Abstract
Study Design.
Systematic review.
Objective.
This systematic review examines validity and responsiveness of three generic preference-based measures in patients with low back pain (LBP).
Summary of Background Data.
LBP is a very common incapacitating disease with a significant impact on health-related quality of life (HRQoL). Health state utility values can be derived from various preference-based HRQoL instruments, and among them the most widely ones are EuroQol 5 dimensions (EQ-5D), Short Form 6 Dimensions (SF-6D), and Health Utilities Index 3 (HUI III). The ability of these instruments to reflect HRQoL has been tested in various contexts, but never for LBP populations.
Methods.
A systematic search on electronic literature databases was undertaken to identify studies of patients with LBP where health state utility values were reported. Records were screened using a set of predefined eligibility criteria. Data on validity (correlations and known group methods) and responsiveness (effect sizes, standardized response means, tests of statistical significance) of instruments were extracted using a customized extraction template, and assessed using predefined criteria.
Results.
There were substantial variations in the 37 included papers identified in relation to study design and outcome measures used. EQ-5D demonstrated good convergent validity, as it was able to distinguish between known groups. EQ-5D was also able to capture changes of health states as results of different interventions. Evidence for SF-6D and HUI III was limited to allow an appropriate evaluation.
Conclusion.
EQ-5D performs well in LBP population and its scores seem to be suitable for economic evaluation of LBP interventions. However, the paucity of information on the other instruments makes it impossible to determine its relative validity and responsiveness compared with them.
Level of Evidence: 2
Keywords: EQ-5D, health economics, health policy, HUI III, low back pain, preference-based measures, psychometric characteristics, responsiveness, SF-6D, validity
Low back pain (LBP) is a common health problem. A review of studies published between 1966 and 1998 reported that LBP lifetime prevalence reaches an 84% peak, whereas point prevalence and 1-year prevalence ranges from 12% to 33% and from 22% to 65%, respectively.1
As an incapacitating disease LBP has an important impact on health-related quality of life (HRQoL), making cost-utility analysis (CUA) the preferred economic evaluation for LBP interventions. In CUA, life years gained are weighted for heath state utility values (HSUVs), which are commonly derived from three generic preference-based measures: EuroQol Five Dimensions (EQ-5D), Short Form Six Dimensions (SF-6D), and Health Utility Index Three (HUI III). Preference-based HRQoL instruments typically comprise a descriptive system covering core dimensions of health (e.g., mobility, self-care, usual activities, pain, and anxieties) and an attached value set, which is obtained on the basis of population's relative desire for dimensions of health. These generic measures are claimed to be applicable across all disease areas, therefore representing an important clinical outcome as well as a common currency for health technology assessment.2
These instruments psychometric performance in terms of validity (i.e., reaching the objectives it has been developed for) and responsiveness (i.e., ability to detect changes over time and across participants) has been already tested in different decision contexts, and more precisely in patients with visual disorders,3 cardiovascular diseases,4 cancer,5 rheumatoid arthritis,6 musculoskeletal diseases,7 and multiple sclerosis,8 but not in LBP populations.9 This systematic review aims at covering this gap and establishing whether these instruments use is appropriate in LBP populations. As it is common in similar studies, included articles will not be required to have conducted an assessment of validity and responsiveness themselves, but will contain information from which the instruments performance can be analyzed.
MATERIALS AND METHODS
The study design is a systematic literature review.
Literature Search
Medline, Embase, and Web of Science were investigated using a strategy developed around the four main constructs of the research question: EQ-5D, SF-6D, HUI-III, LBP. Terms searched were derived from Brazier et al,10 Brooks,11 Dolan,12 Fenny et al,13 Hayden et al,14 and Lin et al.15 The searching strategy included synonyms and spelling variations and was refined using truncation, wildcards, phrase search and proximity operators, and adjusted for differences in databases. Related terms such as “validity” or “psychometric characteristics” were not used because of this systematic review objective (this would have been useful in a systematic review of studies assessing the validity of preference-based instruments). No publication date limit was set. All studies published in English or for which a transator was available were considered. As an example, the complete search strategy for MEDLINE (Ovid) is provided in Appendix I.
Study Selection
Relevant records were imported on Refworks and duplicates were removed. Studies were included in the systematic review if they met all the eligibility criteria presented in Table 1.
TABLE 1.
Eligibility Criteria
| Inclusion criteria |
| The study population had LBP |
| The study examined at least one of the three general preference based instrument (EQ5D, SF6D, HUI3) |
| The study reported an estimate of mean score for the preference based instrument/s examined and for a comparator (e.g., disease specific) |
| Exclusion criteria |
| The study focused on a condition other than LBP |
| The study examined LBP with comorbidities |
| Pharmacodynamic and pharmacokinetic studies |
| Presentation at conferences and poster presentation |
Data Extraction
A customized extraction template model was used for the collection of relevant data, including study characteristics (e.g., study design), patients characteristics (e.g., age), type and method of validity assessment (e.g., convergent, correlations), method of responsiveness assessment (e.g., standardize response mean), validity and responsiveness data.
Quality Assessment
Quality was assessed using the COnsesus-based Standards for the selection of health Measurement INstrument (COSMIN) checklist,16 a rating tool to evaluate the methodological quality of studies on measurement properties of health status instruments. For the four psychometric characteristics relevant to the current systematic review (“measurement error,” “hypothesis testing,” “cross cultural validity,” and “responsiveness”) 11 to 18 items per characteristic were analyzed. Each item was assigned one of the four possible scores: “excellent,” “good,” “fair,” or “poor.” The item with the lowest score determined the overall score for the property under investigation.
Assessment of Validity and Responsiveness
Construct validity has been defined as the extent to which an instrument measures what it is intended to measure. Construct validity was analyzed when papers reported on convergent validity (correlation between instruments) and known groups differences detected by instruments.
Responsiveness has been defined as the extent to which an instrument is sensitive to statistically significant changes in health over time or between treatment arms.17 Responsiveness was analyzed when papers reported on tests of statistical significance (TSS), effect sizes (ES), and/or standardize response mean (SRM).
Instruments validity and responsiveness was assessed against a set of hypotheses derived from the literature18–22 (Table 2).
TABLE 2.
Validity and Responsiveness Hypothesis
| Convergent validity |
| Hypothesis 1. A positive and moderate-to-very strong correlation (>0.4) between generic instruments and disease-specific instruments (for those disease-specific instruments measuring improvements through a reduction in the scores a negative correlation is expected) |
| Hypothesis 2. A positive and strong-to-very strong correlation between generic instruments (>0.6) |
| Hypothesis 3. Stronger correlations between generic preference-based instruments and disease-specific instruments than generic preference-based instruments and disease construct-specific instruments |
| Known groups |
| Hypothesis 1. Generic instruments to distinguish between different grades of disability (lower scores at increasing level of disability) |
| Hypothesis 2. Generic instruments to distinguish between groups with disability and groups without disability (lower scores in the presence of disability) |
| Hypothesis 3. Generic instruments to distinguish between men and women (lower scores for women than for men) |
| Hypothesis 4. Generic instruments to distinguish between acute and recurrent LBP (lower scores for acute cases) |
| Test of statistical significance |
| Hypothesis 1. Generic instruments to be able to detect changes because of treatments |
| Hypothesis 2. Generic instruments to be able to detect differences between interventions |
| Hypothesis 3. Generic instruments to be able to detect changes coherent with those reported by other generic or disease-specific measures |
| Standardized response mean and effect sizes |
| Hypothesis 1. SRM and ES to be moderate to strong (>0.5) |
Monotonic correlations were considered very weak between 0 and 0.19; weak between 0.2 and 0.39; moderate between 0.4 and 0.59; strong between 0.6 and 0.79; and very strong between 0.8 and 1.23 Changes in SRM and ES were considered very weak between 0 and 0.19; weak between 0.2 and 0.49; moderate between 0.5 and 0.79; and strong between 0.8 and 1.24
RESULTS
Characteristics of the Included Studies
A total of 739 potentially relevant articles were found. Title and abstract screening excluded 223 and 432 records respectively. After reviewing the articles full text, 37 reports referred to 35 studies were included. The process is described in Figure 1.
Figure 1.
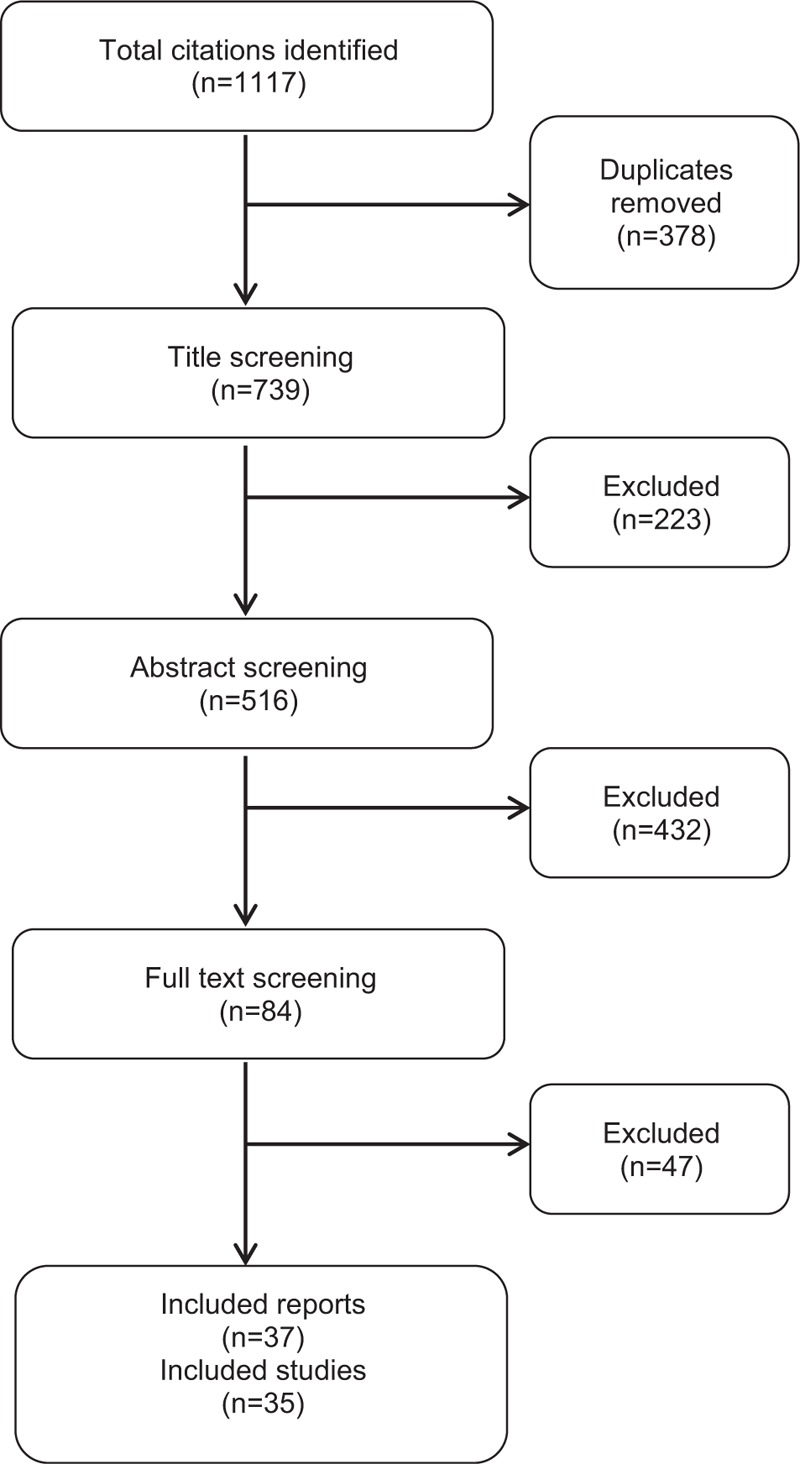
Flow diagram. It represents the screening of the potentially relevant records retrieved with the database search. Thirty-five studies referred to 37 reports were included.
The design feature of included studies varied significantly. The majority of them were randomized controlled trials (RCT),25–41 followed by cross-sectional studies,42–47 observational longitudinal48–58 and cohort studies.59–61
Quality of the Included Papers
Quality scores for the three mostly investigated psychometric characteristics (“measurement error,” “hypothesis testing,” “responsiveness”) varied substantially between studies, with at least one study per characteristic receiving a score of excellent, good, fair, and poor quality. Substantially different scores were seen for different characteristics within the same study. For example, Rivero-Arrias et al40 reported excellent properties for “measurement error,” fair properties for “hypothesis testing” and poor properties for “responsiveness.” In addition to Rivero-Arrias et al,40 only one other study received an assessment of excellent on some of the aspects of methodological quality investigated (Hellum et al)36 and this was for “hypothesis testing” and “responsiveness.” The only two studies for which it was relevant to assess cross-cultural validity received a score of fair (Klemenc-Ketis et al)53 and good (Genevay et al).51Table 3 provides an overview of the quality assessment results for the included studies.
TABLE 3.
Quality of the Included Papers
| Name of the First Author and Year of Publication | Measurement Error | Hypothesis Testing | Cross Cultural Validity | Responsiveness |
| RCTs | ||||
| Bastiaenen et al, 200825 | Good | Poor | n/r | Poor |
| Berg et al, 200926 | Fair | Poor | n/r | Fair |
| Berg et al, 200927 | Fair | Poor | n/r | Fair |
| Carr et al, 200528 | Fair | Poor | n/r | Fair |
| Casserley-Feeney et al, 201229 | Fair | Poor | n/r | Fair |
| Chown et al, 200830 | Fair | Poor | n/r | Fair |
| Cox et al, 201031 | Fair | Poor | n/r | Fair |
| Del Pozo-Cruz et al, 201132 | Good | Good | n/r | Good |
| Djais et al, 200533 | Fair | Poor | n/r | Fair |
| Gilbert et al, 200434 | Good | Good | n/r | Good |
| Gilbert et al, 200435 | Fair | Good | n/r | Fair |
| Hellum et al, 201136 | Good | Excellent | n/r | Excellent |
| Hurley et al, 200137 | Fair | Fair | n/r | Fair |
| Kendrick et al, 200138 | Fair | Fair | n/r | Fair |
| Miller et al, 200239 | Good | Good | n/r | Fair |
| Rivero-Arrias et al, 200640 | Excellent | Fair | n/r | Poor |
| Wilkens et al, 201041 | Good | Good | n/r | Good |
| Cross-sectional | ||||
| Burstrom et al, 200142 | Poor | Good | n/r | Poor |
| Eker et al, 200743 | Good | Good | n/r | Poor |
| Klemenc-Ketis, 201144 | Poor | Fair | n/r | Poor |
| Muraki et al, 201145 | Poor | Fair | n/r | Poor |
| Muraki et al, 201246 | Poor | Fair | n/r | Poor |
| Sogaard et al, 200947 | Poor | Good | n/r | Poor |
| Observational longitudinal | ||||
| Aghayev et al, 201048 | Fair | Poor | n/r | Poor |
| Cheshire et al, 201149 | Fair | Poor | n/r | Poor |
| Garratt et al, 200150 | Fair | Good | n/r | Good |
| Genevay et al, 201251 | Good | Good | Good | Good |
| Gutke et al, 201152 | Good | Good | n/r | Good |
| Klemenc-Ketis, 201153 | Poor | Fair | Fair | Poor |
| Kovacs et al, 200554 | Good | Good | n/r | Good |
| Kovacs et al, 200455 | Good | Good | n/r | Good |
| Parker et al56 | Good | Good | n/r | Good |
| Schluesmann57 | Fair | Fair | n/r | Fair |
| Suarez-Almazor et al, 200058 | Fair | Fair | n/r | Fair |
| Cohort studies | ||||
| Gutke et al, 200659 | Poor | Good | n/r | Poor |
| Jannsonn et al, 200960 | Fair | Good | n/r | Fair |
| Van der Roer et al, 200661 | Fair | Fair | n/r | Good |
n/r , not relevant.
HRQoL Measures Used
The most frequently used descriptive systems are shown in Table 4. As it can be seen, EQ-5D has been used in all the included studies, whereas SF-6D and HUI III have been found only in two.47,58 Other common measures used were Oswestry Disability Questionnaire (ODI), Roland Morris Disability Questionnaire (RMDQ), Aberdeen Back Pain Scale (ABPS), and Lumbar Spine Outcome Assessment Instrument (LSOA).
TABLE 4.
Main Outcome Measures Reported by the Included
| Author, Year | Descriptive System | Rating Scale | Other Instruments Used (Generic non Preference Based, Clinical, Condition specific) | ||||||
| EQ-5D | SF-6D | HUI III | VAS | SF12 or SF-36 | ODI | RDQ | NASS | ABPS | |
| Aghayev et al, 201049 | √ | √ | |||||||
| Bastiaenen et al, 200824 | √ | √ | √ | √ | |||||
| Berg et al, 200925 | √ | √ | √ | √ | |||||
| Berg et al, 200926 | √ | √ | √ | √ | |||||
| Burstrom et al, 200141 | √ | ||||||||
| Carr et al, 200527 | √ | √ | √ | ||||||
| Casserley-Feeney et al, 201228 | √ | √ | √ | ||||||
| Cheshire et al, 201150 | √ | ||||||||
| Chown et al, 200829 | √ | ||||||||
| Cox et al, 201030 | √ | √ | √ | ||||||
| Del Pozo-Cruz et al, 201131 | √ | √ | √ | ||||||
| Djais et al, 200532 | √ | √ | √ | ||||||
| Eker et al, 200751 | √ | √ | |||||||
| Garratt et al, 200152 | √ | √ | √ | ||||||
| Genevay et al, 201253 | √ | √ | |||||||
| Gilbert et al, 200433 | √ | √ | √ | ||||||
| Gilbert et al, 200434 | √ | √ | √ | ||||||
| Gutke et al, 201154 | √ | √ | √ | ||||||
| Gutke et al, 200655 | √ | √ | √ | ||||||
| Hellum et al, 201135 | √ | √ | √ | ||||||
| Hurley et al, 200136 | √ | √ | √ | ||||||
| Jansson et al, 200956 | √ | ||||||||
| Kendrick et al, 200137 | √ | √ | √ | ||||||
| Klemenc-Ketis, 201142 | √ | √ | √ | ||||||
| Klemenc-Ketis, 201157 | √ | √ | |||||||
| Kovacs et al, 200558 | √ | √ | √ | ||||||
| Kovacs et al, 200459 | √ | √ | √ | ||||||
| Miller et al, 200238 | √ | √ | |||||||
| Muraki et al, 201143 | √ | √ | |||||||
| Muraki et al, 201044 | √ | √ | |||||||
| Parker et al, 201245 | √ | √ | √ | ||||||
| Rivero-Arrias et al, 200639 | √ | √ | √ | √ | |||||
| Schluessman et al, 200946 | √ | √ | √ | ||||||
| Sogaard et al, 200947 | √ | √ | √ | ||||||
| Suarez-Almazor et al, 200048 | √ | √ | √ | √ | |||||
| Van der Roer et al, 200660 | √ | ||||||||
| Wilkens et al, 201040 | √ | √ | |||||||
ABPS , Aberdeen Back Pain Scale; EQ-5D, EuroQol 5 Dimensions; HUI 3, Health Utility Index Mark 3; NASS, Lumbar Spine Outcome Assessment Instrument; ODI, Oswestry Disability Index; RDQ, Roland Morris Disability Questionnaire; SF-12, Short Form 12 Dimensions; SF-36, Short Form 36 Dimensions; SF-6D, Short Form 6 Dimensions; VAS, Visual Analogue Scale.
Validity
Convergent Validity Method
Correlations between the outcome measures were reported in 12 studies.26,42–44,47,50–55,58
Hypothesis 1
Correlation between EQ-5D and disease-specific instruments was assessed in 10 studies.26,43,44,50–53,55,58
Five of them analyzed EQ-5D and ODI correlations44,52,53,55,58 and results were generally moderate to strong (in absolute terms). Correlation coefficients were between 0.510 and 0.739 in three studies,44,52,53 0.48 in one,58 and between 0.232 and 0.206 in one.55 In one study data were too sparse to assess correlations.43 Rather strangely, the direction of the correlation changed across studies.
Three of them assessed convergent validity between EQ-5D and RMDQ.50,54,55 Correlations were moderate to strong (ρ between −0.422 to −0.815) in all of them.
EQ-5D was also found to moderately correlate with ABPS (r = −0.44) in one study50 and with Specific Sexual Function Questions (r = −0.51)26 and Core Outcome Measure Index (COMI) (r = −0.54)51 in two others.
One study58 presented results for both EQ-5D and HUI III correlations with ODI and found moderate correlations at 3 and 6 months for both instruments. Correlations between HUI III and ODI were stronger than those between EQ-5D and ODI at 3 months but weaker at 6 months.
Overall, given that only one study55 did not reflect our prior expectations of moderate-to-very strong correlations, findings support the first hypothesis of convergent validity for the EQ-5D, and the small evidence found sustains the first hypothesis for the HUI III.
Hypothesis 2
EQ-5D correlation with other HRQOL instruments was assessed in five studies.42,43,47,54,55
EQ-5D and visual analogue scale (VAS) agreement was examined by three studies.42,54,55 Burstrom et al42 reported strong correlations between the two instruments (r = 0.67). Similarly, in the two papers of Kovacs et al54,55 correlations between EQ-5D and VAS were strong at both 15 and 60 days follow-up. More precisely, the correlation coefficients were 0.70 at 15 days investigation point and 0.76 at 60 days investigation time points54 and 0.67 at 15 days investigation time point in all of the cases.55 Differently from what we expected, correlations were only moderate at baseline (r = 0.5253 and r = 0.42).54
In one study47 EQ-5D and SF-6D correlation was moderate (r = 0.553). Similarly, one study found moderate correlations between EQ-5D and SF36 (r = 0.49).43
Although some papers present data that sustain our prior expectations of positive and strong-to-very strong correlations for the second hypothesis, results are not conclusive given that moderate correlations were also frequently reported.
Hypothesis 3
Only one study presented results for correlation between a generic and a disease construct-specific instrument. In detail, Genevay et al51 found that EQ-5D was weakly associated with COMI symptom specific (r = −0.36).
This study supports the third hypothesis of convergent validity of weak correlations between generic preference-based instruments and disease construct-specific instruments.
Known Group Method
Ten studies allowed an assessment of known groups for EQ-5D.42,43,45,46,53,56,58–61
Hypothesis 1
Five studies (six reports) permitted an assessment of EQ-5D validity after the first hypothesis.45,46,49,56,58,61
Two reports referred to the same study45,46 showed that EQ-5D was able to detect variations in groups with different severity grades of lumbar spondylitis. Differences were statistically significant. One study49 showed that EQ-5D is able to distinguish between women with non-lumbar-pelvic pain, women with lumbar pain, women with pregnancy-related pelvic girdle pain, and women with combined pain. Differences between groups were statistically significant between women without lumbar-pelvic pain and all the other groups, and between women with lumbar pain and women with combined pain. Differences between lumbar pain and pregnancy-related pelvic girdle pain were not statistically significant. One study58 reported EQ-5D to differentiate between the group of patients for which the treatment was successful and the group of patients who did not respond to it (P = 0.003). Parker et al56 presented similar results between patients categorized according to three severity grades: stable; worst and best clinical situation (P ≤ 0.005). EQ-5D presented the highest values for the best clinical situation and the lowest values for the worst situation. Van der Roer et al61 reported similar results for the same severity groups, although it did not provide results for statistical significance.
Overall, EQ-5D responds well when tested on different severity known groups distinguishing between different grades of disability and therefore sustaining the first hypothesis for known group methods.
Hypothesis 2
Only one study permitted an assessment of the second hypothesis for known groups.45,46
The two reports of Muraki et al45,46 registered a higher mean score (P < 0.05) for those patients who declared not to have LBP if compared with those with the symptom.
This sustains the second hypothesis of known group methods, which is the ability of generic preference measure to distinguish between patients and general population.
Hypothesis 3
The third hypothesis of known group method has been tested in four studies.42–44,60
All of them reported women to have significantly lower EQ-5D utility scores than men42–44,60 maintaining constant the clinical condition, and this was always statistically significant.
Results support the third hypothesis of known groups assessment (distinguishing between male and female).
Hypothesis 4
Only one study61 permitted to evaluate the fourth hypothesis of known group.
This study showed EQ-5D to perform well in differentiating patients with acute or recurrent LBP, presenting higher pain and dysfunction for the acute group.
This confirms the fourth hypothesis of the study, namely the ability of distinguishing between acute and recurrent LBP.
Responsiveness
Twenty-four studies allowed for an assessment of responsiveness.25,27–30,32–41,49,50,53,54,56–58,60,61
Twenty-one of them reported TSS,25,27–30,33–41,48,49,54,56,57,60,61 three of them ES,32,53,58 and one of them SRM.50
Test of Statistical Significance Method
Hypothesis 1
Eighteen studies (19 reports) permitted an assessment of the first hypothesis of responsiveness.25,27–30,33–37,40,41,48,49,54,56,57,60,61
Hellum et al36 managed to detect statistically significant improvements in patients treated with surgery with disc prosthesis and patients treated with rehabilitation therapy. Schluessmann et al57 presented significant changes in patients receiving total disc arthroplasty, with an EQ-5D mean score of 0.32 at baseline, and improvements to 0.72 at 3 months and 0.73 at 1 year. Parker et al56 registered significant improvement of EQ-5D after patients had undertaken lumbar fusion, which were statistically significant. Also Berg et al,27 Chown et al,30 Aghayev et al,48 and Cheshire et al49 reported similar results, which were statistically significant.
In studies conducted by Bastiaenen et al,25 Carr et al,28 Casserley-Feeney et al,29 Djas and Kalim,33 Gilbert et al,34,35 Hurley et al37 Jansson et al,60 and Wilkens et al41 EQ-5D values appeared responsive to improvements because of the treatment of LBP, although these were not statistically significant.
According to Kovacs et al,54 Rivero-Arrias et al,40 and Van der Roer et al,61 the EQ-5D is responsive to variations in the health status because of treatment.
Overall, the first hypothesis for TSS holds given that preference-based measures are able to detect changes because of treatment.
Hypothesis 2
Twelve studies permitted to test for the second hypothesis of responsiveness.25,27–31,33–35,41,48,60
In Chown et al30 all patients assigned to the exercise, physiotherapy, or osteopathy groups improved, but patients in the osteopathy group reported significantly higher EQ-5D values if compared with patients in the group exercise (P < 0.01). Similarly, Berg et al27 registered a different increase in mean EQ-5D values from baseline to 1 year for patients assigned to the total disc replacement group compared with patients assigned to the fusion group, with the total disc replacement being more effective (P < 0.05). Aghayev et al48 found that EQ-5D was able to distinguish between patients receiving Dynardi total disc arthroplasty and patients receiving total disc replacement, with the differences between the two groups being statistically significant at P < 0.001. Gilbert et al34,35 found that EQ-5D differentiated between magnetic resonance imaging and delayed magnetic resonance imaging at 8 and 24 months, and that differences were statistically significant in this latter follow-up.
Other seven studies presented data that supported the second hypothesis, although results were not statistically significant.25,28,29,31,33,36,41 Carr et al,28 for instance, registered an increase in EQ-5D mean values from baseline to 3 months of 0.028 and from baseline to 12 months of 0.045 for the individual physiotherapy group, whereas improvements for the group exercise were milder. Similarly, Casserley-Feeney et al29 reported EQ-5D to differ between public physiotherapy and private physiotherapy patients, Djas and Kalim33 for the instrument to be sensitive to differences between patients undergoing radiography and patients not undergoing radiography and Wilkens et al41 for the measurement to recognize patients administered with glucosamine and patients administered with placebo. Bastiaenen et al,25 Hellum et al,36 and Cox et al31 reported similar results.
One study60 managed to differentiate between patients treated with macrodecompression, microscopic decompression, decompression and fusion, and fusion alone.
These results confirm the ability of the EQ-5D to distinguish between different interventions outcomes.
Hypothesis 3
Fifteen studies (16 reports) permitted an assessment of the third hypothesis of responsiveness.25,27–30,33–39,41,54,56,61
Twelve of them reported an EQ-5D behavior that was coherent with the scores registered by other measures.27–30,33–37,41,54,56 For example, Berg et al27 registered an increase in EQ-5D values for the total disc replacement group at 1 year, and a reduction of the mean value at 2 years, and similar trends were reported for ODI and VAS. Also Parker et al56 results of EQ-5D and ODI were coherent. Similarly, Carr et al,28 Chown et al,30 Djas and Kalim,33 Hurley et al,37 and Kovacs et al54 presented improvements that were well detected by both EQ-5D and RMDQ, Van der Roer et al61 by EQ-5D and Quebeck Pain Disability Scale and Gilbert,34,35 and Hellum et al36 by EQ-5D and ABPS.
Although also for Casserley-Feeney et al29 EQ-5D and RMDQ presented similar results, this latter study evidenced that RMDQ is more sensitive than EQ-5D to small differences at low levels of disability. This lack of sensitivity to change in health states seems confirmed also by other studies. For example, in Miller et al39 RMDQ is able to detect a small change in patients’ status at 3 months that passed undetected by EQ-5D and in Bastiaenen et al25 a similar problem occurs with EQ-5D and RMDQ at 6 months. In Kendrick et al,38 median EQ-5D scores remained stable from baseline to 9 months, whereas RMDQ scores detected a small improvement in patients. Also, Wilkens et al41 found an extremely small improvement registered by RMDQ at 1 year follow-up not registered by the EQ-5D.
Overall, the evidence collected supports the third hypothesis of responsiveness which is the ability of reporting changes coherent to those reported by other generic or diseases-specific measures.
Effect Size and Standardize Response Mean
Hypothesis 1
Three studies permitted to test ES32,53,58 and one study SRM.50
EQ-5D ES were moderate and statistically significant in two studies.32,53 The third study58 reported ES for both EQ-5D and HUI III, and found HUI III to be more discriminative than EQ-5D at 3 months, with effect sizes similar to ODI ones. At 6 months, both EQ-5D and HUI III were highly discriminative.
One study presented EQ-5D SRM and found a moderate responsiveness of the instrument.50
ES and SRM were moderate to strong, therefore supporting the hypothesis of responsiveness.
EQ-5D validity and responsiveness results are summarized in Table 5.
TABLE 5.
EQ-5D Summary of Results
| Author, Year | Convergent Validity | Validity—Known Groups | Responsiveness TSS | Responsiveness ES/SRM | |||||||
| H1 | H2 | H3 | H1 | H2 | H3 | H4 | H1 | H2 | H3 | H1 | |
| Aghayev et al, 201049 | √ | √ | √ | ||||||||
| Bastiaenen et al, 200824 | ± | ± | X | ||||||||
| Berg et al, 200925 | √ | ||||||||||
| Berg et al, 200926 | √ | √ | √ | ||||||||
| Burstrom et al, 200141 | √ | √ | |||||||||
| Carr et al, 200527 | ± | ± | √ | ||||||||
| Casserley-Feeney et al, 201228 | ± | ± | √ | ||||||||
| Cheshire et al, 201150 | √ | ||||||||||
| Chown et al, 200829 | √ | √ | √ | ||||||||
| Cox et al, 201030 | ± | ||||||||||
| Del Pozo-Cruz et al, 201131 | √ | ||||||||||
| Djais et al, 200532 | ± | ± | √ | ||||||||
| Eker et al, 200751 | ? | X | √ | ||||||||
| Garratt et al, 200152 | √ | √ | |||||||||
| Genevay et al, 201253 | √ | √ | |||||||||
| Gilbert et al, 200433 | ± | √ | √ | ||||||||
| Gilbert et al, 200434 | ± | √ | √ | ||||||||
| Gutke et al, 201154 | √ | ||||||||||
| Gutke et al, 200655 | √ | ||||||||||
| Hellum et al, 201135 | √ | ± | √ | ||||||||
| Hurley et al, 200136 | ± | √ | |||||||||
| Jansson et al, 200956 | √ | ± | – | ||||||||
| Kendrick et al, 200137 | X | ||||||||||
| Klemenc-Ketis, 201142 | √ | √ | |||||||||
| Klemenc-Ketis, 201157 | √ | √ | |||||||||
| Kovacs et al, 200558 | √ | √ X | – | √ | |||||||
| Kovacs et al, 200459 | √ | √ X | |||||||||
| Miller et al, 200238 | X | ||||||||||
| Muraki et al, 201143 | √ | √ | |||||||||
| Muraki et al, 201044 | √ | √ | |||||||||
| Parker et al, 201245 | √ | √ | √ | ||||||||
| Rivero-Arrias et al, 200639 | – | ||||||||||
| Schluessman et al, 200946 | √ | ||||||||||
| Sogaard et al, 200947 | X | ||||||||||
| Suarez-Almazor et al, 200048 | √ | √ | √ | ||||||||
| Van der Roer et al, 200660 | √ | √ | – | ||||||||
| Wilkens et al, 201040 | ± | ± | √ X | ||||||||
Keys: √ Meeting prior expectations; ± trend meeting prior expectation but not statistically significant; - trend meeting prior expectation but no test of statistical significance performed; X trend nonmeeting prior expectations; ? mixed/not possible to assess.
When two keys for the same item are used, it is because more than one result was found.
ES indicates effect size; H1, hypothesis 1; H2, hypothesis 2; H3, hypothesis 3; H4, hypothesis 4; TSS, test of statistical significance.
DISCUSSION
The 35 studies (37 reports) included in this systematic review show that LBP decreases HRQoL and that EQ-5D is generally able to detect improvements and deteriorations in health states because of health interventions or disease progression.
Comparing our results with those of similar researches it emerges that EQ-5D performs well in LBP populations. In a review of Tosh et al3 EQ-5D correlation with visual acuity, a disease-specific instrument for visual disorders, was often poor or nonsignificant for patients with age-related macular degeneration and cataracts. Similarly, a review of Papaioannou et al62 found generally modest and mostly weak correlations between EQ-5D and disease-specific instruments such as brief psychiatry rating scale and quality-of-life scale, two-schizophrenia HRQoL measures. In light of this, the commonly moderate-to-strong correlations between EQ-5D and disease-specific instruments found in our study show a good performance of the instrument.
Differently from what it was hypothesized, EQ-5D correlation with other generic instruments was strong at follow-ups, but only moderate at baseline. Weaker correlations for baseline data might be because of EQ-5D being more sensitive to the lower end of the utility scale,63 EQ-5D having more distributed frequencies among spine patients compared with other generic instruments64 (the effect of which is lower mean values for patients in worst health states), or EQ-5D measuring constructs that are relevant for greater disability levels than other generic instruments. Nevertheless, moderate correlations between general preference-based instruments have already been seen in other studies (e.g., Dyer et al),4 thus this behavior cannot be considered proper evidence against the instrument validity.
EQ-5D known group assessment showed statistically significant differences between different disease severities, patients with/without LBP and respondents/nonrespondents to treatments. There was also strong and statistically significant evidence that EQ-5D can distinguish between women and men perception of health, with the HRQoL values for the former being lower than the latter. These results sustain our prior hypothesis and are in line with those of other systematic reviews on EQ-5D validity in other population (e.g., Peasgood et al65).
EQ-5D appears to be a responsive instrument, although it seems to be less responsive than disease-specific ones. This is not surprising. Disease-specific and general preference-based instruments are not perfect substitutes. Disease-specific instruments only contain items or health dimensions that are relevant for the specific condition examined, whereas generic instruments assess all domains of HRQoL. By contrast, general preference-based instruments are meant to be perfect substitutes, at least in theory. The current systematic review presents paucity of data as regards between generic instruments comparison. One study found HUI III to be more responsive than EQ-5D at 3 months and equally responsive at 6 months. Another study presented only moderate correlation between EQ-5D and SF-6D. These results seem to suggest that the three preference-based instruments are not equivalent measures of HRQoL and that they assess different domains. However, results cannot be considered conclusive and a study estimating direct correlations between generic instruments might be useful.
This systematic review has some limitations. First, some of the included studies present small sample sizes. This might be one of the reasons for the lack of statistical significance registered in some reports. Second, there is not enough reference to missing data caused by nonrespondents and how these have been accounted for. Finally, some of the included studies did not control for age, sex, social status, and other variables that can influence LBP evaluation.
Nevertheless, our systematic review represents an important effort. It suggests that EQ-5D performs well in LBP population and that its scores are suitable for economic evaluation of LBP interventions, whereas it recommends the use of EQ-5D in combination with disease-specific instruments for clinical evaluation, given its lack of sensitivity to change in health state compared with them. Results for SF-6D and HUI III are too scarce to draw any conclusion.
Key Points.
EQ-5D showed good validity and responsiveness in patients with low back pain.
EQ-5D can be used for economic evaluation of interventions targeting low back pain.
EQ-5D appears unable to detect changes in health status at lower levels of severity.
Assessment for SF-6D and HUI III was not possible because of lack of evidence.
Supplementary Material
Acknowledgments
The authors would like to thank and extend their heartfelt gratitude to the following persons who have made the completion of this work possible: Matthew Glover, Louise Longworth, Joanne Lord, Patrizio Armeni and Francesco Costa. Special thanks go to Yaling Yang, who acted as an advisor to the study and provided helpful comments on the review and manuscript.
Footnotes
The manuscript submitted does not contain information about medical device(s)/drug(s).
No funds were received in support of this work.
Relevant financial activities outside the submitted work: board membership, grants, employment, travel/accommodations/meeting expenses.
References
- 1.Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord 2000; 13:205–217. [DOI] [PubMed] [Google Scholar]
- 2.Brazier J, Ratcliffe J, Salomon JA, et al. Measuring and Valuing Health Benefits for Economic Evaluation. Oxford: Oxford University Press; 2007. [Google Scholar]
- 3.Tosh J, Brazier J, Evans P, et al. Review of generic preference-based measures of health-related quality of life in visual disorders. Value Health 2012; 5:118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dyer MTD, Goldsmith KA, Sharples LS, et al. Review of health utilities using the EQ-5D in studies of cardiovascular disease. Health Qual Life Outcomes 2010; 28:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pickard AS, Wilke CT, Lin HW, et al. Health utilities using the EQ-5D in studies of cancer. Pharmacoeconomics 2007; 25:365–384. [DOI] [PubMed] [Google Scholar]
- 6.Marra CA, Woolcott JC, Kopec JA, et al. A comparison of generic, indirect utility measures (the HUI2, HUI3, SF-6D and EQ-5D) and disease specific instruments (the RAQoL and the HAQ) in rheumatoid arthritis. Soc Sci Med 2005; 60:1571–1582. [DOI] [PubMed] [Google Scholar]
- 7.Salaffi F, DeAngelis R, Stancati A, et al. Health-related quality of life in multiple musculoskeletal conditions: a cross-sectional population based epidemiological study II. The Mapping Study. Clin Exp Rheumatol 2005; 23:829–839. [PubMed] [Google Scholar]
- 8.Fisk JD, Brown MG, Sketris IS, et al. A comparison of health utility measures for the evaluation of multiple sclerosis treatments. J Neurol Neurosurg Psychiatry 2005; 76:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chapman JR, Norevll DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine 2011; 36:S54–S58. [DOI] [PubMed] [Google Scholar]
- 10.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ 2002; 21:271–292. [DOI] [PubMed] [Google Scholar]
- 11.Brooks R. EuroQol: the current state of play. Health Policy 1996; 37:53–72. [DOI] [PubMed] [Google Scholar]
- 12.Dolan P. Modelling valuations for EuroQol health states. Med Care 1997. 1095–1108. [DOI] [PubMed] [Google Scholar]
- 13.Fenny D, Furlong W, Torrance GW, et al. Multi-attribute and single-attribute utility functions for the Health Utility Index Mark 3 System. Med Care 2002; 40:113–128. [DOI] [PubMed] [Google Scholar]
- 14.Hayden J, van Tulder MW, Malmivaara A, et al. Exercise therapy for treatment of non-specific low back pain (review). Chocrane Database Syst Rev 2011. 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin CC, Haas M, Maher C, et al. Cost-effectiveness of guideline-endorsed treatments for low back pain: a systematic review. Eur Spine J 2011; 20:1024–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Terwee CB, Mokkink LB, Knol DL, et al. Rating the methodological quality in systematic reviews of studies on measurement properties: a scoring system for the COSMIN checklist. Qual Life Res 2012; 21:651–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walters SJ. Quality of Life Outcomes in Clinical Trials and Healthcare Evaluation: A Practical Guide to Analysis and interpretation. Chichester: Wiley; 2009. [Google Scholar]
- 18.Terwee CB, Dekker FW, Wiersinga WM, et al. On assessing responsiveness of health related quality of life instruments: guidelines for instrument evaluation. Qual Life Res 2003; 12:349–362. [DOI] [PubMed] [Google Scholar]
- 19.Hurst NP, Kind P, Ruta, et al. Measuring health related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol 1997; 36:551–559. [DOI] [PubMed] [Google Scholar]
- 20.McHorney CA, Ware JE, Raczek AE. The MOS-36 Item-Short Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993; 31:247–263. [DOI] [PubMed] [Google Scholar]
- 21.Kantz ME, Harrys WJ, Levitzky K, et al. Methods for assessing condition-specific and generic functional status outcomes after total knee replacement. Med Care 1992; 30: MS240–52. [DOI] [PubMed] [Google Scholar]
- 22.Olivares PR, Gusi N, Prieto J, et al. Fitness and health related quality of life dimensions in community dwelling middle aged and older adults. Health Qual Life Outcomes 2011; 9:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Evans JD. Straightforward Statistics for the Behavioral Science. Pacific Grove: Brooks/Cole Publishing; 1996. [Google Scholar]
- 24.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed.Hillsdale: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 25.Bastiaenen CH, De Bie RA, Vlaeyen JW, et al. Long-term effectiveness and costs of a brief self-management intervention in women with pregnancy-related low back pain after delivery. BMC Pregnancy Childbirth 2008; 8:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berg S, Fritzell P, Tropp H. Sex life and sexual function in men and women before and after total disc replacement compared with posterior lumbar fusion. Spine J 2009; 9:987–994. [DOI] [PubMed] [Google Scholar]
- 27.Berg S, Tullberg T, Branth B, et al. Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J 2009; 18:1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Carr JL, Klaber Moffett JA, Howarth E, et al. A randomized trial comparing a group exercise programme for back pain patients with individual physiotherapy in a severely deprived area. Disabil Rehabil 2005; 27:929–937. [DOI] [PubMed] [Google Scholar]
- 29.Casserley-Feeney SN, Daly L, Hurley DA. The access randomized clinical trial of public versus private physiotherapy for low back pain. Spine 2012; 37:85–96. [DOI] [PubMed] [Google Scholar]
- 30.Chown M, Whittamore L, Rush M, et al. A prospective study of patients with chronic back pain randomised to group exercise, physiotherapy or osteopathy. Physiotherapy 2008; 94:21–28. [Google Scholar]
- 31.Cox H, Tilbrook H, Aplin J, et al. A randomised controlled trial of yoga for the treatment of chronic low back pain: results of a pilot study. Complement Ther Clinic Pract 2010; 16:187–193. [DOI] [PubMed] [Google Scholar]
- 32.Del Pozo-Cruz B, Hernandez Mocholi MA, Adsuar JC, et al. Effects of the whole body vibration therapy on main outcome measures for chronic non-specific low back pain: a single-blind randomize controlled trial. J Rehab Med 2011; 43:689–694. [DOI] [PubMed] [Google Scholar]
- 33.Djais N, Kalim H. The role of lumbar spine radiography in the outcomes of patients with simple acute low back pain. APLAR J Rheum 2005; 8:45–50. [Google Scholar]
- 34.Gilbert FJ, Grant AM, Gillan MG, et al. Does early imaging influence management and improve outcome in patients with low back pain? A pragmatic randomised controlled trial. Health Technol Assess 2004; 8:1–131. [DOI] [PubMed] [Google Scholar]
- 35.Gilbert FJ, Grant AM, Gillan MG, et al. Low back pain: influence of early MR imaging or CT on treatment and outcome—multicentre randomized trial. Radiology 2004; 231:343–351. [DOI] [PubMed] [Google Scholar]
- 36.Hellum C, Johnsen LG, Storheim K, et al. Surgery with disc prosthesis versus rehabilitation in patients with low back pain and degenerative disc: two year follow-up of randomised study. BMJ 2011; 342:2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hurley DA, Minder PM, McDonough SM, et al. Interferential therapy electrode placement technique in acute low back pain: a preliminary investigation. Arch Phys Med Rehabil 2001; 82:485–493. [DOI] [PubMed] [Google Scholar]
- 38.Kendrick D, Fielding K, Bentley E, et al. Radiography of the lumbar spine in primary care patients with low back pain: randomised controlled trial. Br Med J 2001; 322:400–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Miller P, Kendrick D, Bentley E, et al. Cost-effectiveness of lumbar spine radiography in primary care patients with low back pain. Spine 2002; 27:2291–2297. [DOI] [PubMed] [Google Scholar]
- 40.Rivero-Arias O, Gray A, Frost H, et al. Cost-utility analysis of physiotherapy treatment compared with physiotherapy advice in low back pain. Spine 2006; 31:1381–1387. [DOI] [PubMed] [Google Scholar]
- 41.Wilkens P, Scheel IB, Grundnes O, et al. Effect of glucosamine on pain-related disability in patients with chronic low back pain and degenerative lumbar osteoarthritis: a randomized controlled trial. JAMA 2010; 304:45–52. [DOI] [PubMed] [Google Scholar]
- 42.Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001; 10:621–635. [DOI] [PubMed] [Google Scholar]
- 43.Eker L, Tüzün EH, Daşkapan A, et al. The relationship between EQ-5D and SF-36 instruments in patients with low back pain. Fizyoterapi Rehabilitasyon 2007; 18:3–10. [Google Scholar]
- 44.Klemenc-Ketis Z. Predictors of health-related quality of life and disability in patients with chronic non-specific low back pain. Zdr Vestin 2011; 80:379–385. [Google Scholar]
- 45.Muraki S, Akune T, Oka H, et al. Health-related quality of life in subjects with low back pain and knee pain in a population-based cohort study of Japanese men: the research on osteoarthritis against disability study. Spine 2011; 36:1312–1319. [DOI] [PubMed] [Google Scholar]
- 46.Muraki S, Akune T, Oka H, et al. Impact of knee and low back pain on health-related quality of life in Japanese women: the research on osteoarthritis against disability (ROAD). Mod Rheumatol 2010; 20:444–451. [DOI] [PubMed] [Google Scholar]
- 47.Sogaard R, Christensen FB, Videbaek TS, et al. Interchangeability of the EQ-5D and the SF-6D in long-lasting low back pain. Value Health 2009; 12:606–612. [DOI] [PubMed] [Google Scholar]
- 48.Aghayev E, Roder C, Zweig T, et al. Benchmarking in the SWISS spine registry: results of 52 dynardi lumbar total disc replacements compared with the data pool of 431 other lumbar disc prostheses. Eur Spine J 2010; 19:2190–2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cheshire A, Polley M, Peters D, et al. Is it feasible and effective to provide osteopathy and acupuncture for patients with musculoskeletal problems in a GP setting? A service evaluation. BMC Fam Pract 2011; 12:49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Garratt AM, Klaber Moffett J, Farrin AJ. Responsiveness of generic and specific measures of health outcome in low back pain. Spine 2001; 26:71–77. [DOI] [PubMed] [Google Scholar]
- 51.Genevay S, Cedraschi C, Marty M, et al. Reliability and validity of the cross-culturally adapted French version of the core outcome measures index (COMI) in patients with low back pain. Eur Spine J 2012; 21:130–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gutke A, Lundberg M, Ostgaard HC, et al. Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms. Eur Spine J 2011; 20:440–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Klemenc-Ketis Z. Disability in patients with chronic non-specific low back pain: validation of the Slovene version of the Oswestry disability index. Zdravstveno Varstvo 2011; 50:87–94. [Google Scholar]
- 54.Kovacs FM, Abraira V, Zamora J, et al. The transition from acute to subacute and chronic low back pain: a study based on determinants of quality of life and prediction of chronic disability. Spine 2005; 30:1786–1792. [DOI] [PubMed] [Google Scholar]
- 55.Kovacs FM, Abraira V, Zamora J, et al. Correlation between pain, disability, and quality of life in patients with common low back pain. Spine 2004; 29:206–210. [DOI] [PubMed] [Google Scholar]
- 56.Parker SL, Mendenhall SK, Shau DN, et al. Minimum clinically important difference in pain, disability, and quality of life after neural decompression and fusion for same-level recurrent lumbar stenosis: understanding clinical versus statistical significance—clinical article. J Neurosurg Spine 2012; 16:471–478. [DOI] [PubMed] [Google Scholar]
- 57.Schluessmann E, Diel P, Aghayev E, et al. SWISSspine: a nationwide registry for health technology assessment of lumbar disc prostheses. Eur Spine J 2009; 18:851–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Suarez-Almazor ME, Kendall C, Johnson JA, et al. Use of health status measures in patients with low back pain in clinical settings. Comparison of specific, generic and preference-based instruments. Rheumatology (Oxford) 2000; 39:783–790. [DOI] [PubMed] [Google Scholar]
- 59.Gutke A, Ostgaard HC, Oberg B. Pelvic girdle pain and lumbar pain in pregnancy: a cohort study of the consequences in terms of health and functioning. Spine 2006; 31:E149–E155. [DOI] [PubMed] [Google Scholar]
- 60.Jansson K, Nemeth G, Granath F, et al. Health-related quality of life (EQ-5D) before and one year after surgery for lumbar spinal stenosis. J Bone Joint Surg Br 2009; 91B:210–216. [DOI] [PubMed] [Google Scholar]
- 61.Van der Roer N, Ostelo RW, Bekkering GE, et al. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine 2006; 31:578–582. [DOI] [PubMed] [Google Scholar]
- 62.Papaioannou D, Brazier J, Parry G. How valid and responsive are generic health status measures, such as EQ5D and SF-36, in Schizophrenia? A systematic review. Value Health 2011; 14:907–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Longworth L, Bryan S. An empirical comparison of EQ-5D and SF-6D in liver transplant patients. Health Econ 2003; 12:1061–1067. [DOI] [PubMed] [Google Scholar]
- 64.McDonough CM, Grove MR. Comparison of EQ5D, HUI III and SF36 derived societal health states values among spine patient outcomes research trial participants. Qual Life Res 2005; 14:1321–1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Peasgood T, Brazier J, Papaioannou D. A systematic review on the validity and responsiveness of EQ5D and SF6D for depression and anxiety. HEDS Discussion Paper 12/15 [serial online.]. Available from: http://eprints.whiterose.ac.uk/74659/1/12.15.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


