Abstract
Objective
To investigate the association between kava use and the risk of four-wheeled motor vehicle crashes in Fiji. Kava is a traditional beverage commonly consumed in many Pacific Island Countries. Herbal anxiolytics containing smaller doses of kava are more widely available.
Methods
Data for this population-based case-control study were collected from drivers of ‘case’ vehicles involved in serious injury-involved crashes (where at least one road user was killed or admitted to hospital for 12 hours or more) and ‘control’ vehicles representative of ‘driving time’ in the study base. Structured interviewer administered questionnaires collected self-reported participant data on demographic characteristics and a range of risk factors including kava use and potential confounders. Unconditional logistic regression models estimated odds ratios relating to the association between kava use and injury-involved crash risk.
Findings
Overall, 23% and 4% of drivers of case and control vehicles, respectively, reported consuming kava in the 12 hours prior to the crash or road survey. After controlling for assessed confounders, driving following kava use was associated with a four-fold increase in the odds of crash involvement (Odds ratio: 4.70; 95% CI: 1.90–11.63). The related population attributable risk was 18.37% (95% CI: 13.77–22.72). Acknowledging limited statistical power, we did not find a significant interaction in this association with concurrent alcohol use.
Conclusion
In this study conducted in a setting where recreational kava consumption is common, driving following the use of kava was associated with a significant excess of serious-injury involved road crashes. The precautionary principle would suggest road safety strategies should explicitly recommend avoiding driving following kava use, particularly in communities where recreational use is common.
Introduction
Of the approximately 1.24 million road deaths each year, almost 95% occur in low and middle income countries [1]. Furthermore, the burden of road traffic injuries in many of these countries is projected to increase sharply in coming decades imposing substantial demands on poorly resourced healthcare systems, compromising the development of fragile economies, and making millions of people vulnerable to increased poverty and on-going suffering [1].
These inequitably borne consequences highlight the importance of implementing effective road safety strategies that take particular account of risk factors in less-resourced settings [1–3]. We were concerned that while alcohol, some medicines and drugs (licit and illicit) [1, 4–7] are well-recognised risk factors in high-income countries, little is known of the possible contribution to crashes from kava, a traditional soporific substance commonly consumed in several small island developing states in the Pacific region.
Kava is a popular intoxicating beverage extracted from the roots of the plant Piper methysticum, a perennial shrub native to most Pacific Island countries and territories [8]. As noted in our review of the published literature[9], while some authorities recommend caution when driving and operating heavy machinery following the use of high doses of kava, there is a notable lack of epidemiological studies investigating the contribution of the recreational use of kava to road traffic injuries. The published literature on the potential risks involved are confined to experimental studies on the effects of small doses of kava when operating driving simulators, the results of which are inconclusive [9]. These doses (e.g., 180–300 mg kavalactones) are consistent with the concentrations of kava found in dietary supplements that are becoming more widely available in Western countries as herbal remedies for the relief of anxiety, menopausal symptoms and other putative health benefits [10–12].
Recreational use of kava in many Pacific Island countries typically involves doses more than 50 times that in herbal and therapeutic preparations [13]. We investigated the association between driving after consuming kava and serious injury-involved four-wheeled motor vehicle crashes in Fiji.
Materials and Methods
Study setting and design
A population-based case-control study was undertaken in Viti Levu, Fiji, from July 1, 2005 to December 31, 2006. Viti Levu is home to 70% of Fiji’s resident population of 837,271 [14]. About 20% of the public roads on the island are tar sealed, and cars and commercial vehicles account for approximately 86% of the driving fleet [15]. This study was approved by the Fiji National Research and Ethics Review Committee (FNRERC Ref No. 023–2004), Suva, Fiji and the University of Auckland Human Participants Ethics Committee, Auckland, New Zealand (UAHPEC Ref No. 2005/095). All participants provided written informed consent as approved by the Ethics committees. The roadside survey was granted approval by the Fiji Police Force Highway Unit.
Unintentional injuries such as road traffic injuries are rare events and are therefore suited to a case-control design[16]. For the valid conduct of a case-control study, both the cases and controls need to come from the same study base [17, 18]. Drawing on the deductive research methodology employed in the Auckland Car Crash Injury Study [19], the study base for this research comprised “motor vehicle driving time” (equivalent to person-time) on public roads in Viti Levu.
Eligible vehicles included motorised four-wheeled motor vehicles such as private cars, taxis, minibuses, pick-ups, trucks, and commercial or government vehicles. Buses, motorbikes, ambulance, police vehicles, and vehicles of the Diplomatic Corp were excluded.
Due to the low risk of crashes as indicated by Fiji Police traffic data, the following were excluded from the study base: roads with an average flow of less than 200 vehicles per day and vehicles driven between the hours of 2.00am and before 5.00am [20].
Participants
Case recruitment
The case and control selection process for this study has been described in detail in a previous publication arising from this research that explored the role of sleepiness in car crash injury in this population [21]. Cases comprised four-wheeled motor vehicles involved in a crash in the study base where a road user (driver, passenger or pedestrian) died or was hospitalised for 12 hours or more during the study period. For all cases (crash vehicles), the driver comprised the key informant of interest. Cases were prospectively identified from road crash-related admissions recorded at all trauma-admitting hospitals in Viti Levu. This system identified injured individuals from emergency department registers, admission records, and mortuary registers [22]. In situations where the hospitalised crash victim was someone other than the driver (e.g. a vehicle passenger or a pedestrian), the driver of the crash vehicle was identified through the assistance of Traffic Police or hospital staff and invited to participate. If the driver had died or was unable to participate due to severe injuries, proxy interviews were sought from either a passenger who was also involved in the crash or family member(s).
Control recruitment and sampling
Controls comprised a sample representative of motor vehicle ‘driving time’ in the study base, and were identified using a prospective two-stage cluster sample roadside survey design. Recruitment of eligible four-wheeled motor vehicles occurred at 50 randomly selected eligible road sites (longer than 400 meters and with daily traffic counts of 200 or more vehicles). This sampling approach was used to ensure controls were sampled in proportion to the amount of driving undertaken given that the exposure to risk of a crash only occurred when a person is driving. Random sampling of vehicles occurred over a two-hour period at safe sections of road at each survey site on random days of the week, time of the day, and direction of travel. We also collected traffic counts for each survey of all vehicles travelling in the same direction as the vehicles that were selected for the study. This was to enable a weighting to be assigned to controls from each site that was the inverse of the proportion of all vehicles selected as controls.
In accordance with national transport protocols and institutional review board (ethics committee) requirements in Fiji, Traffic Police managed the slowing of traffic and stopping of selected vehicles. All other research procedures including the provision of information sheets and consent forms for potential participants were undertaken by the research team.
Study instrument and variables
Cases completed an interviewer-administered questionnaire either face-to-face in hospital, at home, or via telephone. For control drivers, interviews were conducted face-to-face on-site or in another location convenient for the driver or via telephone.
The 72-item questionnaire (S1 and S2 Questionnaires) captured information about vehicle details (e.g. type of vehicle, brand, model, year of manufacture, seatbelt fitting), circumstances of the crash/survey (e.g. vehicle speed, wet road conditions), health status (e.g. sleep apnoea, depression, prescription medication use), driving experience, socio-demographic characteristics (e.g. age, gender, ethnicity, household income) and frequency of usual alcohol, kava and recreational drug use in the previous 12 months. In addition, drivers were asked if they had consumed kava or alcohol in the 12 hours prior to the crash or survey (defined as ‘acute use’), and if so the amount they had consumed. They were also asked how frequently they had consumed kava during the previous 12 months (defined as ‘usual kava use’).
Ethnicity data used in this study was self-determined by participants. The two main ethnic groups in Fiji are the indigenous Fijians (iTaukei) and Indians, who make up 57% and 38% of Fiji’s population, respectively [14]. The decision to compare the two major ethnic groups in Fiji in this study was due to their distinct cultural practices and therefore the likely need for ethnic-specific interventions.
Measurement of kava
While we attempted to quantify the amount of kava consumed by drivers, the variable preparations, concentrations and context in which kava was consumed and shared made it difficult to quantify and standardise the amount of kava consumed. Given the resources and technology available, this study did not undertake an objective measurement of kava.
Statistical Analysis
We formulated an analysis plan to firstly describe the characteristics of the cases and controls. Weighted proportions were used for the control data to adjust for the cluster sampling design. Secondly, the relationship between acute kava use (previous 12 hours) and car crash injury was explored. Odds ratios (ORs) and 95% confidence intervals (CIs) were obtained using unconditional logistic regression adjusted for demographic variables and other potential confounders.
The OR is a measure of association which compares the odds of an outcome (e.g. car crash) in in those exposed (e.g. consumed kava 12 hours prior to driving) to the odds of an outcome in those unexposed.[23] This is expressed in the following manner:
Finally, multivariable modelling was undertaken employing the 10% change-in-estimate method described by Greenland [24]. In this approach, variables that remain significant after initial adjustment are placed into a second model. Using the backward-deletion algorithms, the second model commenced with all potential variables (including the exposure variable of interest and those that were forced into the model). As each variable is dropped from the second model, those that result in a 10% change in the estimated exposure effect are selected to remain in model, whereas those that do not are deleted. All factors in the multivariable models had less than 10% missing data.
Population attributable risks were calculated using published methods [25]. The interaction between kava use (previous 12 hours) and alcohol use (previous 12 hours) on the risk of four-wheeled motor vehicle crash was tested statistically. Sensitivity analyses investigated the influence of factors that could bias the effect estimates.
Results
Participant characteristics and response rates
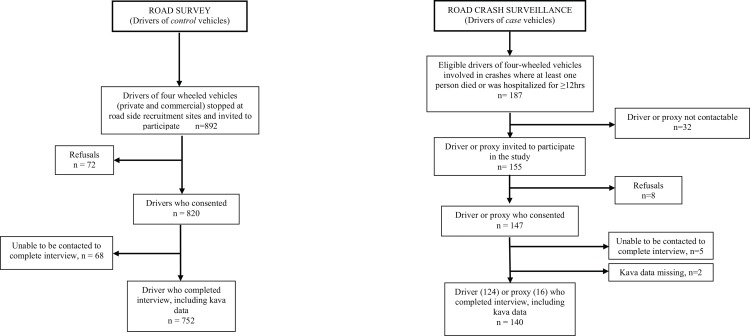
Of the 187 eligible case vehicles, 140 (74.9%) drivers or their proxies completed interviews including information on kava consumption (Fig 1). Eight (4.3%) of the eligible drivers declined to participate, and the remainder (20.8%) could not be contacted, were unable to complete the interview or did not provide kava consumption data. Of the 892 control vehicles, 752 (84.3%) drivers completed interviews, 72 (8.1%) declined, 68 (7.6%) were untraceable or could not be interviewed within one month of consenting to participate (Fig 1).
Fig 1. Case and control selection and recruitment, Viti Levu, Fiji, 2006.
In both cases and control vehicles, over 90% of drivers were male and more than 70% were aged less than 45 years. Most four-wheeled motor vehicles in the study were cars (Table 1).
Table 1. Distribution of kava consumption and potential confounders for cases and controls, Fiji, 2006.
| Characteristics | No. (%) of Drivers | |
|---|---|---|
| Case (n = 140) | Control (n = 752)a | |
| Age of drivers (years) | ||
| 15–24 | 19 (13.6) | 84 (12.9) |
| 25–34 | 48 (34.3) | 220 (31.8) |
| 35–44 | 36 (25.7) | 223 (29.3) |
| 45+ | 37 (26.4) | 223 (25.9) |
| Declined to answer/missing data | 0 (0) | 2 (0.3) |
| Gender | ||
| Female | 6 (4.3) | 35 (6.8) |
| Male | 134 (95.7) | 717 (93.2) |
| Ethnicity | ||
| Fijian (iTaukei) | 42 (30.0) | 154 (21.9) |
| Indian | 96 (68.6) | 551 (70.1) |
| Other | 2 (1.4) | 47 (8.0) |
| Household Income ($FJD) | ||
| ≥$20,000 | 29 (20.7) | 231 (35.3) |
| $10,000 - $19,999 | 38 (27.1) | 239 (38.1) |
| <$10,000 | 66 (47.1) | 275 (25.8) |
| Declined to answer/missing data | 7 (5.0) | 7 (0.9) |
| Acute Kava use (previous 12 hours) | ||
| No | 108 (77.1) | 698 (95.7) |
| Yes | 32 (22.9) | 54 (4.3) |
| Usual Kava use (past 12 months) | ||
| None to less than monthly | 46 (32.9) | 374 (58.3) |
| Once a month to once a week | 50 (35.7) | 221 (25.7) |
| Several times a week to daily | 44 (31.4) | 157 (16.0) |
| Acute alcohol use (previous 12 hours) | ||
| No | 120 (85·7) | 734 (96.5) |
| Yes | 20 (14·3) | 18 (3.5) |
| Time of crash | ||
| 0500 – 1200hrs | 42 (30.0) | 219 (9.8) |
| 1201 – 1900hrs | 50 (35.7) | 387 (78.9) |
| 1901 – 0200hrs | 48 (34.3) | 146 (11.3) |
| Vehicle speed (km per hour) | ||
| ≤50 | 52 (37.1) | 502 (74.4) |
| 51–60 | 29 (20.7) | 160 (21.2) |
| ≥61 | 46 (32.9) | 90 (4.5) |
| Missing data | 13 (9.3) | 0 (0) |
| Car type | ||
| Cars | 88 (62.9) | 468 (67.3) |
| Minibuses/vans | 35 (25.0) | 257 (29.8) |
| Trucks | 17 (12.1) | 27 (2.9) |
| Wet road condition | ||
| No | 109 (77.9) | 680 (94.0) |
| Yes | 31(22.1) | 72 (6.0) |
| Type of driving licence | ||
| Full licence | 114 (81.4) | 712 (94.2) |
| Provisional/ no licence | 26 (18.6) | 40 (5.8) |
| Driver in a crash in the past 5 years | ||
| No | 126 (90.0) | 620 (79.7) |
| Yes | 13 (9.3) | 130 (20.3) |
| Missing data | 1 (0.7) | 2 (<0.1) |
a weighted proportions.
Kava consumption, confounding and crash-related injury
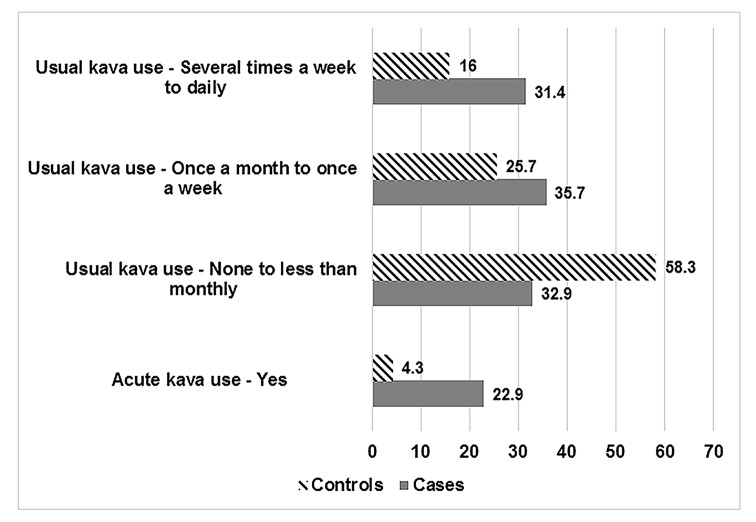
Among drivers of case and control four-wheeled motor vehicles, 22.9% (32/140) and 4.3% (54/752) respectively, reported drinking kava in the 12 hours prior to the crash or survey (Fig 2). Nearly two times more drivers of case vehicles (31.4%; n = 44/140) reported drinking kava ‘several times a week to daily” in the past 12 months as compared to drivers of control vehicles (16%; n = 157/752).
Fig 2. Distribution of acute (previous 12 hours) and usual (past 12 months) kava use among cases and controls.
There was a six-fold excess in the odds of injury-involved road traffic crashes among those consuming kava in the previous 12 hours compared with those who did not, after controlling for the potential socio-demographic confounders of age, gender, ethnicity, and household income (OR: 6.59; 95% CI: 2.88–15.09) (Table 2). Following additional adjustments for usual kava use (past 12 months), acute alcohol use (previous 12 hours), time of crash, vehicle speed and wet road condition, the associated odds ratio remained significant at 4.70 (95% CI: 1.90–11.63) (Table 2). The associated population attributable risk (PAR) was 18.37% (95% CI: 13.77–22.72).
Table 2. Association of self-reported kava use with risk of car crash resulting in injury, Fiji, 2006.
| Variable | Unadjusted Odd Ratioa | p-value | Adjusted Odds Ratiob | p-value | Adjusted Odds Ratioc | p-value |
|---|---|---|---|---|---|---|
| (95% CI) | (95% CI) | (95% CI) | ||||
| Acute kava use (previous 12 hours) | ||||||
| No | 1.00 | <0.001 | 1.00 | <0.001 | 1.00 | 0.001 |
| Yes | 6.57 (2.91, 14.80) | 6.59 (2.88, 15.09) | 4.70 (1·90, 11.63) | |||
| Usual kava use (past 12 months) | ||||||
| None to less than monthly | 1.00 | <0.001 | 1.00 | <0.001 | 1.00 | 0.04 |
| Once a week to once a month | 2.47 (1.45, 4.22) | 2.26 (1.27, 4.02) | 1.75 (0.96, 3.19) | |||
| Several times a week to daily | 3.48 (2.01, 6.04) | 3.20 (1.68, 6.07) | 2.04 (1.10, 3.79) |
CI: confidence interval
a Adjusted for sampling design
b Derived from a multivariable logistic regression model that was adjusted for age, gender, ethnicity and household income
c Derived from a multivariable logistic regression model that adjusted for age, gender, ethnicity, household income, acute kava use (previous 12 hours), usual kava use (past 12 months), acute alcohol use (previous 12 hours), time of crash, vehicle speed, wet road condition.
We further explored the data to assess potential effect modifiers and the influence of biases. We found no interaction between the main effect of interest (driving following kava use and injury-involved crashes) and the alcohol consumption in the same recall period (p = 0.72). Given the potential for misclassification of exposures, a sensitivity analysis was undertaken where data from the 16 proxy respondents were excluded. There was minimal change in the main effect of interest, driving after kava use (OR: 4.93; 95% CI: 1.97–12.35) or the associated PAR (18.71%; 95% CI: 14.25–22.95).
We also examined the association injury-involved crash risk with kava use over the previous 12 months. Monthly to daily use was reported by 67% and 42% of drivers of case and control four-wheeled motor vehicles, respectively. After adjusting for socio-demographic variables, the odds of injury-involved crashes were significantly higher among those reporting kava drinking ‘once a month to once a week’ (OR: 2.26; 95% CI: 1.27–4.02) and ‘several times a week to daily’ (OR: 3.20; 95% CI: 1.68–6.07) when compared with the reference category of ‘none to less than monthly’. (Table 2) Although these effects were attenuated when the estimates were adjusted for other confounders, the associated odds of crash remained significant for kava drinking ‘several times a week to daily’ (OR: 2.04; 95% CI: 1.10–3.79).
Driving within 12 hours of drinking kava (main effect of interest) and usual kava use (frequency of kava use in the previous 12 months) could be considered as factors in the same causal pathway. When usual kava use was excluded from the main effect model, the odds associated with acute kava use increased to 6.04 (95% CI: 2.38–15.28) with an associated PAR of 19.47% (95% CI: 15.82–22.95).
Discussion
This case-control study conducted in Fiji (one of several Pacific Island countries where social or recreational use of the substance is common) found a four-fold excess in the odds of crash involvement associated with driving within 12 hours of consuming kava. This finding remained significant after adjustment for confounding factors including self-reported alcohol use. The related population attributable risk suggests that avoiding driving following kava consumption could reduce the population burden of these injuries by up to 18%. Frequent use of kava over the previous 12 months was also associated with increased odds of injury-involved crashes. To our knowledge, this is the first study to investigate the contribution of driving following the use of kava to serious injury-involved MVCs[9].
Our study was not designed to examine the risk posed by therapeutic doses of kava as found in herbal remedies. However, our findings support concerns raised by previous researchers [26, 27] and the media [28, 29] about driving after consuming kava. The Fiji Land Transport Authority has proposed banning drivers of public service vehicles from consuming kava while on work duties [30], revealing increasing support by policymakers to discourage driving following kava use. However, implementing and monitoring this strategy remains challenging in the absence of readily accessible objective measures of recent kava use and inadequate information on the levels of kava that are of greatest concern [31].
The concerns raised by our findings do not discount some therapeutic benefits of kava, nor do these counter the social and cultural significance of this beverage in Pacific communities where it is commonly consumed. However, as with alcohol and substances that have sedative effects, kava could influence crash risks through theoretically plausible biological mechanisms. For example, the GABAergic effects following the ingestion of large doses of kava include impaired performance on tasks requiring high cognitive demand and visual attention [13, 32, 33], and prolonged reaction times in neurocognitive function tests [34, 35] Although experimental studies suggest that pharmacological doses (180–300 mg kavalactones) of kava produce relatively little effect on driving performance [26, 27, 36–38], the doses investigated were substantially lower (50 to 100 times less potent) than those commonly consumed in recreational settings [9].
The extent to which alcohol potentiates crash risk due to kava requires further investigation. A human experiment conducted by Foo and Lemon revealed that kava alone (in doses found in anti-anxiolytic herbal medications) had no effect on the measures of sedation, cognition, motor coordination, intoxication and willingness to drive a car [36]. However, larger negative effects were detected when kava was combined with alcohol, and this effect was greater than the negative effects of alcohol alone. While we did not observe a significant interaction with alcohol in our study (which may relate to the limited statistical power to investigate this interaction), the experimental data suggests the risks of kava could be greater in the context of co-ingestion of alcohol, a practice (“wash down”) that is reasonably common in Fiji [39].
In this population-based study, case ascertainment was likely to be complete given the prospective recruitment strategy implemented at all hospitals and mortuaries receiving trauma patients in the region, minimising recruitment bias. Controls were sampled in proportion to the amount of driving undertaken, in preference to recruiting from an existing licensed driver database or vehicle register which do not account for driving time. However, the findings must be interpreted in light of other limitations. The study estimated the amount of kava consumed in the 12 hours prior to driving using self-reported information from participants. We were unable to standardise the quantities involved due to variations in kava cultivars, concentrations and drinking cup sizes. Objective assessment of kava remains a challenging issue in the Pacific context where laboratory testing is difficult to implement. Further research is required to establish dose-response relationships and patterns of consumption that pose the greatest crash risk. We did not gather information about environmental factors such as roading design, traffic flow, and other road engineering factors that may have played a role in the road traffic crashes in this study [40–42].
While relatively few case records had missing information in key variables relevant to this analysis, proxy reports may have resulted in misclassification of some exposure measures. However, a sensitivity analysis excluding proxy data found the influence on the effect estimate to be minimal. Differential recall of information by cases and controls can result in recall bias [43]. The methods used to minimise recall bias in this study included the standardised administration of identical exposure questions for drivers linked to a specific event (crashes for cases and a roadside stopping site for controls). While we achieved good response rates, those who did not respond may have differed systematically from those who did with respect to relevant exposures. In our multivariable regression models, we adjusted estimates to control for factors known to be associated with poor response, such as age and socio-economic status, as well as other demographic, lifestyle and travel-related variables. However, residual confounding cannot be excluded, a common challenge with observational designs.
In summary, our study found that driving following the recreational consumption of kava was associated with an excess risk in serious-injury involved road crashes in Fiji. While crash risks associated with lower doses of kava as found in some herbal remedies and the dose-response relationships more generally require further investigation, the precautionary principle would suggest that avoiding driving following kava use should be an explicit road safety target, particularly in communities where recreational use is common.
Supporting Information
(DOCX)
(DOCX)
Acknowledgments
The authors gratefully acknowledge the Fiji Ministry of Health and staff at the trauma admitting hospitals in Viti Levu for supporting and facilitating the conduct of this research. We also acknowledge the members of the TRIP project team including Professor Sitaleki Finau, Dr. Robyn McIntyre for project supervision and guidance, Asilika Naisaki, Mabel Taoi, Ravi Reddy, Ramneek Goundar, Litia Vuniduvu, for overseeing the participant interviews, data entry and cleaning; Nola Vanualaila, for developing and managing the databases.
Data Availability
Due to ethical restrictions pertaining to participant consent, data are available upon request. Individual level data are not available, due to Institutional Review Board restrictions, however aggregated data are available upon request to the Corresponding Author.
Funding Statement
This study was supported by an international collaborative research grant (grant no GRO71671AIA) awarded by the Wellcome Trust (http://www.wellcome.ac.uk/) and the Health Research Council of New Zealand (grant no 04/498) (http://www.hrc.govt.nz/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Global status report on road safety 2013: supporting a decade of action. Geneva: World Health Organization; 2013. [Google Scholar]
- 2.Ameratunga S, Hijar M, Norton R. Road-traffic injuries: confronting disparities to address a global-health problem. The Lancet. 367(9521):1533–40. 10.1016/s0140-6736(06)68654-6 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Global Plan for the Decade of Action for Road Safety 2011–2020, 2011 Nov 5 2012]. Available from: http://www.who.int/roadsafety/decade_of_action/plan/en/.
- 4.Asbridge M, Hayden JA, Cartwright JL. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:1–9. Epub 9 February 2012. 10.1136/bmj.e536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuypers KP, Legrand S-A, Ramaekers JG, Verstraete AG. A case-control study estimating accident risk for alcohol, medicines and illegal drugs. PLoS One. 2012;7(8):e43496 10.1371/journal.pone.0043496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meuleners LB, Duke J, Lee AH, Palamara P, Hildebrand J, Ng JQ. Psychoactive Medications and Crash Involvement Requiring Hospitalization for Older Drivers: A Population-Based Study. Journal of the American Geriatrics Society. 2011;59(9):1575–80. 10.1111/j.1532-5415.2011.03561.x [DOI] [PubMed] [Google Scholar]
- 7.Pickett W, Davison C, Torunian M, McFaull S, Walsh P, Thompson W. Drinking, substance use and the operation of motor vehicles by young adolescents in Canada. PLoS one. 2012;7(8):e42807 10.1371/journal.pone.0042807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh YN. Kava: an overview. Journal of Ethnopharmacology. 1992;37(1):13–45. 10.1016/0378-8741(92)90003-a [DOI] [PubMed] [Google Scholar]
- 9.Wainiqolo I, Kool B, Nosa V, Ameratunga S. Is driving under the influence of kava associated with motor vehicle crashes? A systematic review of the epidemiological literature. Australian and New Zealand journal of public health. 2015;39(5):495–9. 10.1111/1753-6405.12435 [DOI] [PubMed] [Google Scholar]
- 10.Abu N, Akhtar MN, Yeap SK, Lim KL, Ho WY, Zulfadli AJ, et al. Flavokawain A Induces Apoptosis in MCF-7 and MDA-MB231 and Inhibits the Metastatic Process In Vitro. PLoS ONE. 2014;9(10):1–12. 10.1371/journal.pone.0105244 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Currie BJ, Clough AR. Kava hepatoxicity with Western herbal products: does it occur with traditional kava use? Medical Journal of Australia. 2003;178:421–2. [DOI] [PubMed] [Google Scholar]
- 12.Li X, Liu Z, Xu X, Blair CA, Sun Z, Xie J, et al. Kava Components Down-Regulate Expression of AR and AR Splice Variants and Reduce Growth in Patient-Derived Prostate Cancer Xenografts in Mice. PLoS ONE. 2012;7(2):e31213 10.1371/journal.pone.0031213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cairney S, Maruff P, Clough AR, Collie A, Currie J, Currie BJ. Saccade and cognitive impairment associated with kava intoxication. Human Psychopharmacology: Clinical and Experimental. 2003b;18(7):525–33. 10.1002/hup.532 [DOI] [PubMed] [Google Scholar]
- 14.Fiji Statistics at a Glance [Internet]. Fiji Bureau of Statistics. 2013. Available from: http://www.statsfiji.gov.fj/.
- 15.Wensley C. Technical Assistance (financed by the Japan Special Fund) To the Republic of the Fiji Islands for preparing the Fourth Road Upgrading (Sector) Project. Asian Development Bank; 2004.
- 16.Beaglehole R, Bonita R, Kjellstrom T. Basic Epidemiology. Geneva: World Health Organization; 1993. [Google Scholar]
- 17.Roberts I. Methodologic issues in injury case-control studies. Injury Prevention. 1995;1(1):45–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wacholder S, Silverman DT, McLaughlin JK, Mandel JS. Selection of Controls in Case-Control Studies: II. Types of Controls. American Journal of Epidemiology. 1992;135(9):1029–41. [DOI] [PubMed] [Google Scholar]
- 19.Connor J, Norton R, Ameratunga S, Robinson E, Civil I, Dunn R, et al. Driver sleepiness and risk of serious injury to car occupants: population based case control study. BMJ. 2002;324(7346):1125 10.1136/bmj.324.7346.1125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Herman J, Ameratunga SN, Wainiqolo I, Kafoa B, Robinson E, McCaig E, et al. Prevalence of sleepiness while driving four-wheel motor vehicles in Fiji: a population-based survey (TRIP 9). Injury Prevention. 2013. 10.1136/injuryprev-2012-040570 [DOI] [PubMed] [Google Scholar]
- 21.Herman J, Kafoa B, Wainiqolo I, Robinson E, McCaig E, Connor J, et al. Driver sleepiness and risk of motor vehicle crash injuries: A population-based case control study in Fiji (TRIP 12). Injury. 2014;45(3):586–91. 10.1016/j.injury.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wainiqolo I, Kafoa B, McCaig E, Kool B, McIntyre R, Ameratunga S. Development and piloting of the Fiji Injury Surveillance in Hospitals System (TRIP Project-1). Injury. 2013;44(1):126–31. 10.1016/j.injury.2011.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Szumilas M. Explaining odds ratios. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2010;19(3):227 [PMC free article] [PubMed] [Google Scholar]
- 24.Greenland S. Modeling and variable selection in epidemiologic analysis. American Journal of Public Health. 1989;79(3):340–9. 10.2105/ajph.79.3.340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Coughlin SS, Benichou J, Weed DL. Attributable Risk Estimation in Case-Control Studies. Epidemiologic Reviews. 1994;16(1):51–64. [DOI] [PubMed] [Google Scholar]
- 26.LaPorte E, Sarris J, Stough C, Scholey A. Neurocognitive effects of kava (Piper methysticum): a systematic review. Human Psychopharmacology: Clinical and Experimental. 2011;26(2):102–11. 10.1002/hup.1180 [DOI] [PubMed] [Google Scholar]
- 27.Sarris J, Laporte E, Scholey A, King R, Pipingas A, Schweitzer I, et al. Does a medicinal dose of kava impair driving? A randomized, placebo-controlled, double-blind study. Traffic Injury Prevention. 2013;14(1):13–7. 10.1080/15389588.2012.682233 . [DOI] [PubMed] [Google Scholar]
- 28.Kava Tea DUI Case Puts Spotlight on Community Steeped in Tradition [Internet]. John P Puerner. 2000 [cited 7 May 2015]. Available from: http://articles.latimes.com/2000/may/07/news/mn-27475.
- 29.Man convicted for driving under the influence of kava [Internet]. New Zealand Media & Entertainment. 2007 [cited 30 June 2015]. Available from: http://www.nzherald.co.nz/nz/news/article.cfm?c_id=1&objectid=10448828.
- 30.LTA plans kava ban—Taxi bases, drivers under scrutiny [Internet]. Hank Arts. 2012 [cited 15 April 2015]. Available from: http://www.fijitimes.com/story.aspx?id=206710.
- 31.Land Transport Act 1998 [Internet]. Land Transport Authority,. 1998 [cited 21 April 2015]. Available from: http://www.ltafiji.com/aboutus_the_lta_act.php.
- 32.Cairney S, Maruff P, Clough AR. The neurobehavioural effects of kava. Australian and New Zealand Journal of Psychiatry. 2002;36(5):657–62. 10.1046/j.1440-1614.2002.01027.x [DOI] [PubMed] [Google Scholar]
- 33.Singh YN. Kava: An Old Drug in a New World. Cultural Critique [Internet]. 2009; 71:[107–28 pp.]. Available from: http://muse.jhu.edu.ezproxy.auckland.ac.nz/journals/cultural_critique/v071/71.singh.html.
- 34.Prescott J, Jamieson D, Emdur N, Duffield P. Acute effects of kava on measures of cognitive performance, physiological function and mood. Drug and Alcohol Review. 1993;12(1):49–57. 10.1080/09595239300185731 [DOI] [PubMed] [Google Scholar]
- 35.Thompson RWRU. Enhanced cognitive performance and cheerful mood by standardized extracts of Piper methysticum (Kava-kava). Human Psychopharmacology: Clinical & Experimental. 2004;19(4):243–50. . [DOI] [PubMed] [Google Scholar]
- 36.Foo H, Lemon J. Acute effects of kava, alone or in combination with alcohol, on subjective measures of impairment and intoxication and on cognitive performance. Drug and Alcohol Review. 1997;16(2):147–55. 10.1080/09595239700186441 [DOI] [PubMed] [Google Scholar]
- 37.Herberg K. Driving ability after intake of kava special extract WS 1490. Z Allgemeinmed. 1991;69:271–7. [Google Scholar]
- 38.Herberg K. The influence of Kava-specialextract WS 1490 on safety-related performance alone and in combination with ethylalcohol. Blutalkohol. 1993;30(2):96–105. [PubMed] [Google Scholar]
- 39.Cornelius M, Decourten M, Pryor J, Saketa S, Waqanivalu T, Laqeretabua A, et al. Fiji Non Communicable Disease (NCD) STEP Survey 2002. Suva: Ministry of Health, 2004. [Google Scholar]
- 40.Peden M, Scurfield R, Sleet D, Mohan D, Hyder A A, Jarawan E, et al. , editors. World report on road traffic injury prevention Geneva: World Health Organization; 2004. [Google Scholar]
- 41.Tang T-Q, Caccetta L, Wu Y-H, Huang H-J, Yang X-B. A macro model for traffic flow on road networks with varying road conditions. Journal of Advanced Transportation. 2014;48(4):304–17. 10.1002/atr.215 [DOI] [Google Scholar]
- 42.Nagatani T, Yonekura S. Multiple-vehicle collision induced by lane changing in traffic flow. Physica A: Statistical Mechanics and its Applications. 2014;404:171–9. 10.1016/j.physa.2014.02.028 [DOI] [Google Scholar]
- 43.Rothman KJ, Greenland S. Modern Epidemiology. Philadelphia: Lipincott Williams & Wilkins; 1998. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
Data Availability Statement
Due to ethical restrictions pertaining to participant consent, data are available upon request. Individual level data are not available, due to Institutional Review Board restrictions, however aggregated data are available upon request to the Corresponding Author.