Abstract
Study Objectives:
To evaluate the burden of narcolepsy--with respect to psychiatric comorbidities, Health-Related Quality of Life (HRQoL), direct costs for healthcare resource utilization, and indirect costs for reported work loss–through comparison of patients to matched controls.
Methods:
This analysis was conducted on data from the 2011, 2012, and 2013 US National Health and Wellness Survey (NHWS; 2011 NHWS n = 75,000, 2012 NHWS n = 71,157, and 2013 NHWS n = 75,000). Patients who reported a narcolepsy diagnosis (n = 437) were matched 1:2 with controls (n = 874) on age, sex, race/ethnicity, marital status, education, household income, body mass index, smoking status, alcohol use, exercise, and physical comorbidity. Chi-square tests and one-way analyses of variance were used to assess whether the narcolepsy and control groups differed on psychiatric comorbidities, HRQoL, labor force participation, work productivity, and healthcare resource utilization.
Results:
Patients with narcolepsy, in comparison to matched controls, reported substantially (two to four times) greater psychiatric comorbidity, HRQoL impairment, prevalence of long-term disability, absenteeism, and presenteeism, and greater resource use in the past 6 mo as indicated by higher mean number of hospitalizations, emergency department visits, traditional healthcare professional visits, neurologist visits, and psychiatrist visits (each p < 0.05).
Conclusions:
These population-based data suggest that a narcolepsy diagnosis is associated with substantial adverse impact on mental health, HRQoL, and key economic burdens that include work impairment, resource use, and both direct and indirect costs. Although this study is cross-sectional, the results highlight the magnitude of the potential opportunity to improve mental health, lower costs, and augment work-related productivity through effective assessment and treatment of narcolepsy.
Citation:
Flores NM, Villa KF, Black J, Chervin RD, Witt EA. The humanistic and economic burden of narcolepsy. J Clin Sleep Med 2016;12(3):401–407.
Keywords: burden of illness, costs of illness, mental disorders, narcolepsy, quality of life
INTRODUCTION
Narcolepsy is a chronic disorder characterized by excessive daytime sleepiness that can be associated with significant effect on quality of life and disability. Narcolepsy is also associated with obesity, nighttime sleep disturbances, and functional impairment.1,2 Narcolepsy typically presents during teenage years or young adulthood and persists through adulthood. Prevalence estimates range between 25 and 50 per 100,000 people.3,4
Numerous studies have found health-related quality of life (HRQoL) among narcolepsy patients to be significantly impaired in comparison with healthy controls or the general population.5–14 Patients are impaired on several domains of HRQoL including mood, psychopathology, and other areas such as marital and work problems.5–14 Narcolepsy has been associated with a negative impact on work productivity including increased unemployment,15 early retirement,16 accidents at work,5 welfare enrollment,11 time missed from work, general impairment at work,8 and lower wages.11
Healthcare resource use in narcolepsy is high and has been associated with approximately two times greater resource use and cost than observed among matched controls.17 Inpatient, outpatient, emergency department, and prescription costs have all been found to be significantly higher among narcolepsy patients compared with non-narcolepsy controls.11,15–17
BRIEF SUMMARY
Current Knowledge/Study Rationale: Although the burden of narcolepsy has been documented, larger scale studies have yet to examine health outcomes of interest. Therefore, the goal of the current study was to evaluate the burden of narcolepsy using respondents from a large general health survey to compare those with narcolepsy to matched controls with regard to the following outcomes: mental health, health-related quality of life (HRQoL), work productivity loss, resource use, and direct and indirect costs.
Study Impact: The results suggest that there is a substantial humanistic and economic burden associated with narcolepsy as evidenced by higher observed rates of psychiatric comorbidities, lower HRQoL, greater work-productivity loss, greater healthcare resource use, and greater associated direct and indirect costs among those reporting a narcolepsy diagnosis compared with matched controls. The large adverse impact of narcolepsy observed in this study suggests high unmet need in this population.
Although the burden of narcolepsy has been well-documented across various health outcomes of interest, including psychiatric disorders, few studies have examined this burden in relation to its societal costs, from work productivity loss and healthcare resource use.11,15,17–22 Accordingly, larger-scale evaluations are required to better characterize the prevalence of these costly and impactful psychiatric conditions in regards to HRQoL, direct costs, and direct costs among patients with narcolepsy.
The aim of the current study, therefore, was to evaluate the burden of narcolepsy by comparing patients with narcolepsy to matched controls from a large general health survey, with a focus on several key outcomes: mental health, HRQoL, direct costs based on measures of healthcare resource utilization, and indirect costs based on reported work productivity loss.
METHODS
Source and Sample
This analysis was conducted on data from the 2011, 2012, and 2013 US National Health and Wellness Survey (2011 NHWS n = 75,000, 2012 NHWS n = 71,157, and 2013 NHWS n = 75,000). Respondents who took the survey more than once during those 3 y were only counted once and their most recent responses used yielding n = 176,093 unique respondents. The NHWS is a self-administered, Internet-based survey of US adults (aged 18 y or older). NHWS participants are selected from an opt-in Internet panel maintained by Lightspeed Research. A stratified random sample (with strata by sex and age) was implemented to ensure that the demographic composition of the sample is identical to that of the corresponding adult population as measured by the US Census. Previous research has revealed that the NHWS data compares favorably with estimates of US demographic composition according to the census as well as estimates from other sources such as the National Health Interview Survey.23–25 All participants were required to read and write English, be at least 18 y of age or older, and provide informed consent to participate. The study protocol was approved a priori by the Essex Institutional Review Board (Lebanon, NJ, USA).
The focal group for analyses were those individuals who reported ever having been diagnosed with narcolepsy by a physician (n = 437). To evaluate baseline differences between those with a narcolepsy diagnosis and those without (n = 175,656), comparisons were examined for demographics and health characteristics. However, for health outcome comparisons and psychiatric comorbidities, a comparison group was created via propensity matching (n = 837) from the remaining sample of respondents in whom narcolepsy was not diagnosed.
Measures
Independent Variable
NARCOLEPSY DIAGNOSIS: Participants who reported a narcolepsy diagnosis were matched to those who did not via propensity score matching using a 2:1 control to target matching algorithm (see Statistical Analyses). This resulted in a matched control group (n = 874).
Covariates in Propensity Score Model
DEMOGRAPHIC AND HEALTH CHARACTERISTICS: The following demographic and health characteristic variables were first examined between those with and without a narcolepsy diagnosis and then included as covariates for propensity score matching: age, sex, race/ethnicity, marital status, education, income, body mass index (BMI), smoking status, pregnancy status, whether or not they currently drink alcohol, exercise status, and the Charlson Comorbidity Index (CCI).26
Dependent Variables
COMORBIDITIES: Psychiatric comorbidities were also examined. These included self-reported diagnoses of depression, bipolar disorder, anxiety disorder, generalized anxiety disorder, posttraumatic stress disorder, social anxiety disorder, panic disorder, phobia disorder, obsessive compulsive disorder, and total diagnosed anxiety.
HEALTH-RELATED QUALITY OF LIFE: HRQoL was measured via the Medical Outcomes Study Short Form-12 for 2011 NHWS and Medical Outcomes Study Short Form-36 for 2012 and 2013 NHWS. Specifically, the mental component summary (MCS) and physical component summary scores (PCS) and the Health Utilities score were used; both SF versions yield comparable scores.27–30
LABOR FORCE PARTICIPATION, DISABILITY STATUS, AND WORK PRODUCTIVITY LOSS: Labor force participation (employed full time, employed part-time, self-employed, or not employed) was measured via one item. Additionally, patients were categorized into one of three disability statuses (long-term, short-term, and not disabled) based on one question. Work productivity loss and activity impairment were measured via the Work Productivity and Activity Impairment-General Health scale (WPAI-GH).31 The WPAI examines the following constructs: presenteeism, absenteeism, overall work impairment, and activity impairment over the past 7 d. Presenteeism measures the degree to which one's work productivity is affected by health problems, which is then converted into a percentage of time one's productivity is impaired while working. Absenteeism measures the amount of time one misses work due to health problems, which is then converted to a percentage of work missed due to health problems. Overall work impairment is a combination of presenteeism and absenteeism which measures the percentage of time one's work productivity is impaired overall. Last, activity impairment measures the percentage of time one's abilty to perform daily activities, outside of work, is impaired.
ESTIMATED DIRECT AND INDIRECT COSTS: Estimated healthcare resource use costs were calculated by applying unit costs extrapolated from the Medical Expenditure Panel Survey (MEPS) and the Bureau of Labor Statistics (BLS) to Healthcare Resource Use variables from the NHWS. Direct (emergency department visits, hospitalizations, healthcare professional visits) and indirect costs (absenteeism and presenteeism for employed participants only) were calculated separately and totaled.
Statistical Analyses
Descriptive analyses were conducted to describe the sociodemographic and health characteristics of the total sample and the narcolepsy and control groups. Bivariate analyses (chi-square tests for categorical variables and t-tests for continuous variables) were conducted to assess whether patients with or without a narcolepsy diagnosis differed significantly on any sociodemographic or health characteristic variables.
Propensity score matching was carried out to match the narcolepsy diagnosis group to a group of control individuals. Specifically, all covariates identified a priori (age, sex, race/ ethnicity, marital status, education, household income, BMI, smoking status, alcohol use, exercise status, and CCI) were entered into a logistic regression predicting narcolepsy diagnosis. The predicted scores for each individual (ranging from 0–1; i.e., the propensity score) were then saved. People in the two groups were paired 2:1 (control to case) by propensity score using a greedy matching algorithm. This resulted in a matched group of those without a narcolepsy diagnosis (n = 874). Bivariate analyses (chi-square tests for categorical variables and t-tests for continuous variables) were then conducted to assess whether the narcolepsy and control groups differed significantly on the psychiatric comorbidities described in the Measures section, or on HRQoL, work force participation, disability status, work productivity, or healthcare resource utilization.
An examination of the matched variables (e.g., BMI) post-match revealed a successful propensity score match. This was determined by examining measures of standardized bias for each covariate prematch and postmatch. A “good” match is defined as one in which all measures of standardized bias are below 0.25. Prematch, all measures except smoking status, BMI, and CCI were below this criterion. Postmatch, all measures were below 0.15, indicating a successful match.
All analyses were performed using IBM SPSS Statistics version 20. The level of significance was p < 0.05.
RESULTS
Prematch Comparisons
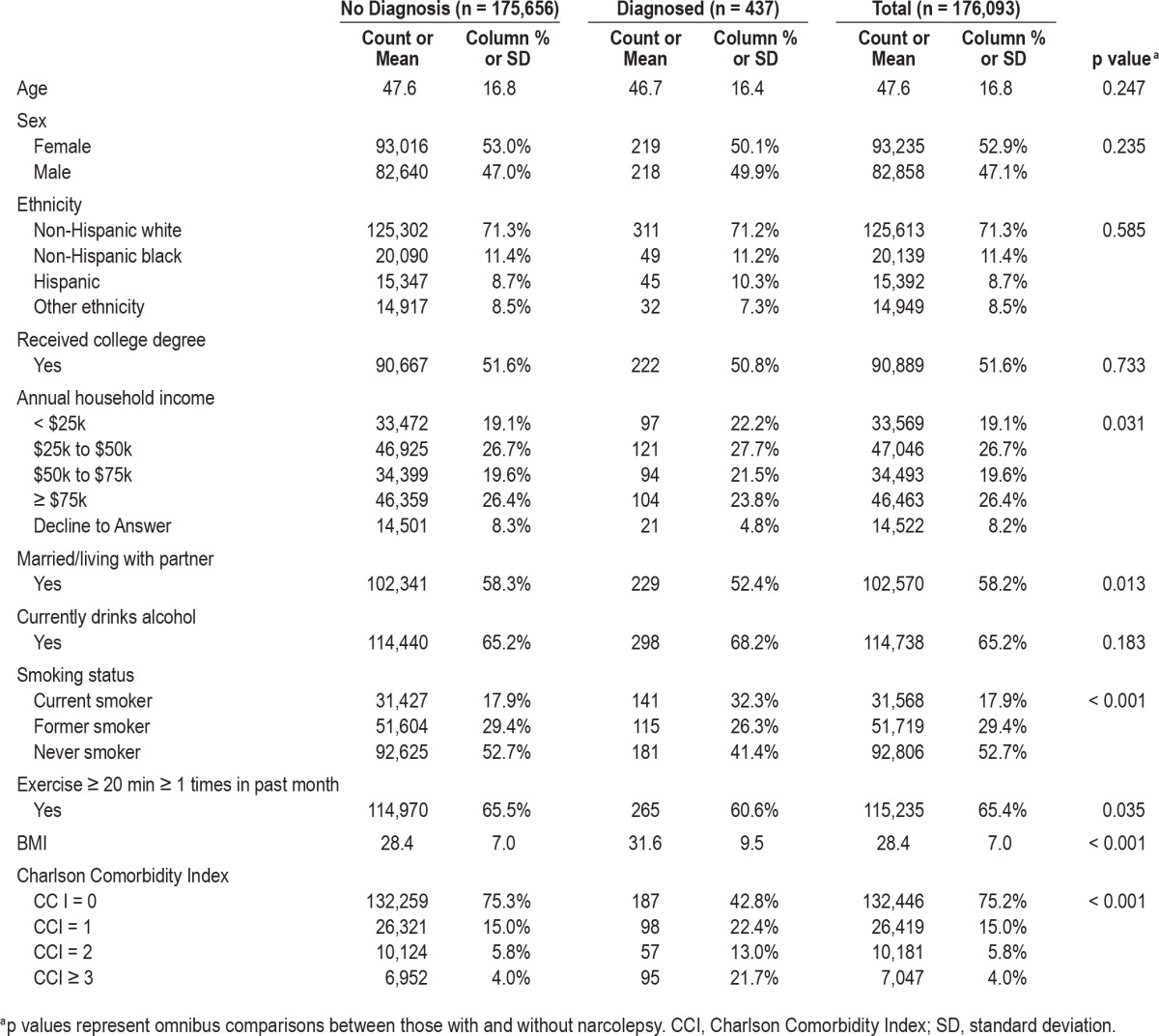
Prior to propensity score matching analyses, all potential covariates (demographics and health characteristics) were examined for bivariate differences between subjects with and without narcolepsy. Results suggested that marital status, household income, smoking status, exercise behavior, and BMI category differed significantly between groups (p < 0.05; see Table 1). Notably, the groups also differed significantly on comorbidity burden (CCI), with more than five times the proportion of narcolepsy patients, in comparison to controls, reporting three or more CCI comorbidities (p < 0.001).
Table 1.
Demographics and health characteristics for overall sample by narcolepsy diagnosis.
Postmatch Comparisons
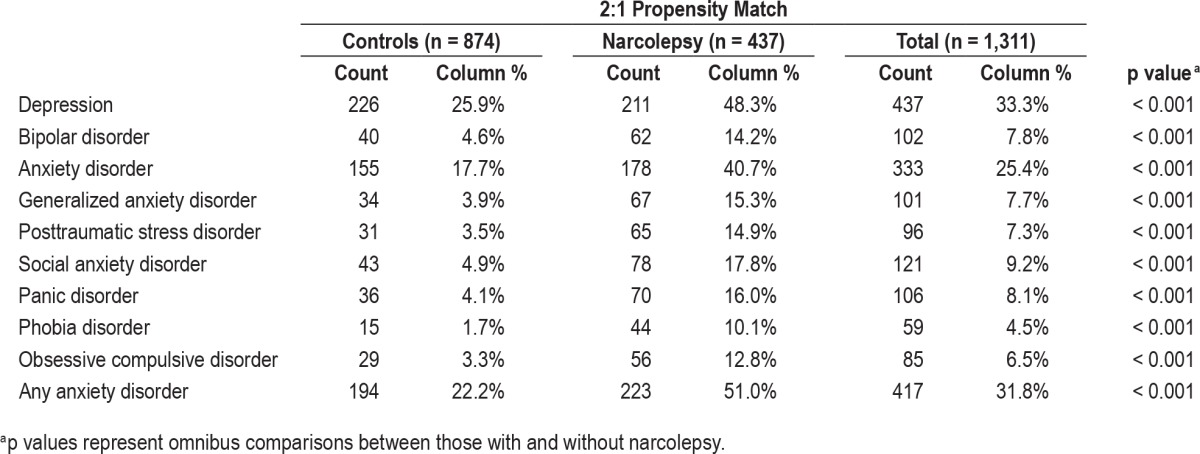
The matched groups differed substantially on every psychiatric comorbidity examined (p < 0.001; see Table 2). Notably, narcolepsy patients in comparison to nonnarcolepsy patients were nearly twice as likely to report depression, more than twice as likely to report an anxiety disorder, and nearly three times as likely to report bipolar disorder (each p < 0.001).
Table 2.
Diagnosis of psychiatric comorbidities among subjects with narcolepsy and matched controls.
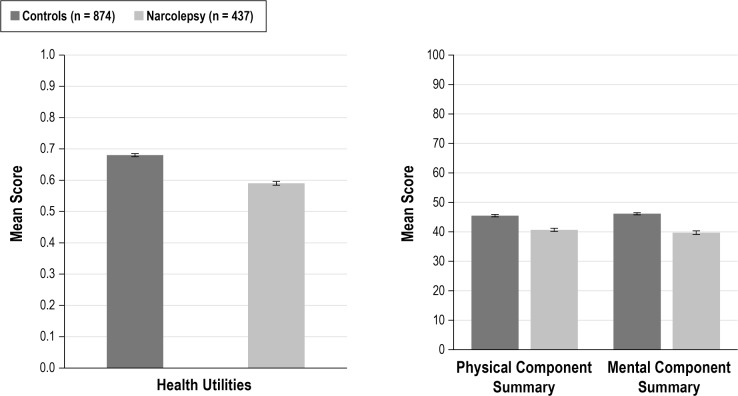
The narcolepsy group in comparison to the matched controls reported substantially lower HRQoL (see Figure 1). Specifically, the narcolepsy group reported significantly lower mean health utility, MCS, and PCS scores (each p < 0.001).
Figure 1. Health-related quality of life for those diagnosed with narcolepsy and matched controls.
Error bars represent standard errors. All comparisons between subjects with and without narcolepsy, for each outcome, are significant at the p < 0.001 level.
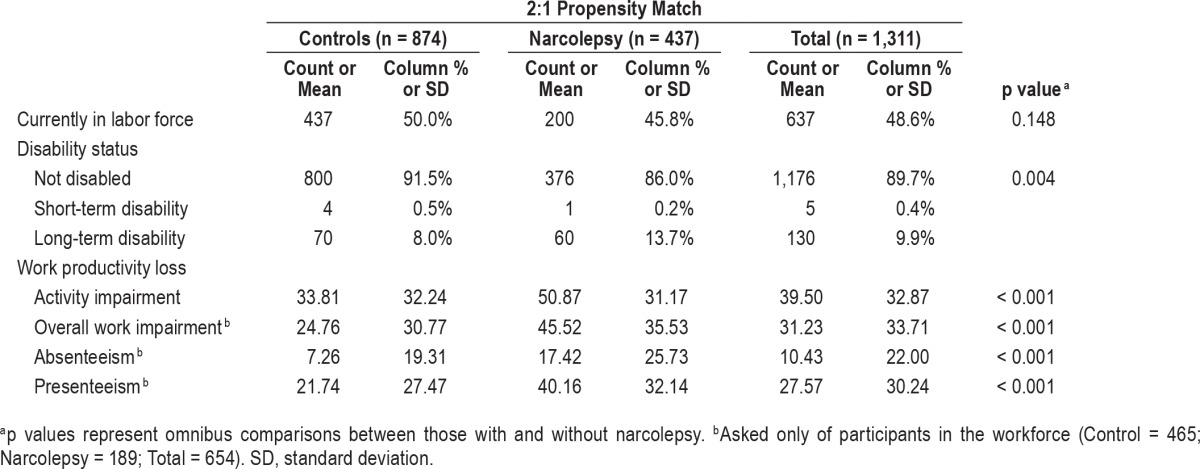
Work productivity loss was substantially higher among narcolepsy patients than their control peers (see Table 3). In particular, narcolepsy patients reported more than 70% greater long-term disability (p = 0.004). Moreover, among employed individuals, narcolepsy patients in comparison to controls reported greater mean percentages of absenteeism, presenteeism, overall work impairment, and activity impairment (all p < 0.001).
Table 3.
Labor force participation, disability status, and work productivity loss for those with a narcolepsy diagnosis and matched controls.
Healthcare resource use was also substantially greater among narcolepsy patients than matched controls (see Table S1 supplemental material). Specifically, in the past 6 mo the narcolepsy group in comparison to matched controls reported, on average, two to three times more hospitalizations, emergency deparment visits, traditional healthcare professional visits, neurologist visits, and psychiatrist visits (all p ≤ 0.001).
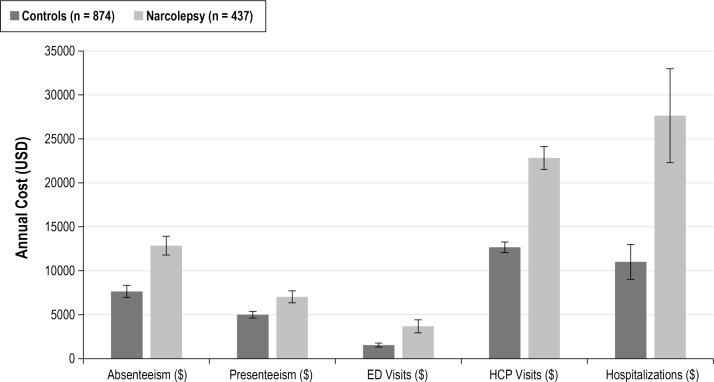
Cost multipliers were applied to the aforementioned work productivity loss and healthcare resource use data to derive indirect and direct societal costs of narcolepsy (see Figure 2). The narcolepsy group in comparison to matched controls had significantly higher costs associated with absenteeism ($12,839 versus $7,631), presenteeism ($7,013 versus $4,987), emergency department ($3,667 versus $1,543), healthcare professional ($22,828 versus $12,667), and hospitalization ($27,642 versus $10,998) (each p < 0.001).
Figure 2. Annual direct and indirect costs for those with a diagnosis of narcolepsy and matched controls.
Error bars represent standard errors. Absenteeism and Presenteeism costs were only calculated for participants in the workforce (Control = 465; Narcolepsy = 189; Total = 654). All comparisons between subjects with and without narcolepsy, for each outcome, are significant at the p < 0.001 level.
DISCUSSION
Data from this large, population-based comparison of patients who report a diagnosis of narcolepsy and matched controls, suggests that narcolepsy is associated with a serious and costly impact on a range of patient outcomes. Those individuals with a diagnosis of narcolepsy had greater psychiatric comorbidity, lower HRQoL, higher activity and work impairment, higher likelihood of long-term disability, and higher resource use. Higher resource use and higher work productivity loss, in turn, led to higher direct and indirect costs for the narcolepsy cohort compared to controls. The magnitude of psychiatric comorbidities associated with narcolepsy was substantial. The proportion of narcolepsy patients who also reported depression, bipolar disorder, or an anxiety disorder was multiples larger than the proportion of controls who reported those disorders, respectively—even after matching narcolepsy patients and controls with similar physical comorbidity status. Strengths of this study include use of a large sample representative of the US population and propensity score matching of the study groups, which adjusted for physical morbidity and various sociodemographic factors that otherwise might have biased the results. Overall, the results highlight the potential impact that narcolepsy may have on HRQoL, medical costs, and work-place-related costs.
The current study corroborates previous reports that narcolepsy may be associated with psychiatric comorbidities such as depression and anxiety.18–22,32,33 However, the current study demonstrates consistent and substantially higher prevalence of several psychiatric disorders among narcolepsy patients compared to matched controls. In addition, this study corroborates previous findings that narcolepsy is strongly associated with impairment in physical and mental HRQoL.5–10,12–14
To our knowledge, few prior studies have reported the societal costs that arise from the work productivity loss and healthcare resource use associated with narcolepsy in the United States.17 Black et al.17 did find that compared to matched controls, patients in whom narcolepsy was diagnosed had approximately twofold higher annual rates of inpatient admissions, emergency department visits (without admission), hospital outpatient visits, other outpatient services, and physician visits (all p < 0.001). The current study found similar differences in physician visits and number of inpatient and outpatient admissions. Additionally, our findings suggest that the indirect costs related to work productivity loss are substantially higher among narcolepsy patients than their peers in the United States. As narcolepsy patients were matched to controls with similar sociodemographic and health variables, the current results suggest that narcolepsy itself may be a significant source of excess burden on the health-care system and society at large.
The current cross-sectional data preclude assessment of whether narcolepsy preceded putative outcomes, and cannot prove cause-and-effect relationships. It seems somewhat unlikely that greater provision of healthcare would increase the likelihood of narcolepsy diagnosis because of the relative seriousness and well-defined nature of this sleep disorder. However, the relationship of psychiatric comorbidities and narcolepsy may be more complicated and merit further investigation. Prior research suggests that narcolepsy patients commonly experience distress about their symptoms, which may be exacerbated by fear of accidents, concerns about their employment, and functional limitations such as difficulty obtaining driving licensure.5,34–39 It seems likely that in patients with a diagnosis of narcolepsy, psychiatric conditions develop at least partly in response to, or as a comorbid component of, the condition and, as a result, these patients are not fully functional at work and have reduced quality of life. Moreover, they seek medical help from general and specialist physicians, and are admitted to inpatient and outpatient services in response to their condition and its comorbidities.
Limitations
Because of the Internet-based method of sampling, the current study may not have included older or more ill individuals. As the study utilized matching to control for differences between the narcolepsy and control groups, mean differences would most likely not have been affected, but the descriptive statistics presented here may be more indicative of healthier patients than those who might have been sampled from the non–Internet-using population. However, the current study controlled for various potential confounders, including age and CCI, to ensure the validity of the relative differences between the study groups. Resource use questions were not condition specific and thus the observed differences in resource use cannot solely be attributed to narcolepsy. However, these analyses did control for general comorbidity via the CCI to account for variance attributable to conditions included in the CCI. Still, unmeasured and uncontrolled confounders may have biased the observed differences. Study measures were self-reported, some misclassification of disease status may have occurred, and diagnoses could not be confirmed independently for each of the individuals in this sizeable sample.
Implications and Future Directions
Current findings suggest that a diagnosis of narcolepsy could have substantial impact on productivity, resource use, and quality of life, as well as an increased risk for other comorbid health conditions identified in this analysis. Given these findings, future research should investigate how effective identification and treatment of narcolepsy could improve quality of life, reduce psychiatric burden, save substantial health system costs, and improve work-related outcomes.
DISCLOSURE STATEMENT
The study was funded by Jazz Pharmaceuticals. The study was conducted at Kantar Health. Dr. Flores and Dr. Witt are employees at Kantar Health. Jazz Pharmaceuticals, Inc. paid Kantar Health for access to survey data, analysis, and manuscript preparation. Ms. Villa and Dr. Black are full-time and part-time, respectively, employees of Jazz Pharmaceuticals, Inc. Dr. Chervin reports research funding and salary support from the NIH and University of Michigan; service on the Boards of Directors for the American Academy of Sleep Medicine and the International Pediatric Sleep Association; service as an editor for UpToDate; and consulting with Zansors. Jan-Samuel Wagner was a contributor on this manuscript and a paid consultant to Kantar Health (provided editorial support for manuscript preparation).
ABBREVIATIONS
- BLS
Bureau of Labor Statistics
- BMI
body mass index
- CCI
Charlson Comorbidity Index
- ED
emergency department
- HCP
healthcare professional
- HRQoL
health-related quality of life
- MCS
mental component summary
- MEPS
Medical Expenditure Panel Survey
- NHWS
National Health and Wellness Survey
- PCS
physical component summary
- SD
standard deviation
- WPAI-GH
Work Productivity and Activity Impairment-General Health
REFERENCES
- 1.Akintomide GS, Rickards H. Narcolepsy: a review. Neuropsychiatr Dis Treat. 2011;7:507–18. doi: 10.2147/NDT.S23624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sonka K, Kemlink D, Buskova J, et al. Obesity accompanies narcolepsy with cataplexy but not narcolepsy without cataplexy. Neuroendocrinol Lett. 2010;31:631–4. [PubMed] [Google Scholar]
- 3.Dauvilliers Y, Arnulf I, Mignot E. Narcolepsy with cataplexy. Lancet. 2007;369:499–511. doi: 10.1016/S0140-6736(07)60237-2. [DOI] [PubMed] [Google Scholar]
- 4.Longstreth WT, Jr, Koepsell TD, Ton TG, Hendrickson AF, van Belle G. The epidemiology of narcolepsy. Sleep. 2007;30:13–26. doi: 10.1093/sleep/30.1.13. [DOI] [PubMed] [Google Scholar]
- 5.Broughton WA, Broughton RJ. Psychosocial impact of narcolepsy. Sleep. 1994;17:S45–9. doi: 10.1093/sleep/17.suppl_8.s45. [DOI] [PubMed] [Google Scholar]
- 6.Daniels E, King MA, Smith IE, Shneerson JM. Health-related quality of life in narcolepsy. J Sleep Res. 2001;10:75–81. doi: 10.1046/j.1365-2869.2001.00234.x. [DOI] [PubMed] [Google Scholar]
- 7.David A, Constantino F, dos Santos JM, Paiva T. Health-related quality of life in Portuguese patients with narcolepsy. Sleep Med. 2012;13:273–7. doi: 10.1016/j.sleep.2011.06.021. [DOI] [PubMed] [Google Scholar]
- 8.Dean B, Aguilar D, Shapiro C, et al. Impaired health status, daily functioning, and work productivity in adults with excessive sleepiness. J Occup Environ Med. 2010;52:144–9. doi: 10.1097/JOM.0b013e3181c99505. [DOI] [PubMed] [Google Scholar]
- 9.Dodel R, Peter H, Spottke A, et al. Health-related quality of life in patients with narcolepsy. Sleep Med. 2007;8:733–41. doi: 10.1016/j.sleep.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Ervik S, Abdelnoor M, Heier MS, Ramberg M, Strand G. Health-related quality of life in narcolepsy. Acta Neurol Scand. 2006;114:198–204. doi: 10.1111/j.1600-0404.2006.00594.x. [DOI] [PubMed] [Google Scholar]
- 11.Jennum P, Ibsen R, Petersen ER, Knudsen S, Kjellberg J. Health, social, and economic consequences of narcolepsy: a controlled national study evaluating the societal effect on patients and their partners. Sleep Med. 2012;13:1086–93. doi: 10.1016/j.sleep.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Ozaki A, Inoue Y, Hayashida K, et al. Quality of life in patients with narcolepsy with cataplexy, narcolepsy without cataplexy, and idiopathic hypersomnia without long sleep time: comparison between patients on psychostimulants, drug-naive patients and the general Japanese population. Sleep Med. 2012;13:200–6. doi: 10.1016/j.sleep.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 13.Rovere H, Rossini S, Reimao R. Quality of life in patients with narcolepsy: a WHOQOL-bref study. Arquivos de neuro-psiquiatria. 2008;66:163–7. doi: 10.1590/s0004-282x2008000200004. [DOI] [PubMed] [Google Scholar]
- 14.Vignatelli L, Plazzi G, Peschechera F, Delaj L, D'Alessandro R. A 5-year prospective cohort study on health-related quality of life in patients with narcolepsy. Sleep Med. 2011;12:19–23. doi: 10.1016/j.sleep.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Jennum P, Knudsen S, Kjellberg J. The economic consequences of narcolepsy. J Clin Sleep Med. 2009;5:240–5. [PMC free article] [PubMed] [Google Scholar]
- 16.Dodel R, Peter H, Walbert T, et al. The socioeconomic impact of narcolepsy. Sleep. 2004;27:1123–8. doi: 10.1093/sleep/27.6.1123. [DOI] [PubMed] [Google Scholar]
- 17.Black J, Reaven NL, Funk SE, et al. The Burden of Narcolepsy Disease (BOND) study: health-care utilization and cost findings. Sleep Med. 2014;15:522–9. doi: 10.1016/j.sleep.2014.02.001. [DOI] [PubMed] [Google Scholar]
- 18.Bruck D. The impact of narcolepsy on psychological health and role behaviours: negative effects and comparisons with other illness groups. Sleep Med. 2001;2:437–46. doi: 10.1016/s1389-9457(01)00067-3. [DOI] [PubMed] [Google Scholar]
- 19.Dauvilliers Y, Lopez R, Ohayon M, Bayard S. Hypersomnia and depressive symptoms: methodological and clinical aspects. BMC Med. 2013;11:78. doi: 10.1186/1741-7015-11-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dauvilliers Y, Paquereau J, Bastuji H, Drouot X, Weil JS, Viot-Blanc V. Psychological health in central hypersomnias: the French Harmony study. J Neurol Neurosurg Psychiatry. 2009;80:636–41. doi: 10.1136/jnnp.2008.161588. [DOI] [PubMed] [Google Scholar]
- 21.Fortuyn HA, Lappenschaar MA, Furer JW, et al. Anxiety and mood disorders in narcolepsy: a case-control study. Gen Hosp Psychiatry. 2010;32:49–56. doi: 10.1016/j.genhosppsych.2009.08.007. [DOI] [PubMed] [Google Scholar]
- 22.Ohayon MM. Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med. 2013;14:488–492. doi: 10.1016/j.sleep.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 23.Bolge SC, Balkrishnan R, Kannan H, Seal B, Drake CL. Burden associated with chronic sleep maintenance insomnia characterized by nighttime awakenings among women with menopausal symptoms. Menopause (New York, NY) 2010;17:80–6. doi: 10.1097/gme.0b013e3181b4c286. [DOI] [PubMed] [Google Scholar]
- 24.DiBonaventura MD, Wagner JS, Yuan Y, L'Italien G, Langley P, Ray Kim W. Humanistic and economic impacts of hepatitis C infection in the United States. J Med Econ. 2010;13:709–18. doi: 10.3111/13696998.2010.535576. [DOI] [PubMed] [Google Scholar]
- 25.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital and health statistics Series 10, Data from the National Health Survey. 2012:1–207. [PubMed] [Google Scholar]
- 26.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 27.Kosinski M, Turner-Bowker D, Gandek B, Ware J. Lincoln, RI: Quality Metric; 2008. User's Manual for the SF-12v2 Health Survey. [Google Scholar]
- 28.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE., Jr . Lincoln, RI: Quality Metric; 2008. User's manual for the SF-36v2 health survey. [Google Scholar]
- 30.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Medical Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 31.Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics. 1993;4:353–65. doi: 10.2165/00019053-199304050-00006. [DOI] [PubMed] [Google Scholar]
- 32.Chabas D, Foulon C, Gonzalez J, et al. Eating disorder and metabolism in narcoleptic patients. Sleep. 2007;30:1267–73. doi: 10.1093/sleep/30.10.1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Costa e Silva JA. Sleep disorders in psychiatry. Metabolism. 2006;55:S40–4. doi: 10.1016/j.metabol.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 34.Chakravorty SS, Rye DB. Narcolepsy in the older adult: epidemiology, diagnosis and management. Drugs Aging. 2003;20:361–76. doi: 10.2165/00002512-200320050-00005. [DOI] [PubMed] [Google Scholar]
- 35.Ingravallo F, Vignatelli L, Brini M, et al. Medico-legal assessment of disability in narcolepsy: an interobserver reliability study. J Sleep Res. 2008;17:111–9. doi: 10.1111/j.1365-2869.2008.00630.x. [DOI] [PubMed] [Google Scholar]
- 36.Kotterba S, Mueller N, Leidag M, et al. Comparison of driving simulator performance and neuropsychological testing in narcolepsy. Clin Neurol Neurosurg. 2004;106:275–9. doi: 10.1016/j.clineuro.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 37.Pandi-Perumal SR, Verster JC, Kayumov L, et al. Sleep disorders, sleepiness and traffic safety: a public health menace. Braz J Med Biol Res. 2006;39:863–71. doi: 10.1590/s0100-879x2006000700003. [DOI] [PubMed] [Google Scholar]
- 38.Philip P, Sagaspe P, Lagarde E, et al. Sleep disorders and accidental risk in a large group of regular registered highway drivers. Sleep Med. 2010;11:973–9. doi: 10.1016/j.sleep.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 39.Smolensky MH, Di Milia L, Ohayon MM, Philip P. Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev. 2011;43:533–48. doi: 10.1016/j.aap.2009.12.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.