Abstract
Group sex events are epidemiologically important part of some gay and bisexual men's sexual culture in Canada. Associated with condomless anal intercourse and polysubstance use, such events have been cited as disproportionally contributing to HIV infection rates. We analysed questionnaire data from the Momentum Health Study in Vancouver, Canada to understand substance use, sexual behaviour, psychosocial variables (Sexual Sensation Seeking, Sexual Escape Motivation, and Treatment Optimism), and HIV prevention strategies (sero-sorting, strategic positioning, avoiding anal sex, disclosure, treatment as prevention) of men attending such events, which were defined as group (n≥4 partners) sex parties, blackout events, and darkrooms. Analysis by multivariable logistic regression compared men attending group sex events within the past 6 months (n=180) with non-attendees (n=539). Results showed that attendees reported 1) significantly higher use of sex drugs and alcohol consumption, 2) higher scores on the Sexual Sensation Scale, more anal sex partners, greater odds of any condomless anal sex with sero-discordant partners, and greater odds of reporting fisting and sex toy use, and 3) different prevention practices that varied by HIV-serostatus. Findings are interpreted in light of the importance of pleasure, sociality, and HIV/STI prevention strategies associated with group sex events. Findings contribute to the development of appropriate education and intervention for attendees.
Keywords: gay and bisexual men, group sex events, substance use, prevention strategies, Canada
Introduction
Group sex events are epidemiologically important phenomena in heterosexual and gay and bisexual men's sexual cultures (Friedman, Mateau-Gelabert, and Sandoval 2011). In the latter context, they range from circuit parties (Weidel, Provencio-Vasquez, and Grossman 2008) attended by thousands of men to private POZ Parties restricted to HIV-positive men (Clatts, Goldsamt, and Yi 2005). Common factors reported for gay and bisexual men's group sex events include condomless anal sex and polysubstance use (Ghaziani and Cook 2005; Hurley and Prestage 2007, 2009; Adam et al. 2008; Mimiaga et al. 2010, 2011; Grov 2012; Grov, Cruz, and Parsons 2014; Phillips et al. 2013), and community samples show that up to 25% of gay and bisexual men met their recent sexual partners at such events (Grov, Parsons, and Bimbi 2007; Mimiaga et al. 2010). Because of these factors, group sex events are cited as disproportionally contributing to HIV infection rates (Kurtz 2009; Prestage, Grierson et al. 2009; Prestage, Hudson et al. 2009; O'Bryne and Holmes 2011), generating calls for HIV/STI education/intervention programmes specifically designed for gay and bisexual men attending group sex events (Mimiaga et al. 2011; Phillips et al. 2013). In an attempt to meet this call we compared the sexual behaviour, substance use patterns, psychosocial factors, and prevention strategies of recent group sex event attendees with non-attendees enrolled in the Momentum Health Study, a longitudinal study of gay and bisexual men in Metro Vancouver, British Columbia, Canada.
Previous research in North America and Australia posits the existence of distinct gay sub-populations associated with group sex events that feature distinctive patterns. In North America, this group has been referred to as a ‘fast lane’ sub-culture (Kurtz 2009), while in Australia two similar, related sub-cultures are called ‘sexual adventurism’ (Kippax et al. 1998; Smith, Worth, and Kippax 2004) and ‘intensive sex partying’ (Hurley and Prestage 2007, 2009). Sexual adventurism refers to gay and bisexual men who prefer group sex, rimming, sex toys, fisting and/or other more esoteric sexual practices. Intensive sex partying is interpreted as an attempt to maximise sexual pleasure by combining sociality and polysubstance use at group sex events. Equally important, there is global evidence that group sex event attendees practice prevention strategies to protect themselves and their partners from HIV/STI infection. Examples from gay and bisexual men's group sex events include on-site prevention aids in the form of condoms, lubricants, and coupons for easy access to no-cost STI testing (Mimiaga et al. 2010).
Given the above, this study attempts to describe recent group sex event attendees by testing three specific hypotheses: 1) Recent group sex event attendees feature higher levels of substance use, including recreational substance use, e.g. alcohol, marijuana, cocaine, ketamine, gamma-hydroxybutyrate, Ecstasy, and particularly sex drugs, crystal methamphetamine, erectile dysfunction drugs and amyl nitrates (poppers) than non-attendees; 2) Recent group sex event attendees feature higher levels of sexual adventurism, measured by number of sex partners, condomless anal sex with sero-discordant and/or unknown serostatus partners, fisting, rimming, and sex toy use, than non-attendees; and 3) Recent group sex event attendees practice emic harm reduction tactics, distinctive from non-attendees.
Methods
To test these hypotheses, we analysed survey data collected by the Momentum Health Study, a longitudinal study designed to identify the concomitants of British Columbia's initiatives to dramatically expand HIV testing and treatment. The province has provided antiretroviral therapy at no cost to all HIV-positive residents of British Columbia (Montaner et al. 2006, 2010, 2014; Lima et al. 2015) since 1992, and beginning in 2010 has directed additional funding to support a more active approach to HIV diagnosis and engaging HIV-positive individuals in care and treatment. Momentum uses respondent driven sampling (Heckathorn 1997) as a recruitment strategy, an approach developed to recruit participants from hard-to-reach or ‘hidden’ populations (i.e., those for whom probability-based sampling is challenging). Respondent driven sampling is based on the concept of homophily, which states that, “contact between similar people occurs at a higher rate than among dissimilar people”, (McPherson, Smith-Lovin, and Cook 2001, 416) and begins by recruiting ‘seeds’ who share key characteristics, e.g. sexual orientation, substance use, etc., with members of a target population. Seeds give vouchers to people sharing social/sexual networks and in turn these ‘respondents’ recruit other members in a modified snowball or long-chain sampling approach.
As discussed fully in Forrest et al. (2014), Momentum recruited multiple seeds who each distributed paper and/or electronic vouchers to men meeting the study eligibility criteria: 16 years and older, identifying as a man, having had sex with other men in the six months prior to baseline study visit, living in Metro Vancouver, and able to understand and complete a questionnaire written in English. Eligible men completed a computer-assisted self-interview questionnaire and biological tests including a point of care HIV test, blood tests for hepatitis C and syphilis serology, and optional tests for gonorrhoea and chlamydia. Participants received an honorarium of fifty Canadian dollars, were given a maximum of six vouchers to recruit other participants, and earned ten Canadian dollars for each additional eligible recruited respondent who completed the survey and biological tests. All study procedures received human ethics clearance from Simon Fraser University, the University of British Columbia, and the University of Victoria.
One questionnaire section focused on three related group sex events, all defined as having four or more participants to exclude sexual threesomes and emphasise the social importance of group sex events. These were: 1) group sex parties – defined as spontaneous or planned events in which four or more people get together to have sex in either public or private settings, 2) darkrooms – a place in a bar, club or bathhouse where men can have anonymous sex, and 3) blackout events – usually held in sex-on-premises venues like a bathhouse, these feature dimmed or extinguished lighting to facilitate anonymous sex. Sexual behaviour, substance use, and prevention strategies formed independent variables for three separate logistic regression models (Allison 2012), each with attendance (yes vs. no) at one or more of the group sex events specified above within the past six months as the dependent categorical variable. These models are described below.
Model I: Substance use
This model's independent variables included responses to whether the participant used alcohol, erectile dysfunction drugs, poppers, crystal methamphetamine, Ecstasy/ MDMA, gamma-hydroxybutyrate, and/or ketamine in the past six months. Previous research indicated linkages between some substances and specific sexual behaviour. For example, erectile dysfunction drugs are associated with insertive anal sex (Mansergh et al. 2006), while poppers facilitate receptive anal intercourse because of their smooth muscle relaxant properties (Plankey et al. 2007). In addition, reports that crystal methamphetamine greatly enhances sexual pleasure but reduces erectile functioning suggests that it is often taken in combination with erectile dysfunction drugs or poppers (Fisher et al. 2011). Recognising these patterns we performed interactions for: 1) crystal methamphetamine X erectile dysfunction drugs and 2) crystal methamphetamine X poppers. Finally, because a recent meta-analysis of event-level data showed that binge drinking (>5 drinks per one sitting) was significantly associated with high risk sexual behaviour among gay and bisexual men (Vosbergh et al. 2012), the Alcohol Use Disorders Identification Test (Saunders et al. 1993) was included as an independent variable.
Model II: Sexual behaviour and psychosocial scales
Independent variables for this model included measures of sexual adventurism represented by participants engaging in fisting, using sex toys, rimming, number of anal sex partners, and high risk sex, defined here as unprotected anal sex with sero-discordant or unknown sero-status partners in the past six months. In addition, this model included potential psychosocial mediators in the form of three validated scales: 1) the McKiran et al. (2001) Sexual Escape Scale (12 questions, Cronbach's study α = 0.90), 2) Kalichman et al. (1994) Sensation Seeking Scale (Revised) (11 questions, study α = 0.73), and 3) a Treatment Optimism Scale, adapted from Van de Ven et al. 2000 (12 questions, study α = 0.85).
Model III: Prevention tactics
The final model attempted to delineate group sex events attendees’ emic prevention tactics, exemplified in the Momentum questionnaire by HIV disclosure, condom use, strategic positioning (e.g., HIV-positive partners assumes receptive sexual position during anal sex), sero-sorting (e.g., only have condomless anal sex with partners of same HIV status), withdrawal, avoiding anal intercourse and knowledge regarding their partners’ HIV viral load and treatment status by response to the question, “Some guys use strategies to prevent getting HIV. Do you do any of the following to prevent getting HIV?”
The first two models included self-reported HIV status (HIV-positive, HIV-negative, and unknown) and age. For the third model, separate runs were made for HIV-positive and HIV-negative/unknown status men since prevention strategies were expected to differ by sero-status. Univariable and multivariable models used the SAS (Version 9.3) PROC LOGISTIC sub-routine, which generated point estimates, unadjusted and adjusted odds ratios and 95% confidence intervals. Final multivariable models were determined using a backward elimination procedure based on the Akaike Information Criterion and Type-III p values (Lima et al. 2007). A central premise of respondent driven sampling is that the overall respondents’ social network size can be used to estimate sampling probabilities and generate population estimates (Heckathorn 2002). Accordingly, the sample's basic socio-demographic data are adjusted by the respondent-driven sampling program RDSAT version 7.1 (Volz et al. 2012) using respondents’ social network size estimates and each corresponding variable to generate point estimates and 95% confidence intervals of the population parameters for this information.
Results
Sample characteristics
From February 2012 to February 2014 Momentum recruited 719 gay and bisexual men, of whom 119 were recruited directly as seeds. Table 1 depicts sample characteristics, giving crude and respondent driven sampling-adjusted values for participants’ HIV status, age, sexual orientation, ethnicity, income, and education. Overall, the raw values are close to the respondent driven sampling-adjusted figures, with only a few crude measures falling outside the generated 95% confidence intervals. Notable exceptions include crude measures showing participants with annual incomes less than $20,000 Canadian dollars, and those having no more than a high school education falling below the lower confidence interval limits.
Table 1.
Demographics and descriptive statistics of substance use, sexual behaviour, psychosocial factors, and sero-adaptive strategies for the full Momentum Health Study cross-sectional sample (n = 719)
| n | %(95% CI) or median(IQR) | |
|---|---|---|
| Age (n=719) (continuous) | 33(26, 47) | |
| Sexual Orientation (n=719) | ||
| Gay | 612 | 80.7(76.3, 85.2) |
| Bisexual | 66 | 15.3(10.6, 19.5) |
| Other | 41 | 4.0(2.4, 6.1) |
| Ethnicity (n=719) | ||
| White | 539 | 68.0(61.0, 74.2) |
| Asian | 72 | 9.8(6.3, 14.9) |
| Aboriginal | 50 | 10.3(5.5, 15.9) |
| Other | 58 | 11.9(7.1, 17.3) |
| Annual Income (n=719) | ||
| <$20,000 | 328 | 52.5(46.4, 59.2) |
| >=$20,000 | 391 | 47.5(40.8, 53.6) |
| Post-Secondary Education (n=705) | ||
| Did not complete | 291 | 52.2(45.6, 59.7) |
| Completed | 414 | 47.8(40.3, 54.4) |
| HIV Testing (n=524)* | ||
| Not in the past 2 years | 89 | 21.1(15.9, 28.8) |
| Yes in the past 2 years | 435 | 78.9(71.2,84.1) |
| HIV Status (self-report) (n=719) | ||
| Negative | 467 | 68.6(61.1, 75.5) |
| Positive | 195 | 22.2(14.3, 30.0) |
| Unknown | 57 | 9.2(6.5, 12.9) |
| AUDIT (n=714) | ||
| Non/Social drinker | 373 | 54.6(48.4, 61.4) |
| Harmful/Hazardous | 234 | 30.5(25.3, 36.5) |
| Alcohol dependent | 107 | 14.9(9.9, 19.7) |
| Substances Used in P6M (n=719) | ||
| EDD | 162 | 17.3(12.5, 22.1) |
| Crystal meth | 136 | 19.6(13.7, 25.7) |
| Poppers | 266 | 34.3(28.5, 40.3) |
| Ecstasy | 176 | 18.9(14.2, 24.2) |
| Ketamine | 94 | 12(7.8, 16.3) |
| Gamma-hydroxybutyrate | 126 | 19.1(13.4, 24.1) |
| Psychosocial Scales (continuous) | ||
| Treatment Optimism (n=716) | 25(21, 28) | |
| Sexual Sensation Seeking (n=698) | 31(28, 34) | |
| Escape Motive (n=705) | 29(25, 33) | |
| Male Sex Partners in P6M (n=719) | ||
| Less than 5 | 314 | 50.4(44.2, 57.1) |
| 5 or more | 405 | 49.6(42.9, 55.8) |
| Sexual Behaviours in P6M (n=716) | ||
| Insertive anal sex | 512 | 65.2(58.8, 71.4) |
| Receptive anal sex | 484 | 63.9(57.7, 69.7) |
| Rimming | 436 | 49.1(41.9, 55.2) |
| Used sex toys | 199 | 24.7(19.5, 29.9) |
| Fisting | 73 | 7.1(4.6, 9.9) |
| Risky Sex (n=703) | ||
| No | 441 | 64.1(58.2, 70.6) |
| Yes | 262 | 35.9(29.4, 41.8) |
| Anal Sex Preference (n=687) | ||
| Bottom | 241 | 36.0(29.6, 41.4) |
| Versatile | 193 | 27.6(22.2, 33.3) |
| Top | 253 | 36.4(31.4, 42.5) |
| Sero-adaptive Strategies Used (n=715) | ||
| Always using condoms | 403 | 57.3(50.6, 63.5) |
| Being the top for anal sex | 209 | 23.6(19.0, 28.6) |
| Not having anal sex | 325 | 37.7(33.0, 44.8) |
| If HIV−, condomless sex only with HIV− men (n=520) | 182 | 30.3(22.8, 36.7) |
| If HIV+, condomless sex only with HIV+ men (n=195) | 102 | 46.4(32.4, 61.1) |
| Condomless sex only with HIV+ men with low viral load / on HIV treatment | 119 | 12.8(9.4, 17.8) |
| Withdrawal | 202 | 24.3(19.1, 29.3) |
| Asking partner's their HIV serostatus before sex | 421 | 50.5(43.6, 56.6) |
| Assumption of anal sex partner's HIV status if not disclosed (n=716) | ||
| Assume positive | 195 | 30.4(23.5, 36.7) |
| Assume negative | 175 | 22.8(18.3, 28.1) |
| Look for other signs | 65 | 8.1(5.3, 11.6) |
| Make no assumptions | 281 | 38.7(32.9, 44.5) |
| Seek HIV concordant partners to avoid using condoms | ||
| If HIV−, seek HIV− partners (n=509) | 139 | 31.6(24.2, 38.0) |
| If HIV+, seek HIV+ partners (n=191) | 108 | 52.2(36.9, 67.0) |
95% CI = 95% Confidence Interval, IQR = interquartile range, OR = odds ratio, AOR = adjusted odds ratio, P6M = past six months, EDD = erectile dysfunction drugs
NB: All statistics are RDS-adjusted (except raw sample size, n)
N/A for self-reported HIV+ participants
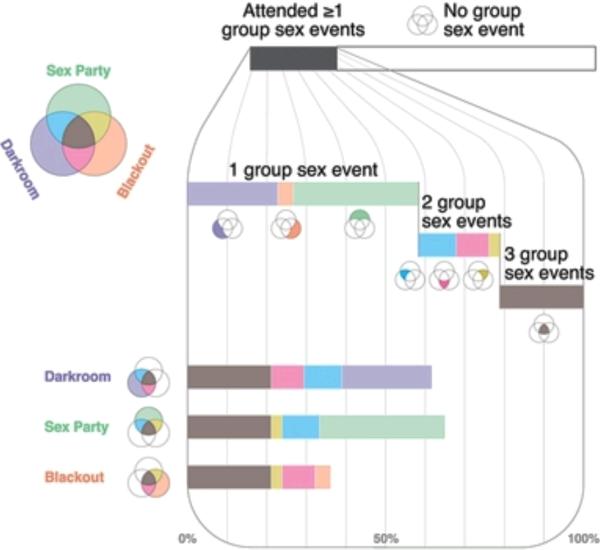
Table 2 presents the raw values for men attending specific group sex event venues and their reported sexual behaviour there. Altogether 180 men, or 21.4% (95% Confidence Interval [CI]: 15.9%-26.5%) of the total sample, reported attending at least one group sex event in the past six months. In terms of type of group sex event, more participants attended group sex parties (n=117), followed closely by darkrooms (n=111) and blackout events (n=65). Figure 1 shows group sex event attendance by type of event for the sample. Since men could attend more than one type of group sex event, the data are interdependent and we did not test for significant differences between specific events.
Table 2.
Type of group sex event attendance and distribution of sexual behaviour of Momentum respondents who attended group sex parties in past six months (n=180).
| Sex Party n=117 | Blackout Event n=65 | Darkroom n=111 | |
|---|---|---|---|
| n(%) | n(%) | n(%) | |
| No sex | 4(3%) | 4 (6%) | 6 (5%) |
| Fondled touched | 64(55%) | 36 (55%) | 57 (51%) |
| Oral sex | 86(74%) | 48 (74%) | 79 (71%) |
| Anal sex (any top) | 68(58%) | 31 (48%) | 39 (35%) |
| Anal sex (any bottom) | 58(50%) | 32 (49%) | 49 (44%) |
| Anal sex (only top) | 28(24%) | 14 (22%) | 19 (17%) |
| Anal sex (both top and bottom) | 40(34%) | 17 (26%) | 20 (18%) |
| Anal sex (only bottom) | 18(15%) | 15 (23%) | 29 (26%) |
Figure 1.
Group sex event types and attendance
Model I: Substance use
As shown in Table 3, all substances considered were positively statistically associated with group sex event attendance in the univariable analysis, and erectile dysfunction drugs, poppers, and the Alcohol Dependent classification (scores >= 20) for the Alcohol Use Disorders Identification Test Scale remained significant in the final multivariable analysis. Interaction analyses performed on: 1) erectile dysfunction drugs and crystal methamphetamine and 2) poppers and crystal methamphetamine showed that only was former was statistically significant. The impact of erectile dysfunction drug use and group sex event attendance depends on the level of crystal methamphetamine use. When crystal is not used the odds of using both erectile dysfunction drugs and attending group sex events are 2.86 times (95% CI: 1.66, 4.92) that of not using erectile dysfunction drugs for men attending group sex events. However, for men using crystal, the odds of using erectile dysfunction drugs and attending group sex events are 12.35 (95% CI: 4.70, 32.47) times that of not using erectile dysfunction drugs for men attending group sex events. Taken together, these results strongly support our first hypothesis that group sex event attendees feature greater substance use, particularly sex drugs, than non-attendees.
Table 3.
Frequency of substance use by and association with having sex at a group sex event (GSE) in the six months prior to survey
| No sex at GSE | Yes, had sex at GSE | Univariate OR | Multivariate AOR | |||
|---|---|---|---|---|---|---|
| n | %(95% CI) or median(IQR) | n | %(95% CI) or median(IQR) | (95% CI) | (95% CI) | |
| Age (n=719) | 33(25, 46) | 34(27, 49) | 1.01(0.99, 1.02) | Not selected | ||
| HIV Status (n=719) | ||||||
| Negative | 359 | 65.1(59.4, 70.9) | 108 | 65.0(54.2, 75.8) | Referent | Not selected |
| Positive | 129 | 25.7(20.2, 31.2) | 66 | 32.2(21.7, 42.8) | 1.26(0.85, 1.85) | |
| Unknown | 51 | 9.2(6.3, 12.2) | 6 | 2.8(0.0, 6.2) | 0.30(0.11, 0.83) | |
| AUDIT (n=714) | ||||||
| Non/Social drinker | 276 | 52.8(46.8, 58.8) | 97 | 55.3(43.9, 66.7) | Referent | Referent |
| Harmful/Hazardous | 187 | 33.8(28.3, 39.4) | 47 | 22.4(13.1, 31.7) | 0.63(0.41, 0.98) | 0.80(0.49, 1.31) |
| Alcohol dependent | 72 | 13.4(9.2, 17.5) | 35 | 22.3(12.4, 32.2) | 1.59(0.99, 2.55) | 2.39(1.40, 4.08) |
| Substances Used in P6M (n=719)* | ||||||
| EDD | 82 | 11.8(8.5, 15.2) | 80 | 43.0(31.6, 54.4) | 5.62(3.73, 8.47) | 2.86(1.66, 4.92) |
| Crystal meth | 76 | 14.6(10.1, 19.2) | 60 | 29.4(19, 39.8) | 2.42(1.59, 3.69) | 0.66(0.31, 1.41) |
| Interaction: EDD & Crystal Meth | -- | 4.32(1.44, 12.94) | ||||
| -- | 12.35(4.70, 32.47) | |||||
| -- | 2.85(1.28, 6.33) | |||||
| Poppers | 161 | 25.5(20.6, 30.6) | 105 | 63.1(52.5, 73.8) | 5.01(3.43, 7.33) | 3.76(2.49, 5.70) |
| Ecstasy | 116 | 18.2(13.9, 22.6) | 60 | 30.8(20.4, 41.2) | 2.00(1.33, 3.00) | Not selected |
| Ketamine | 56 | 10.0(6.5, 13.6) | 38 | 19.3(9.7, 28.9) | 2.15(1.32, 3.50) | Not selected |
| Gamma-hydroxybutyrate | 66 | 13.6(9.2, 18.0) | 60 | 31.6(20.7, 42.6) | 2.95(1.94, 4.49) | Not selected |
95% CI = 95% Confidence Interval, IQR = interquartile range, OR = odds ratio, AOR = adjusted odds ratio, P6M = past six months, EDD = erectile dysfunction drugs
referent is not having used that specific substance
NB: All statistics are RDS-adjusted (except raw sample size, n)
Model II: Sexual behaviour and psychosocial scales
As shown in Table 4, all sexual behaviours previously cited as representing sexual adventurism (Smith et al. 2004) were significant in the univariable model, as were the three psychosocial scales. In the final multivariable analysis recent group sex event attendees featured significantly more (>5 vs. ≤5) anal sex partners in the past six months, were more likely to have high-risk sex (defined as unprotected anal sex with a sero-discordant or unknown sero-status partner), to report fisting and sex toy use, and score higher on the Sexual Sensation Seeking Scale. These results support our second hypothesis, that Momentum participants who attended group sex events in the past six months feature significantly higher levels of sexual adventurism relative to non-attendees.
Table 4.
Sexual behaviour and psychosocial factors associated with having sex at a group sex event (GSE) in the six months prior to survey
| No sex at GSE | Yes, had sex at GSE | Univariate OR | Multivariate AOR | |||
|---|---|---|---|---|---|---|
| n | %(95% CI) or median(IQR) | n | %(95% CI) or median(IQR) | (95% CI) | (95% CI) | |
| Age (n=719) | 33(25, 46) | 34(27, 49) | 1.01(0.99, 1.02) | Not selected | ||
| HIV Status (n=719) | ||||||
| Negative | 359 | 65.1(59.4, 70.9) | 108 | 65(54.2, 75.8) | Referent | Not selected |
| Positive | 129 | 25.7(20.2, 31.2) | 66 | 32.2(21.7, 42.8) | 1.25(0.85, 1.85) | |
| Unknown | 51 | 9.2(6.3, 12.2) | 6 | 2.8(0.0, 6.2) | 0.30(0.11, 0.83) | |
| Psychosocial Scales (continuous) | ||||||
| Treatment Optimism (n=716) | 24(21, 27) | 26(22, 30) | 1.05(1.02, 1.09) | Not selected | ||
| Sexual Sensation Seeking (n=698) | 30(27, 33) | 32(30, 35) | 1.15(1.10, 1.20) | 1.10(1.04, 1.15) | ||
| Escape Motive (n=705) | 28(24, 32) | 30(26, 35) | 1.05(1.02, 1.07) | Not selected | ||
| Male Anal Sex Partners in P6M (n=719) | ||||||
| Less than 5 | 288 | 57.5(51.6, 63.3) | 26 | 16.5(7.9, 25.2) | Referent | Referent |
| 5 or more | 251 | 42.5(36.7, 48.4) | 154 | 83.5(74.8, 92.1) | 6.81(4.30, 10.79) | 4.64(2.84, 7.59) |
| Sexual Behaviours in P6M (n=716)* | ||||||
| Rimming | 293 | 46.4(40.5, 52.3) | 143 | 76.1(66.6, 85.6) | 3.68(2.44, 5.53) | Not selected |
| Used sex toys | 116 | 18.9(14.6, 23.2) | 83 | 44.0(32.5, 55.5) | 3.36(2.29, 4.93) | 2.49(1.59, 3.89) |
| Fisting | 34 | 4.2(2.5, 6.0) | 39 | 18.6(10.2, 27.1) | 5.717(2.9090, 9.2222) | 2.929(1.717, 4.949) |
| Risky Sex (n=703) | ||||||
| No | 371 | 72.8(67.6, 78.2) | 70 | 38.9(27.6, 50.1) | Referent | Referent |
| Yes | 154 | 27.2(21.8, 32.5) | 108 | 61.1(49.9, 72.4) | 4.22(2.89, 6.17) | 2.35(1.52, 3.64) |
95% CI = 95% Confidence Interval, IQR = interquartile range, OR = odds ratio, AOR = adjusted odds ratio, P6M = past six months
referent is not having done that specific sexual behaviour
NB: All statistics are RDS-adjusted (except raw sample size, n)
Model III: Prevention strategies
The third model aimed to delineate prevention strategies among recent group sex event attendees stratified by self-reported HIV status. For HIV-negative participants, Table 5a shows that sero-sorting, represented by favouring condomless anal sex only with other HIV-negative men is inversely associated with group sex events, indicating lower use of this sero-adaptive strategy among group sex event attendees compared with non-attendees. However, HIV-negative group sex event attendees were almost five times more likely to favour condomless anal sex with HIV-positive men on HIV treatment and/or assumed to have low viral loads compared with non-attendees. In addition, the HIV-negative sample who attended group sex events had one positively significant strategy for anal sex partners who do not disclose their status; that is, these men were more likely to look for other signs of his HIV status (e.g.: a biohazard or ‘+’ tattoo, or signs of HIV disease, or HIV medication bottles) than assume their anal sex partner was HIV-positive if they hadn't disclosed any status. In contrast, Table 5b shows that sero-sorting for HIV-positive men, represented by condomless anal sex only with HIV-positive men, was positively associated in the multivariable model. Finally, while neither treatment adherence nor most recent viral load measurements were significant variables in both the univariable and multivariable models, HIV-positive men who were diagnosed 13-19 years previously were significantly less likely to attend group sex events in the past 6 months.
Table 5a.
Frequency of sero-adaptive strategies by and association with having sex at a group sex event (GSE) in the six months prior to survey for HIV-negative participants (n=520)
| No sex at GSE | Yes, had sex at GSE | Univariate OR | Multivariate AOR | |||
|---|---|---|---|---|---|---|
| n | %(95% CI) | n | %(95% CI) | (95% CI) | (95% CI) | |
| Age (n=719) | 33(25, 46) | 34(27, 49) | 1.01(0.99, 1.02) | Not selected | ||
| Sero-adaptive strategies used (n=520)* | ||||||
| Always using condoms | 275 | 69.1(63.0, 75.2) | 60 | 54.7(40.9, 68.5) | 0.54(0.35, 0.84) | Not selected |
| Being the top for anal sex | 99 | 21.2(16.1, 26.3) | 39 | 28.7(17.8, 39.6) | 1.50(0.92, 2.44) | Not selected |
| Not having anal sex | 200 | 42.4(35.9, 48.8) | 58 | 43.8(30.3, 57.2) | 1.06(0.68, 1.64) | Not selected |
| Only have condomless sex with HIV− men | 147 | 32.7(26.7, 38.8) | 35 | 22.4(13.2, 31.5) | 0.59(0.36, 0.99) | 0.53(0.31, 0.91) |
| Only have condomless sex with HIV+ men with low viral load / on HIV treatment | 24 | 5.2(2.1, 8.3) | 27 | 19.7(10.2, 29.2) | 4.49(2.36, 8.54) | 4.92(2.49, 9.74) |
| Withdrawal | 104 | 22.2(16.6, 27.7) | 42 | 28.3(17.8, 38.7) | 1.38(0.85, 2.28) | Not selected |
| Ask partner their HIV serostatus before sex | 260 | 59.8(53.0, 66.5) | 66 | 58.9(45.0, 72.7) | 0.96(0.62, 1.50) | Not selected |
| Assumption of anal sex partner's HIV status if not disclosed (n=521) | ||||||
| Assume positive | 74 | 21.4(15.3, 27.6) | 27 | 24.4(12.7, 36.2) | Referent | Referent |
| Assume negative | 142 | 32.0(25.9, 38.0) | 24 | 18.5(7.9, 29.2) | 0.51(0.27, 0.98) | 0.68(0.34, 1.35) |
| Look for other signs | 33 | 6.6(3.7, 9.5) | 16 | 18.6(5.7, 31.4) | 2.45(1.19, 5.07) | 3.10(1.45, 6.67) |
| Make no assumptions | 158 | 40.0(33.3, 46.6) | 47 | 38.5(25.3, 51.7) | 0.84(0.48, 1.48) | 1.05(0.58, 1.90) |
| Seek HIV− partners to avoid using condoms (n=509) | ||||||
| No | 287 | 68.9(62.4, 75.3) | 83 | 73.8(61.3, 86.3) | Referent | Not selected |
| Yes | 112 | 31.1(24.7, 37.6) | 27 | 26.2(13.7, 38.7) | 0.78(0.48, 1.29) | |
OR = odds ratio, AOR = adjusted odds ratio, 95% CI = 95% Confidence Interval, P6M = past six months
referent is not having done that specific sexual behaviour
NB: All statistics are RDS-adjusted (except raw sample size, n)
Table 5b.
Frequency of sero-adaptive strategies by and association with having sex at a group sex event (GSE) in the six months prior to survey for HIV-positive participants (n=195)
| No sex at GSE | Yes, had sex at GSE | Univariate OR | Multivariate AOR | |||
|---|---|---|---|---|---|---|
| n | %(95% CI) | n | %(95% CI) | (95% CI) | (95% CI) | |
| Sero-adaptive strategies used (n=195)* | ||||||
| Always using condoms | 52 | 37.7(25.1, 50.2) | 16 | 22(7.9, 36.1) | 0.47(0.21, 1.05) | Not selected |
| Being the bottom for anal sex | 43 | 26.8(16.4, 37.2) | 28 | 49(28.7, 69.2) | 2.62(1.27, 5.38) | Not selected |
| Not having anal sex | 38 | 37.1(24.1, 50.2) | 29 | 41.2(22.5, 59.9) | 1.19(0.58, 2.41) | Not selected |
| Only have condomless sex with HIV+ men | 62 | 38.9(27.2, 50.7) | 40 | 70.5(54.8, 86.3) | 3.76(1.77, 7.96) | 3.20(1.37, 7.44) |
| Only have condomless sex with men if ‘my viral load is low or I'm on HIV treatment’ | 35 | 24.4(14.2, 34.7) | 33 | 49.7(29.6, 69.9) | 3.06(1.48, 6.34) | 2.19(0.93, 5.14) |
| Withdrawal | 30 | 24.5(14.2, 34.8) | 26 | 40.5(20.1, 60.9) | 2.10(1.00, 4.38) | Not selected |
| Ask partner their HIV serostatus before sex | 58 | 35.7(24.3, 47.1) | 37 | 41.9(23.5, 60.3) | 1.30(0.64, 2.65) | Not selected |
| Assumption of anal sex partner's HIV status if not disclosed (n=195) | ||||||
| Assume positive | 60 | 52.4(39.8, 65.0) | 34 | 52.2(32.0, 72.4) | Referent | Not selected |
| Assume negative | 8 | 6.5(1.4, 11.5) | 1 | 1.8(0.0, 5.3) | 0.27(0.02, 3.04) | |
| Look for other signs | 9 | 5.4(1.6, 9.2) | 7 | 5.9(0.0, 11.8) | 1.10(0.24, 5.08) | |
| Make no assumptions | 52 | 35.8(24.0, 47.5) | 24 | 40.2(20.0, 60.3) | 1.13(0.54, 2.36) | |
| Seek HIV+ partners to avoid using condoms (n=191) | ||||||
| No | 6060 | 53.5(40.6, 66.4) | 23 | 47.8(27.3, 68.4) | Referent | Not selected |
| Yes | 6565 | 46.5(33.6, 59.4) | 43 | 52.2(31.6, 72.7) | 1.26(0.62, 2.53) | |
| Number of years since HIV diagnosis (n=130) | ||||||
| 0-5 | 17 | 19.8(9.1, 30.4) | 13 | 25.4(7.4, 43.5) | Referent | |
| 6-12 | 13 | 12.2(4.2, 20.3) | 19 | 31.4(12.7, 50.0) | 1.99(0.57, 6.90) | 1.21(0.30, 4.93) |
| 13-19 | 26 | 34.4(19.0, 49.8) | 8 | 18.5(2.5, 34.6) | 0.42(0.12, 1.44) | 0.23(0.05, 0.99) |
| 20+ | 26 | 33.6(18.0, 49.2) | 8 | 24.7(0.6, 48.8) | 0.57(0.18, 1.85) | 0.26(0.06, 1.17) |
| On treatment (adherence >95%) (n=177) | ||||||
| No | 31 | 25.1(14.1, 36.0) | 22 | 30.4(13.3, 47.6) | Referent | Not selected |
| Yes | 88 | 74.9(64.0, 85.9) | 36 | 69.6(52.4, 86.7) | 0.77(0.34, 1.70) | |
| Most recent viral load (n=195) | ||||||
| < 50 | 91 | 69.4(57.2, 81.5) | 45 | 74.0(55.1, 93.0) | Referent | Not selected |
| 50-200 | 17 | 12.1(3.7, 20.4) | 10 | 18.0(0.0, 37.1) | 1.40(0.54, 3.67) | |
| 200+ | 21 | 18.6(7.9, 29.2) | 11 | 7.9(1.9, 14.0) | 0.40(0.12,1.34) | |
OR = odds ratio, AOR = adjusted odds ratio, 95% CI = 95% Confidence Interval, P6M = past six months
referent is not having done that specific sexual behaviour
NB: All statistics are RDS-adjusted (except raw sample size, n)
Discussion
This paper used data from the Momentum Health Study to answer the question: what are the characteristics of gay and bisexual men who go to group sex events? This question is important, because it may help develop and target appropriate educational and intervention programmes for group sex event attendees, whether first time or repeat participants. Multivariable analyses supported our three hypotheses that recent gay and bisexual men group sex event attendees (21.4% of all gay and bisexual men) were significantly more likely to: 1) engage in substance use, particularly sex drugs, e.g. erectile dysfunction drugs, poppers and crystal methamphetamine, 2) be sexual adventurous, as denoted by a higher score on the Sexual Sensation Seeking Scale, have higher number of anal sex partners, engage in condomless anal sex with sero-discordant or unknown status partners, and practice fisting, and sex toy use, and 3) feature distinctive prevention strategies based on self-reported HIV status.
Results from the first two models regarding substance use and sexual adventurism are not truly surprising, since going to group sex events in itself may be sexually adventurous, and group sex event attendees are almost by definition engaging in intensive sex partying. The real value of these terms is that they provide a set of associated behaviours that allowed us to make specific hypotheses. Going beyond these somewhat tautological terms, we interpret the results of the first two models as depicting group sex event attendees attempting to maximise pleasure, a quality often neglected when studying sexual behaviour and/or substance use (Westshaver 2006; Holt and Treloar 2008; Lorvick et al. 2012). Recognising this emphasis on pleasure maximisation for group sex event attendees must be a central plank of any future educational and/or intervention programme, as it affects what prevention strategies would be accepted and practised by group sex event attendees. Certainly, higher Sexual Sensation Seeking scores and sex drug use for group sex event attendees suggests that a specialised set of prevention strategies practiced within group sex events and accepted by attendees needs to be identified.
The third model showed that prevention strategies differed for HIV-positive and HIV-negative men who attended group sex events. HIV-positive men took up established practices of withdrawal and sero-sorting (irrespective of their treatment and viral load status), consistent with findings from a decade earlier for Montreal HIV-positive men in which sero-status rather than treatment beliefs was considered more important in risk perception and negotiation (Cox, Beauchemin, and Allard 2004). HIV-negative attendees practised newer behaviours based on Treatment as Prevention measures, including information on their partners’ antiretroviral therapy use and viral loads. HIV-positive men attending group sex events were more likely to only have condomless sex with men if “my viral load is low or I'm on HIV treatment” and viral suppression appeared to be higher among this group. There were also a higher proportion of HIV-positive men in the group sex event attending group. These findings highlight the importance of understanding the context of group sex events as sero-specific or not, in order to appropriately tailor educational and intervention programmes. These findings may also indicate the diffusion of British Columbia's current Treatment as Prevention strategy amongst group sex event attendees, which is particularly important for scale up and messaging of this program.
Group sex event attendees were also less likely to assume the status of an undisclosed partner to be negative, though this was not statistically significant, and there were a smaller proportion of men with ‘unknown’ HIV serostatus among group sex event attendees. These findings suggest that for group sex event attending gay and bisexual men, serostatus may be evolving into a complex construction that incorporates antiretroviral therapy-based statuses of treatment and viral load, consistent with a context specific HIV risk hierarchy resembling estimates of per act HIV transmission risk found in a study of Australian gay men (Mao et al. 2013). This multidimensional understanding of ‘HIV status’ within gay men's sexual environments is reflected in the ability to indicate serostatus and safer sex behaviour preferences in user profiles on popular hook-up mobile phone applications (Race 2010), for example HIV-positive users can choose either ‘positive’ or ‘undetectable’ as their profile status on BarebackRT.com. This shift in emphasis from HIV status to HIV viral load / treatment status may explain why our measure of sexual risk (condomless anal intercourse with a sero-discordant or sero-unknown partner) was positively associated with group sex event attendance. Future research should explore and consider carefully different definitions and operationalisation of sexual ‘risk’ across group sex events as well as within research itself given shifting cultural beliefs and diffusion of recent biomedical interventions (Persson 2013).
Group sex event attending HIV-negative men in this study were also less likely to seek HIV-negative sexual partners, suggesting that they have more confidence in the serostatus of a known HIV-positive partner than an assumed HIV-negative or unknown status partner. Yet another statistically significant variable for group sex event attending HIV-negative men was to ‘look for other signs’ when their partner did not directly disclose their serostatus; suggesting that HIV-negative men engage in what Zablotska and colleagues (2009) termed ‘sero-guessing’ in their work with Australian gay men and their casual partners. This may be an attempt to help alleviate the stigma of HIV disclosure placed on HIV-positive men (Adam et al. 2011), though could also be indicative of heightened anxiety about HIV acquisition. There are important implications of this finding in terms of criminalisation of HIV non-disclosure in Canada, which has placed fully the burden on HIV-positive individuals to disclose their status to sexual partners (CHALN 2004; Symington 2009).
Finally, we must consider how these prevention strategies would work in the context of group sex events, which represent a unique risk environment. For example Freidman, Mateu-Gelabert, and Sandoval (2011) noted that even basic harm reduction measures like condom use are less effective in group sex events where participants may have multiple partners. Likewise, some HIV prevention strategies examined, e.g. sero-sorting and strategic positioning, depend on disclosure, which may not be applicable to group sex event environments such as blackout events. Consideration of group sex event behaviours points to the need for new, innovative prevention strategies that also consider group values and social mores such as normative masculinity that may challenge prevention efforts (McInnes, Bradley, and Prestage 2009). Innovative strategies include less commonly considered options such as microbicides in lube, particularly oil-based lubes used in fisting and other intensive penetrative sex in which there is a demonstrable link between risk of hepatitis C transmission and these practices (van de Laar et al. 2011; Larsen et al. 2011; Schmidt et al. 2011; Owen 2008; Le Talec 2013). In addition, for HIV-negative men, the potential of pre-exposure prophylaxis (PrEP), for group sex event attendees is considerable, but was not included in these Momentum questionnaires. We are in the process of exploring the feasibility of these strategies in an on-going qualitative project with group sex event attending participants in the Momentum Health Study.
Readers should be cautious when interpreting our results. First and foremost, this work analyses the self-reported behaviours of men attending group sex events; our study did not explore gathering detailed information on actual behaviour at gay and bisexual men's group sex events. However, our work does provide important insights into the range or behaviours that do occur at group sex events and the extent of these individual behaviours. These data are also cross-sectional and therefore cannot determine if the behaviours reported are actually effective in preventing HIV transmission or acquisition. Second, while we improved the sample representativeness by respondent driven sampling weighting procedures we make no claims in this study that the final weighted sample is truly representative, and urge caution in comparisons with other populations and locales. Lastly, while attempting to explore possible shared beliefs and behaviours among group sex event attendees, this study's true unit of analysis was the individual. As the name states, group sex events are events representing group-level social behaviour. As such, the present analysis cannot determine any sense of community and sociality group sex events represent. Certainly, gay and bisexual today need not attend group sex events to find a sexually adventurous partner who will share substances. Something more, representing group sociality, community and shared social norms, must be present for group sex events to be prevalent in so many different formats throughout North American gay and bisexual men's populations. Despite these caveats, our work showed Vancouver gay and bisexual men who are group sex event attendees feature distinctive patterns of substance use, sexual behaviour, and HIV/STI prevention strategies. Addressing the question of which gay and bisexual men attend group sex events should be important in constructing, targeting, and delivering educational and/or intervention programmes that should enhance pleasure and reduce the possibility of HIV and other STI transmission.
Acknowledgements
This work was supported by the Canadian Institutes for Health Research [107544, 134046]; National Institutes for Health, National Institute for Drug Abuse [R01DA031055]. We thank our community colleagues at the Health Initiative for Men, YouthCO HIV & Hep C Society of BC, Positive Living Society of BC for their support. We also thank the research participants for sharing their important data with the Momentum Health Study. DMM is supported by a Scholar Award from the Michael Smith Foundation for Health Research.
Footnotes
Disclosure Statement
The co-authors acknowledge that they have no financial interest or benefit arising from the direct application of this research to disclose.
References
- Adam BD, Husbands W, Murray J, Maxwell J. Circuits, Networks, and HIV Risk Management. AIDS Education and Prevention. 2008;20(5):420–434. doi: 10.1521/aeap.2008.20.5.420. [DOI] [PubMed] [Google Scholar]
- Adam BD, Murray J, Ross S, Oliver J, Lincoln SG, Rynard V. hivstigma.com, An Innovative Web-supported Stigma Reduction Intervention for Gay and Bisexual Men. Health Education Research. 2011;26(5):795–807. doi: 10.1093/her/cyq078. [DOI] [PubMed] [Google Scholar]
- Allison P. Logistic Regression Using SAS. SAS.; Cary, North Carolina: 2012. [Google Scholar]
- Canadian HIV/AIDS Legal Network (CHALN) Disclosure of HIV status after Cuerrier: Resources for Community Based AIDS Organizations. 2004 http://www.aidslaw.ca/publications/publicationsdocEN.php?ref536.
- Clatts M, Goldsamt L, Yi Y. An Emerging HIV Risk Environment: A Preliminary Epidemiological Profile of an MSM POZ Party in New York City. Sexually Transmitted Infections. 2005;81(5):373–376. doi: 10.1136/sti.2005.014894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox J, Beauchemin J, Allard R. HIV Status of Sexual Partners is More Important than Antiretroviral Treatment Related Perceptions for Risk Taking by HIV Positive MSM in Montreal, Canada. Sexually Transmitted Infections. 2004;80(6):518–523. doi: 10.1136/sti.2004.011288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher D, Reynolds G, Ware M, Napper L. Methamphetamine and Viagra Use: Relationship to Sexual Risk Behaviors. Archives of Sexual Behavior. 2011;40(2):273–279. doi: 10.1007/s10508-009-9495-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrest J, Stevenson B, Rich A, Michelow W, Pai J, Jollimore J, Raymond HF, Moore D, Hogg R, Roth EA. Community Mapping and Respondent-Driven Sampling of Gay and Bisexual Men's Communities in Vancouver, Canada. Culture, Health & Sexuality. 2014;16(3):288–301. doi: 10.1080/13691058.2014.881551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman S, Mateu-Gelabert P, Sandoval M. Group Sex Events Amongst Non-Gay Drug Users: An Understudied Risk Environment. International Journal of Drug Policy. 2011;22(1):1–8. doi: 10.1016/j.drugpo.2010.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaziani A, Cook T. Reducing HIV Infections at Circuit Parties: From Description to Explanation and Principles of Intervention Design. Journal of the International Association of Physicians in AIDS Care. 2005;4(2):32–46. doi: 10.1177/1545109705277978. [DOI] [PubMed] [Google Scholar]
- Grov C. HIV Risk and Substance Use in Men Who Have Sex with Men Surveyed in Bathhouses, Bars/Clubs, and on Craigslist.org: Venue of Recruitment Matters. AIDS and Behavior. 2012;16(4):807–817. doi: 10.1007/s10461-011-9999-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Cruz J, Parsons J. Men Who Have Sex with Men's Attitudes Toward Using Color-Coded Wristbands to Facilitate Sexual Communication at Sex Parties. Sexuality Research and Social Policy. 2014;11(1):11–19. doi: 10.1007/s13178-014-0145-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Parsons J, Bimbi D. Sexual Risk Behavior and Venues for Meeting Sex Partners: An Intercept Survey of Gay and Bisexual Men in LA and NYC. AIDS and Behavior. 2007;11(6):915–926. doi: 10.1007/s10461-006-9199-y. [DOI] [PubMed] [Google Scholar]
- Heckathorn D. Respondent-Driven Sampling: A New Approach to the Study of Hidden Populations. Social Problems. 1997;44(2):174–199. [Google Scholar]
- Heckathorn D. Respondent-Driven Sampling II: Deriving Valid Population Estimates from Chain-Referral Samples of Hidden Populations. Social Problems. 2002;49(1):11–34. [Google Scholar]
- Holt M, Treloar C. Pleasure and Drugs. International Journal of Drug Policy. 2008;19(5):349–52. doi: 10.1016/j.drugpo.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Hurley M, Prestage G. Intensive Sex Partying: Contextual Aspects of Sexual Dysfunction. Journal of HIV Therapy. 2007;12(2):44–47. [PubMed] [Google Scholar]
- Hurley M, Prestage G. Intensive Sex Partying among Gay Men in Sydney. Culture, Health and Sexuality. 2009;11(6):597–610. doi: 10.1080/13691050902721853. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Johnson JR, Adair V, Rompa D, Multhauf K, Kelly JA. Sexual Sensation Seeking: Scale Development and Predicting AIDS-Risk Behavior among Homosexually Active Men. Journal of Personality Assessment. 1994;62(3):385–397. doi: 10.1207/s15327752jpa6203_1. [DOI] [PubMed] [Google Scholar]
- Kippax S, Campbell D, Van de Ven P, Crawford J, Prestage G, Knox S, Culpin A, Kaldor J, Kinder P. Cultures of Sexual Adventurism as Markers of HIV Seroconversion: A Case Control Study in a Cohort of Sydney Gay Men. AIDS Care. 1998;10(6):677–88. doi: 10.1080/09540129848307. [DOI] [PubMed] [Google Scholar]
- Kurtz S. Between Kansas and Oz: Drugs, Sex, and the Search for Gay Identity in the Fast Lane. In: Hammack P, Cohler B, editors. The Story of Sexual Identity: Narrative Perspectives on the Gay and Lesbian Life Course. Oxford University Press; New York: 2009. pp. 157–175. [Google Scholar]
- Larsen C, Chaix M-L, Le Strat Y, Velter A, Gervais A, Auperin I, Alric L, et al. Gaining Greater Insight into HCV Emergence in HIV-infected Men Who Have Sex with Men: the HEPAIG study. PloS One. 2011;6(12):e29322. doi: 10.1371/journal.pone.0029322. doi:10.1371/journal.pone.0029322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Le Talec J. When 'Raw Sex' Turns to a “Raw Deal” ... Taking the Opportunity to Think About Sex? Interviews with HIV-positive Gay Men Diagnosed with Acute Hepatitis C. Culture, Health & Sexuality. 2013;15(10):1133–47. doi: 10.1080/13691058.2013.809478. [DOI] [PubMed] [Google Scholar]
- Lima VD, Lourenco L, Yip B, Hogg RS, Phillips P, Montaner JSG. Trends in AIDS Incidence and AIDS-related Mortality in British Columbia Between 1981 and 2013. Lancet HIV. 2015 doi: 10.1016/S2352-3018(15)00017-X. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima V, Geller J, Bangsberg D, Patterson T, Daniel M, Kerr T, Montaner J, Hogg R. The Effect of Adherence on the Association between Depressive Symptoms and Mortality among HIV-Infected Individuals First Initiating HAART. AIDS. 2007;21:1175–1183. doi: 10.1097/QAD.0b013e32811ebf57. [DOI] [PubMed] [Google Scholar]
- Lorvick J, Bourgois P, Wenger L, Arreola S, Lutnick A, Wechsberg W, Kral A. Sexual Pleasure and Sexual Risk among Women who Use Methamphetamine: A Mixed Methods Study. International Journal of Drug Policy. 2012;23(5):385–392. doi: 10.1016/j.drugpo.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansergh G, Shouse RL, Marks G, Guzman R, Rader M, Buchbinder S, Colfax GN. Methamphetamine and Sildenafil (Viagra) Use are Linked to Unprotected Receptive and Insertive Anal Sex, Respectively, in a Sample of Men Who Have Sex with Men. Sexually Transmitted Infections. 2006;82(2):131–134. doi: 10.1136/sti.2005.017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao L, Adam P, Kippax S, Holt M, Prestage G, Calmette Y, Zablotska I, de Wit J. HIV-Negative Gay Men's Perceived HIV Risk Hierarchy: Imaginary or Real? AIDS Behavior. 2013;17(4):1362–9. doi: 10.1007/s10461-012-0406-8. [DOI] [PubMed] [Google Scholar]
- McInnes D, Bradley J, Prestage G. The Discourse of Gay Men's Group Sex: The Importance of Masculinity. Culture, Health & Sexuality. 2009;11(6):641–54. doi: 10.1080/13691050902850009. [DOI] [PubMed] [Google Scholar]
- McKirnan D, Vanable P, Ostrow D, Hope B. Expectancies of Sexual ‘Escape’ and Sexual Risk among Drug and Alcohol-Involved Gay and Bisexual Men. Journal of Substance Abuse. 2001;13(1–2):137–54. doi: 10.1016/s0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, Cook J. Birds of a Feather: Homophily in Social Networks. Annual Review of Sociology. 2001;27:415–444. [Google Scholar]
- Mimiaga M, Reisner S, Bland S, Driscoll A, Cranston K, Isenberg D, Vanderwarker R, Mayer K. Sex Parties among Urban MSM: An Emerging Culture and HIV Risk Environment. AIDS & Behavior. 2011;15(2):305–318. doi: 10.1007/s10461-010-9809-6. [DOI] [PubMed] [Google Scholar]
- Mimiaga M, Reisner S, Bland S, Cranston K, Isenberg D, Driscoll M, VanDerwarker R, Mayer K. ‘It's a Quick Way to Get What You Want”: A Formative Exploration of HIV Risk among Urban Massachusetts Men Who Have Sex with Men who Attend Sex Parties. AIDS Patient Care and STDs. 2010;24(10):659–673. doi: 10.1089/apc.2010.0071. [DOI] [PubMed] [Google Scholar]
- Montaner JSG, Hogg R, Wood E, Kerr T, Tyndall M, Levy AR, Harrigan PR. The Case For Expanding Access to Highly Active Antiretroviral Therapy to Curb the Growth of the HIV Epidemic. The Lancet. 2006;368(9534):531–536. doi: 10.1016/S0140-6736(06)69162-9. [DOI] [PubMed] [Google Scholar]
- Montaner J, Lima V, Harrigan PR, Lourenço L, Yip B, Nosyk B, Wood E, et al. Expansion of HAART Coverage is Associated with Sustained Decreases in HIV/AIDS Morbidity, Mortality and HIV Transmission: The ‘HIV Treatment as Prevention’ Experience in a Canadian Setting. PloS One. 2014;9(2):e87872. doi: 10.1371/journal.pone.0087872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montaner J, Lima V, Barrios R, Yip B, Wood E, Kerr T, Shannon K, Harrigan PR, Hogg RS, Daly P, Kendall P. Association of Highly Active Antiretroviral Therapy Coverage, Population Viral Load, and Yearly New HIV Diagnoses in British Columbia, Canada: A Population-Based Study. The Lancet. 2010;376(9740):532–539. doi: 10.1016/S0140-6736(10)60936-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Byrne P, Holmes D. Desire, Drug Use and Unsafe Sex: Examination of Gay Men Who Attend Gay Circuit Parties. Culture, Health & Sexuality. 2011;13(1):1–13. doi: 10.1080/13691058.2010.510610. [DOI] [PubMed] [Google Scholar]
- Owen G. An 'Elephant in the Room'? Stigma and Hepatitis C Transmission among HIV-positive “Serosorting” Gay Men. Culture, Health & Sexuality. 2008;10(6):601–10. doi: 10.1080/13691050802061673. [DOI] [PubMed] [Google Scholar]
- Persson A. Notes on the Concepts of ‘Serodiscordance’ and ‘Risk’ in Couples with Mixed HIV Status. Global Public Health. 2013;8(2):209–220. doi: 10.1080/17441692.2012.729219. [DOI] [PubMed] [Google Scholar]
- Phillips G, Magnus M, Kuo I, Rawls A, Peterson J, West-Ojo T, Jia Y, Opoku J, Greenberg A. Correlates of Group Sex among a Community-Based Sample of Men Who Have Sex with Men (MSM) in Washington, DC. AIDS and Behavior. 2013;18(8):1413–9. doi: 10.1007/s10461-013-0527-8. doi:10.1007/s10461-013-0527-8. [DOI] [PubMed] [Google Scholar]
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP. The Relationship between Methamphetamine and Popper Use and Risk of HIV Seroconversion in the Multicenter AIDS Cohort Study. Journal of Acquired Immune Deficiency Syndromes. 2007;45(1):85. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestage G, Grierson J, Bradley J, Hurley M, Hudson J. The Role of Drugs During Group Sex among Gay Men in Australia. Sexual Health. 2009a;6(4):310–317. doi: 10.1071/SH09014. [DOI] [PubMed] [Google Scholar]
- Prestage G, Hudson J, Down I, Bradley J, Corrigan N, Hurley M, Grulich A, McInnes D. Gay Men Who Engage in Group Sex are at Increased Risk of HIV Infection and Onward Transmission. AIDS & Behavior. 2009b;13(4):724–730. doi: 10.1007/s10461-008-9460-7. [DOI] [PubMed] [Google Scholar]
- Race K. Click Here for HIV Status: Shifting Templates of Sexual Negotiation. Emotion, Space and Society. 2010;3(1):7–14. [Google Scholar]
- Saunders J, Aasland O, Babor T, de la Fuente J, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt AJ, Rockstroh JK, Vogel M, An der Heiden M, Baillot A, Krznaric I, Radun D. Trouble with Bleeding: Risk Factors for Acute Hepatitis C among HIV- Positive Gay Men from Germany—A Case-Control Study. PLoS ONE. 2011;6(3):e17781. doi: 10.1371/journal.pone.0017781. doi:10.1371/journal.pone.0017781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith G, Worth H, Kippax S. Sexual Adventurism among Sydney Gay Men. National Centre in HIV Social Research; Monograph 3/2004. Sydney: 2004. [Google Scholar]
- Symington A. Criminalization Confusion and Concerns: The Decade since the Cuerrier Decision. HIV/AIDS Policy & Law Review. 2009;14(1):4–10. [PubMed] [Google Scholar]
- van de Laar TJ, Paxton WA, Zorgdrager F, Cornelissen M, de Vries HJC. Sexual Transmission of Hepatitis C Virus in Human Immunodeficiency Virus-Negative Men Who Have Sex With Men: A Series of Case Reports. Sexually Transmitted Diseases. 2011;38(2):102. doi: 10.1097/OLQ.0b013e3181ec9de5. [DOI] [PubMed] [Google Scholar]
- Van de Ven P, Crawford J, Kippax S, Knox S, Prestage G. A Scale of Optimism– Scepticism in the Context of HIV Treatments. AIDS Care. 2000;12(2):171–176. doi: 10.1080/09540120050001841. [DOI] [PubMed] [Google Scholar]
- Volz E, Wejnert C, Cameron C, Spiller M, Barash V, Degani I, Heckathorn D. Respondent-Driven Sampling Analysis Tool (RDSAT) Version 7.1. Cornell University; Ithaca, NY: 2012. [Google Scholar]
- Vosburgh H, Mansergh G, Sullivan P, Purcell D. A Review of the Literature on Event-Level Substance Use and Sexual Risk Behavior Among Men Who Have Sex with men. AIDS & Behavior. 2012;16(6):1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Weidel J, Provencio-Vasquez E, Grossman J. Sex and Drugs: High-Risk Behaviors at Circuit Parties. American Journal of Men's Health. 2008;2(4):344–352. doi: 10.1177/1557988308322299. [DOI] [PubMed] [Google Scholar]
- Westshaver R. Coming Out of Your Skin: Circuit Parties, Pleasure and the Subject. Sexualities. 2006;8(3):347–374. [Google Scholar]
- Zablotska I, Imrie J, Prestage G, Crawford J, Rawstorne P, Grulich A, Jin F, Kippax S. Gay Men's Current Practice of HIV Seroconcordant Unprotected Anal Intercourse: Serosorting or Seroguessing? AIDS Care. 2009;21(4):501–510. doi: 10.1080/09540120802270292. [DOI] [PubMed] [Google Scholar]