Abstract
Background
Because of health disparities, incarcerated persons are at higher risk for multiple health issues, including HIV. Correctional facilities have an opportunity to provide HIV services to an underserved population. This article describes Centers for Disease Control and Prevention (CDC)–funded HIV testing and service delivery in correctional facilities.
Methods
Data on HIV testing and service delivery were submitted to CDC by 61 health department jurisdictions in 2013. HIV testing, HIV positivity, receipt of test results, linkage, and referral services were described, and differences across demographic characteristics for linkage and referral services were assessed. Finally, trends were examined for HIV testing, HIV positivity, and linkage from 2009 to 2013.
Results
Of CDC-funded tests in 2013 among persons 18 years and older, 254,719 (7.9%) were conducted in correctional facilities. HIV positivity was 0.9%, and HIV positivity for newly diagnosed persons was 0.3%. Blacks accounted for the highest percentage of HIV-infected persons (1.3%) and newly diagnosed persons (0.5%). Only 37.9% of newly diagnosed persons were linked within 90 days; 67.5% were linked within any time frame; 49.7% were referred to partner services; and 45.2% were referred to HIV prevention services. There was a significant percent increase in HIV testing, overall HIV positivity, and linkage from 2009 to 2013. However, trends were stable for newly diagnosed persons.
Conclusions
Identification of newly diagnosed persons in correctional facilities has remained stable from 2009 to 2013. Correctional facilities seem to be reaching blacks, likely due to higher incarceration rates. The current findings indicate that improvements are needed in HIV testing strategies, service delivery during incarceration, and linkage to care postrelease.
At the end of 2013, more than 1.5 million persons were incarcerated in state and federal prisons in the United States, and 731,200 were held in jails.1 Incarcerated persons are often disproportionately affected by multiple health issues, including HIV and other sexually transmitted diseases (STDs).2 According to the Bureau of Justice Statistics, the rate of HIV/AIDS among incarcerated persons has declined from 194 per 10,000 in 2001 to 146 per 10,000 in 2010. However, at the end of 2010, 20,093 incarcerated persons were living with HIV/AIDS.3 Data on Centers for Disease Control and Prevention (CDC)–funded testing in 2006 indicated 0.9% HIV positivity in correctional facilities and 0.7% newly diagnosed HIV-infected persons (new positives).4 Men aged 25 to 34 years, blacks, Hispanics/Latinos, persons tested in the South, men who have sex with men, and persons who inject drugs are more likely to be HIV infected or new positives.4–6 New positives in correctional facilities also have reported riskier behavior, including sex with someone other than their main partner, unsafe vaginal/anal sex, and sex with an at-risk partner (i.e., injected drugs, HIV-infected, or men who have sex with men).5,7
In addition to disproportionate incarceration rates, minority populations are disproportionately affected by HIV/AIDS. Blacks accounted for 44% of new infections in 2010 and 41.0% of persons living with HIV in 2011.8,9 Among CDC-funded HIV testing in 2013, 54.9% of all new positives were blacks.10 Moreover, Hispanic/Latinos accounted for 21.0% of new infections in 2010 and 20.0% of persons living with HIV in 2011.8,9 Correctional facilities are an important setting to provide HIV testing and service delivery for underserved, vulnerable populations who may be at risk for HIV/STDs.2,11
The CDC recommends routine HIV screening in health care settings for persons aged 13 to 64 years, where prevalence is 0.1% or greater.12 The CDC for HIV testing in correctional medical clinics has recommended that testing be performed unless the person declines (opt-out screening).13 Some implementation challenges with testing in correctional facilities include privacy, rapid release from jail, lack of resources, feasibility, and costs.2,14 Recent evidence suggests that opt-out testing and rapid HIV testing are feasible methods to identify persons unaware of their HIV status because results are delivered within 20 minutes. These methods may be beneficial in facilities with short lengths of stay and allow for early initiation of HIV treatment.2,5–7,14
However, challenges remain along the continuum of care for HIV-infected persons. A recent systematic review found low rates of HIV awareness, linkage and retention in care, and viral suppression among incarcerated populations.15 Most incarcerated persons spend time in jails only,16 and turnover and short-release times can frequently disrupt HIV care.17 Because there is a 40% probability of recidivism, jails can help with continuity of care through effective transitional programs for HIV-infected persons.15,16,18
HIV testing in correctional facilities provides an opportunity to target a population at high risk for HIV infection who may not otherwise access health care services. HIV service provision would not only benefit incarcerated persons but also their sexual and drug-using networks.4,11 Therefore, a better understanding of HIV testing, HIV positivity, and service delivery in correctional facilities is necessary. This article describes CDC-funded HIV testing and HIV-related services in correctional facilities in 2013. The aims are to assess (1) HIV testing; (2) identification of HIV-infected persons, including new positives; (3) linkage to HIV medical care; (4) referral to partner services; and (5) referral to HIV prevention services. Demographic characteristics of persons who received HIV-related services in correctional facilities were described. In addition, differences across demographic characteristics on linkage and referral services were analyzed, and trends for HIV testing, HIV positivity, and linkage in CDC-funded correctional facilities from 2009 to 2013 were examined.
MATERIALS AND METHODS
Data Source
Since 2012, the CDC has funded 61 health department jurisdictions, which include the 50 states, District of Columbia, Puerto Rico, US Virgin Islands, and 8 directly funded city/county health departments to provide HIV testing and other HIV prevention activities. Previously, from 2009 to 2011, 59 health departments were funded. HIV testing data are collected locally and submitted biannually to the National HIV Prevention Program Monitoring and Evaluation (NHM&E) system, a secure CDC-supported online reporting system. Data submitted by June 2, 2014, from CDC-funded nonclinical and clinical correctional facilities, were included for 2013 analyses. A nonclinical correctional facility is defined as a penal or correctional facility, prison, jail detention center, community-based rehabilitation center, or any similar institution designed for the confinement or rehabilitation of criminal offenders. A clinical correctional facility is defined as an area within a penal or correctional facility, including prison and adult or juvenile detention facilities, that provides medical or health services.
Measures
Demographics
This included self-reported data on age, sex, and race/ethnicity. Jurisdictions were assigned to the Northeast, South, Midwest, and West, using US Census categorizations.
HIV Testing Events and Receipt of HIV Test Results
HIV testing events included all HIV testing records submitted to the NHM&E system, for which a test technology (conventional, rapid, nucleic acid amplification test, RNA viral load testing, or other) or test result (positive, negative, indeterminate, or invalid) was reported. Data on test technology were categorized as rapid test only, conventional test only (nucleic acid amplification test/RNA or other conventional HIV test), or rapid and conventional. Receipt of HIV test result measured whether persons received results from the initial testing site or obtained results from another agency for at least one test in the testing event.
HIV Positivity
HIV-infected persons included those who tested HIV-positive during the current test event. New positives included those who tested HIV positive during the current test event but self-reported not having a previous HIV-positive test result.
Linkage to HIV Medical Care
Linkage was defined as attendance at first medical appointment for HIV-infected persons. Grantees collect these data in various ways, including client self-report, medical records, surveil-lance, or local program data. Linkage was examined for new positives in 2013. Trend analyses from 2009 to 2013 examined linkage for both HIV-infected persons and new positives. In addition, linkage within 90 days and linkage within any time frame (i.e., within 90 days and >90 days) are described.
Referral for Partner Services
Partner services are a set of confidential, voluntary services to help HIV-infected persons notify their sex and drug injection partners of possible HIV exposure, to offer services that can protect the health of partners, and to prevent STD reinfection.19 Persons who were either referred to or interviewed for partner services were considered referred. Referral for partner services was examined for new positives in 2013.
Referral to HIV Prevention Services
HIV prevention services are defined as any service or intervention directly aimed at reducing risk for transmitting or acquiring HIV infection (e.g. risk-reduction counseling).20 It excludes HIV posttest counseling and indirect services such as mental health services or housing. Referral to HIV prevention services was examined for new positives in 2013.
Data Analysis Plan
Descriptive statistics examined HIV testing and service delivery in correctional facilities by demographic characteristics. In addition, log binominal analyses assessed differences across demographic characteristics for linkage and referral services. Finally, estimated annual percent change (EAPC) analyses examined trends in HIV testing and service delivery in correctional facilities from 2009 to 2013. Analyses were conducted in SAS, version 9.3.
RESULTS
HIV Testing and Receipt of HIV Test Results
In 2013, 3,213,187 CDC-funded HIV testing events were conducted among persons 18 years and older. Of those, 254,719 (7.9%) were conducted in correctional facilities. Puerto Rico and the US Virgin Islands did not submit data from correctional facilities in 2013; therefore, results are from 59 health department jurisdictions. Most HIV testing events in correctional facilities were conducted among persons aged 18 to 29 years (44.2%) and 30 to 39 years (26.5%), males (75.8%), and in the South (46.7%) and Northeast (34.0%). By race/ethnicity, 45.8% of HIV testing events were among blacks, compared with 29.6% among whites and 18.9% among Hispanics/Latinos. Rapid HIV testing was the most commonly used HIV test technology, accounting for 69.6% of testing events (Table 1).
TABLE 1.
HIV Testing and HIV Positivity Among Persons in Correctional Facilities by Demographic Characteristics in the United States, 59 CDC-funded Health Department Jurisdictions, 2013
| HIV Testing Events* |
Test Technology† |
HIV Test Results Received† |
HIV-infected Persons† |
Newly Diagnosed HIV-infected Persons† |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rapid Only |
Conventional Only |
Rapid and Conventional |
||||||||||||
| Demographic Characteristics | n | (Col%) | n | (%) | n | (%) | N | (%) | n | (%) | n | (%) | n | (%) |
| Age groups, y | ||||||||||||||
| 18–29 | 112,526 | (44.2) | 77,618 | (69.0) | 34,448 | (30.6) | 222 | (0.2) | 84,963 | (75.5) | 552 | (0.5) | 274 | (0.2) |
| 30–39 | 67,440 | (26.5) | 46,947 | (69.6) | 20,187 | (29.9) | 188 | (0.3) | 51,500 | (76.4) | 608 | (0.9) | 212 | (0.3) |
| 40–49 | 39,849 | (15.6) | 28,341 | (71.1) | 11,257 | (28.2) | 161 | (0.4) | 31,057 | (77.9) | 636 | (1.6) | 199 | (0.5) |
| 50+ | 24,527 | (9.6) | 17,564 | (71.6) | 6,805 | (27.7) | 119 | (0.5) | 18,876 | (77.0) | 482 | (2.0) | 148 | (0.6) |
| Sex | ||||||||||||||
| Male | 192,994 | (75.8) | 137,095 | (71.0) | 54,992 | (28.5) | 540 | (0.3) | 151,442 | (78.5) | 1,833 | (0.9) | 672 | (0.3) |
| Female | 60,990 | (23.9) | 39,813 | (65.3) | 20,906 | (34.3) | 147 | (0.2) | 42,586 | (69.8) | 442 | (0.7) | 165 | (0.3) |
| Race/Ethnicity and sex | ||||||||||||||
| White | 75,403 | (29.6) | 49,063 | (65.1) | 26,053 | (34.6) | 98 | (0.1) | 54,804 | (72.7) | 380 | (0.5) | 154 | (0.2) |
| White men | 51,796 | (20.3) | 33,496 | (64.7) | 18,112 | (35.0) | 62 | (0.1) | 37,944 | (73.3) | 293 | (0.6) | 115 | (0.2) |
| White women | 23,499 | (9.2) | 15,501 | (66.0) | 7,899 | (33.6) | 36 | (0.2) | 16,788 | (71.4) | 87 | (0.4) | 39 | (0.2) |
| Black or African American | 116,691 | (45.8) | 89,105 | (76.4) | 26,824 | (23.0) | 509 | (0.4) | 95,864 | (82.2) | 1,570 | (1.3) | 543 | (0.5) |
| Black or African American men | 94,191 | (37.0) | 73,295 | (77.8) | 20,276 | (21.5) | 412 | (0.4) | 78,948 | (83.8) | 1,265 | (1.3) | 441 | (0.5) |
| Black or African American women | 22,359 | (8.8) | 15,714 | (70.3) | 6,508 | (29.1) | 92 | (0.4) | 16,811 | (75.2) | 295 | (1.3) | 100 | (0.4) |
| Hispanic or Latino | 48,263 | (18.9) | 31,611 | (65.5) | 16,568 | (34.3) | 69 | (0.1) | 36,072 | (74.7) | 266 | (0.6) | 112 | (0.2) |
| Hispanic or Latino men | 37,065 | (14.6) | 24,836 | (67.0) | 12,164 | (32.8) | 53 | (0.1) | 28,809 | (77.7) | 219 | (0.6) | 92 | (0.2) |
| Hispanic or Latina women | 11,123 | (4.4) | 6,715 | (60.4) | 4,389 | (39.5) | 16 | (0.1) | 7,200 | (64.7) | 47 | (0.4) | 20 | (0.2) |
| Region | ||||||||||||||
| Northeast | 86,630 | (34.0) | 62,442 | (72.1) | 23,576 | (27.2) | 125 | (0.1) | 59,004 | (68.1) | 335 | (0.4) | 159 | (0.2) |
| Mdwest | 10,670 | (4.2) | 9,015 | (84.5) | 1,629 | (15.3) | 25 | (0.2) | 10,478 | (98.2) | 37 | (0.3) | 28 | (0.3) |
| South | 118,941 | (46.7) | 77,850 | (65.5) | 40,571 | (34.1) | 517 | (0.4) | 96,297 | (81.0) | 1,808 | (1.5) | 597 | (0.5) |
| West | 38,478 | (15.1) | 28,036 | (72.9) | 10,415 | (27.1) | 27 | (0.1) | 28,679 | (74.5) | 109 | (0.3) | 57 | (0.1) |
| Total | 254,719 | (100.0) | 177,343 | (69.6) | 76,191 | (29.9) | 694 | (0.3) | 194,458 | (76.3) | 2,289 | (0.9) | 841 | (0.3) |
The percentages for HIV testing events are column percentages.
The denominator of the percentages for test technology, HIV test results received, HIV-infected persons, and newly diagnosed HIV-infected persons is HIV testing events.
HIV test results were provided for 76.3% of all CDC-funded testing events in correctional facilities. Descriptive analyses revealed that 77.9% of persons aged 40 to 49 years, 77.0% of persons 50 years and older, 78.5% of males, 82.2% of blacks, 98.2% of persons in the Midwest, and 81.0% of persons in the South received their results. Only 64.7% of Hispanic/Latina females received their results, which was relatively lower than other racial/ethnic and sex groups (Table 1).
HIV Positivity
HIV positivity was 0.9% (2289) in correctional facilities. Persons aged 40 to 49 years (1.6%) and 50 years and older (2.0%), blacks (1.3%), and persons in the South (1.5%) were the groups with the highest percentages of HIV-infected persons. Among all HIV testing events, 0.3% (841) were new positives, and among all HIV-infected persons, 36.7% (841/2289) were new positives. Descriptive analyses revealed that 0.5% of persons aged 40 to 49 years, 0.6% of persons 50 years and older, 0.5% of blacks, and 0.5% of persons in the South were new positives. By race/ethnicity, 0.5% of blacks, 0.2% of Hispanics/Latinos, and 0.2% of whites were new positives (Table 1).
Linkage to HIV Medical Care and Referral Services
Among the 841 new positives, 67.5% were linked to HIV medical care within any time frame after testing. Descriptive analyses revealed that 72.3% of persons 50 years and older, 67.9% of males, and 72.3% of persons in the Northeast were linked within any time frame. Log binomial regression analyses indicated that whites (59.1%) were linked within any time frame significantly less than blacks (69.6%). In addition, persons in the Midwest (32.1%) were linked within any time frame significantly less than persons in the South (67.5%; Table 2).
TABLE 2.
Linkage to HIV Medical Care, Referral to Partner Services, and Referral to HIV Prevention Services Among Newly Diagnosed HIV-infected Persons in Correctional Facilities by Demographic Characteristics in the United States, 59 CDC-funded Health Department Jurisdictions, 2013
| Newly Diagnosed HIV-Infected Persons |
Linkage to HIV Medical Care within Any Time Frame* |
Linkage to HIV Medical Care within 90 days* |
Referral to HIV Partner Services* |
Referral to HIV Prevention Services* |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Demographic Characteristics | No. | No. | (%) | PR† (95% CI) | No. | (%) | PR† (95% CI) | No. | (%) | PR† (95% CI) | No. | (%) | PR† (95% CI) |
| Age groups, y | |||||||||||||
| 18–29 | 274 | 179 | (65.3) | Referent | 120 | (43.8) | Referent | 165 | (60.2) | Referent | 141 | (51.5) | Referent |
| 30–39 | 212 | 144 | (67.9) | 1.04 (0.92–1.18) | 76 | (35.8) | 0.82 (0.65–1.02) | 100 | (47.2) | 0.78 (0.66–0.93) | 86 | (40.6) | 0.79 (0.65–0.96) |
| 40–49 | 199 | 134 | (67.3) | 1.03 (0.91–1.17) | 70 | (35.2) | 0.80 (0.64–1.01) | 82 | (41.2) | 0.68 (0.56–0.83) | 91 | (45.7) | 0.89 (0.73–1.07) |
| 50+ | 148 | 107 | (72.3) | 1.11 (0.97–1.26) | 49 | (33.1) | 0.76 (0.58–0.99) | 66 | (44.6) | 0.74 (0.60–0.91) | 59 | (39.9) | 0.77 (0.62–0.97) |
| Sex | |||||||||||||
| Male | 672 | 456 | (67.9) | Referent | 257 | (38.2) | Referent | 330 | (49.1) | Referent | 306 | (45.5) | Referent |
| Female | 165 | 110 | (66.7) | 0.98 (0.87–1.11) | 60 | (36.4) | 0.95 (0.76–1.19) | 84 | (50.9) | 1.04 (0.88–1.23) | 72 | (43.6) | 0.96 (0.79–1.16) |
| Race/Ethnicity | |||||||||||||
| Black | 543 | 378 | (69.6) | Referent | 229 | (42.2) | Referent | 277 | (51.0) | Referent | 242 | (44.6) | Referent |
| Hispanic or Latino | 112 | 82 | (73.2) | 1.05 (0.93–1.19) | 40 | (35.7) | 0.85 (0.65–1.11) | 50 | (44.6) | 0.88 (0.70–1.09) | 47 | (42.0) | 0.94 (0.74–1.19) |
| White | 154 | 91 | (59.1) | 0.85 (0.74–0.98) | 38 | (24.7) | 0.59 (0.44–0.78) | 65 | (42.2) | 0.83 (0.68–1.01) | 75 | (48.7) | 1.09 (0.91–1.32) |
| Race/Ethnicity and sex | |||||||||||||
| Male | |||||||||||||
| Black | 441 | 305 | (69.2) | Referent | 193 | (43.8) | Referent | 231 | (52.4) | Referent | 200 | (45.4) | Referent |
| Hispanic or Latino | 92 | 67 | (72.8) | 1.05 (0.92–1.21) | 26 | (28.3) | 0.65 (0.46–0.91) | 36 | (39.1) | 0.75 (0.57–0.98) | 37 | (40.2) | 0.89 (0.68–1.16) |
| White | 115 | 69 | (60.0) | 0.87 (0.74–1.02) | 27 | (23.5) | 0.54 (0.38–0.76) | 44 | (38.3) | 0.73 (0.57–0.94) | 55 | (47.8) | 1.05 (0.85–1.31) |
| Female | |||||||||||||
| Black | 100 | 72 | (72.0) | Referent | 35 | (35.0) | Referent | 44 | (44.0) | Referent | 41 | (41.0) | Referent |
| Hispanic or Latino | 20 | 15 | (75.0) | 1.04 (0.79–1.38) | 14 | (70.0) | 2.00 (1.35–2.96) | 14 | (70.0) | 1.59 (1.11–2.29) | 10 | (50.0) | 1.22 (0.74–2.01) |
| White | 39 | 22 | (56.4) | 0.78 (0.58–1.06) | 11 | (28.2) | 0.81 (0.46–1.42) | 21 | (53.8) | 1.22 (0.85–1.76) | 20 | (51.3) | 1.25 (0.85–1.84) |
| Region | |||||||||||||
| South | 597 | 403 | (67.5) | Referent | 225 | (37.7) | Referent | 317 | (53.1) | Referent | 214 | (35.8) | Referent |
| Northeast | 159 | 115 | (72.3) | 1.07 (0.96–1.20) | 47 | (29.6) | 0.78 (0.60–1.02) | 43 | (27.0) | 0.51 (0.39–0.66) | 115 | (72.3) | 2.02 (1.75–2.33) |
| Midwest | 28 | 9 | (32.1) | 0.48 (0.28–0.82) | 9 | (32.1) | 0.85 (0.49–1.48) | 13 | (46.4) | 0.87 (0.58–1.31) | 11 | (39.3) | 1.10 (0.68–1.76) |
| West | 57 | 41 | (71.9) | 1.07 (0.90–1.26) | 38 | (66.7) | 1.77 (1.43–2.18) | 45 | (78.9) | 1.49 (1.27–1.73) | 40 | (70.2) | 1.96 (1.60–2.39) |
| Total | 841 | 568 | (67.5) | 319 | (37.9) | 418 | (49.7) | 380 | (45.2) | ||||
The denominator for the percentages for linkage to HIV medical care, referral to partner services, and referral to HIV prevention services is newly diagnosed HIV-infected persons.
Unadjusted prevalence ratio.
Among all new positives, 37.9% were linked to HIV medical care within 90 days. Descriptive analyses revealed that 43.8% of persons aged 18 to 29 years, 38.2% of males, 42.2% of blacks, and 66.7% of persons in the West were linked within 90 days. Log binomial regression analyses indicated that persons 50 years and older (33.1%) were linked within 90 days significantly less than persons aged 18 to 29 years (43.8%). In addition, whites (24.7%) were linked within 90 days significantly less than blacks (42.2%). Finally, white males (23.5%) and Hispanic/Latino males (28.3%) were linked within 90 days significantly less than black males (43.8%), and Hispanic/Latina females (70.0%) were linked within 90 days significantly more than black females (35.0%; Table 2).
Approximately half of new positives were referred to partner services. Descriptive analyses revealed that 70.0% of Hispanic/ Latina females and 53.8% of white females were referred to partner services, whereas only 39.1% of Hispanic/Latino males and 38.3% of white males were referred. Log binomial regression analyses indicated that persons aged 30 to 39 years (47.2%), 40 to 49 years of age (41.2%), and 50 years and older (44.6%) were referred to partner services significantly less than persons aged 18 to 29 years (60.2%). Also, Hispanic/Latino males (39.1%) and white males (38.3%) were referred to partner services significantly less than black males (52.4%). Hispanic/Latina females (70.0%) were referred to partner services significantly more than black females (44.0%). Finally, persons in the Northeast (27.0%) were referred to partner services significantly less than persons in the South (53.1%), whereas those in the West (78.9%) were referred significantly more than those in the South (Table 2).
Finally, 45.2% of new positives were referred to HIV prevention services. Descriptive analyses indicated that 51.5% of persons aged 18 to 29 years, 45.5% of males, and 48.7% of whites were referred to HIV prevention services. Log binomial regression analyses indicated that persons aged 30 to 39 years (40.6%) and 50 years and older (39.9%) were referred to HIV prevention services significantly less than persons aged 18 to 29 years (51.5%). Also, persons in the Northeast (72.3%) and in the West (70.2%) were referred to HIV prevention services significantly more than persons in the South (35.8%; Table 2).
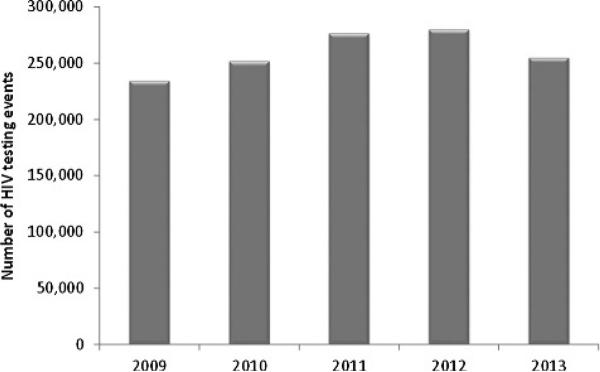
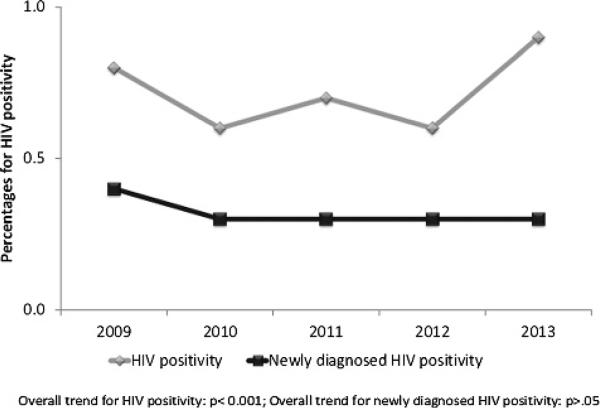
HIV Testing and HIV Positivity From 2009 to 2013
Trend analyses indicated that the number of HIV testing events in correctional facilities increased from 2009 to 2012 and decreased slightly in 2013. The EAPC increase for the number of HIV testing events between 2009 and 2013 was 2.7% (Fig. 1). The percentage of HIV-infected persons and new positives varied between years. From 2009 to 2013, the EAPC for total HIV positivity increased by 4.4% (P < 0.001). Although not statistically significant, the EAPC for new positives between 2009 and 2013 decreased by 2.1% (P > 0.05). Overall, identification of new positives remained stable at 0.3% from 2010 to 2013 (Fig. 2).
Figure 1.
Number of CDC-funded HIV testing events in correctional facilities in the United States, 2009–2013.
Figure 2.
Percentages of HIV-infected and newly diagnosed HIV-infected persons in correctional facilities in the United States, 2009–2013.
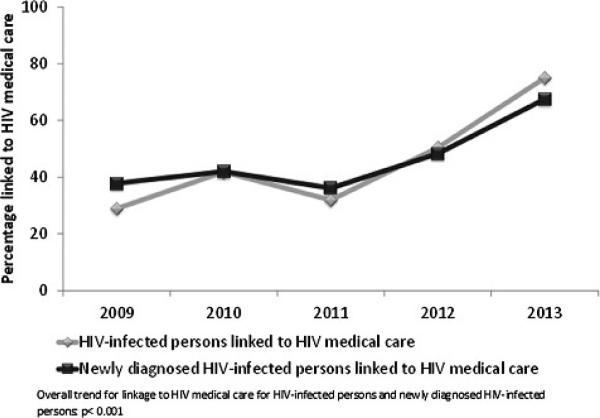
The EAPC of HIV-infected persons linked to HIV medical care within any time frame increased from 2009 to 2010, decreased in 2011, and increased in 2012 and in 2013. The percentage of HIV-infected persons linked significantly increased by 26.8% (P < 0.001) between 2009 and 2013. The percentage of new positives linked to HIV medical care within any time frame increased from 2009 to 2010 but decreased in 2011, resulting in a fairly stable percentage of persons linked between the 3 years. However, the linkage percentages increased considerably in 2012 and in 2013. The EAPC of new positives linked significantly increased by 15.6% (P < 0.001) between 2009 and 2013 (Fig. 3).
Figure 3.
Percentages of HIV-infected and newly diagnosed HIV-infected persons linked to HIV medical care within any time frame in correctional facilities in the United States, 2009–2013.
DISCUSSION
HIV testing and knowledge of HIV status are gateways to services along the HIV continuum of care. Early initiation of and adherence to antiretroviral therapy has substantial medical and prevention benefits for HIV-infected persons by reducing HIV transmission to HIV-negative partners by up to 96%.21,22 Therefore, it is critical to ensure all HIV-infected persons receive necessary HIV prevention, care, and treatment services. The National HIV/AIDS Strategy23 has set goals of reducing new HIV infections and having 85% of new positives linked to HIV medical care within 90 days by 2015. In 2013, only 37.9% of new positives in correctional facilities were linked to medical care within 90 days, and 67.5% were linked within any time frame. Percentages for referral to partner services and HIV prevention services also were relatively low at 49.7% and 45.2%, respectively. Linkage and referral percentages should be significantly improved to ensure that HIV-infected persons and their partners have access to HIV prevention and treatment services.
Overall, blacks accounted for 45.8%, and black males accounted for 37.0% of the CDC-funded HIV testing events conducted in correctional facilities. In addition, overall HIV positivity among blacks was highest compared with other racial/ethnic groups. The percentage of new positives also was highest among blacks at 0.5%, although lower than the 1.0% found in a previous study on CDC-funded testing in correctional facilities.4 These findings are consistent with blacks being disproportionately affected by HIV in the United States.9,10
HIV testing events funded by CDC in correctional facilities increased overall from 2009 to 2012 but decreased in 2013. Although overall HIV positivity increased from 2009 to 2013, the percentage of new positives has remained stable at 0.3% since 2010. This suggests that despite the overall increase in HIV testing, it has become more challenging to identify new positives. For example, a previous study on CDC-funded testing in 2006 found 0.7% new positives.4 In addition, in comparison to several other CDC-funded site types in 2013, correctional facilities identified a lower percentage of new positives.24
The findings have limitations. Type of correctional facility is not a required reporting variable by CDC. Jails have a rapid turnover, whereas prisons have longer incarceration times so testing and HIV-related service delivery may occur more frequently. Because of challenges with ensuring linkage and continuation of services for persons postrelease, data on services provided post-release were likely not reported, leading to missing data. Moreover, the percentage of missing data was high across service delivery indicators. Therefore, results are likely underestimating service delivery and represent the minimum percent achieved. Linkage to HIV medical care within 90 days became a required reporting variable starting in 2012. This may contribute to incomplete data because of the time it may take grantees to update their data systems for reporting. However, there have been significant improvements in data quality each year. In addition, self-report was used to identify new positives. The percentage of new positives is likely an overestimate because of self-report bias and because HIV testing programs often offer incentives for getting tested. Finally, although the sample size is large, this article only represents CDC-funded tests in correctional facilities. Therefore, findings may not be generalizable to all correctional facilities in the United States.
Centers for Disease Control and Prevention guidance recommends that HIV testing in correctional facilities be offered both upon entry and before release as part of routine care.2,13 However, because of varying policies and limited resources, implementation varies by state, county, and facility.25 A recent study found that only 19% of prisons and 35% of jails provide opt-out testing. In addition, less than 20% followed CDC's recommendations regarding discharge planning services.26 To reduce new HIV infections, it is important to test and treat, as indicated, populations at high risk for HIV. In 2006, an estimated 14% of HIV-infected persons had contact with a correctional facility.16 This provides an opportunity to link underserved HIV-infected persons into HIV medical care and other prevention services before they return to their communities and sexual and drug-using networks. However, previous research suggests that it is challenging to retain HIV-infected persons who receive services while incarcerated in HIV care and other prevention services postrelease.15,27,28 They may not adhere to their HIV medications, discontinue treatment, and/or engage in high risk behavior that may increase HIV transmission.27,28 Other factors that may contribute are poor access to health care upon release, substance use, mental health issues, unstable housing, and unemployment.11,13,27,29–31
Routine HIV testing and provision of HIV-related services in correctional facilities have important public health implications. Efforts should be made to increase opt-out testing and improve the continuum of care postrelease.15 Transitional programs beyond case management could facilitate HIV medical care and other prevention services postrelease. Collaboration between prisons and community-based organizations may ensure continuation of services.13,32 Incarcerated persons with HIV are a vulnerable and underserved population. Providing HIV-related services will not only benefit their health but also the health of the communities to which they return. Various cost-effective and feasible program-matic models that consider the unique policy and economic factors of HIV testing and provision of HIV-related services in correctional facilities and postrelease should be evaluated.
Acknowledgments
The authors thank Dr Charles Rose from the Centers for Disease Control and Prevention (CDC) for his statistical consultation.
Footnotes
Conflicts of Interest: None.
CDC disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the CDC.
REFERENCES
- 1.Glaze LE, Kaeble D. Correctional Populations in the United States, 2013. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics.; Washington, DC: 2014. NCJ 248479. [Google Scholar]
- 2.Centers for Disease Control and Prevention [November 20, 2014];HIV in correctional settings. 2012 Available at: http://www.cdc.gov/hiv/risk/other/correctional.html.
- 3.Maruschak LM. HIV in Prisons, 2001–2010. U.S. Department of Justice, Office of Justice Programs, Bureau of Justice Statistics; Washington, DC: 2012. NCJ 238877. [Google Scholar]
- 4.VanHandel M, Beltrami JF, MacGowan RJ, et al. Newly identified HIV infections in correctional facilities, United States, 2007. Am J Public Health. 2012;102:S201–S204. doi: 10.2105/AJPH.2011.300614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Macgowan R, Margolis A, Richardson-Moore A, et al. Voluntary rapid human immunodeficiency virus (HIV) testing in jails. Sex Transm Dis. 2009;36(2 suppl):S9–S13. doi: 10.1097/OLQ.0b013e318148b6b1. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention (CDC) Routine HIV screening during intake medical evaluation at a County Jail—Fulton County, Georgia, 2011–2012. MMWR Morb Mortal Wkly Rep. 2013;62:495–497. [PMC free article] [PubMed] [Google Scholar]
- 7.de Voux A, Spaulding AC, Beckwith C, et al. Early identification of HIV: Empirical support for jail-based screening. PLoS One. 2012;7:e37603. doi: 10.1371/journal.pone.0037603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention Estimated HIV incidence in the United States, 2007–2010. [April 17, 2015];HIV Surveillance Supplemental Report 2012. 2012 Dec;17(No. 4) Available at: http://wwwcdcgov/hiv/pdf/statistics_hssr_vol_17_no_4pdf. [Google Scholar]
- 9.Bradley H, Hall HI, Wolitski RJ, et al. Vital Signs: HIV diagnosis, care, and treatment among persons living with HIV—United States, 2011. MMWR Morb Mortal Wkly Rep. 2014;63:1113–1117. [PMC free article] [PubMed] [Google Scholar]
- 10.Seth P, Walker T, Hollis N, et al. HIV testing and service delivery among Blacks or African Americans—61 health department jurisdictions, United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:87–90. [PMC free article] [PubMed] [Google Scholar]
- 11.Rich JD, DiClemente R, Levy J, et al. Correctional facilities as partners in reducing HIV disparities. J Acquir Immune Defic Syndr. 2013;63:S49–S53. doi: 10.1097/QAI.0b013e318292fe4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(RR-14):1–17. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention [November 20, 2014];HIV testing implementation guidance for correctional settings. 2009 Available at: http://www.cdc.gov/hiv/pdf/risk_Correctional_Settings_Guidelines.pdf.
- 14.Spaulding AC, Booker CA, Freeman SH, et al. Jails, HIV testing, and linkage to care services: An overview of the EnhanceLink Initiative. AIDS Behav. 2013;17:S100–S107. doi: 10.1007/s10461-012-0339-2. [DOI] [PubMed] [Google Scholar]
- 15.Iroh PA, Mayo H, Nijhawan AE. The HIV care cascade before, during, and after incarceration: A systematic review and data synthesis. Am J Public Health. 2015;105:e5–e16. doi: 10.2105/AJPH.2015.302635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spaulding AC, Seals RM, Page MJ, et al. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: Declining share of epidemic but persistent public health opportunity. PLoS One. 2009;4:e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Westergaard RP, Kirk GD, Richesson DR, et al. Incarceration predicts virologic failure for HIV-infected injection drug users receiving antiretroviral therapy. Clin Infect Dis. 2011;53:725–731. doi: 10.1093/cid/cir491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Springer SA, Spaulding AC, Meyer JP, et al. Public health implications for adequate transitional care for HIV-infected prisoners: Five essential components. Clin Infect Dis. 2011;53:469–479. doi: 10.1093/cid/cir446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention [October 6, 2014];Recommended prevention services. 2013 Available at: http://www.cdc.gov/hiv/prevention/programs/pwp/partnerservices.html.
- 20.Centers for Disease Control and Prevention, Health Resources and Services Administration, National Institutes of Health et al. [December 12, 2014];Recommendations for HIV Prevention with Adults and Adolescents with HIV in the United States, 2014. 2014 Dec; Available at: http://stacks.cdc.gov/view/cdc/26062.
- 21.Kitahata MM, Gange SJ, Abraham AG, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–1826. doi: 10.1056/NEJMoa0807252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 Infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White House Office of National AIDS Policy [April 24, 2014];National HIV/AIDS strategy for the United States. 2010 Available at: http://www.whitehouse.gov/sites/default/files/uploads/NHAS.pdf.
- 24.Seth P, Wang G, Collins NT, et al. Identifying new positives and linkage to HIV medical care—23 testing site types, United States, 2013. MMWR Morb Mortal Wkly Rep. 2015;64:663–667. [PMC free article] [PubMed] [Google Scholar]
- 25.Pope JL. HIV testing in state correctional systems, 22. J.L. & Health. 2009 Available at: http://engagedscholarship.csuohio.edu/jlh/vol22/iss1/4.
- 26.Solomon L, Montague BT, Beckwith CG, et al. Survey finds that many prisons and jails have room to improve HIV testing and coordination of postrelease treatment. Health Aff (Millwood) 2014;33:434–442. doi: 10.1377/hlthaff.2013.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Milloy MJ, Montaner JS, Wood E. Incarceration of people living with HIV/AIDS: Implications for treatment-as-prevention. Curr HIV/AIDS Rep. 2014;11:308–316. doi: 10.1007/s11904-014-0214-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Baillargeon J, Giordano TP, Rich JD, et al. Accessing antiretroviral therapy following release from prison. JAMA. 2009;301:848–857. doi: 10.1001/jama.2009.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Binswanger IA, Stern MF, Deyo RA, et al. Release from prison—A high risk of death for former inmates. N Engl J Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wakeman SE, McKinney ME, Rich JD. Filling the gap: The importance of medicaid continuity for former inmates. J Gen Intern Med. 2009;24:860–862. doi: 10.1007/s11606-009-0977-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control andPrevention Integrated prevention services for HIV infection, viral hepatitis, sexually transmitted diseases, and tuberculosis for persons who use drugs illicitly: Summary guidance from CDC and the U.S. Department of Health and Human Services. Morb Mortal Wkly Rep Recomm Rep. 2012;61(RR-5):1–40. [PubMed] [Google Scholar]
- 32.Teixeira PA, Jordan AO, Zaller N, et al. Health outcomes for HIV-infected persons released from the New York City jail system with a transitional care-coordination plan. Am J Public Health. 2015;105:351–357. doi: 10.2105/AJPH.2014.302234. [DOI] [PMC free article] [PubMed] [Google Scholar]