Abstract
Study Objectives:
The association of REM sleep without atonia (RSWA) as well as REM sleep behavior disorder (RBD) with the intake of selective serotonin reuptake inhibitors (SSRI) and selective norepinephrine reuptake inhibitors (SNRI) is well established. Our study objective was to determine the prevalence of RSWA and RBD among a group of sleep center patients taking SSRI and SNRI.
Methods:
A retrospective chart review was done at our tertiary sleep center, and 10,746 consecutive records from October 1, 2007, through October 31, 2013, were searched for SSRI and SNRI names using the Sleep Cataloguer Software.
Results:
The search resulted in 1,444 records, which were then reviewed for keywords of RSWA and RBD. The AASM scoring criteria were used to determine RSWA. Reports of 41 patients with known narcolepsy or α-synucleinopathies were excluded. The remaining records were mined for age, sex, presence of obstructive sleep apnea (OSA), type of antidepressant (SSRI or SNRI), and diagnosis for which antidepressant was prescribed. We used logistic regression analysis to adjust for age, OSA, and sex. Of the 1,444 participants on antidepressants, 176 (12.2%) had RSWA (all confirmed by the investigators) compared to 226 of the entire sleep lab population of 10,746 (2.1%), risk ratio (95% CI) 9.978 (8.149, 12.22). Seven of the 176 patients on antidepressants had RBD (0.48%) compared to 108 of 10,746 (1%), p = 0.005.
Conclusions:
SSRI and SNRI are associated with a higher prevalence of RSWA but not of RBD. This is independent of medication type.
Citation:
Lee K, Baron K, Soca R, Attarian H. The prevalence and characteristics of rem sleep without atonia (RSWA) in patients taking antidepressants. J Clin Sleep Med 2016;12(3):351–355.
Keywords: REM sleep behavior disorder, REM sleep without atonia, antidepressants, selective serotonin reuptake inhibitors
INTRODUCTION
REM sleep without atonia (RSWA) is a polysomnographic (PSG) finding characterized by increased tonic or phasic motor tone on the electromyography (EMG) channels during REM sleep.1 REM sleep behavior disorder (RBD) is characterized by the presence of RSWA and as well as a history of dream enacting behavior (DEB). Both RSWA and RBD can occur as idiopathic2 or secondary to narcolepsy,3 obstructive sleep apnea (OSA),4 α-synucleinopathies,5–8 and in the setting of certain medications such as antidepressants. RSWA is one of the hallmarks of RBD, and RBD can be a predictor for neurodegenerative disorders. RBD also can lead to significant injury to self and bed partner. Lastly the presence of RBD in Parkinson disease (PD) is associated with higher risk of cognitive decline.2
Selective serotonin reuptake inhibitors (SSRI) and selective norepinephrine (NE) reuptake inhibitors (SNRI) have been associated with RSWA and in some instances, RBD. About 15% of patients taking the SSRI fluoxetine in a sleep clinic population were shown to have RSWA.9 Although a few case reports have demonstrated resolution of RSWA and RBD upon discontinuation of fluoxetine,10–12 there is a suggestion from case-control studies that antidepressants may “unmask” RBD rather than cause it.13 This is all in the setting of increased usage of antidepressants in the United States, as the rate continues to rise with an increase of over 400% in the last two decades, now becoming the third most commonly prescribed medication class in all ages, and the most frequently used in the age group of 18–44.14
BRIEF SUMMARY
Current Knowledge/Study Rationale: Several case series have demonstrated a relationship between antidepressant use and RSWA. Since there is a dramatic increase in the number of antidepressant prescriptions we wanted to assess the prevalence of RSWA among patients taking antidepressant and the characteristics of those who are more likely to develop RSWA.
Study Impact: The knowledge that antidepressants increase the risk of RSWA by 10 fold will lead to more careful assessment of patients needing these medications. It will also increase awareness of the presence of this polysomnographic finding in patients who may otherwise have subtler symptoms.
The odds ratio of idiopathic RBD is 1.9 with antidepressant use,15 but the factors that predict the risk of developing RSWA while on SSRI/SNRI and its prevalence remains unknown. Our goal was to investigate the prevalence of RSWA in a large population of sleep disorder patients taking SSRI/SNRI medications, the prevalence of diagnosis of RBD in this population, as well as evaluate other parameters that may influence RSWA and RBD risk with antidepressants, such as the effect of age, presence of OSA, the specific type of SSRI/SNRI and the indication for usage. We hypothesized the risk of RSWA increases significantly with antidepressant use independent of age, sex, and OSA, and this may translate to higher prevalence of RBD.
METHODS
Subjects and Methods
This study was approved by the Northwestern University Institutional Review Board. A retrospective chart review was conducted using Sleep Cataloguer software on all PSG reports done at Northwestern University Sleep Lab from October 1, 2007, through October 31, 2013, using the following search terms “Celexa,” “Citalopram,” “Cymbalta,” “Duloxetine,” “Pristiq,” “Desvenlafaxine,” “Effexor,” “Venlafaxine,” “Escitalopram,” “Lexapro,” “Fluoxetine,” “Prozac,” “Sarafem,” “Floxyfral,” “Fluvoxamine,” “Luvox,” “Fevarin,” “Paroxetine,” “Paxil,” “Brisdelle,” “Sertraline,” “Zoloft.” All PSGs were conducted using the standard AASM montage of 6 EEG channels, chin and bilateral lower limb EMG channels, 2 EOG channels, pressure transducer, thermistor, effort belts, snore microphone, single channel ECG, and pulse oximetry.
Of a total number of 10,746 individual PSG records in that time period, 1,485 were identified as being on SSRI or SNRI. Forty-one were excluded because of known diagnosis of narcolepsy, PD, progressive supranuclear palsy (PSP), multisystem atrophy (MSA), or other α-synucleinopathies. From the remaining 1,444 patients who reported using one or more SSRI/ SNRI during the time they had their PSG, detailed data was collected including type of SSRI/SNRI, the presence of RSWA was defined by the AASM scoring criteria, RBD per the International Classification of Sleep Disorders, Third Edition criteria.1 The RSWA per epoch in our lab is usually evaluated by sustained muscle activity (tonic) over 20-s or 30-s epochs, and by transient muscle activity (phasic) over 3-s mini-epochs.16 RBD was defined by RSWA and history DEB from the patients' charts, videographic evidence of DEB, or mention of DEB on the pre-PSG intake questionnaire. In addition, we collected data on the presence of OSA, age, gender, and clinical indication for the antidepressant (generalized anxiety disorder, depression, obsessive compulsive disorder, fibromyalgia, bipolar affective disorder, or other). Because of similarity of action among medications within the same class, we compared SNRI to SSRI to see if one class was more likely to cause RSWA than the other. Risk ratio was calculated by Fisher exact test. Logistic regression analysis was performed to assess the association of OSA, age, and gender with RSWA, and statistical significance was defined for all other comparisons at p value of < 0.05.
Since there are no published criteria on how many epochs with RSWA are needed to mark a record as having RSWA, the few papers that come close to addressing this do it only for RBD,16,17 we relied on the individual physician's assessment of which records had RSWA and which did not. We did not go back and review all 10,746 PSGs. Similarly we relied on the interpreting physicians' report of presence or absence of RBD and the diagnoses of OSA.
We have always defined OSA as an apnea-hypopnea index (AHI) ≥ 5/hour. Since 2007 our lab has used the 30% reduction in airflow and 4% oxyhemoglobin desaturation rule to define a hypopnea.18 Lastly, in the setting of potential RSWA or RBD our interpreting physicians often stage epochs as REM sleep based primarily on eye movement density and EEG as suggested in the literature.19
RESULTS
Prevalence of RSWA in Those Taking Antidepressant Medications vs. General Sleep Lab Population
Of the 1,444 patients taking SSRI/SNRI medications, 176 patients had findings of RSWA (12.2%). This was significantly more than the prevalence of RSWA in the entire sleep lab population during the same time period (226 of 10,746; 2.1%), z-score 26.33, Fisher exact p < 0.0000001). Risk ratio (95% confidence interval) for RSWA in the setting of SSRI/SNRI intake was 9.978 (8.15, 12.22). Further information is presented in Tables 1 and 2.
Table 1.
Demographics of our cohort.
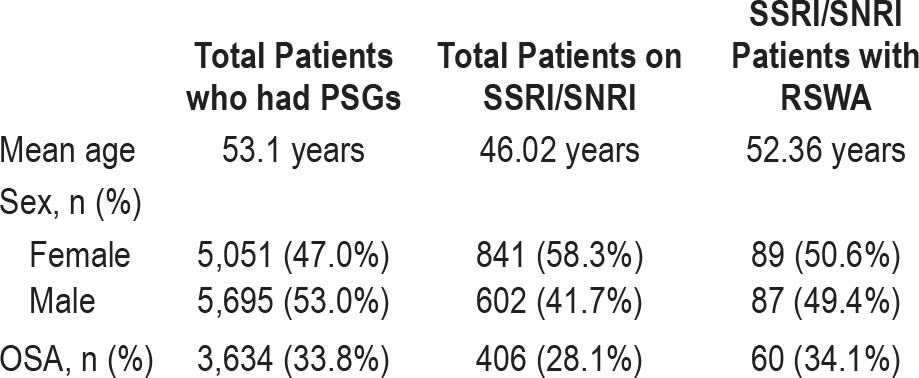
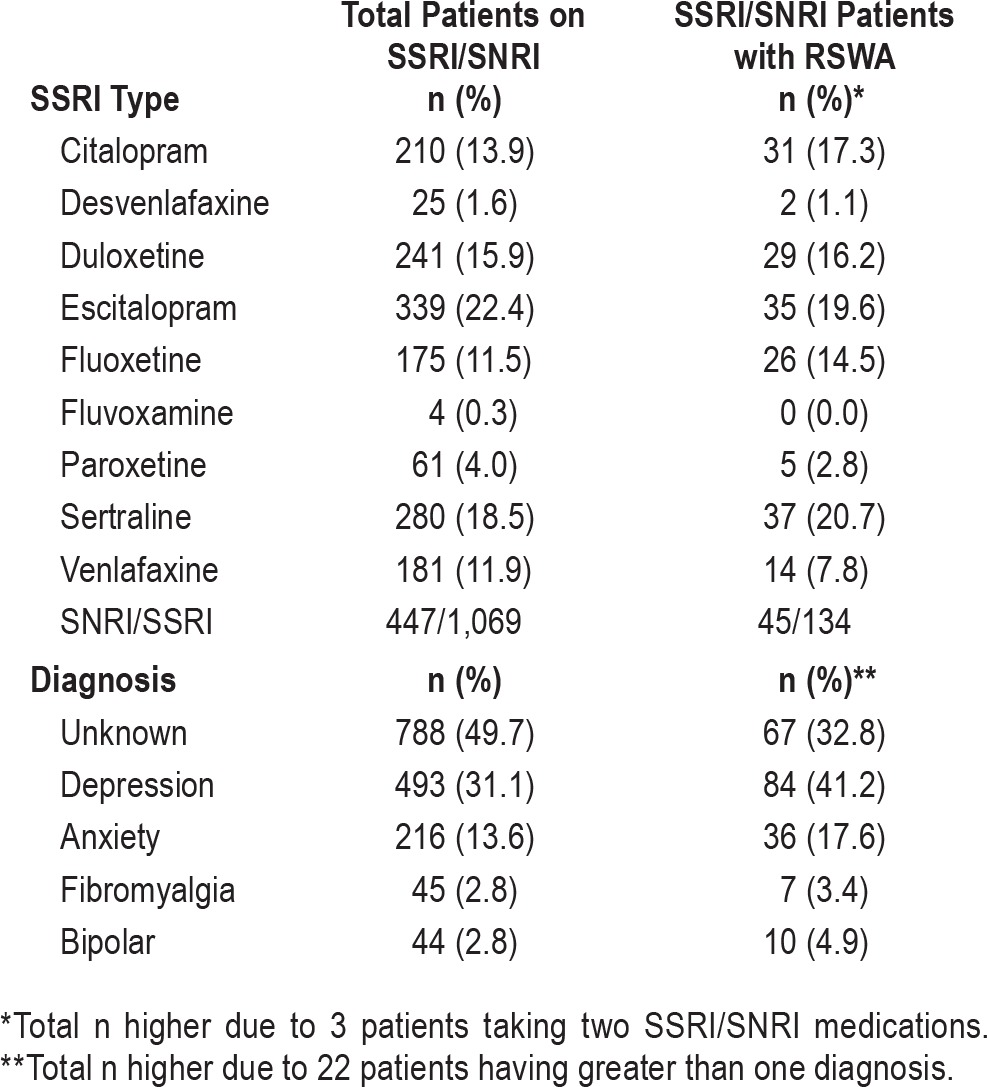
Table 2.
Antidepressant types and RSWA.
Demographics and Diagnosis of OSA
There were no differences in gender or age or diagnosis of OSA between patients on SSRI/SNRI with and without RSWA and the general lab population. Of the 176 patients with RSWA on SSRI/SNRI, 87 were male (49.4%) and 89 were female (50.6%). This was not significantly different than the gender distribution in the general sleep lab population (53% male and 47% female). The mean age of those with RSWA on SSRI and SNRI was 52.36 years, and that of the general lab population 53.1 years. OSA defined as an AHI ≥ 5/h was present in 33.8% (3,634/10,746) of the general lab population and in 34.1% (60/176) of our subjects on antidepressants and RSWA. Logistic regression showed that after controlling for age, gender, and presence of OSA, SSRI/ SNRI intake remained a significant predictor of RSWA.
Antidepressant Class
There was not a significant difference in RSWA based on antidepressant class. Among those on a single SNRI the prevalence of RSWA was 9.7% and among those on a single SSRI the prevalence of RSWA was 12.4%; p = 0.497) Thirty-two subjects were on 2 antidepressants simultaneously, one from each class, 3 of whom had RSWA (9.4%).
The review of their electronic medical records did not reveal a diagnosis associated with antidepressant prescriptions 55% of the time. Half those with two antidepressants carried the dual diagnosis of anxiety and depression.
REM Sleep Behavior Disorder
The prevalence of RBD diagnosis among those on SSRI/SNRI was 0.48% (7 of 1,444). This was significantly lower than the prevalence of RBD in the general lab population during the same time period of 1% (108 of 10,746); p value < 0.005 on Fisher exact test.
DISCUSSION
The goal of this study was to establish the prevalence of RSWA in the setting of SSRI/SNRI exposure in a large sleep laboratory population and to identify factors that are associated with it. Our results are consistent with previous studies that demonstrate increased prevalence of RSWA in patients taking anti-depressants.15,20,21 We also found that this increased risk is not due to age, gender, and type of SSRI/SNRI or presence of OSA. The most recent theories about REM sleep initiation advocate for a double switch model that may be triggered by neurons that are located in the brainstem.22,23 A complex interaction between REM-ON and REM-OFF neurons controls REM sleep. The latter utilizes NE to suppress REM sleep. When GABAergic inhibitory input turns off REM-OFF cells, REM-ON cells are released from this NE induced inhibition and initiate REM sleep. In the mesopontine tegmentum GABAergic activity inhibits the REM sleep suppression effects of the REMOFF cells, while in the locus ceruleus (LC), it directly inhibits REM-OFF cells altogether.24 REM-ON neurons have direct projections into the spinal cord tracts that send inhibitory signals to the lower motor neurons. Antidepressants, particularly SSRI and SNRI may interfere with this inhibition of monoamine activity during REM sleep, as they block serotonin and NE reuptake in the postsynaptic terminal.
Our study demonstrates nearly 10-fold increase in risk for RSWA while taking these medications. Interestingly however, the prevalence of RBD among those on SSRI/SNRI was lower than the larger group of sleep patients during the same time period. This finding may be an artifact of us excluding subjects with a known cause of RSWA/RBD, such as neurodegenerative disorders and narcolepsy, or it may represent the intriguing possibility that antidepressant exposure may be protective against RBD.
OSA by fragmenting REM sleep can lead to RSWA and what is known as pseudo RBD.4 Our analysis did not show a significant difference in the prevalence of OSA among those with RSWA on antidepressants and the general sleep lab population. Both age and gender have been associated with changes in RBD and RSWA prevalence. Men and older adults have a higher prevalence of these conditions.8 Again we did not find a significant difference in age distribution and in gender distribution between the two groups mentioned above. Logistic regression showed that none of the above variables (OSA, gender, and age) were driving the effect of higher prevalence.
Because of the more selective action of SSRI compared to SNRI, we postulated that SSRI were more likely to be associated with RSWA and RBD than SNRI, but this did not turn out to be the case in our cohort. Therefore, our results suggest that any disturbance in monoaminergic systems can increase the risk of RSWA. With the SNRI there is an increase in NE at the postsynaptic terminal. This leads to REM sleep suppression by continuing to activate REM-OFF cells in the LC, leading to a state similar to REM sleep deprivation.24 Animal models have shown that REM sleep can be suppressed with the activation of NE neurons in LC and that LC is important in motor control during sleep.24 The relationship between NE activity in the LC and REM sleep is not as simple as the previous sentence may suggest. It has been repeatedly shown that some level of NE is needed for the initiation and maintenance of REM sleep.25 Moreover REM sleep affects brain excitability and REM sleep deprivation can lead to increase in agitation and aggressive behavior.26 These therefore can partially explain how continued use of SNRI both suppress REM sleep and increase motor activity in REM sleep leading to RSWA and potentially RBD. Lastly, a potential treatment for RSWA, could include modulation of NE both by medications that either decrease NE release or block postsynaptic NE receptors.27
In order to postulate how SSRI and tricyclic antidepressants (TCA) can cause RSWA and RBD it is important to briefly review how normal REM sleep atonia is achieved. Normal REM sleep atonia is the result of two mechanisms. Decreased serotonergic neuronal activity in the descending pathways decreases the firing of lower motor neurons in NREM sleep and with continued decline in serotonergic activity, the lower motor neurons completely stop firing in REM sleep. In addition to this passive mechanism, there is an active cholinergicglutaminergic-glycinergic inhibition of the postsynaptic lower motor neurons. Theoretically SSRI, by increasing serotonergic activity, prevent the passive mechanism while TCAs that have anticholinergic properties block the active mechanism.28
Lastly, dopaminergic dysfunction also contributes to the development of RSWA, as neuroimaging in some patients with idiopathic RBD has shown decreased dopamine transporter activity and increased hyper-echogenicity in the midbrain substantia nigra area.29
There are several limitations to our study: (1) The one is that we relied on PSG reports primarily and did not go back and review the 10,746 PSGs to assess for RSWA, RBD, OSA, or tally data on separate phasic and tonic activity in PSGs with RSWA or account for age-related factors.17 Although we, as a group, are quite aware of RSWA and try not to miss it on all of our clinical PSGs there is always ample room for individual interpretations. Therefore some RSWA cases may have been missed. (2) This is a retrospective chart review performed using a database search. We did not contact individual subjects to verify their information. (3) Again, because this is a retrospective chart review and we did not review every single PSG, we relied on the diagnosis of OSA made at the time of the study and reported by then-interpreting physician. Although we try to use primarily the strict 30% reduction in airflow with 4% desaturation definition of hypopnea some of the records may have overestimated the apnea hypopnea index and hence the diagnosis of OSA; the same holds true for staging epochs with RSWA as REM sleep. (4) An automated quantitative approach with a computerized algorithm would have been more accurate but we did not have access to said method therefore were unable to use it. (5) We only eliminated records of subjects with narcolepsy and neurodegenerative disorders from the cohort on antidepressants, and the general population hence potentially introducing a bias that could explain the falsely low RBD rate among antidepressant users. (6) As this was a retrospective chart review of a large dataset we were unable to subgroup patients based on duration of illness for which they were prescribed antidepressants, the duration of treatment or by the doses of the medications. Some of those data were not available to us given the nature of the search engine we used. (7) Lastly, since the majority of the records did not indicate the diagnosis for which the antidepressants were prescribed, we could not factor in the elevated risk for RSWA a certain diagnosis such as anxiety or depression may confer, as there may be a link to psychiatric diagnoses and increase in RBD.30 Future directions should include prospective longitudinal study of people on SSRI/SNRI and those with RSWA and idiopathic RBD. People on these medications should be also stratified by diagnosis for which medications were prescribed. Risk of RSWA should be assessed in older antidepressant classes such as monoamine oxidase inhibitors (MAOI) and TCAs and this risk compared with those on SSRI and SNRI
CONCLUSIONS
Despite its limitations our study is the first to report both prevalence and risk ratio of RSWA in a group of people on SSRI/ SNRI. The risk appears to be independent of other confounding variables such as OSA, age, and sex. Since these medications are very commonly prescribed with an estimated 11% of Americans aged 12 and older now on an antidepressant,14 it is important to be cautious of physiologic changes they may induce, even if the clinical significance of these changes is not fully elucidated.
DISCLOSURE STATEMENT
This was not an industry supported study. Kelly Baron is on the scientific advisory board of General Sleep Corp. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dr. Indranil Sen-Gupta for developing the sleep cataloguer software and allowing its use for this project.
ABBREVIATIONS
- MSA
multi system atrophy
- OSA
obstructive sleep apnea
- PSP
progressive supranuclear palsy
- RBD
REM sleep behavior disorder
- REM sleep
rapid eye movement sleep
- RSWA
REM sleep without atonia
- SNRI
selective norepinephrine reuptake inhibitors
- SSRI
selective serotonin reuptake inhibitors
REFERENCES
- 1.American Academy of Sleep Medicine. International classification of sleep disorders. 3rd ed. Darien, IL: American Academy of Sleep Medicine; 2014. [Google Scholar]
- 2.Vendette M, Gagnon JF, Décary A, et al. REM sleep behavior disorder predicts cognitive impairment in Parkinson disease without dementia. Neurology. 2007;69:1843–9. doi: 10.1212/01.wnl.0000278114.14096.74. [DOI] [PubMed] [Google Scholar]
- 3.Nightingale S, Orgill JC, Ebrahim IO, de Lacy SF, Agrawal S, Williams AJ. The association between narcolepsy and REM behavior disorder (RBD) Sleep Med. 2005;6:253–8. doi: 10.1016/j.sleep.2004.11.007. [DOI] [PubMed] [Google Scholar]
- 4.Iranzo A, Santamaria J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005;28:203–6. doi: 10.1093/sleep/28.2.203. [DOI] [PubMed] [Google Scholar]
- 5.Olson EJ, Boeve BF, Silber MH. Rapid eye movement sleep behaviour disorder: demographic, clinical and laboratory findings in 93 cases. Brain. 2000;123(Pt 2):331–9. doi: 10.1093/brain/123.2.331. [DOI] [PubMed] [Google Scholar]
- 6.Rupprecht S, Walther B, Gudziol H, et al. Clinical markers of early nigrostriatal neurodegeneration in idiopathic rapid eye movement sleep behavior disorder. Sleep Med. 2013;14:1064–70. doi: 10.1016/j.sleep.2013.06.008. [DOI] [PubMed] [Google Scholar]
- 7.McCarter SJ, St Louis EK, Boeve BF. REM sleep behavior disorder and REM sleep without atonia as an early manifestation of degenerative neurological disease. Curr Neurol Neurosci Rep. 2012;12:182–92. doi: 10.1007/s11910-012-0253-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kang SH, Yoon IY, Lee SD, Han JW, Kim TH, Kim KW. REM sleep behavior disorder in the Korean elderly population: prevalence and clinical characteristics. Sleep. 2013;36:1147–52. doi: 10.5665/sleep.2874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schenck CH, Mahowald MW, Kim SW, O'Connor KA, Hurwitz TD. Prominent eye movements during NREM sleep and REM sleep behavior disorder associated with fluoxetine treatment of depression and obsessive-compulsive disorder. Sleep. 1992;15:226–35. doi: 10.1093/sleep/15.3.226. [DOI] [PubMed] [Google Scholar]
- 10.Applebee GA, Attarian HP, Schenck C. An angry bed partner. J Clin Sleep Med. 2009;5:477–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Sheyner I, Khan S, Stewart JT. A case of selective serotonin reuptake inhibitor-induced rapid eye movement behavior disorder. J Am Geriatr Soc. 2010;58:1421–2. doi: 10.1111/j.1532-5415.2010.02947.x. [DOI] [PubMed] [Google Scholar]
- 12.Parish J. Violent dreaming and antidepressant drugs: or how paroxetine made me dream that I was fighting Saddam Hussein. J Clin Sleep Med. 2007;3:529–31. [PMC free article] [PubMed] [Google Scholar]
- 13.Postuma RB, Gagnon JF, Tuineaig M, et al. Antidepressants and REM sleep behavior disorder: isolated side effect or neurodegenerative signal? Sleep. 2013;36:1579–85. doi: 10.5665/sleep.3102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pratt LA, Brody DJ, Gu Q. Antidepressant use in persons aged 12 and over: United States, 2005-2008. NCHS Data Brief. 2011;76:1–8. [PubMed] [Google Scholar]
- 15.Hoque R, Chesson A. Pharmacologically induced/exacerbated restless legs syndrome, periodic limb movements of sleep, and REM behavior disorder/REM sleep without atonia: literature review, qualitative scoring, and comparative analysis. J Clin Sleep Med. 2010;6:79–83. [PMC free article] [PubMed] [Google Scholar]
- 16.Montplaisir J, Gagnon JF, Fantini ML, et al. Polysomnographic diagnosis of idiopathic REM sleep behavior disorder. Mov Disord. 2010;25:2044–51. doi: 10.1002/mds.23257. [DOI] [PubMed] [Google Scholar]
- 17.Ferri R, Gagnon JF, Postuma RB, Rundo F, Montplaisir JY. Comparison between an automatic and a visual scoring method of the chin muscle tone during rapid eye movement sleep. Sleep Med. 2014;15:661–5. doi: 10.1016/j.sleep.2013.12.022. [DOI] [PubMed] [Google Scholar]
- 18.Ruehland WR, Rochford PD, O'Donoghue FJ, Pierce RJ, Singh P, Thornton AT. The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep. 2009;32:150–7. doi: 10.1093/sleep/32.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lapierre O, Montplaisir J. Polysomnographic features of REM sleep behavior disorder: development of a scoring method. Neurology. 1992;42:1371–4. doi: 10.1212/wnl.42.7.1371. [DOI] [PubMed] [Google Scholar]
- 20.Zhang B, Hao Y, Jia F, Tang Y, Li X, Liu W, Arnulf I. Sertraline and rapid eye movement sleep without atonia: an 8-week, open-label study of depressed patients. Prog Neuropsychopharmacol Biol Psychiatry. 2013;47:85–92. doi: 10.1016/j.pnpbp.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 21.Boeve BF, Silber MH, Ferman TJ, et al. Clinicopathologic correlations in 172 cases of rapid eye movement sleep behavior disorder with or without a coexisting neurologic disorder. Sleep Med. 2013;14:754–62. doi: 10.1016/j.sleep.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Peever J, Luppi PH, Montplaisir J. Breakdown in REM sleep circuitry underlies REM sleep behavior disorder. Trends Neurosci. 2014;37:279–88. doi: 10.1016/j.tins.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 23.Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007;130:2770–88. doi: 10.1093/brain/awm056. [DOI] [PubMed] [Google Scholar]
- 24.Mallick BN, Singh A, Khanday MA. Activation of inactivation process initiates rapid eye movement sleep. Prog Neurobiol. 2012;97:259–76. doi: 10.1016/j.pneurobio.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Gottesmann C. Noradrenaline involvement in basic and higher integrated REM sleep processes. Prog Neurobiol. 2008;85:237–72. doi: 10.1016/j.pneurobio.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 26.Mallick BN, Singh A. REM sleep loss increases brain excitability: role of noradrenaline and its mechanism of action. Sleep Med Rev. 2011;15:165–78. doi: 10.1016/j.smrv.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Herholz J, Crisponi L, Mallick BN, Rutsch F. Successful treatment of cold-induced sweating in Crisponi syndrome and its possible mechanism of action. Dev Med Child Neurol. 2010;52:494–7. doi: 10.1111/j.1469-8749.2010.03630.x. [DOI] [PubMed] [Google Scholar]
- 28.Zhang B, Hao Y, Jia F, Tang Y, Li X, Liu W, Arnulf I. Sertraline and rapid eye movement sleep without atonia: an 8-week, open-label study of depressed patients. Prog Neuropsychopharmacol Biol Psychiatry. 2013;47:85–92. doi: 10.1016/j.pnpbp.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 29.Arnulf I. REM sleep behavior disorder: motor manifestations and pathophysiology. Mov Disord. 2012;27:677–89. doi: 10.1002/mds.24957. [DOI] [PubMed] [Google Scholar]
- 30.Lam SP, Fong SY, Ho CK, Yu MW, Wing YK. Parasomnia among psychiatric outpatients: a clinical, epidemiologic, cross-sectional study. J Clin Psychiatry. 2008:1374–82. doi: 10.4088/jcp.v69n0904. [DOI] [PubMed] [Google Scholar]


