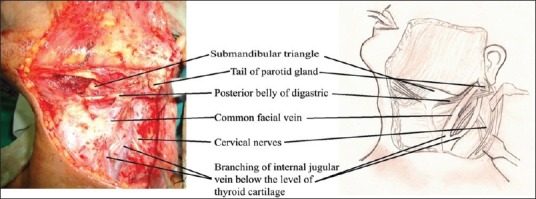
Internal jugular vein branching above the level of omohyoid muscle
Case 2
A 53-year-old female patient was planned for modified radical neck dissection for carcinoma of left lateral tongue. After flap elevation and dissection of jugular vein, there was trifurcation of internal jugular vein at the level of thyroid cartilage two branches were passing bellow the posterior belly of digastrics while anterior branch forming common facial vein [Figure 2].
Figure 2.
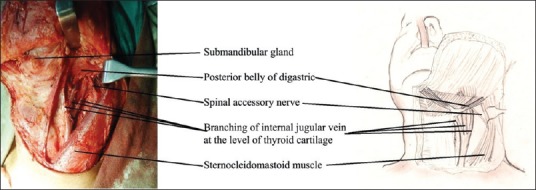
Trifurcation of internal jugular vein at the level of thyroid cartilage
Case 3
In a case planned for selective neck dissection for carcinoma of left lower gingivobuccal sulcus, it was seen that after elevation of subplatysmal flap and dissection around the internal jugular vein, there was posterior branching of internal jugular vein above the level of inferior belly of omohyoid muscle, the posterior branch was entering deep to the anterior border of trapezius muscle [Figure 3].
Figure 3.
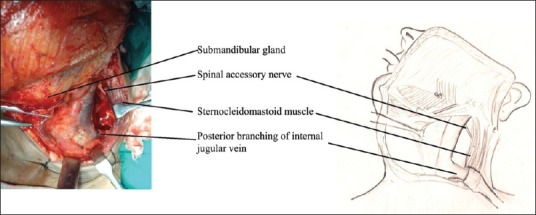
Posterior branching of internal jugular vein above the level of inferior belly of omohyoid muscle
DISCUSSION
Varying venous patterns in the region of head and neck is important for the surgeons in order to avoid any intraoperative trial and error procedures which might lead to unnecessary bleeding. Various articles have been reported regarding the anomalies of the internal jugular vein. Churchman[3] reported double internal jugular vein running parallel to each other found during his routine operation for the removal of the tuberculous gland.
Paolo et al.,[4] reported bifurcation of the right internal jugular vein, about 2 cm from the jugular foramen. Both branches of the internal jugular vein had the same thickness and poured into the right subclavian vein. The anterior branch was parallel to the carotid artery and received the common facial vein, the superior and inferior thyroid veins, and the transverse cervical vein. The posterior branch passed within the carotid sheath, drained only the cerebral blood, and emptied into the subclavian vein lateral to the medial branch.
Asouhidou et al.,[5] compared the dimensions of the internal jugular vein with the dimensions of the external jugular vein and common carotid artery in 186 cadaver neck side. They reported that the external jugular vein was larger than normal in three cases where the diameter of the internal jugular vein was smaller than 6 mm.[5] In another study performed on cadaver by Devi Sankar and Sharmila Banu[6] noticed a case with Internal Jugular Vein fenestrated in the upper part and rejoined in the lower part to form a single trunk; however, there was no duplication of the Internal Jugular Vein. Similar studies conducted by Lalwani et al.,[7] reported a case with communication of the external and internal jugular vein in 45-year-old male cadaver.
Lim et al.,[8] studied anatomical variations of the internal jugular veins and their relationship to the carotid arteries based on the computed tomography findings and found that the right IJV (80.5%) was more often larger than the left IJV. With reference to the Common Carotid Artery, 85.2% of the IJV were found in the lateral position, 12.5% anteriorly, 1.1% medially, and 1.1% posteriorly. Seven IJV were found to be hypoplastic and in one case this was seen bilaterally in both the right and left IJV. The maximum depth of IJV from the skin was 27.9 mm. More than half (69.5%) of the IJV were less than 1 mm from the carotids.
The jugular veins are important for any ligations which are to be performed during radical neck dissection surgeries. The jugular veins are often used for catheterization and prior anatomical knowledge is needed before such procedures. Awareness of these variations is important for the surgeons to prevent accidental injury and bleeding from the vein.[6] Color Doppler sonography is essential for detecting collateral pathways Conkbayir et al.[9]
CONCLUSION
Knowledge of variations in the anatomy of internal jugular veins of the face and neck is of immense importance both clinically and surgically. Awareness of these variations is important for the surgeons to prevent accidental injury and bleeding from the vein; further, more awareness of these types of variations will also help to avoid radiologic misinterpretations or misidentifications of the veins of neck during the conventional radiographic procedures like angiography and catheterization or hemodialysis in renal failure patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hollinshead WH. Anatomy for Surgeons. 3rd ed. Vol. 3. Jagerstown: Harper and Row; 1982. pp. 467–70. [Google Scholar]
- 2.Gray’s Anatomy. The Anatomical Bases of Medicine and Surgery. 38th ed. pp. 1579–80. [Google Scholar]
- 3.Churchman JW. Double internal jugular vein-high bifurcation of common carotid artery. Ann Surg. 1915;61:235–236.1. doi: 10.1097/00000658-191502000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Paolo B, Giuseppe C, Giulio G, Gianpaolo T, Raffaele R. Internal jugular vein duplication. Indian J Plast Surg. 2009;42:273–4. doi: 10.4103/0970-0358.59303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Asouhidou I, Natsis K, Asteri T, Sountoulides P, Vlasis K, Tsikaras P. Anatomical variation of left internal jugular vein: Clinical significance for an anaesthesiologist. Eur J Anaesthesiol. 2008;25:314–8. doi: 10.1017/S0265021508003700. [DOI] [PubMed] [Google Scholar]
- 6.Sankar KD, Bhanu PS. Variant anatomy of fenestrated internal jugular vein with unusual retromandibular and facial vein. Int J Anat Var. 2011;4:144–8. [Google Scholar]
- 7.Wen Y, Zhou S, Wang C. Compensation of external jugular vein to the reflux of cerebral blood after bilateral ligation of the internal jugular vein. Zhonghua Kou Qiang Yi Xue Za Zhi. 2000;35:64–6. [PubMed] [Google Scholar]
- 8.Lim CL, Keshava SN, Lea M. Anatomical variations of the internal jugular veins and their relationship to the carotid arteries: A CT evaluation. Australas Radiol. 2006;50:314–8. doi: 10.1111/j.1440-1673.2006.01589.x. [DOI] [PubMed] [Google Scholar]
- 9.Conkbayir I, Men S, Yanik B, Hekimoglu B. Color Doppler sonographic finding of retrograde jugular venous flow as a sign of innominate vein occlusion. J Clin Ultrasound. 2002;30:392–8. doi: 10.1002/jcu.10081. [DOI] [PubMed] [Google Scholar]


