Abstract
Background
The modified Lapidus procedure is widely used to correct hallux valgus but has been reported with high nonunion rates. In this study, we retrospectively reviewed the nonunion rate of the modified Lapidus procedure performed with rigid cross screw fixation, meticulous joint preparation, and shear-strain-relieved calcaneal bone graft.
Questions/Purposes
Does the performance of the Lapidus procedure with rigid cross screw fixation, complete joint preparation, and shear-strain-relieved calcaneal bone graft achieve higher union rates than currently reported? If nonunion does occur, what is the clinical course?
Methods
We reviewed both radiographic and clinical results of the modified Lapidus procedure with the above technique in 171 patients (182 feet). Evaluation included age, gender, tobacco use, diabetic status, and radiographic analysis at least 3 months postoperatively.
Results
The modified Lapidus procedure described above resulted in a union rate of 97.3% (177 of 182 feet). Three of the five feet with radiographic nonunions were clinically symptomatic.
Conclusions
The union rate of the modified Lapidus procedure is higher than previously reported when performed with rigid cross screw fixation, meticulous joint preparation, and shear-strain-relieved bone graft. Nonunion of the first tarsometatarsal joint should be considered an infrequent occurrence.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-015-9462-8) contains supplementary material, which is available to authorized users.
Keywords: hallux valgus, lapidus, bunion, fusion, arthrodesis, autograft
Introduction
The modified Lapidus procedure, consisting of fusion of the first tarsometatarsal (TMT) joint with concurrent distal soft tissue realignment, has commonly been utilized for patients with moderate to severe hallux valgus deformity in the setting of a hypermobile first ray [10, 13, 16, 18]. Instability of the first ray is believed to contribute to deformity and pain. Lesser metatarsal overload is often seen as a result of first ray instability. Arthrodesis of the first TMT joint with distal soft tissue procedures effectively resolves instability, deformity, and pain.
Historically, some surgeons may have limited the use of the modified Lapidus procedure, even in the setting of a hypermobile first ray, due to its associated complications of nonunion, malunion, and shortening [2, 7, 8, 10, 13, 16, 18]. The biggest concern in previous publications is a relatively high nonunion rate, up to 12% (Table 1) [2, 10, 11, 13, 18]. However, most of these studies with high nonunion rates involved varied joint preparation and different types of fixation [2, 3, 7, 8, 10, 13, 16, 18]. Most recently, a meta-analysis in 2011 found a nonunion rate of 5% in 537 patients and recommended further investigation [3].
Table 1.
Nonunion rates reported in previous studies
Various components of the surgical technique have been described to theoretically increase the union rate of the first tarsometatarsal joint. First, rigid compression with cross screw fixation has been shown to increase primary bone healing in general [14]. Meticulous joint preparation, taking care to remove all cartilage and drill numerous channels to allow blood inflow, has also been reported to aid in bone healing [18]. Finally, shear-strain-relieved bone graft has been described to promote secondary bone healing at the periphery of joint fusions where shear strain is higher [6]. Healing occurs on the edges of the first tarsometatarsal joint as cartilaginous tissue ossifies. The small gap between the two bones then disappears which effectively minimizes motion, eliminates the more interior shear strains, and allows the whole joint to heal. The results of the combination of rigid cross screw fixation, meticulous joint preparation, and shear-strain-relieved calcaneal graft in the setting of a Lapidus procedure have not been reported.
The purpose of this study was to determine the fusion rate of the modified Lapidus procedure for hallux valgus with the above technique, and compare these to rates reported in the literature. Additionally, if nonunion occurred, we followed the clinical course of the patient to understand the nature of the complication. Our study utilizes a large cohort of patients with similar methods of fixation, postoperative regimens, and the utilization of compression fixation, joint preparation, and calcaneal bone graft.
Patients and Methods
Approval from the Institutional Review Board was obtained before the study was conducted. A retrospective chart review from January 2003 to June 2012 identified all patients undergoing a modified Lapidus procedure for symptomatic hallux valgus performed by one of two fellowship-trained foot and ankle attending surgeons. Only patients who were over the age of 18, had at least a 3-month clinical and radiographic follow-up, and who underwent surgery with calcaneal bone graft were included in the study. Patients were excluded if they underwent multiple tarsometatarsal joint fusions or other simultaneous midfoot or hindfoot procedures that may have altered their postoperative recovery. Additional procedures such as neuroma excision, removal of hardware, and soft tissue excision did not exclude patients from the study.
Overall, 182 feet in 171 patients were included in the study. There were 159 women and 12 men. The foot involved was the left in 101 cases and the right in 81 cases. At least one secondary procedure was done in 96% of patients (Table 2). The average age was 58.2 (range, 18 to 81) years old. The average follow-up was 180 days.
Table 2.
Other procedures performed
| Procedure | Number performed |
|---|---|
| Akin osteotomy | 144 |
| Hammer toe corrections | 91 |
| Gastrocnemius recession | 78 |
| Lesser metatarsal shortening osteotomies | 53 |
The surgical technique applied by each attending surgeon was similar in the technique of joint preparation, method of fixation, and postoperative management. Clinical assessment of patients was performed by the surgeons at 2, 6, and 12 weeks postoperatively. Radiographs were taken at 6 and 12 weeks. If there was any question of union at 3 months, patients returned to the office at 6 months for reevaluation. Clinical concern for nonunion was suspected with continued pain or swelling at the first TMT joint. In the absence of pain or abnormalities on radiographs taken at 12 weeks after surgery, the decision to follow a patient or order imaging at 6 months was made by the treating surgeon, but in some cases not deemed necessary.
A foot and ankle fellowship-trained attending surgeon, who was blinded to the clinical results and not involved in the clinical care of any patients, determined if radiographs showed evidence of nonunion. All radiographs were reviewed by the same individual on two different occasions in random order. Nonunion was defined as greater than 50% lucency on either the A-P and lateral radiographs or broken hardware at the fusion site. If lucency, sclerosis, or lack of trabeculation extended more than one-half the length of the fusion site, on either the A-P or lateral radiograph, a radiographic nonunion was declared. Intrarater agreement was assessed by calculating the simple Kappa statistic and 95% confidence interval. A Kappa statistic >0.8 indicates excellent agreement.
For the operative procedure, each patient was placed supine with a proximal thigh tourniquet for hemostasis. Prior to preparation of the TMT joint, a medial longitudinal incision and capsulotomy allowed access to shave the medial eminence and perform a medial capsular plication. If necessary, soft tissue release was performed with a lateral capsulotomy through a separate incision over the first webspace. A dorsal longitudinal skin incision was then made over the first TMT joint. Dissection proceeded between the extensor hallucis longus and extensor hallucis brevis, taking care to protect the dorsal cutaneous nerves. Upon verifying the first tarsometatarsal joint, a capsulotomy was performed by sharp dissection. An oscillating saw was used to remove a triangular wedge of bone from the medial cuneiform and base of the first metatarsal, leaving the medial subchondral plate intact (Fig. 1). A larger amount of bone was removed from the lateral surface to ensure adequate reduction of the intermetarsal angle. Care was taken to ensure that all cartilage was removed during these saw cuts. Intraoperative radiographic assessment confirmed the reduction of the intermetatarsal angle. A 0.062-in. Kirschner wire was used to meticulously fenestrate the joint edges to promote cancellous bleeding (Fig. 2). The joint was then reduced and compression was obtained by using a combination of 3.5-mm and 4.0-mm cortical lag screws, based on surgeon preference, in a crossed compression screw pattern. This provided rigid fixation of the metatarsocuneiform joint. Final alignment was confirmed on fluoroscopy. At the discretion of the attending surgeon, demineralized bone matrix putty was added to the periphery of the fusion site in some patients (53 feet in 52 patients).
Fig. 1.
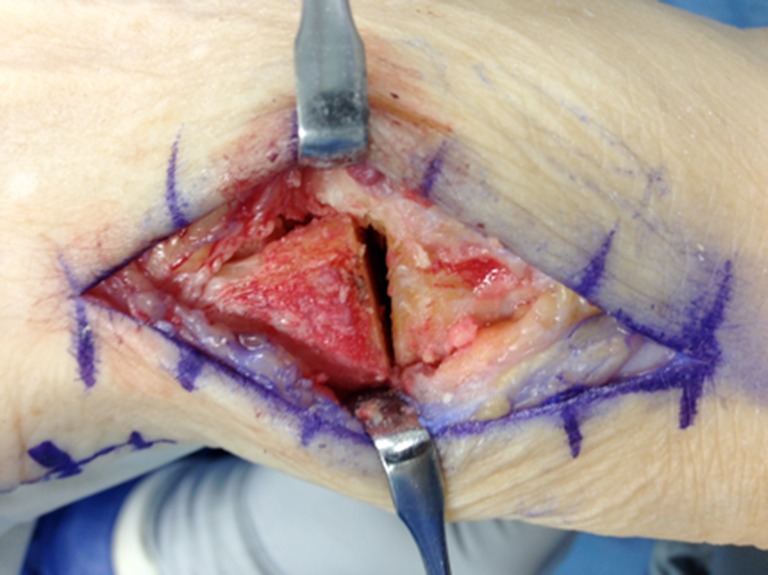
Wedge resection. Using an oscillating saw, a wedge of bone is removed from the medial cuneiform and the first metatarsal base to create a flat surface.
Fig. 2.

Joint surface preparation. The joint surface is fenestrated with a 0.062-in. Kirschner wire to promote cancellous bleeding.
Calcaneal autograft was obtained through a small, 1-cm incision made parallel and inferior to the peroneal tendons over the lateral aspect of the calcaneus. After an incision through skin, blunt dissection down to bone ensured protection of branches of the sural nerve [12]. A periosteal elevator exposed the lateral wall of the calcaneus and gentle penetration of the wall was made with a soft tissue protector used for a 4.5-mm drill (Fig. 3). Redirection of the soft tissue protector through the original hole allowed for two to three plugs of cancellous bone graft to be obtained. Next, a motorized burr was used to create two 4.0-mm troughs in the dorsomedial and dorsolateral first TMT joint. These troughs were filled with the plugs of calcaneal bone graft and were used as stress–strain troughs to promote a successful union (Fig. 4). The total volume of calcaneal bone graft placed at the fusion site was approximately 67 mm3 (2 × 4/3 × π × r3 where r = 2 mm, representing two spherical plugs of calcaneal bone graft placed in two burr holes).
Fig. 3.

Calcaneal autograft harvest. Bone graft from the calcaneus is obtained with a soft tissue protector via a small lateral incision.
Fig. 4.

Placement of autograft. After troughs are created on the dorsal aspect of the fusion site, plugs of calcaneal autograft are inserted in the holes.
Postoperatively, patients were placed in a well-padded posterior splint for 2 weeks with strict nonweightbearing. When sutures were removed at 2 weeks, patients were transitioned to a CAM boot and remained nonweightbearing for an additional 4 weeks. At 6 weeks, patients underwent radiographic evaluation and progressively advanced their weightbearing in the walking boot. At 10 weeks postoperatively, patients returned to full weightbearing in supportive shoes with gradual return to activities.
Results
One hundred seventy-seven (97.3%) feet healed without pain or radiographic evidence of nonunion. Radiographic nonunions were identified on the first radiographic review in five feet (2.7%) in five patients (Table 3). The second review, done primarily to determine reliability of the radiographic assessment, found nonunion in four of the five above patients (nonunion rate of 2.2%). One patient previously read as a nonunion was determined in the new analysis to have union. However, the subsequent analysis below was carried out with the worst case scenario (i.e., the group of five).
Table 3.
Subjects with nonunion
| Patient | Age (year) | Sex | Radiographs | Complication | Additional procedures |
|---|---|---|---|---|---|
| 1 | 69 | F | Screws intact, lucency | Symptomatic nonunion | 2nd metatarsal shortening osteotomy and HT correction |
| 2 | 57 | F | Screws intact, lucency | Symptomatic nonunion | Akin osteotomy |
| 3 | 51 | M | Screws broken, lucency | Asymptomatic nonunion | Gastrocnemius recession, Akin, 2/3 metatarsal shortening osteotomies, 2/3 HT corrections |
| 4 | 48 | F | Screws broken, lucency | Symptomatic nonunion | None |
| 5 | 66 | F | Screws intact, lucency | Asymptomatic nonunion | Demineralized bone matrix putty |
The average age of the five patients with nonunions was 58.2 (range, 48 to 69) years old. Lucency greater than 50% across the arthrodesis site was present in all five nonunions (Fig. 5). Broken hardware was evident in two nonunions (Fig. 6). Demineralized bone matrix putty was utilized in one of these nonunions. Additionally, there were no reports of painful hardware in any of the patients included in this study. There were also no postoperative complaints of pain at the calcaneal harvest site.
Fig. 5.

Nonunion. Radiographic evidence of nonunion in this study subject is confirmed by greater than 50% lucency at the fusion site.
Fig. 6.

Nonunion. This study subject was found to have a nonunion at the fusion site with evidence of broken hardware.
Three nonunions were clinically symptomatic and revision surgery was recommended. One of the clinically symptomatic nonunions underwent a revision Lapidus procedure with calcaneal bone graft and subsequently went on to a successful union. Two clinically symptomatic nonunions were lost to follow-up.
Two nonunions were clinically asymptomatic, yet had evidence of nonunion on radiographs. One of these nonunions also had demineralized bone matrix putty utilized during the initial procedure. Neither of these patients had residual pain nor required revision surgery. None of the nonunions had a medical history of tobacco use, peripheral neuropathy, steroid use, osteoporosis, or diabetes. All nonunions were compliant with the nonweightbearing postoperative protocol. A Kappa statistic of 0.886 [0.665, 1.000], indicated excellent intraobserver reliability.
Discussion
Since Lapidus first described arthrodesis of the base of the first metatarsocuneiform joint in 1934, there have been numerous modifications to improve its efficacy [8]. Methods of joint preparation, type of fixation, use of bone graft, and length of nonweightbearing have varied throughout the literature leading to a wide range in reported success. Our study shows one of the lowest nonunion rates (2.7%) in the literature when a large cohort is used.
A significant strength of our study is the large number of patients included with only two operating surgeons. Additionally, bias was minimized by having radiographs read by a third foot and ankle fellowship-trained surgeon, who was uninvolved in the patients’ care and was blinded to the patients’ clinical results. Finally, reliability was assessed by having the same surgeon review the radiographs in a random fashion for a second time and was found to be excellent.
We recognize there are some limitations in our study. Many other studies follow patients routinely for 6 months postoperatively, whereas we chose 3 months as complete follow-up. The analysis of union was limited to this time because of the retrospective nature of the study: the treating surgeons may not have seen the patients in follow-up or ordered radiographs after 3 months if they were doing well clinically and the joint looked radiographically healed with intact hardware at that time. If there was any question of radiographic or clinical union, then the patient returned to the office for repeat radiographs at 6 months. We felt this provided us with enough time to determine a complete union. Gérard et al. noted that his arthrodeses had fused by 3 months [5]. Another weakness is that our fusion rate was determined solely by clinical and radiographic analysis. A superior method would involve CT scans to assess the completeness of union. However, this is not the standard of care in our practice for an uncomplicated fusion procedure. Given the retrospective nature of the study and the radiation exposure entailed, this would not have been feasible or appropriate in this setting.
Another variable in our study is that 53 patients had demineralized bone matrix putty added to their fusion site. One of these patients went on to a radiographic nonunion. While our sample size is too small to calculate its effect, we have stopped utilizing demineralized bone matrix putty in our modified Lapidus procedures, as it does not appear to have an appreciable effect on our union rates.
Patient satisfaction after the modified Lapidus procedure ranges from 75 to 96% [7]. Despite high levels of satisfaction, the modified Lapidus procedure has faced a stigma of relatively high nonunion rates, with symptomatic nonunions present in roughly half [18]. Sangeorzan and Hansen reported a nonunion rate of 10% in 40 feet in 1989 [16]. In a larger study in the podiatric literature in 2004, Patel et al. reported a nonunion rate of 5.3% in 227 feet [13]. Their technique was standardized with joint cartilage denuding with a sharp osteotome and fenestration of the fusion surface with two crossed screws, but they did not use any additional bone graft at the fusion site. Our study utilized additional bone graft in every patient and resulted in a lower nonunion rate.
In 2005, Thompson et al. reported a nonunion rate of 4% in 201 feet treated with a modified Lapidus for both flatfoot deformity and hallux valgus [18]. They utilized local autogenous bone graft for strain relief, but did not have a uniform set of hallux valgus patients. Our study only included patients who were having surgery with a diagnosis of hallux valgus. Donnenwerth et al. reviewed five studies between 2001 and 2005 in a meta-analysis with similar joint preparation, crossed screw fixation, and postoperative nonweightbearing regimen [3]. They determined a nonunion rate of 5 % in 599 feet. The authors regarded this number to be a relatively high rate of nonunion that warranted additional studies.
Bone grafting is commonly used in foot and ankle surgery to improve the biology of healing and subsequently lead to improved union rates [4]. While high complication rates, ranging from 10 to 49%, have been reported for harvesting iliac crest bone graft, several studies have shown high satisfaction and low complication rates with harvesting calcaneal bone graft for foot and ankle procedures [1, 15, 17]. More recently, O’Malley et al. explored a large cohort of patients who had calcaneal bone graft and stated that while it was easy to harvest, there were some residual complaints related to the incision in 13.8% of patients [12]. Despite these minor complaints, using calcaneal bone graft to augment the union of the first TMT joint appears to provide numerous benefits. The bone graft is obtained from the ipsilateral foot in the same surgical field. It is easily accessible through one small additional incision, and it does not change the postoperative protocol. With low morbidity and ample supply, this autologous cancellous bone is osteoinductive, osteoconductive, and osteogenic and offers no risk of disease transmission [9]. In our study, there were no reports of persistent incisional pain or complications from harvesting calcaneal bone graft. While we cannot report that the low nonunion rate is directly a result of our use of calcaneal bone graft, we do believe the reduction of strain at the fusion site may have been beneficial in aiding union.
Stable fixation is important to allow for primary bone healing. However, even with adequate internal fixation, there is still micro motion leading to shear stresses at the fusion site. Hansen described using bone graft to reduce the shear strain at the bone interface by increasing surface area with small burr holes, filled with bone graft [6]. We believe that our technique utilizing flat cuts, combined with shear strain reduction from troughs filled with bone graft, aids in improving fusion rates of the first tarsometatarsal joint.
In our study, there are many successful unions, and some definitive nonunions. However, there were also patients who radiographically had failed, but clinically were a success. Two patients (out of the five nonunions) fell into this category of asymptomatic nonunions. They continued to function well without the need for revision surgery. In comparison, Patel et al. [13] reported two asymptomatic nonunions out of their total 12 nonunions and Thompson et al. [18] reported four asymptomatic nonunions of their total eight nonunions. With these details, it appears that an isolated radiographic nonunion may not classify as a complete failure and we should continue to account for both clinical and radiographic factors in assessing our patients postoperatively. Therefore, while nonunion can be radiographically identified, it does not appear to always mandate revision surgery when clinically asymptomatic.
To our knowledge, this study represents the second largest published cohort of patients undergoing the modified Lapidus procedure for hallux valgus. In addition, our reported nonunion rate of 2.7% is lower than most percentages in the literature. Clinically relevant nonunions that required further intervention were only 1.6% of our cohort. We attribute these results to an operative technique utilizing rigid internal fixation, meticulous joint preparation, and use of shear-strain-relieved bone calcaneal autograft.
Overall, our series shows favorable union rates for patients undergoing a modified Lapidus procedure for the correction of hallux valgus. Successful union was obtained in 97.3% of patients in a large cohort. Rigid internal fixation, meticulous joint preparation, and the addition of shear-strain-relieved calcaneal bone graft appear to provide the best environment to promote union at the first TMT joint in the modified Lapidus procedure for hallux valgus.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Acknowledgments
Disclosures
ᅟ
Conflict of Interest:
Sriniwasan B. Mani, BS, Eric W. Lloyd, MD, Aoife MacMahon, BA, Matthew M. Roberts, MD, David S. Levine, MD and Scott J. Ellis, MD have declared that they have no conflict of interest.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent:
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: IV, Retrospective Case Series
Work performed at Hospital for Special Surgery in New York City, NY.
References
- 1.Biddinger KR, Komenda GA, Schon LC, Myerson MS. A new modified technique for harvest of calcaneal bone grafts in surgery on the foot and ankle. Foot Ankle Int. 1998;19(5):322–326. doi: 10.1177/107110079801900510. [DOI] [PubMed] [Google Scholar]
- 2.Blitz NM, Lee T, Williams K, Barkan H, DiDimenico LA. Early weight bearing after modified Lapidus arthodesis: a multicenter review of 80 cases. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2010;49(4):357–362. doi: 10.1053/j.jfas.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 3.Donnenwerth MP, Borkosky SL, Abicht BP, Plovanich EJ, Roukis TS. Rate of nonunion after first metatarsal-cuneiform arthrodesis using joint curettage and two crossed compression screw fixation: a systematic review. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2011;50(6):707–709. doi: 10.1053/j.jfas.2011.08.003. [DOI] [PubMed] [Google Scholar]
- 4.Fitzgibbons TC, Hawks MA, McMullen ST, Inda DJ. Bone grafting in surgery about the foot and ankle: indications and techniques. J Am Acad Orthop Surg. 2011;19(2):112–120. doi: 10.5435/00124635-201102000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Gérard R, Stern R, Assal M. The modified Lapidus procedure. Orthopedics. 2008;31(3):230–236. doi: 10.3928/01477447-20080301-14. [DOI] [PubMed] [Google Scholar]
- 6.Hansen ST. Shear-Strain-Relieved Bone Graft. In: Functional Reconstruction of the Foot and Ankle. Vol 1st ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2000:485–486.
- 7.Kopp FJ, Patel MM, Levine DS, Deland JT. The modified Lapidus procedure for hallux valgus: a clinical and radiographic analysis. Foot Ankle Int. 2005;26(11):913–917. doi: 10.1177/107110070502601103. [DOI] [PubMed] [Google Scholar]
- 8.Lapidus PW. Operative correction of the metarsus varus primus in hallux valgus. Surg Gynecol Obstet. 1934;54:183–191. [Google Scholar]
- 9.McGarvey WC, Braly WG. Bone graft in hindfoot arthrodesis: allograft vs autograft. Orthopedics. 1996;19(5):389–394. doi: 10.3928/0147-7447-19960501-08. [DOI] [PubMed] [Google Scholar]
- 10.McInnes BD, Bouché RT. Critical evaluation of the modified Lapidus procedure. J Foot Ankle Surg. 2001;40(2):71–90. doi: 10.1016/S1067-2516(01)80048-X. [DOI] [PubMed] [Google Scholar]
- 11.Menke CRD, McGlamry MC, Camasta CA. Lapidus arthrodesis with a single lag screw and a locking H-plate. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2011;50(4):377–382. doi: 10.1053/j.jfas.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 12.O’Malley MJ, Sayres SC, Saleem O, et al. Morbidity and complications following percutaneous calcaneal autograft bone harvest. Foot Ankle Int. 2014;35(1):30–37. doi: 10.1177/1071100713511806. [DOI] [PubMed] [Google Scholar]
- 13.Patel S, Ford LA, Etcheverry J, Rush SM, Hamilton GA. Modified Lapidus arthrodesis: rate of nonunion in 227 cases. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 2004;43(1):37–42. doi: 10.1053/j.jfas.2003.11.009. [DOI] [PubMed] [Google Scholar]
- 14.Perren SM. The biomechanics and biology of internal fixation using plates and nails. Orthopedics. 1989;12(1):21–34. doi: 10.3928/0147-7447-19890101-06. [DOI] [PubMed] [Google Scholar]
- 15.Raikin SM, Rasouli MR, Espandar R, Maltenfort MG. Trends in treatment of advanced ankle arthropathy by total ankle replacement or ankle fusion. Foot Ankle Int. 2014;35(3):216–224. doi: 10.1177/1071100713517101. [DOI] [PubMed] [Google Scholar]
- 16.Sangeorzan BJ, Hansen ST. Modified Lapidus procedure for hallux valgus. Foot Ankle Int. 1989;9(6):262–266. doi: 10.1177/107110078900900602. [DOI] [PubMed] [Google Scholar]
- 17.Schulhofer SD, Oloff LM. Iliac crest donor site morbidity in foot and ankle surgery. J Foot Ankle Surg Off Publ Am Coll Foot Ankle Surg. 1997; 36(2): 155-8. discussion 161. [DOI] [PubMed]
- 18.Thompson IM, Bohay DR, Anderson JG. Fusion rate of first tarsometatarsal arthrodesis in the modified Lapidus procedure and flatfoot reconstruction. Foot Ankle Int. 2005;26(9):698–703. doi: 10.1177/107110070502600906. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)


