Abstract
Objective
The purpose of this study was to explore the relationship between patients’ self-reported and performance-based function after total hip arthroplasty (THA).
Design
Twenty-three patients (age 61.4 ± 8.3 years) undergoing primary THA for hip osteoarthritis participated. Self-reported function and recovery was measured using The Hip Dysfunction and Osteoarthritis Outcome Score (HOOS) ADL and Pain subscales. Performance-based functional measures included Timed Up and Go Test (TUG), Stair Climbing Test (SCT), and the 6 Minute Walk Test (6MW). Outcome measures were assessed pre- and post-operatively at one and six months.
Results
One month after THA, performance-based function declined compared to baseline as follows: TUG: −22.1 ± 25.4%; SCT: −58.5 ± 63.6%; and 6MWT: −22.6 ± 31.7%. In contrast, self-reported function on the HOOS ADL significantly improved one month after THA compared to baseline: 40.8 ± 33.3%. One to six months after THA, there were significant improvements in TUG, SCT and 6MWT which paralleled improvements on the HOOS subscales, although changes were not significantly correlated.
Conclusion
The disparity between changes in HOOS scores and functional performance post-operatively suggests that patients may overestimate their functional capacity early after THA, likely in response to pain improvements over the same time period. Therefore, outcomes assessment after THA should include both self-report and performance-based functional measures.
Keywords: Hip Arthroplasty, HOOS, Functional performance, Osteoarthritis, Outcomes
Introduction
Degenerative hip disease secondary to osteoarthritis (OA) continues to exist as a significant disabling affliction that compromises the quality of life of 20 million individuals in the United States.1 More than 500,000 total hip arthroplasty (THA) procedures are projected to be performed yearly in America by 2030.2 Total hip arthroplasty is known to reliably reduce pain and improve self-reported function in older adults with hip OA. However, full recovery of pre-operative or pre-disease function and strength is rarely assessed using performance-based outcomes following THA. Functional and strength deficits are of particular concern in older patients with limited capability to rehabilitate following surgery.3 Coupled with strength and functional deficits imposed by surgical intervention, many patients have profound pre-operative weakness and atrophy that accompany degenerative joint disease. Such weakness results in decreased walking capacity, impaired postural control, and difficulty negotiate uneven terrain.4,5 As a result, deficits are observed in the post-operative period that may be best measured with performance-based outcome assessments.
Several outcome measurement tools have been utilized to assess patient-reported functional recovery following THA. Self-report questionnaires provide a global measure of patient perception of functional abilities and typically include a range of important functional skills. The values of self-report questionnaires include high levels of internal consistency, cost-effectiveness, and ease of administration.6,7 Such questionnaires include The Western Ontario and McMaster University Osteoarthritis Index (WOMAC),8 Harris Hip Score (HHS),9 Medical Outcomes Study Short Form-36 (SF-36),10 UCLA Activity Score,11 and more recently, the Hip and Osteoarthritis Outcome Score (HOOS).12 The HOOS is an extension of the WOMAC and may be useful in younger and/or more active patients with hip injury or OA, and has been validated for tracking outcomes after THA.13 With the addition of questions regarding sport and recreation, the utilization of HOOS may be ideal given the potential for increased use among a younger population undergoing THA in the future.14
Although self-report measures such as the HOOS hold value in measuring outcomes following THA, limitations do exist. Self-report measures are dependent upon patient perception. With the possibility of over- or under-estimating functional ability, perceptions may be tempered based upon presence or absence of pain. Previous data has demonstrated such overestimation of ability following pain reduction after total knee arthroplasty.15 Coupled with the debilitating sequelae of OA, collective assessment of recovery based on patient perception may not fully detail the recovery process.
Assessment of functional outcomes following THA has been well described.16 Performance-based measures such as the 6 Minute Walk (6MW) Test, Timed up and Go Test (TUG), and the Stair Climbing Test (SCT) quantify performance with tasks mimicking activities of daily living, as opposed to relying on individuals’ perception of performance.7,15,17 Hence, they may provide a more objective measure of functional capacity. However, the relationship between self-reported outcomes and performance-based outcomes after THA is unclear. Further, it is unknown which outcomes may best guide post-operative clinical decision making.
The purpose of this investigation was to more fully characterize patient outcomes after THA by (1) examining longitudinal changes in both self-report measures (HOOS ADL and Pain subscales) and performance measures (TUG, SCT, 6MW) over the first 6 months after THA, (2) evaluating correlations between changes in HOOS self-report function (ADL and Pain subscales) vs change in functional performance (TUG, SCT, 6MW) from before surgery to 1 month after THA and 1 month to 6 months after THA. It was hypothesized that neither changes in HOOS ADL nor Pain subscale scores would be correlated with changes in functional performance at all time points assessed. This investigation further sought to evaluate the relationship between changes in HOOS pain and ADL subscale scores. Based on findings from other arthroplasty populations,7,18,19,20 it was hypothesized that changes in HOOS pain and ADL subscale scores would be significantly correlated.
Methods
Study Design
This study is a prospective cohort investigation examining self-reported and performance-based outcomes for patients scheduled to undergo a primary, posterior approach THA secondary to osteoarthritis (OA). Patients were excluded from the study if they had bilateral disease, history of hip trauma, or septic joint disease. Additional exclusion criteria included uncontrolled hypertension, uncontrolled diabetes mellitus, body mass index (BMI) >40 kg/m2, additional orthopedic pathology or neurologic disorders that impaired daily function.
All patients were scheduled for a unilateral, primary THA at one of four local hospitals between June 2010 and August 2011. Patients were evaluated approximately 2 weeks prior to surgery and at 1 and 6 months after surgery using both self-report (HOOS) and performance-based (TUG, SCT, 6MW) measures. All performance-based measures were performed by individuals blinded to self-report questionnaire assessments. At each time point, self-report measures were completed following the testing session in which the performance-based measures were assessed. The study was approved by the Colorado Multiple Institutional Review Board. Informed consent was obtained from all participants, and the rights of participants were protected.
Outcomes
Self-Reported Outcomes
The HOOS assesses function over the previous week of activity and is composed of 5 separately scored subscales: Pain, Symptoms, Function in daily living (ADL), Function in sports and recreation (Sport/Rec), and Hip-related QoL.12 Responses to questions are given using a Likert scale (values from 0 to 4). A normalized score is calculated for each subscale (100 indicates no symptoms and 0 indicates extreme symptoms). The HOOS is reliable and valid when used for short and long term follow-up after THA.13
Performance-Based Outcomes
Measures of functional performance included stair climbing test (SCT), timed up and go test (TUG), and 6 minute walking (6MW) test. These functional outcomes encompass three activities that are represented in the content of HOOS subscale ADL questions (ascending/descending stairs, rising from a bed, walking on a flat surface). The SCT measures the time it takes to ascend and descent 12 stairs. This test places demand on both the quadriceps and gluteal muscles, and minimizes the possibility that an upper limit can be easily reached due to the fact it is a demanding physical task. The TUG measures the time it takes a patient to rise from an armchair, walk 3 meters, turn, and return to sitting in the same chair without physical assistance. This test has excellent inter-rater and intra-rater reliability.7 A widely used performance-based test, the 6MW, measures the distance walked in 6 minutes. Although this test was originally used extensively to measure endurance in patients with pulmonary disease, it has since been validated to measure functional mobility in a variety of patient populations, including those with lower extremity joint replacement. The 6MW is safe, easy to administer, well tolerated, and responsive to change after joint arthroplasty.21
Statistical Methods
Data were processed using IBM SPSS Statistics (Version 22, Armonk, NY, USA). A 1-way repeated-measures analysis of variance was performed for all outcome measures. Separate analyses were performed for performance and self-report outcomes. Post-hoc comparisons using linear contrasts were performed to examine changes from 1) pre-op to 1 month after THA and 2) 1 month to 6 months after THA. Pearson product moment correlations were calculated by using change scores from baseline ([initial-final/initial] × 100) for targeted comparisons to evaluate the relationship between changes in (1) HOOS ADL and TUG, (2) HOOS ADL and SCT, and (3) HOOS ADL and 6MW from pre-op to 1 month post-op and 1 month to 6 months after THA. The HOOS ADL subscale was chosen for correlation analyses because its content was most closely related to the performance-based measures being evaluated. In addition, similar correlational analysis was performed to evaluate the relationships between changes in the HOOS Pain subscale and changes in all three functional performance measures over the same timeframes to investigate the relationship between function and self-reported pain outcomes. Finally, Pearson product moment correlations were calculated to evaluate the relationship between the changes in HOOS ADL and HOOS Pain subscales over the same timeframes. All reported P-values are 2-tailed with an alpha value of 0.05. Correlations were defined as low if the coefficient was less than 0.3, moderate if it was between 0.3 and 0.5, and strong if it was greater than 0.5.
Results
Twenty-three adults, 16 women and 7 men, aged 61.4 ± 8.3 years with mean body mass index of 29.2 ± 5.1 kg/m2 participated in the study. Each participant had been diagnosed with end-stage hip OA and was scheduled for primary, posterior approach THA to be performed within 2 weeks of the pre-operative study visit. Scores on the HOOS ADL subscale significantly improved on average almost 40% at 1 month post-operative (p<0.001; Table 1) and HOOS Pain subscale scores improved on average almost 60% (p< 0.01; Figure 1). In contrast, there were significant declines in TUG time (p=0.02), SCT time (p<0.001), and 6MW (p=0.03) (Figure 1; Table 1) one month after THA. During the 1 to 6 month time frame, HOOS ADL and Pain subscales significantly improved on average 29% and 18%, respectively (p<0.01; Table 1). Over the same time frame, TUG time improved on average 26% (p<0.01), SCT time improved on average 42% (p<0.01) and 6MW time improved on average 29% (p<0.01) (Table 1, Figure 1).
Table 1.
Raw data for all outcome measures. Data are mean ± SD. Abbreviations: HOOS=Hip dysfunction and Osteoarthritis Outcome Score; ADL=Activities of Daily Living; TUG=Timed up and Go; SCT=stair climb test; 6MW= Six minute walk.
| Outcome | Preoperative | One month postoperative | Six months postoperative |
|---|---|---|---|
| TUG (s) | 8.80 ± 3.27 | 10.86 ± 5.87 | 7.28 ± 1.90 |
| SCT (s) | 14.84 ± 6.35 | 21.56 ± 13.70 | 11.21 ± 3.92 |
| 6MW (m) | 460.99 ± 123.36 | 419.77 ± 119.75 | 544.62 ± 111.55 |
| HOOS ADL subscale | 54.22 ± 18.81 | 74.68 ± 14.36 | 93.16 ± 7.88 |
| HOOS Pain subscale | 51.74 ± 18.13 | 78.04 ± 14.53 | 89.67 ± 11.06 |
Figure 1.
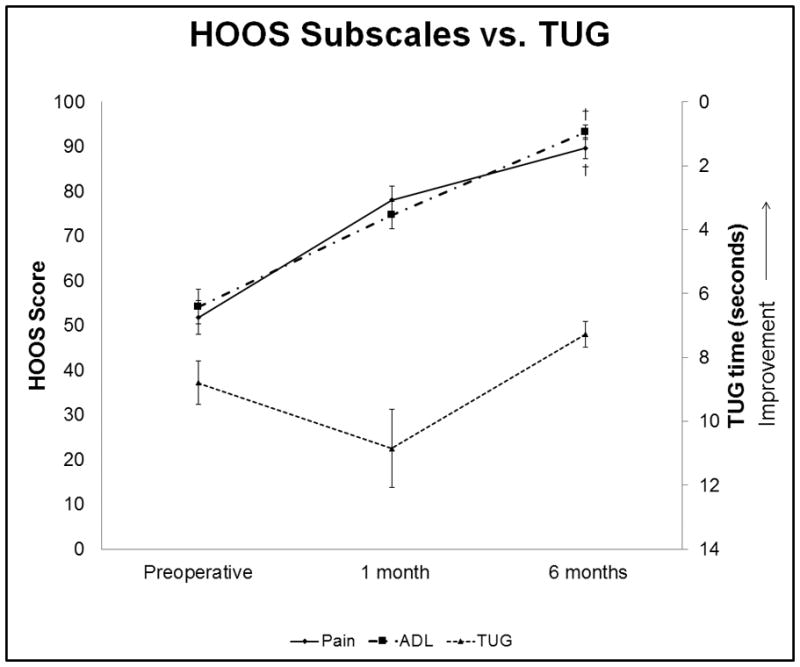
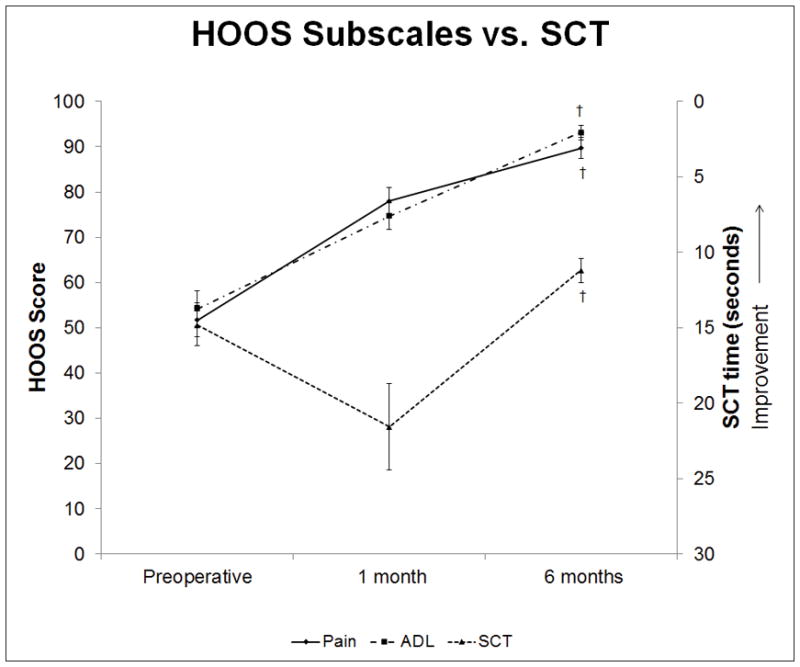
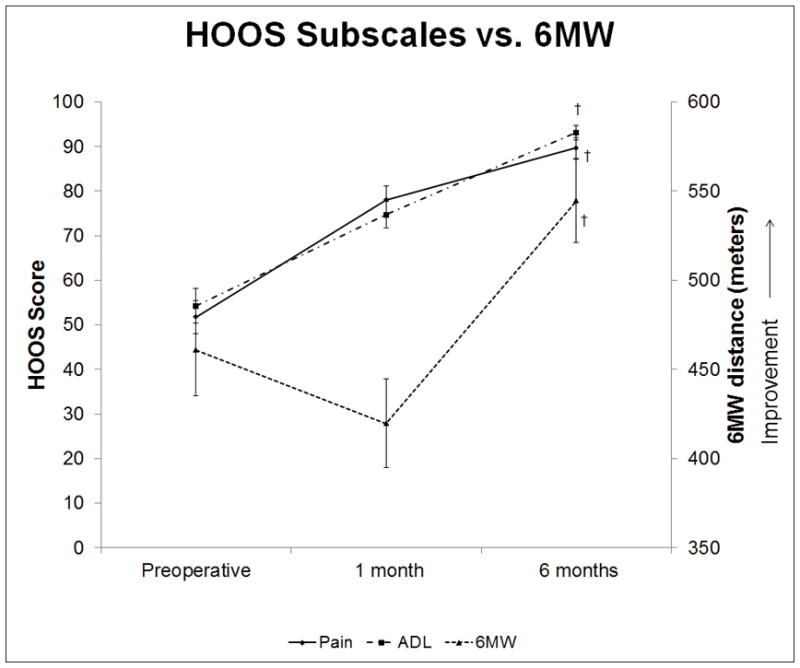
A–C. Functional performance outcomes compared to HOOS subscales. Data are mean ±SE. * indicates significant difference from pre-operative measures to one month postoperative. † indicates significant difference from one to six months post-operative.
Consistent with the first hypothesis, changes in HOOS ADL subscale were not well correlated with performance-based assessments both at 1 and 6 months after THA. Specifically, the results of the correlational analysis from pre-op to 1 month indicated there was poor correlation between change in HOOS ADL subscale and change in TUG (r=0.08, p=0.68, Table 2) and between change in HOOS ADL subscale and change in SCT (r=0.08, p=0.72, Table 2). However, a moderate correlation existed between HOOS ADL and 6MW time (r=0.46, p=0.03). Additionally, the results of the correlational analysis from 1 to 6 months post-op indicate continued discord between self-report and performance-based measures. There was poor correlation between change in the HOOS ADL subscale and change in TUG (r=.32, p=0.16), SCT(r=.27, p=0.24), and 6MW (r=0.34, p=0.13) performance during this time frame.
Table 2.
Correlations between the change in functional measures (TUG, SCT, 6MW) and change in self report (HOOS ADL and Pain subscales) measures from the preoperative time point to one month postoperative and from one month to six months postoperative. Abbreviations: HOOS=Hip dysfunction and Osteoarthritis Outcome Score; ADL=Activities of Daily Living; TUG=Timed up and Go; SCT=stair climb test; 6MW= Six minute walk.
| Preoperative-One Month Outcomes | One-Six Month Outcomes | ||||
|---|---|---|---|---|---|
| Correlation Coefficient | P-value | Correlation Coefficient | P-value | ||
| HOOS ADL vs. TUG | 0.08 | 0.68 | HOOS ADL vs. TUG | 0.32 | 0.16 |
| HOOS ADL vs. SCT | 0.08 | 0.72 | HOOS ADL vs. SCT | 0.27 | 0.24 |
| HOOS ADL vs. 6MW | 0.46 | 0.03 | HOOS ADL vs. 6MW | 0.34 | 0.13 |
| HOOS Pain vs. TUG | 0.04 | 0.87 | HOOS Pain vs. TUG | 0.11 | 0.64 |
| HOOS Pain vs. SCT | 0.04 | 0.85 | HOOS Pain vs. SCT | 0.01 | 0.96 |
| HOOS Pain vs. 6MW | 0.49 | 0.02 | HOOS Pain vs. 6MW | 0.07 | 0.77 |
| HOOS ADL vs. HOOS Pain subscales | 0.51 | 0.02 | HOOS ADL vs. HOOS Pain subscales | 0.70 | <0.01 |
Also consistent with the first hypothesis, changes in HOOS Pain subscale scores were not correlated with changes in functional performance at both the 1 and 6 month post-op time points. Specifically, there was poor correlation between change in HOOS Pain subscale and change in TUG (r=−0.04, p=.87) and between change in HOOS Pain subscale and change in SCT (r=0.04; p=0.85) from pre-op to 1 month post-op. Similar to the relationship with the HOOS ADL subscale, there was a moderate, but significant correlation between HOOS Pain subscale and change in 6MW distance (r=0.49, p=0.02) during this time frame. Further, poor correlations were found between changes in HOOS Pain subscale and changes in TUG (r=.107, p=0.64), SCT (r=0.01, p=0.96), and 6MW distance (r=0.07, p=0.77) during the 1 to 6 month post-op time frame.
Finally, there was a moderate and significant correlation between changes in the HOOS ADL subscale and the HOOS Pain subscale (r=0.51, p=0.02) from pre-op to 1 month post-op and strong and significant correlation between changes in each HOOS subscale (r=0.70, p<0.01) during the 1 to 6 month post-op time frame.
Discussion
Self-report measures, such as the HOOS, are used to evaluate recovery and success of THA surgery. However, self-report measures may not fully capture limitations in functional recovery. Performance-based outcome measures may provide additional information regarding patients’ functional capacity to inform clinical decision making. This investigation sought to characterize the changes in both self-report and performance-based measures to compare the relationship between these outcomes in patients undergoing THA. The findings presented indicated that changes in self-reported measures and performance-based measures are not correlated with each other during the first 6 months of recovery after THA. Important postoperative changes occur early after THA, as functional performance is compromised as early as one week after THA.22 Consistent with this literature, this cohort demonstrated functional decline which was still present 1 month after surgery. Specifically, these patients demonstrated difficulty walking, transitioning from seated to standing, and climbing stairs. Additionally, during this time frame after surgery, individuals often still use an assistive device for ambulation and require assistance at home for activities of daily living and self-care.
Despite the relative decline in functional capacity 1 month after THA, individuals in this study reported improvements in their HOOS ADL subscale scores 1 month after THA. This finding confirmed our hypothesis that the HOOS ADL subscale score and functional performance (TUG, SCT, and 6MW) data would not correlate with one another during recovery from THA. Specifically, individual comparisons between the HOOS ADL sub-scale and change in the three functional demonstrated poor correlation at the first post-operative assessment, with only the change in 6MW distance demonstrating a moderate, but significant correlation to the HOOS ADL subscale during this time (Table 2). The finding of a moderate relationship between the HOOS ADL subscale and 6MW distance is likely due to the fact that, relative to the other functional performance measures, there was less decline in 6MW distance 1 month after THA. Specifically, 6MW distance declined about 40 meters (<10% decline) so although patients reported improvements in the HOOS ADL subscale (in contrast to the decline in 6MW), the smaller magnitude of 6MW change compared to other functional measures, likely accounted for the moderate correlation. During the recovery period which follows the first post-operative month (1–6 months), improvements in self-report on the HOOS ADL subscale were accompanied by improvements in functional performance. However, the self-reported and performance-based outcomes were still poorly correlated. The improvement of HOOS ADL subscale scores is notable as it does not appear to affect or be affected by the changing trend in functional scores from pre-op to 1- and 6-month post-operatively. Final functional performance values at 6 months, compared to those at the pre-operative assessment (Table 1), attest to the increase in performance that occurred following the first post-operative month. Although a stronger relationship begins to emerge, suggesting that patient perception of recovery and actual functional capacity may be more closely aligned at a later time, these relationships were still not strong enough to be significantly correlated. This finding supports the combined use of self-report and functional performance outcomes throughout the post-operative period.
Further support for the presence of disagreement between self-reported outcomes and functional performance measures early after THA was found when examining the relationship between the HOOS Pain subscale and functional performance measures. Similar to the relationship between the HOOS ADL subscale and functional performance early after surgery, patients reported improvements in pain, while declines in functional performance existed. This finding suggests that functional capacity is not determined by pain experienced by the patient after THA. While patients experience the majority of post-operative pain in the early peri-operative period, perception of pain after surgery may not approach the cumulative discomfort associated with underlying pre-operative degenerative disease before surgery. Hence, self-reported post-operative HOOS Pain scores may represent an optimistic outlook relative to both the pre-operative state and decline in functional performance during the early post-operative period. The significant correlations found between HOOS ADL and HOOS Pain trajectories appear to indicate that patients’ perception of ability to complete functional tasks may be related to their perception of whether or not that task is painful, rather than the efficiency by which they complete the task. This observation is similar to that noted in a recent investigation and supports the assertion that improvements in pain observed post-operatively among patients undergoing THA will likewise improve all facets of self-report.7 Despite the suggestion that patient perception of function is driven by pain, self-report measures are valuable. Assessment of patients’ perception of recovery provides additional information to consider when making post-operative decisions such as participation in rehabilitation. Further, this information could be useful in educating patients regarding appropriate activity resumption.
The disparity between early functional performance measures and self-report is consistent with studies of patients following joint arthroplasty, such as TKA. 7,15,19,23 Interestingly, in contrast to a similar study with TKA, the functional performance measures in THA returned to and exceeded pre-operative levels by 6 months post-operatively.7,15 Yet, published data has also suggested that functional performance both pre- and post-operatively among patients following TKA is significantly less than that of healthy age-matched controls.24 While similar data does not currently exist in a similarly reported manner for patients undergoing THA, deficits in this patient population will encourage future investigations designed to improve patient outcomes.
The HOOS instrument was designed to assess patients’ perception of functional ability. Specifically, the HOOS asks for responses on patients’ current self-perceived functional status by asking patients to recall difficulty with specific tasks within the last week. However, it does not ask patients to answer the questions relative to previous time points, such as pre-operative functional status. However, the lack of significant correlations between HOOS subscales and performance-based outcome measures is important to note, suggesting that self-report measures may fail to provide an accurate picture of patients’ functional capacity after THA. Outcomes assessment after THA is important to guide post-operative management and rehabilitation priorities. However, self-report and performance-based measures suggest inverse trajectories of recovery, and a poor relationship to one another throughout the first 6 months of recovery after surgery. The findings of the study suggest that patients’ perception of their functional performance may be driven by improvements in pain post-operatively, although their underlying capacity to produce movement for these tasks is compromised compared with pre-operative levels. Thus, the combination of self-report and performance-based outcome measures, rather than the sole reliance on self-report measures should be utilized to characterize recovery and inform post-operative decisions.
Limitations
Potential limitations of this study are acknowledged. The present investigation includes a relatively low number of enrolled patients; with the number of patients present, however, some significant differences were noted. It is also worthwhile to consider the follow-up period was only 6 months. While it is clear that temporal differences in the first post-operative month do exist in the rate of recovery between HOOS subscales and performance-based measures in patients undergoing THA, the relationships begin to improve during the 1–6 month time frame, suggesting a possibility that this relationship may further improve at time points further out from surgery. Lastly, functional performance measures, while objective and uniquely contributory, assess only individual modeled tasks, and may fail to broadly capture a cross-section of daily activities. This last limitation may allow any given patient to perform at an exceptional level with unique individual activities, while excluding additional functional activities not achievable. Therefore, patient perception of progress on a day to day basis, even if subjective, may encompass a greater breadth of function than an individual assessment can make at a given time point.
To our knowledge, this is the first investigation to characterize the relationship between the changes HOOS ADL and Pain subscales and changes in performance-based measures after THA. The findings are consistent with previous publications which suggest that discrepancies between self-report and performance-based measures exist.7,15,19,23 Specifically, results from these investigations suggested more profound negative changes in performance-based measures immediately following surgery accompanied with significant positive responses in self-report measures closer to one year post-operatively. The consistency of the present results with previous literature has implications for clinical practice. Although self-report measures are often used due to their ease of administration and cost-effectiveness, clinical decisions regarding post-operative care should not solely rely on these instruments, particularly in the first post-operative month. Considering both performance-based and self-report measures may provide a more comprehensive picture to inform post-operative clinical decision making. The consideration of both performance-based recovery and patients’ self-report of recovery should guide post-operative management and rehabilitation priorities to ensure both maximal recovery and patient satisfaction.
In summary, multiple factors are important in establishing outcomes following THA. Self-report outcomes as assessed by HOOS ADL and Pain subscales did not reflect the magnitude of deficits present in the first post-operative month and failed to accurately represent changes in functional capacity during the first 6 months of recovery. Patient perception of pain, as measured by the HOOS Pain subscale may contribute to this finding. Further work may focus on the differential effects of varying surgical approaches in THA, effects of rehabilitation programs after THA, improvement in functional performance and whether the relationship to self-reported measures such as the HOOS remains the same.
Footnotes
Author Disclosures:
Funding: NIH K23AG029978 and UL1 TR000154; American College of Rheumatology REF/Abbot Health Professionals Graduate Student Research Preceptorship Award The authors affirm that we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript, except as disclosed in an attachment and cited in the manuscript.
References
- 1.Buckwalter JA, Saltzman C, Brown T. The impact of osteoarthritis: implications for research. Clin Orthop Relat Res. 2004;(Suppl):S6–S15. doi: 10.1097/01.blo.0000143938.30681.9d. [DOI] [PubMed] [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Schnaser E, Scarcella NR, Vallier HA. Acetabular fractures converted to total hip arthroplasties in the elderly: How does function compare to primary total hip arthroplasty? J Orthop Trauma. 2014 Apr 30; doi: 10.1097/BOT.0000000000000145. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 4.Keeler E, Guralnik JM, Tian H, Wallace RB, Reuben DB. The impact of functional status on life expectancy in older persons. J Gerontol A Biol Sci Med Sci. 2010;65(7):727–33. doi: 10.1093/gerona/glq029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Seeman I. Data on disability. Am J Public Health. 2010;100(8):1367. doi: 10.2105/AJPH.2010.193276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC; a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–40. [PubMed] [Google Scholar]
- 7.Gandhi R, Tsvetkov D, Davey JR, Syed KA, Mahomed NN. Relationship between self-reported and performance-based tests in a hip and knee joint replacement population. Clin Rheumatol. 2009;28:253–7. doi: 10.1007/s10067-008-1021-y. [DOI] [PubMed] [Google Scholar]
- 8.Stucki G, Sangha O, Stucki S, Michel BA, Tyndall A, Dick W, Theiler R. Comparison of the WOMAC (Western Ontario and McMaster Universities) osteoarthritis index and a self-report format of the self-administered Lequesne-Algofunctional index in patients with knee and hip osteoarthritis. Osteoarthritis Cartilage. 1998;6(2):79–86. doi: 10.1053/joca.1997.0097. [DOI] [PubMed] [Google Scholar]
- 9.Söderman P, Malchau H, Herberts P. Outcome of total hip replacement: A comparison of different measurement methods. Clin Orthop Relat Res. 2001;(390):163–72. doi: 10.1097/00003086-200109000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Soohoo NF, Vyas RM, Samimi DB, Molina R, Lieberman JR. Comparison of the responsiveness of the SF-36 and WOMAC in patients undergoing total hip arthroplasty. J Arthroplasty. 2007;22(8):1168–73. doi: 10.1016/j.arth.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 11.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13(8):890–5. doi: 10.1016/s0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]
- 12.Nilsdotter AK, Lohmander LS, Klässbo M, Roos EM. Hip disability and osteoarthritis outcome score (HOOS) - validity and responsiveness in total hip replacement. BMC Musculoskelet Disord. 2003;30(4):10. doi: 10.1186/1471-2474-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nilsdotter AK. Patient relevant outcome 7 years after total hip replacement for OA - a prospective study. BMC Musculoskelet Disord. 2010;11:47. doi: 10.1186/1471-2474-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009;467(10):2606–12. doi: 10.1007/s11999-009-0834-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stevens-Lapsley JE, Schenkman ML, Dayton MR. Comparison of self-reported knee injury and osteoarthritis outcome score to performance measures in patients after total knee arthroplasty. Phys Med and Rehab. 2011;3:541–9. doi: 10.1016/j.pmrj.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Judd DL, Dennis DA, Thomas AC, Wolfe P, Dayton MR, Stevens-Lapsley JE. Muscle strength and functional recovery during the first year after THA. Clin Orthop Relat Res. 2014;472(2):654–64. doi: 10.1007/s11999-013-3136-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stratford PW, Kennedy DM, Riddle DL. New study design evaluated the validity of measures to assess change after hip or knee arthroplasty. J Clin Epidemiol. 2009;62:347–352. doi: 10.1016/j.jclinepi.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 18.Jacobs CA, Christensen CP. Correlations between knee society function scores and functional force measures. Clin Orthop Relat Res. 2009;467:2414–2419. doi: 10.1007/s11999-009-0811-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kennedy D, Stratford PW, Pagura SM, Walsh M, Woodhouse LJ. Comparison of group and gender differences in self-report and physical performance measures in total hip and knee arthroplasty candidates. J Arthroplasty. 2002;17:70–7. doi: 10.1054/arth.2002.29324. [DOI] [PubMed] [Google Scholar]
- 20.Witvrouw E, Victor J, Bellemans J, et al. A correlation study of objective functionality and WOMAC in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2002;10:347–351. doi: 10.1007/s00167-002-0302-2. [DOI] [PubMed] [Google Scholar]
- 21.Parent E, Moffet H. Comparative responsiveness of locomotor tests and questionnaires used to follow early recovery after total knee arthroplasty. Arch Phys Med Rehabil. 2002;83:70–80. doi: 10.1053/apmr.2002.27337. [DOI] [PubMed] [Google Scholar]
- 22.Holm B, Thorborg K, Husted H, Kehlet H, Bandholm T. Surgery-induced changes and early recovery of hip-muscle strength, leg-press power, and functional performance after fast-track total hip arthroplasty: a prospective cohort study. PLoS One. 2013;8(4):e62109. doi: 10.1371/journal.pone.0062109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mizner RL, Petterson SC, Clements KE, Zeni JA, Jr, Irrgang JJ, Snyder-Mackler L. Measuring functional improvement after total knee arthroplasty requires both performance-based and patient-report assessments: a longitudinal analysis of outcomes. J Arthroplasty. 2010 Sep 17; doi: 10.1016/j.arth.2010.06.004. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Finch E, Walsh M, Thomas SG, Woodhouse LJ. Functional ability perceived by individuals following total knee arthroplasty compared to age-matched individuals without knee disability. J Orthop Sports Phys Ther. 1998;27:255–63. doi: 10.2519/jospt.1998.27.4.255. [DOI] [PubMed] [Google Scholar]


