Abstract
Background
Esophageal cancer has been a common cancer in China for many years. Using the most recent data collected from the National Central Cancer Registry, we present estimates of the esophageal cancer burden in China in 2011.
Methods
Age‐specific incidence and mortality rates by gender and area for 18 age groups were calculated based on data from 177 qualified population‐based cancer registries. The number of new cases of esophageal cancer and cancer deaths were computed by multiplying these rates by the 2011 population. Crude incidence and mortality rates of esophageal cancer were estimated.
Results
The estimated number of new esophageal cancer cases and deaths were 291 238 and 218 957, respectively. The crude incidence and mortality rates for esophageal cancer were 21.62/100 000 and 16.25/100 000, respectively. The age‐standardized incidence and mortality rates by world population were 15.83/100 000 and 11.62/100 000, respectively. Both the incidence and mortality rates of esophageal cancer were higher in rural areas than in urban areas, and in men than in women. The age‐specific esophageal cancer incidence and mortality rates increased with age. In China, squamous cell cancer was the most common pathological type of the disease.
Conclusion
Esophageal cancer remains a major public health issue in China. Primary and secondary prevention are essential for disease control.
Keywords: China, esophageal cancer, incidence, mortality
Introduction
Esophageal cancer is a major public health problem in China. It is the eighth most common cancer worldwide, and the sixth most common cause of death from cancer. About 80% of the cases occur in developing countries. China contributed almost half of the global new esophageal cancer cases in 2012; it was the sixth most common cancer in China in 2011.3 While published studies have shown that incidence rates of esophageal cancer have decreased in China over the last 20 years, esophageal cancer still represents a significant burden.4 Subtypes of the disease include esophageal adenocarcinoma (EAC) and esophageal squamous cell carcinoma (ESCC).
The National Central Cancer Registry (NCCR) in China has collected population‐based cancer statistics for more than 20 years and is the only source to report national population‐based cancer incidence and mortality data. The cancer registration network has expanded during the past five years. Up to 2014, there were a total of 304 cancer registries in China, covering 300 million of the population.3 In the present study, we provide the expected numbers of new esophageal cancer cases and deaths in 2011 in the Chinese population, as well as a comprehensive overview of esophageal cancer incidence and mortality using the latest population‐based cancer registration data. Because of the time required for data collection, quality control, and analysis, the latest cancer statistics available have a three to four year lag behind the current year.
Materials and methods
Source of the data
Population‐based cancer registries systematically collect the data of all new cancer cases and deaths from local hospitals, healthcare centers, the health insurance database, the death surveillance system, and clinics, using passive and active methods. Cancer registries are responsible for compiling new cancer cases and cancer deaths, using identification card numbers as personal identification codes. However, cancer death records should be matched with incidence records to enable detection of missing and duplicated cases. Local registries collect information on patient age, gender, date of diagnosis, identification number, anatomical and sub‐sites, and diagnostic methods. Each year, local registries report new cancer incidence and mortality data to NCCR. By June 2014, 234 cancer registries from 31 provinces submitted population‐based data of new cancer cases and cancer deaths to NCCR. Of the 234 registries, 98 registries were from urban areas and 136 from rural areas. The overall population coverage for the registries was 221.4 million, accounting for 16.43% of the whole Chinese population.
The quality and completeness of cancer registration data was assessed using IARC‐crgTools (International Agency for Research on Cancer, Lyon, France) to identify errors, inconsistencies, and unusual combinations of cancer site, morphology, gender, and age at diagnosis. Questionable records were returned to the cancer registry for verification and correction. After data quality control, a total of 177 cancer registries (77 in urban and 100 in rural areas), from 28 provinces, met quality requirements for reporting the cancer statistics, covering 13.01% of the national population. A detailed distribution of the cancer registries has previously been reported.3 All cancer cases were classified according to the International Classification of Diseases for Oncology‐3 (ICD‐O‐3) and ICD‐10. Invasive cases of esophageal cancer (C15) were retrieved from the entire cancer database.
The National Bureau of Statistics provided the 2011 overall population data by area and gender.5 The fifth and sixth National Population Census data provided 2000 and 2010 population data by age group, gender, and area.5 To further estimate the 2011 age‐specific population data in each age strata (0–, 1–4, 5–84 by 5 years, 85+ years) by gender and area, we first calculated a change in the age specific death probability between the fifth and sixth National Population Census data, assuming a linear interpolation. With the estimated death probability in each age group, the 2011 age‐specific population by gender, area, and age were derived based on the existing population statistics.
Statistical analysis
The crude incidence and mortality rates of esophageal cancer were calculated by area, gender, and age group using data from 177 cancer registries. Using the cancer registration statistics in each strata (by age group, gender, and area), we calculated the estimated numbers of new cases and deaths of esophageal cancer using the respective 2011 Chinese population. The overall cancer incidence and mortality rates were estimated. The age‐standardized incidence and mortality rates were based on the 2000 standard Chinese population and world Segi's population, and expressed per 100 000 population. The cumulative risk of developing or dying from cancer before the age of 75 (in the absence of competing causes of death), was calculated and presented as a percentage.
Results
Detailed quality control indicators of esophageal cancer for the 177 cancer registries are shown in Table 1. The mortality/incidence (M/I) ratio for all qualified registries was 0.76 (0.81 in urban and 0.73 in rural areas). The percentage of morphologic verification (MV) was 80.02% overall (78.37% for urban and 81.05% for rural areas). The percentage of death certificate only (DCO) was 2.09% overall (2.34% in urban and 1.94% in rural areas). The percentage of uncertified basis of diagnosis (UB%) was 0.16%.
Table 1.
Quality control indicators of esophageal cancer in 177 Chinese cancer registries
| Areas | Gender | M/I | MV% | DCO% | UB% |
|---|---|---|---|---|---|
| ALL | Both | 0.76 | 80.02 | 2.09 | 0.16 |
| Male | 0.76 | 80.25 | 2.08 | 0.16 | |
| Female | 0.76 | 79.46 | 2.13 | 0.16 | |
| Urban | Both | 0.81 | 78.37 | 2.34 | 0.26 |
| Male | 0.80 | 78.92 | 2.29 | 0.25 | |
| Female | 0.82 | 76.82 | 2.47 | 0.28 | |
| Rural | Both | 0.73 | 81.05 | 1.94 | 0.10 |
| Male | 0.74 | 81.15 | 1.93 | 0.10 | |
| Female | 0.73 | 80.84 | 1.96 | 0.09 |
DCO, death certificate only; M/I, mortality/incidence; M/V, morphologic verification; UB, uncertified basis.
Based on data from 177 population based cancer registries from 28 provinces, we calculated the crude incidence and mortality rates in cancer registration areas by age, gender, and area. The age‐specific esophageal cancer incidence and mortality rates are shown in Table 2 and Figure 1. The age‐specific incidence and mortality rates were relatively low up to 40 years of age in each area and increased dramatically after age 40. The incidence rates for men in urban areas reached a peak at 85+ years, whereas for women in urban areas and subjects in rural areas, the incidence rates were highest at 80− years. The mortality rates were highest for subjects aged 80− or 85+ years.
Table 2.
Age specific incidence and mortality rates of esophageal cancer by area and gender in cancer registries (per 100 000)
| Age group | Incidence | Mortality | ||||||
|---|---|---|---|---|---|---|---|---|
| Urban male | Urban female | Rural male | Rural female | Urban male | Urban female | Rural male | Rural female | |
| 0 | 0.00 | 0.00 | 0.23 | 0.00 | 0.00 | 0.00 | 0.23 | 0.00 |
| 1 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 5 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.05 | 0.00 | 0.00 |
| 10 | 0.00 | 0.00 | 0.04 | 0.00 | 0.00 | 0.00 | 0.04 | 0.00 |
| 15 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| 20 | 0.08 | 0.03 | 0.12 | 0.03 | 0.00 | 0.08 | 0.12 | 0.03 |
| 25 | 0.12 | 0.10 | 0.27 | 0.17 | 0.02 | 0.05 | 0.27 | 0.17 |
| 30 | 0.31 | 0.13 | 0.65 | 0.25 | 0.08 | 0.05 | 0.65 | 0.25 |
| 35 | 1.21 | 0.39 | 1.93 | 0.83 | 0.48 | 0.19 | 1.93 | 0.83 |
| 40 | 3.46 | 0.90 | 7.17 | 3.04 | 1.95 | 0.51 | 7.17 | 3.04 |
| 45 | 12.21 | 2.31 | 22.79 | 7.08 | 7.80 | 1.19 | 22.79 | 7.08 |
| 50 | 25.81 | 4.02 | 49.56 | 15.71 | 18.13 | 2.21 | 49.56 | 15.71 |
| 55 | 47.32 | 10.84 | 106.55 | 37.06 | 32.29 | 5.65 | 106.55 | 37.06 |
| 60 | 75.92 | 20.25 | 167.56 | 70.17 | 49.65 | 12.29 | 167.56 | 70.17 |
| 65 | 96.80 | 35.14 | 195.13 | 90.78 | 72.94 | 26.54 | 195.13 | 90.78 |
| 70 | 111.11 | 40.80 | 241.01 | 117.51 | 95.08 | 31.97 | 241.01 | 117.51 |
| 75 | 118.22 | 55.22 | 267.98 | 135.58 | 115.40 | 51.78 | 267.98 | 135.58 |
| 80 | 129.32 | 59.63 | 280.25 | 149.95 | 141.29 | 68.48 | 280.25 | 149.95 |
| 85 | 132.10 | 57.52 | 259.36 | 118.61 | 173.23 | 75.24 | 259.36 | 118.61 |
Figure 1.
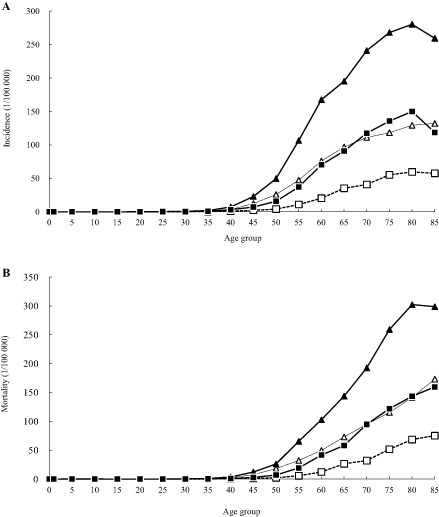
(a) 2011 age‐specific esophageal cancer incidence in China. (b) 2011 age‐specific esophageal cancer mortality in China.  , Urban male;
, Urban male;  , Urban female;
, Urban female;  , Rural male;
, Rural male;  , Rural female.
, Rural female.
Using age‐specific incidence and mortality rates by area and gender in cancer registration areas, we estimated esophageal cancer incidence in China using 2011 Chinese population data in each strata. As shown in Table 3, in 2011, a total of 291 238 new cases of esophageal cancer occurred, with crude rates of 21.62/100 000. The estimated crude incidence rate for men was 29.76/100 000, which was higher than for women at 13.05/100 000. The crude incidence rates were 13.46/100 000 in urban and 30.19/100 000 in rural areas. The age‐standardized incidence rates by China (ASRcn) and world population (ASRwld) were 15.58/100 000 and 15.83/100 000, respectively. The ASRcn in urban areas was 9.57/100 000, which was much lower than in rural areas (22.06/100 000). The cumulative rate for subjects (0–74) developing esophageal cancer was 2.01%. The truncated age‐standardized rate (TASR) (age 35–64) using world standard population was 23.87/100 000.
Table 3.
Estimated esophageal cancer incidence in China in 2011
| Areas | Gender | Number of cases | Crude rate | ASRcn | ASRwld | Cumulative rate | TASR |
|---|---|---|---|---|---|---|---|
| (1/105) | (1/105) | (1/105) | 0–74 (%) | 35–64 (1/105) | |||
| All | Both | 291 238 | 21.62 | 15.58 | 15.83 | 2.01 | 23.87 |
| Male | 205 560 | 29.76 | 22.47 | 22.90 | 2.90 | 35.78 | |
| Female | 85 678 | 13.05 | 8.85 | 8.94 | 1.12 | 11.61 | |
| Urban | Both | 92 996 | 13.46 | 9.57 | 9.71 | 1.22 | 14.49 |
| Male | 69 386 | 19.68 | 14.62 | 14.88 | 1.87 | 23.33 | |
| Female | 23 610 | 6.98 | 4.67 | 4.69 | 0.57 | 5.36 | |
| Rural | Both | 198 242 | 30.19 | 22.06 | 22.41 | 2.85 | 34.22 |
| Male | 136 174 | 40.28 | 30.93 | 31.49 | 3.96 | 49.54 | |
| Female | 62 068 | 19.49 | 13.39 | 13.54 | 1.71 | 18.49 |
ASRcn, age‐standardized rate (using China standard population, 2000); ASRwld, age‐standardized rate (using world standard population); TASR, truncated age‐standardized rate (using world standard population).
The estimated esophageal cancer mortality rates in China are shown in Table 4. In 2011, 218 957 esophageal cancer deaths occurred, with a crude mortality rate of 16.25/100 000. The estimated crude mortality rate was higher for men (22.38/100 000) than for women (9.80/100 000) and was lower in urban (10.67/100 000) than in rural (22.12/100 000) areas. The ASRcn and ASRwld mortality rates were 11.51/100 000 and 11.62/100 000, respectively. The ASRcn in urban areas was 7.46/100 000, which was lower than in rural areas, at 15.85/100 000. The cumulative rate (0–74) of death from esophageal cancer was 1.40%. The TASR (age 35–64) using world standard population was 14.26/100 000.
Table 4.
Estimated esophageal cancer mortality in China in 2011
| Areas | Gender | Number of cases | Crude rate | ASRcn | ASRwld | Cumulative rate | TASR |
|---|---|---|---|---|---|---|---|
| (1/105) | (1/105) | (1/105) | 0–74 (%) | 35–64 (1/105) | |||
| All | Both | 218 957 | 16.25 | 11.51 | 11.62 | 1.40 | 14.26 |
| Male | 154 587 | 22.38 | 16.86 | 17.05 | 2.06 | 22.02 | |
| Female | 64 371 | 9.80 | 6.38 | 6.42 | 0.75 | 6.26 | |
| Urban | Both | 73 724 | 10.67 | 7.46 | 7.53 | 0.89 | 9.36 |
| Male | 54 618 | 15.49 | 11.46 | 11.62 | 1.39 | 15.48 | |
| Female | 19 106 | 5.65 | 3.63 | 3.63 | 0.40 | 3.04 | |
| Rural | Both | 145 233 | 22.12 | 15.85 | 15.98 | 1.94 | 19.58 |
| Male | 99 969 | 29.57 | 22.65 | 22.84 | 2.74 | 29.14 | |
| Female | 45 264 | 14.21 | 9.35 | 9.41 | 1.12 | 9.77 |
ASRcn, age‐standardized rate (using China standard population, 2000); ASRwld, age‐standardized rate (using world standard population); TASR, truncated age‐standardized rate (using world standard population).
Using data with detailed pathological information, we analyzed the pathological types of esophageal cancer in China. As shown in Figure 2, ESCC was the most common type, accounting for 88.84% of all esophageal cancer, while EAC only accounted for 8.39%.
Figure 2.
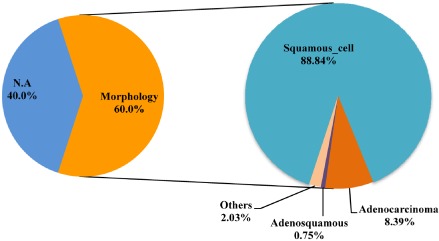
Pathological types of esophageal cancer in China.
Discussion
In the present study, we used a data from 177 qualified population‐based cancer registries to estimate the overall esophageal cancer statistics in China in 2011. The crude incidence and mortality rates for esophageal cancer were 21.62/100 000 and 16.25/100 000, respectively. The age‐standardized incidence and mortality rates by world population were 15.83/100 000 and 11.62/100 000, respectively. Our results indicated that both incidence and mortality rates of esophageal cancer were higher in rural than in urban areas. Age‐specific esophageal cancer incidence and mortality rates increased with age. ESCC was the most common pathological type of esophageal cancer in China. With 291 238 cases and 218 957 new cancer deaths in 2011, esophageal cancer remains a common disease in China, especially in rural areas and in men.
The geographical variations of incidence and mortality rates of esophageal cancer in China shown in our study were similar to previous reports.6 Both incidence and mortality rates of esophageal cancer in rural areas were about twice the rate in urban areas. Such disparities may be a result of different socioeconomic status and lifestyle. The two major histological types of esophageal cancer include EAC and ESCC. Both ESCC and EAC share common risk factors, such as cigarette smoking. The risk factors of ESCC include diets low in fruit and vegetables, high in meat, moldy food, smoking, and drinking.7 Population‐attributable risks of smoking, obesity, history of gastroesophageal reflux, and low fruit and vegetable consumption accounted for about 79% of EAC cases. In China, ESCC was the predominant histological type of the disease, which differed from the situation in the United States.8, 9 Differences in the rates of subtypes of esophageal cancer may reflect different lifestyles and genetic backgrounds.10, 11 Our previous results showed that esophageal cancer incidence rates have recently declined in China, mainly resulting from changes in dietary patterns and food preservation methods.4
The prognosis for esophageal cancer is dismal in China; the relative survival rates are about 20%.12 The earlier esophageal cancer is detected, the better chance a person has of surviving five years after diagnosis. Five‐year survival of localized esophageal cancer reaches 40% in the United States, whereas for distant disease, five‐year survival is only 3.8%.13 Population screening with endoscopy and biopsy is effective in the early detection of cancer, and has been conducted in areas of China with a high‐risk of esophageal cancer incidence, such as Cixian and Linzhou.14
Our study provided estimated esophageal cancer statistics using updated population‐based data from 177 qualified cancer registries. This data may be useful for basic, clinical, and translational research on esophageal cancer. With the increasing emphasis on cancer surveillance from the Chinese government, the quality of cancer registration data in China will continue to improve.
Disclosure
No authors report any conflict of interest.
Acknowledgment
We gratefully acknowledged the cooperation of the 177 population‐based cancer registries in providing cancer statistics, data collection, sorting, verification, and database creation. The authors assume full responsibility for analyses and interpretation of these data.
References
- 1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin 2015; 65: 87–108. [DOI] [PubMed] [Google Scholar]
- 2. Ferlay J, Soerjomataram I, Dikshit R et al Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015; 136: E359–386. [DOI] [PubMed] [Google Scholar]
- 3. Chen W, Zheng R, Zeng H, Zhang S, He J. Annual report on status of cancer in China, 2011. Chin J Cancer Res 2015; 27: 2–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zeng HM, Zheng RS, Zhang SW et al [Analysis and prediction of esophageal cancer incidence trend in China]. Zhonghua Yu Fang Yi Xue Za Zhi 2012; 46: 593–597. (In Chinese.) [PubMed] [Google Scholar]
- 5. National Bureau of Statistics of China . Tabulation on the 2010 population census of the People's Republic of China. 2015. [Cited 5 Mar 2015.] Available from URL: http://data.stats.gov.cn.
- 6. Chen W, He Y, Zheng R et al Esophageal cancer incidence and mortality in China, 2009. J Thorac Dis 2013; 5: 19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Freedman ND, Abnet CC, Leitzmann MF et al A prospective study of tobacco, alcohol, and the risk of esophageal and gastric cancer subtypes. Am J Epidemiol 2007; 165: 1424–1433. [DOI] [PubMed] [Google Scholar]
- 8. González L, Magno P, Ortiz AP et al Esophageal cancer incidence rates by histological type and overall: Puerto Rico versus the United States Surveillance, Epidemiology, and End Results population, 1992–2005. Cancer Epidemiol 2013; 37: 5–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Trivers KF, Sabatino SA, Stewart SL. Trends in esophageal cancer incidence by histology, United States, 1998–2003. Int J Cancer 2008; 123: 1422–1428. [DOI] [PubMed] [Google Scholar]
- 10. Engel LS, Chow WH, Vaughan TL et al Population attributable risks of esophageal and gastric cancers. J Natl Cancer Inst 2003; 95: 1404–1413. [DOI] [PubMed] [Google Scholar]
- 11. Liu S, Dai JY, Yao L et al Esophageal adenocarcinoma and its rare association with Barrett's esophagus in Henan, China. (Published erratum appears in PLoS ONE 2015; 10: e0127135) PLoS ONE 2014; 9: e110348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zeng H, Zheng R, Guo Y et al Cancer survival in China, 2003–2005: A population‐based study. Int J Cancer 2015; 136: 1921–1930. [DOI] [PubMed] [Google Scholar]
- 13. Howlader N, Noone AM, Krapcho M. et al, eds. SEER Cancer Statistics Review, 1975–2011 . National Cancer Institute, Bethesda, MD. [Cited 15 Mar 2015.] Available from URL: http://seer.cancer.gov/csr/1975_2011/; based on November 2013 SEER data submission, posted to the SEER web site, April 2014.
- 14. Lu XJ, Chen ZF, Guo CL et al Endoscopic survey of esophageal cancer in a high‐risk area of China. World J Gastroenterol 2004; 10: 2931–2935. [DOI] [PMC free article] [PubMed] [Google Scholar]


