Abstract
Multiple studies have investigated the association of gene variant of Deleted in colorectal carcinoma (DCC) and Prostate Stem cell antigen (PSCA) with various cancer susceptibility; however, the results are discrepant. Since SNPs are emerging as promising biomarker of cancer susceptibility, here, we aimed to execute a meta-analysis of DCC (rs714 A > G) and PSCA (rs2294008 C > T, rs2976392 G > A) polymorphism to demonstrate the more accurate strength of these associations. We followed a rigorous inclusion/exclusion criteria and calculated the pooled odds ratios (ORs) and 95% confidence intervals (CIs). Overall, the pooled analysis showed that the DCC rs714 conferred increased risk of cancer only in Asians (AA vs. GG: OR = 1.86, p ≤ 0.0001; AG vs. GG: OR = 1.43, p = 0.005; GA + AA vs. GG: OR = 1.66, p ≤ 0.0001; AA vs. GG + GA; OR = 1.52, p ≤ 0.004, A vs. G allele: OR = 1.41, p ≤ 0.0001). PSCA rs2294008 was associated with increased overall cancer risk (TT vs. CC: OR = 1.28, p = 0.002; CT vs. CC: OR = 1.21, p ≤ 0.0001; CT + TT vs. CC: OR = 1.24, p ≤ 0.0001; TT vs. CC + CT; OR = 1.17, p ≤ 0.005, T vs. C allele: OR = 1.16, p ≤ 0.0001); however, in stratified analysis this association was limited only to gastric and bladder cancer and the strength was more prominent in Asians. In contrast, the PSCA rs2976392 SNP did not modulate the cancer risk. Therefore, we concluded that rs714 and rs2294008 polymorphism may represent a potential genetic biomarker for cancer risk in Asians and gastric as well as bladder cancer, respectively. However, since our study is limited to Asians and cancer types, further larger studies involving other cancers and/or population, gene-environment interactions and the mechanism of DCC and PSCA gene deregulation are desired to define the role of genotype with overall cancer risk.
Keywords: PSCA, DCC, polymorphism, cancer, meta-analysis
1. Introduction
Cancer initiation and progression is a complex and multifaceted process involving numerous genetic as well as environmental risk factors [1]. Moreover, inheritance of the majority of cancers is polygenic, and several genes with mild consequence are involved in the carcinogenesis [2]. Multiple studies (Genome wide association studies/GWAS, case-control and cohort) have unveiled single-nucleotide polymorphisms (SNPs) as the most common forms of human genetic variation that may affect individual’s susceptibility to cancer. Further, emerging evidence has shown that SNPs may be used as promising biomarker of individual genetic background to envisage therapeutic responses and prognosis in cancer patients, thus representing an interesting field of cancer research [3,4].
The deleted in colorectal carcinoma (DCC) is a well familiar tumor suppressor gene that functions in cell migration, cell cycle arrest and apoptosis, and has been found to be frequently deregulated or inactivated in various cancers [5,6,7]. Loss of heterozygosity (LOH), the most common genetic alteration of the DCC gene, is established to be implicated in pathogenesis of various cancers [8,9]. Further, DCC gene variants have been associated with increased susceptibility of various cancers. DCC rs714 A > G polymorphism, the most widely studied SNP of DCC gene, is LOH marker associated with decreased expression of DCC and with increased risk of colorectal and gallbladder cancer [10,11,12,13]. However, the published articles have generally been confined in terms of sample size, ethnicity and study designs.
Prostate stem cell antigen (PSCA) is a member of Ly-6/Thy-1 family of glycosylphosphatidyl-inositol (GPI)-anchored cell-surface proteins having a crucial role in cell adhesion, proliferation, and survival [14]. PSCA was found to be aberrantly expressed in several human cancers, and since it has restricted expression in normal tissues, PSCA represents an ideal target for cancer diagnosis and therapy [15,16,17,18,19,20,21]. Human PSCA gene maps on chromosome 8q24.2 containing 464 SNPs. rs2294008 C > T and rs2976392 G > A are the most extensively studied SNPs in the PSCA gene shown to be associated with increased risk of bladder and stomach cancer [22,23]. However, in our previous study, we failed to find an association between rs2294008 SNP and gallbladder cancer risk [24]. A number of studies have also investigated the association of these SNPs with various cancer susceptibility, though the results are discrepant as the PSCA gene function in a tissue/organ specific manner, i.e., act as an oncogene in some cancers while tumor suppressor gene in others [25,26,27,28].
Considering the panoptic role of DCC (rs714) and PSCA (rs2294008, rs2976392) polymorphism in the carcinogenesis, and increasing number of reports on different cancer in recent years, there is a prerequisite to reconcile all the discordant results to clarify its role in cancer susceptibility. Since meta-analysis represents an effective way to merge information from several studies dealing with the same concern, we performed a meta-analysis of all eligible case-control studies to better interpret the associations between these SNPs and cancer.
2. Materials and Methods
We adopted the statement of PRISMA for reporting meta-analysis [29].
2.1. Literature Search
A systematic and comprehensive literature search was performed from electronic database to find all the published case-control studies on the association of DCC (rs714 A > G) and PSCA (rs2294008 C > T and rs2976392 G > A) polymorphism with cancer susceptibility until September 2015. The search strategies were without time or geographical restriction, but limited to human-associated studies and English language papers. The “Pubmed”, “Medline”, “Google Scholar”, “EMBASE”, and “Scopus” database were examined using the following MeSH index keywords: “prostate stem cell antigen”, “DCC rs714 (A > G)”, “PSCA rs2294008 (C > T) and/or rs2976392 (G > A)”, “single nucleotide polymorphism (SNP)/variation/genotype”, in combination with “Cancer/carcinoma” or “tumor”. The titles and abstracts of potential articles were sorted to achieve their relevancy, and irrelevant studies were left off. Additional relevant studies were collected through manual examination of reference list of the retrieved articles and previous reviews on the topic.
2.2. Study Selection
The selection criteria of the study were (1) original case-control study accounting the association of DCC (rs714 A > G) and PSCA (rs2294008 C > T or rs2976392 G > A) polymorphism with cancer; (2) studies with sufficient information to estimate the relative risk and 95% confidence intervals (CI); (3) enlisting pathologically confirmed incident cancer cases; (4) studies including only cancer-free (healthy) controls; (5) concordance of genotypic frequencies with Hardy-Weinberg equilibrium (HWE) in controls.
The major exclusion criteria were as follows: (1) ecological studies, case reports, reviews, abstract, comment and editorials; (2) articles published in a language other than English; (3) lack of control population; (4) studies with benign, hyperplasia or other related pre-malignant taken as controls; (5) insufficient data; (6) duplicate studies; (7) not for cancer research; (8) not in accordance with Hardy-Weinberg equilibrium in control groups.
2.3. Data Extraction
The qualification evaluation of each eligible study was carried out by two investigators separately and the information was cautiously extracted from all eligible publications according to the inclusion and exclusion criteria listed above. Any disagreements were further discussed and resolved by consensus.
Data including first author name, year of publication, country of origin, ethnicity, genotyping methods, cancer types, frequency of cases and controls, genotype frequency, minor allelic frequencies, etc., were extracted from each study. If identical data were reported in more than one publication or had previously been reported somewhere else, only the original report with the largest sample size was included. Articles covering different ethnic groups and different countries or different cancer were viewed as different studies for each category cited above. Subgroup analysis, stratified by cancer type and ethnicity was also performed. Those cancer types appeared in only one or two studies, were placed into the “other cancers” subgroup. Ethnicity was classified as Caucasian, Asian and Mixed.
2.4. Statistical Analysis
The intensity level of association between studied SNPs and cancer susceptibility was assessed by computing crude ORs and corresponding 95% CI. The pooled ORs was estimated for allele contrast, log-additive, dominant, and recessive models. Deviation from HWE was analyzed by using the Chi-square goodness of fit test (significant at the 0.05 level). The analyses were stratified on the basis of cancer types (gastric cancer/GC, bladder cancer/BC and others) and ethnicity (Asian and Caucasian). Chi-square-based Q statistics was calculated to evaluate the heterogeneity across the studies, and it was considered significant at p < 0.05. Heterogeneity was measured using the I2 value, the percentage of variation across studies that are due to heterogeneity rather than chance. The value of I2 = 0%, 25%, 50% and 75% represent no observed heterogeneity, low, moderate, and high heterogeneity, respectively [30]. The pooled ORs were calculated by the fixed-effect model in case of no heterogeneity [31] otherwise, a random-effect model was used [32]. Moreover, a sensitivity analysis was performed to check if the alteration of inclusion criteria affects the results of the meta-analysis. For this, the meta-analysis estimates were computed after excluding one study at a time. The publication bias was assessed graphically using Funnel plot, and the plot asymmetry was investigated by Egger test [33] and p < 0.05 was considered as statistically significant publication bias. All of the statistical analyses were done by Comprehensive Meta-analysis software (Version 2.0, BIOSTAT, Englewood, NJ, USA).
3. Result
3.1. Study Characteristics
According to the search strategy mentioned above, only four articles were found eligible for DCC (rs714 A > G) meta-analysis [10,12,13,34]. Among them, Malik et al. (2013) analyzed the association of rs714 polymorphism with gastric cancer (GC) and esophageal cancer (EC), and hence these were counted as two different studies [12]. Thus a total of five studies from four articles with a total of 1018 multiple cancer cases and 952 controls was included for DCC rs714 A > G meta-analysis.
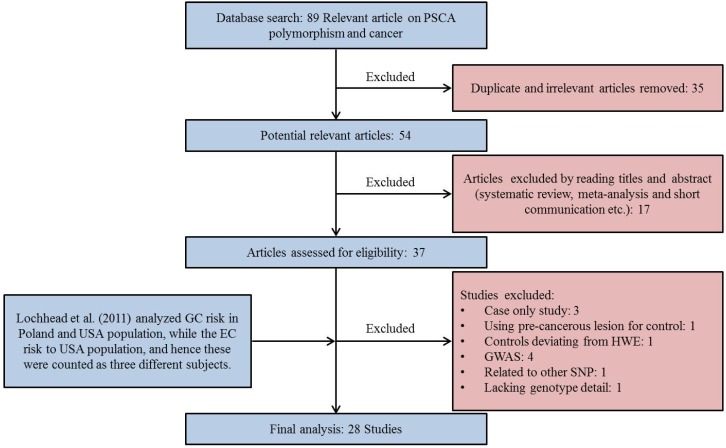
For PSCA meta-analysis, a total of 27 articles ([24,28,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58] Figure 1) were found eligible. Remarkably, the study by Lochhead et al. (2011) analyzed the association of rs2294008 polymorphism with GC risk in Poland and USA population, while the EC risk to USA population, and hence these were counted as three different studies [42]. However, the frequency of PSCA SNP deviated from HWE in Poland control subjects, hence excluded. Finally, 28 studies from 27 articles met our established inclusion criteria for rs2294008 with a total of 17,479 multiple cancer cases and 19,799 controls. Among them only 11 study (with a total of 5970 multiple cancer cases and 5707 controls) investigated the rs2976392 polymorphism in various cancers [27,36,37,38,41,44,47,53,54,57,58].
Figure 1.
Flow chart of study selection for Prostate Stem cell antigen (PSCA) rs2294008 polymorphism. The study by Lochhead et al. (2011) [42] involved three case-control studies out of which one study was excluded because of deviation from Hardy-Weinberg equilibrium (HWE) in control population, so the number of case-control studies are different than number of articles included in the meta-analysis.
The characteristics of eligible studies included in the analysis are presented in Table 1. All studies were retrospective case-control studies using validated genotyping methods and genotype frequencies in the control cohort were in accordance with Hardy-Weinberg equilibrium (HWE).
Table 1.
Studies included in meta-analysis.
| SN | Author | Reference | Country | Ethnicity | Cancer Type | Case/Control | pHWE | MAF | Genotyping Method |
|---|---|---|---|---|---|---|---|---|---|
| DCC rs714 (A > G) | |||||||||
| 1 | Toma et al., 2009 | [34] | Romania | Caucasian | CRC | 120/60 | 0.603 | 0.28 | PCR-RFLP |
| 2 | Rai et al., 2013 | [10] | India | Asian | GBC | 406/260 | 0.062 | 0.38 | PCR-RFLP |
| 3 | Malik et al., 2013 | [12] | India | Asian | EC | 135/195 | 0.187 | 0.36 | PCR-RFLP |
| 4 | Malik et al., 2013 | [12] | India | Asian | GC | 108/195 | 0.187 | 0.36 | PCR-RFLP |
| 5 | Djansugurova et al., 2015 | [13] | Kazakhstan | Mixed | CRC | 249/242 | 0.187 | 0.36 | PCR-RFLP |
| PSCA rs2294008 (C > T) | |||||||||
| 1 | Wu et al., 2009 | [36] | China | Asian | GC | 1736/1020 | 0.587 | 0.28 | PCR-RFLP |
| 2 | Matsuo et al., 2009 | [27] | Japan | Asian | GC | 708/708 | 0.638 | 0.38 | Taqman |
| 3 | Wang et al., 2010 | [28] | China | Asian | BC | 581/580 | 0.508 | 0.27 | PCR-RFLP |
| 4 | Lu et al., 2010 | [37] | China | Asian | GC | 1053/1100 | 0.166 | 0.25 | PCR-RFLP |
| 5 | Ou et al., 2010 | [38] | China | Asian | GC | 196/246 | 0.924 | 0.27 | PCR-LDR |
| 6 | Zeng et al., 2011 | [39] | China | Asian | GC | 460/549 | 0.493 | 0.27 | PCR-RFLP |
| 7 | Song et al., 2011 | [40] | Korea | Asian | GC | 3245/1700 | 0.131 | 0.48 | PCR-RFLP |
| 8 | Joung et al., 2011 | [41] | Korea | Asian | PC | 194/169 | 0.963 | 0.47 | MASS ARRAY |
| 9 | Lochhead et al., 2011 | [42] | USA | Caucasian | EC | 159/211 | 0.405 | 0.5 | Taqman |
| 10 | Lochhead et al., 2011 | [42] | USA | Caucasian | GC | 309/211 | 0.405 | 0.5 | Taqman |
| 11 | Sala et al., 2012 | [43] | Europe | Caucasian | GC | 411/1530 | 0.088 | 0.44 | SNP ARRAY |
| 12 | Kim et al., 2012 | [44] | Korea | Asian | BrC | 456/461 | 0.324 | 0.49 | MALDI-TOF MS |
| 13 | Smith et al., 2012 | [45] | Scotland | Caucasian | CRC | 77/804 | 0.981 | 0.4 | Taqman |
| 14 | Li et al., 2012 | [46] | China | Asian | GC | 300/300 | 0.65 | 0.26 | MASS-ARRAY IPLEX |
| 15 | Ono et al., 2013 | [47] | Japan | Asian | GBC | 44/173 | 0.242 | 0.39 | Taqman |
| 16 | Ma et al., 2013 | [48] | China | Asian | BC | 184/962 | 0.562 | 0.25 | MASS-ARRAY IPLEX |
| 17 | Zhao et al., 2013 | [35] | China | Asian | GC | 717/951 | 0.913 | 0.3 | PCR-DHPLC |
| 18 | Rai et al., 2013 | [24] | India | Asian | GBC | 405/247 | 0.492 | 0.43 | Taqman |
| 19 | Dai et al., 2014 | [49] | China | Asian | EC | 2083/2220 | 0.944 | 0.27 | Taqman |
| 20 | Sun et al., 2014 | [50] | Texas | Caucasian | GC | 132/125 | 0.926 | 0.49 | Taqman |
| 21 | Wang et al., 2014 | [51] | China | Asian | BC | 1210/1008 | 0.739 | 0.25 | Taqman |
| 22 | Lee et al., 2014 | [52] | Korea | Asian | BC | 411/1700 | 0.13 | 0.48 | HRM |
| 23 | Kupcinskas et al., 2014 | [53] | Lithuania | Caucasian | GC | 252/246 | 0.834 | 0.48 | Taqman |
| 24 | Sun et al., 2015 | [54] | China | Asian | GC | 692/774 | 0.105 | 0.28 | Taqman |
| 25 | MA et al., 2015 | [55] | Spain | Caucasian | GC | 603/675 | 0.349 | 0.45 | Taqman |
| 26 | Ichikawa et al., 2015 | [56] | Japan | Asian | GC | 193/266 | 0.185 | 0.42 | PCR-RFLP |
| 27 | Zhang et al., 2015 | [57] | China | Asian | GC | 476/481 | 0.617 | 0.27 | MASS ARRAY |
| 28 | Kupcinskas et al., 2015 | [58] | Latvia | Caucasian | CRC | 192/382 | 0.943 | 0.48 | Taqman |
| PSCA rs2976392 (G > A) | |||||||||
| 1 | Wu et al., 2009 | [36] | China | Asian | GC | 1724/1002 | 0.35 | 0.29 | PCR-RFLP |
| 2 | Matsuo et al., 2009 | [27] | Japan | Asian | GC | 707/707 | 0.635 | 0.37 | Taqman |
| 3 | Lu et al., 2010 | [37] | China | Asian | GC | 1043/1082 | 0.336 | 0.26 | PCR-RFLP |
| 4 | Ou et al., 2010 | [38] | China | Asian | GC | 196/246 | 0.298 | 0.26 | PCR-LDR |
| 5 | Joung et al., 2011 | [41] | Korea | Asian | PC | 194/168 | 0.848 | 0.47 | MASS ARRAY |
| 6 | Kim et al., 2012 | [44] | Korea | Asian | BrC | 453/460 | 0.397 | 0.49 | MALDI-TOF MS |
| 7 | Ono et al., 2013 | [47] | Japan | Asian | GBC | 44/173 | 0.328 | 0.61 | Taqman |
| 8 | Kupcinskas et al., 2014 | [53] | Lithuania | Caucasian | GC | 249/232 | 0.986 | 0.48 | Taqman |
| 9 | Sun et al., 2015 | [54] | China | Asian | GC | 692/774 | 0.13 | 0.29 | Taqman |
| 10 | Zhang et al., 2015 | [57] | China | Asian | GC | 476/481 | 0.939 | 0.28 | MASS ARRAY |
| 11 | Kupcinskas et al., 2015 | [58] | Latvia | Caucasian | CRC | 192/382 | 0.856 | 0.48 | Taqman |
GC—Gastric cancer, BC—Bladder cancer, GBC—Gallbladder cancer, EC—Esophageal cancer, BrC—Breast Cancer, CRC—Colorectal cancer, PC—Prostate Cancer, HWE Hardy—Weinberg equilibrium, MAF—Minor allelic frequency, PCR—Polymerase chain reaction, RFLP—Restriction fragment length polymorphism, LDR—Ligation detection reaction, DHPLC—Denaturing high performance liquid chromatography, HRM—High-resolution melting, SNP—Single nucleotide polymorphism, MALDI-TOF-MS—Matrix Assisted Laser Desorption/Ionization Time of Flight Mass Spectrometry.
3.2. Quantitative Synthesis
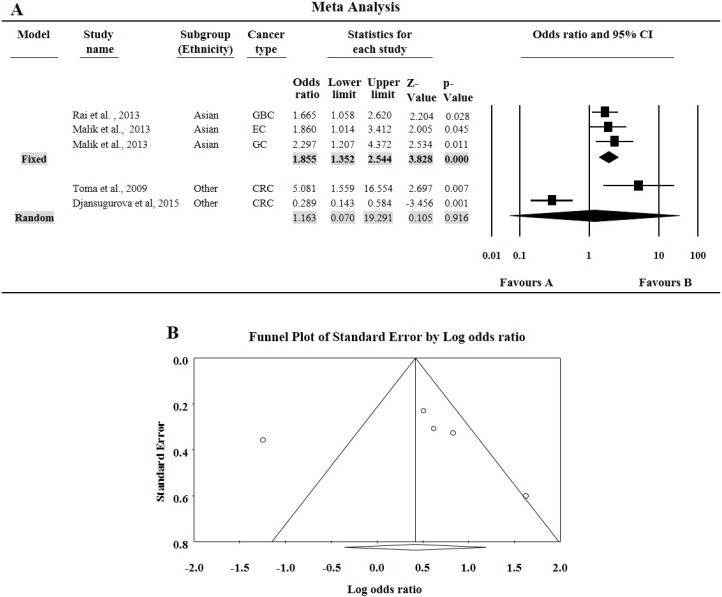
The minor allele frequency (MAF) for rs714 SNP varies from 28% to 38% (Table 2). For rs714 A > G polymorphism, none of the genotypic combination was found to affect the risk of overall cancer compared with the wild genotype. Since there are only five studies we did not perform subgroup analysis except for ethnicity. In Asian subgroups, having three studies with a total number of 649 multiple cancer cases and 650 controls, all the four genotypic model were found to significantly associated with increased risk of cancer (A vs. G: OR = 1.41, 95% CI = 1.20–1.66, p ≤ 0.000; AA vs. GG: OR = 1.86, 95% CI = 1.35–2.54, p ≤ 0.000; GA vs. GG: OR = 1.43, 95% CI = 1.11–1.85, p = 0.005; GA + AA vs. GG: OR = 1.66, 95% CI = 1.31–2.09, p ≤ 0.000; AA vs. GG + GA: OR = 1.52, 95% CI = 1.14–2.03, p = 0.004, Figure 2A.
Table 2.
Meta-analysis Result for DCC rs714 A > G polymorphism.
| Variables | N | Case/Control | A vs. G Allele | AA vs. GG | GA vs. GG | GA + AA vs. GG | AA vs. GG + GA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | |||
| All | 5 | 1018/952 | 1.31 (0.93–1.86) | 0.121 | 0.000/84.033 | 1.52 (0.70–3.3) | 0.289 | 0.000/85.434 | 1.37 (0.98–1.92) | 0.068 | 0.032 62.210 | 1.49 (0.98–2.28) | 0.063 | 0.001/79.104 | 1.27 (0.64–2.52) | 0.495 | 0.000/84.117 |
| Ethnicity | |||||||||||||||||
| Caucasian | 1 | 120/60 | 2.14 (1.34–3.43) | 0.002 | 1.000/0.000 | 5.08 (1.56–16.55) | 0.007 | 1.000/0.000 | 2.53 (1.29–4.97) | 0.007 | 1.000/0.000 | 2.87 (1.50–5.50) | 0.001 | 1.000/0.000 | 2.97 (0.97–9.09) | 0.056 | 1.000/0.000 |
| Asian | 3 | 649/650 | 1.41 (1.20–1.66) | 0.000 | 0.810/0.000 | 1.86 (1.35–2.54) | 0.000 | 0.725/0.000 | 1.43 (1.11–1.85) | 0.005 | 0.107 55.174 | 1.66 (1.31–2.09) | 0.000 | 0.182/41.288 | 1.52 (1.14–2.03) | 0.004 | 0.193/39.43 |
| Mixed | 1 | 249/242 | 0.70 (0.54–0.92) | 0.011 | 1.000/0.000 | 0.29 (0.14–0.58) | 0.001 | 1.000/0.000 | 0.99 (0.68–1.44) | 0.975 | 1.000/0.000 | 0.81 (0.57–1.16) | 0.246 | 1.000/0.000 | 0.29 (0.15–0.57) | 0.000 | 1.000/0.000 |
Significant associations are shown in bold, ph—p value of Q test for heterogeneity, OR—Odds Ratio, CI—Confidence Interval.
Figure 2.
(A) Forest plots for meta-analysis of DCC rs714 polymorphism (AA vs. GG) and cancer risk after ethnicity based stratification. For each study, the estimates of odds ratio (OR) and 95% confidence interval (CI) were plotted with square and horizontal line. The size of the square points is the relative weight of the respective study. Diamond indicates the pooled OR and its 95% CI; (B) Funnel plot analysis to detect publication bias for the Deleted in colorectal carcinoma (DCC) rs714 polymorphism (AA vs. GG) and overall cancer risk. Each dot represents an individual study for the indicated association. Areas of squares of individual studies are inversely proportional to the variance of the log odds ratios and the horizontal lines represent CIs.
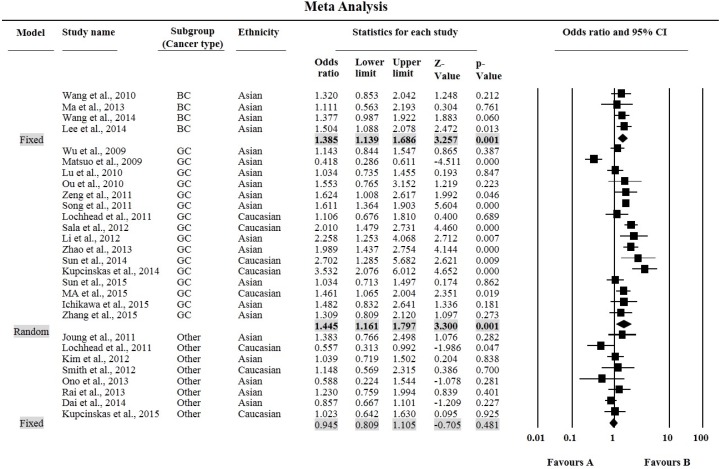
The MAF for PSCA rs2294008 polymorphism varies as 25%–49% in Asians, and 40%–50% in Caucasians. The results of our meta-analysis are shown in Table 3. Overall, the individuals carrying the TT or CT genotype were at an increased risk of cancer compared with the CC genotype (TT: OR = 1.28, 95% CI = 1.10–1.50, p = 0.002, Figure 3 and CT: OR = 1.21, 95% CI = 1.09–1.34, p ≤ 0.0001, respectively, Table 3.). Moreover, significant associations were also found in T vs. C allele (OR = 1.16, 95% CI = 1.07–1.25, p ≤ 0.0001.), as well as in dominant (CT + TT vs. CC: OR = 1.24, 95% CI = 1.11–1.39, p ≤ 0.0001) and recessive models (TT vs. CC + CT: OR = 1.17, 95% CI = 1.05–1.30, p = 0.005), in the pooled analyses. When stratifying by cancer type, significantly increased risk was limited to gastric cancer and bladder cancer in all genetic models except for the recessive model for bladder cancer. Further, subgroup analyses based on ethnicity showed that rs2294008 polymorphism modulate the risk of cancer in Caucasian ethnicity with only TT genotype and recessive model, while in the Asian ethnicity subgroup, all genetic models (except recessive model) were associated with increased cancer risk (Table 3).
Table 3.
Meta-analysis Result for PSCA rs2294008 C > T polymorphism.
| Variables | N | Case/Control | T vs. C Allele | TT vs. CC | CT vs. CC | CT + TT vs. CC | TT vs. CC + CT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | |||
| All | 28 | 17,479/19,799 | 1.16 (1.07–1.25) | 0.000 | 0.000/79.335 | 1.28 (1.10–1.50) | 0.002 | 0.000/74.804 | 1.21 (1.09–1.34) | 0.000 | 0.000/75.122 | 1.24 (1.11–1.39) | 0.000 | 0.000/80.158 | 1.17 (1.05–1.30) | 0.005 | 0.000/60.832 |
| Ethnicity | |||||||||||||||||
| Caucasian | 8 | 2135/4184 | 1.20 (0.99–1.45) | 0.053 | 0.000/79.874 | 1.45 (1.02–2.08) | 0.040 | 0.000/78.000 | 1.03 (0.75–1.40) | 0.877 | 0.000/78.481 | 1.16 (0.84–1.60) | 0.373 | 0.000/82.426 | 1.46 (1.28–1.66) | 0.000 | 0.120/38.884 |
| Asian | 20 | 15,344/15,615 | 1.14 (1.05–1.24) | 0.002 | 0.000/79.288 | 1.22 (1.03–1.45) | 0.020 | 0.000/73.249 | 1.27 (1.14–1.41) | 0.000 | 0.000/74.134 | 1.27 (1.13–1.43) | 0.000 | 0.000/80.253 | 1.08 (0.96–1.22) | 0.262 | 0.001/57.234 |
| Cancer type | |||||||||||||||||
| BC | 4 | 2386/4250 | 1.21 (1.12–1.32) | 0.000 | 0.992/0.000 | 1.39 (1.14–1.69) | 0.001 | 0.873/0.000 | 1.37 (1.21–1.54) | 0.000 | 0.576/0.000 | 1.36 (1.22–1.53) | 0.000 | 0.689/0.000 | 1.12 (0.945–1.33) | 0.192 | 0.848 /0.000 |
| GC | 16 | 11,483/10,882 | 1.21 (1.09–1.35) | 0.000 | 0.000/83.251 | 1.45 (1.16–1.78) | 0.001 | 0.000/80.616 | 1.30 (1.16–1.45) | 0.000 | 0.000/62.932 | 1.36 (1.19–1.55) | 0.000 | 0.000/76.780 | 1.25 (1.07–1.47) | 0.007 | 0.000/72.933 |
| Other Cancer | 8 | 3610/4667 | 0.96 (0.90–1.03) | 0.291 | 0.218/26.402 | 0.95 (0.81–1.11) | 0.481 | 0.321/13.908 | 0.90 (0.72–1.11) | 0.312 | 0.013/60.713 | 0.92 (0.75–1.11) | 0.383 | 0.019/58.256 | 1.02 (0.89–1.17) | 0.765 | 0.552/0.000 |
Significant associations are shown in bold, ph—p value of Q test for heterogeneity, OR—Odds Ratio, CI—Confidence Interval.
Figure 3.
Forest plots for meta-analysis of PSCA rs2294008 C > T polymorphism (TT vs. CC) and cancer risk after cancer site based stratification. For each study, the estimates of OR and 95% CI were plotted with square and horizontal line. The size of the square points is the relative weight of the respective study. Diamond indicates the pooled OR and its 95% CI.
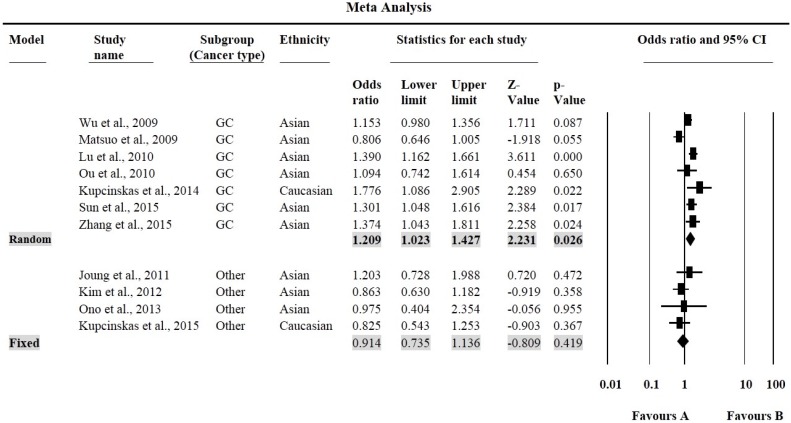
The MAF for rs2976392 SNP varies from 26% to 48% (Table 4). For, rs2976392 G > A polymorphism, individuals carrying the GA genotype were at an increased risk of only GC cancer (OR = 1.21, 95% CI = 1.02–1.43, p = 0.026, Figure 4).
Table 4.
Meta-analysis Result for PSCA rs2976392 G > A polymorphism.
| Variables | N | Case/Control | A vs. G Allele | AA vs. GG | GA vs. GG | GA + AA vs. GG | AA vs. GG + GA | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | OR (95% CI) | p | ph/I2 | |||
| All | 11 | 5970/5707 | 1.09 (0.95–1.25) | 0.210 | 0.000/81.116 | 1.10 (0.82–1.48) | 0.654 | 0.000/78.184 | 1.13 (0.98–1.31) | 0.087 | 0.004/61.549 | 1.161 (0.93–1.33) | 0.256 | 0.000/77.837 | 1.04 (0.82–1.32) | 0.756 | 0.000/73.621 |
| Ethnicity | |||||||||||||||||
| Caucasian | 2 | 431/614 | 1.39 (0.77–2.51) | 0.281 | 0.001/90.899 | 1.90 (0.60–6.03) | 0.276 | 0.001/90.399 | 1.20 (0.57–2.54) | 0.639 | 0.020/81.566 | 1.22 (0.36–4.19) | 0.753 | 0.000/94.07 | 1.66 (0.88–3.13) | 0.120 | 0.024/80.307 |
| Asian | 9 | 5053/4612 | 1.04 (0.91–1.19) | 0.540 | 0.000/76.841 | 0.981 (0.75–1.28) | 0.891 | 0.001/69.334 | 1.13 (0.98–1.31) | 0.100 | 0.008/61.119 | 1.10 (0.94–1.30) | 0.242 | 0.000/71.634 | 0.93 (0.75–1.16) | 0.529 | 0.010/60.305 |
| Cancer type | |||||||||||||||||
| GC | 7 | 5087/4524 | 1.14 (0.95–1.38) | 0.165 | 0.000/87.766 | 1.16 (0.76–1.77) | 0.498 | 0.000/86.220 | 1.21 (1.02–1.43) | 0.026 | 0.003/69.157 | 1.22 (0.99–1.50) | 0.066 | 0.000/82.190 | 1.04 (0.73–1.48) | 0.829 | 0.000/82.477 |
| Other Cancer | 4 | 873/1183 | 1.02 (0.90–1.16) | 0.264 | 0.428/0.000 | 1.05 (0.82–1.35) | 0.713 | 0.000/0.520 | 0.91 (0.74–1.14) | 0.419 | 0.676/0.000 | 0.87 (0.71–1.07) | 0.189 | 0.210/33.715 | 1.10 (0.89–1.36) | 0.365 | 0.349/8.804 |
Significant associations are shown in bold, ph—p value of Q test for heterogeneity, OR—Odds Ratio, CI—Confidence Interval.
Figure 4.
Forest plots for meta-analysis of PSCA rs2976392 G > A polymorphism (GA vs. GG) and cancer risk stratified by cancer site. For each study, the estimates of OR and 95% CI were plotted with square and horizontal line. The size of the square points is the relative weight of the respective study. Diamond indicates the pooled OR and its 95% CI.
3.3. Tests of Heterogeneity and Sensitivity Analysis
The present meta-analysis revealed significant heterogeneity for all studied SNPs. For rs714 polymorphism, the removal of the study by Djansugurova et al. (2015) [13] was found to remove heterogeneity in all genotype models (AA vs. GG: ph = 0.354, I2 = 7.759; GA vs. GG: ph = 0.077, I2 = 56.193; GA + AA vs. GG: ph = 0.119, I2 = 48.666; AA vs. GG + GA: ph = 0.205, I2 = 34.523; A vs. G: ph = 0.376, I2 = 3.346). However, it was found to significantly change the pooled result.
For PSCA polymorphism, our sensitivity analysis showed that removal of the studies by Lochhead et al. (2011) [42], Matsuo et al. (2009) [27], Kupcinskas et al. (2014) [53] and Dai et al. (2014) [49] collectively abolished heterogeneity at the allele (T vs. C: ph = 0.056, I2 = 34.210) and heterogenotype level (CT vs. CC: ph = 0.090, I2 = 29.731), without significantly influencing the pooled ORs of the overall cancer risk. Similarly, Dai et al. (2014) [49], Kupcinskas et al. (2014) [53], Kupcinskas et al. (2015) [58], Lochhead et al. (2011) [42] and Matsuo et al. (2009) [27] seemed to be responsible for heterogeneity at variant level (TT vs. CC: ph = 0.053, I2 = 35.265) as well as in dominant model (CT + TT vs. CC: ph = 0.098, I2 = 29.281) while only Kupcinskas et al. (2014) [53] and Matsuo et al. (2009) [27] were responsible for heterogeneity in recessive models (TT vs. CC + CT: ph = 0.143, I2 = 25.154). Further, our sensitivity analysis affirmed the consistency of the results and the corresponding pooled ORs were not significantly altered by any single study in the entire four genetic models .
For rs2976392 polymorphism, the removal of the studies by Matsuo et al. (2009) [27], Kupcinskas et al. (2014) [53] collectively abolished heterogeneity in all log additive and recessive genonotypic model (AA vs. GG: ph = 0.928, I2 = 0.000; GA vs. GG: ph = 0.150, I2 = 33.533; AA vs. GG + GA: ph = 0.893, I2 = 0.000; A vs. G: ph = 0.586, I2 = 0.000). However, dominant model required the removal of Matsuo et al. (2009) [27], Kupcinskas et al. (2014) [53] and Kupcinskas et al. (2015) [58] to remove heterogeneity (GA + AA vs. GG: ph = 0.328, I2 = 13.123).
3.4. Publication Bias
DCC rs714 polymorphism showed funnel plot symmetry in all genetic models. Egger’s test (AA vs. GG: t = 0.146, p = 0.893, Figure 2B.; GA vs. GG: t = 0.275, p = 0.801; GA + AA vs. GG: t = 0.569, p = 0.609; AA vs. GA + GG: t = 0.153, p = 0.566; and A vs. G allele: t = 0.875, p = 0.446) as well as Begg and Mazumdar rank correlation (AA vs. GG: p2tailed = 893; GA vs. GG: p2tailed = 0.807; GA + AA vs. GG: p2tailed = 0.807; AA vs. GA + GG: p2tailed = 1.000 and A vs. G allele: p2tailed = 0.221) also confirmed the funnel plot symmetry.
For PSCA polymorphism, a review of funnel plot also demonstrated no apparent asymmetry in all comparison models; in the overall and subgroup meta-analysis (Figure 5). Egger’s test also did not indicate any evidence of publication bias and statistically establish the funnel plot symmetry (for rs2294008—TT vs. CC: t = 0.466, p = 0.645; CT vs. CC: t = 0.573, p = 0.572; CT + TT vs. CC: t = 874, p = 0.390; TT vs. CT + CC: t = 0.634, p = 0.549; and T vs. A allele: t = 0.351, p = 0.728, and for rs2976392 SNP, AA vs. GG: t = 0.349, p = 0.735; GA vs. GG: t = 0.387, p = 0.708; GA + AA vs. GG: t = 0.261, p = 0.800; AA vs. GA + GG: t = 0.133, p = 0.897; and A vs. G allele: t = 0.150, p = 0.884). Similarly, Begg and Mazumdar rank correlation test also did not indicate any publication bias (for rs2294008—TT vs. CC: p2tailed = 0.921; CT vs. CC: p2tailed = 0.678; CT + TT vs. CC: p2tailed = 0.890; TT vs. CT + CC: p2tailed = 0.387 and T vs. A allele: p2tailed = 0.621 and for rs2976392 AA vs. GG: p2tailed = 0.876; GA vs. GG: p2tailed = 0.756; GA + AA vs. GG: p2tailed = 0.756; AA vs. GA + GG: p2tailed = 1.000 and A vs. G allele: p2tailed = 0.756) suggesting that our results were statistically robust.
Figure 5.
(A) Funnel plot analysis to detect publication bias for the PSCA rs2294008 C > T polymorphism (TT vs. CC). Each dot represents an individual study for the indicated association. Areas of squares of individual studies are inversely proportional to the variance of the log odds ratios and the horizontal lines represent CIs; (B) Funnel plot analysis to detect publication bias for the PSCA rs2976392 G > A polymorphism (GA vs. GG). Each dot represents an individual study for the indicated association. Areas of squares of individual studies are inversely proportional to the variance of the log odds ratios and the horizontal lines represent CIs.
4. Discussion
In the present meta-analysis, we found that DCC rs714 conferred a significantly increased risk of cancer only in Asians. Previously, it was shown to be associated with GBC, GC and EC in Asian population [10,12]. Toma et al. (2009) showed increased risk of CRC in Caucasians [34], though our meta-analysis is limited for Caucasian ethnicity due to lack of published data. On the other hand, a study by Djansugurova et al. (2015) involving mixed population showed that A allele of rs714 confers protection against the CRC risk [13].
We also established that the PSCA rs2294008 polymorphism is significantly associated with increased cancer susceptibility, overall. However, the estimate of the association is predominantly determined by that for gastric and bladder cancer as we failed to detect the association of PSCA rs2294008 polymorphism with other cancer risk. This may be ascribable to the fact that different cancer has a different molecular mechanism of the disease process and the number of studies is limited in other cancer subgroups. Further, the significant association of this polymorphism with cancer was more prominent in Asians as compared to Caucasians. A previous meta-analysis also showed that PSCA rs2294008C > T polymorphism is closely associated with increased risk of GC for Eastern Asians [59]. Though we have excluded GWAS studies from our meta-analysis, our results are in agreement with the previous GWAS studies [22,23,60] and meta-analysis investigating the association of rs2294008 polymorphism with cancer risk, including gastric [59,61,62,63,64,65,66] and bladder cancer [67,68]. These findings suggested rs2294008 as a most promising genetic marker for GC and BC susceptibility. Although, the exact mechanism of PSCA to promote carcinogenesis remains unclear, its expression has been associated with the malignant progression of pre-malignant lesions and advanced clinical stage and metastasis in prostate cancer [25]. The rs2294008 C > T is located in exon 1, and in vitro experiments have revealed that the variant is associated with the reduced transcriptional activity of an upstream fragment of PSCA [22,35].
In contrast, we did not find any association of PSCA rs2976392 SNP with cancer risk. Previously, heterogenotype and dominant model of rs2976392 was found to confer significantly increased risk of GC, specifically in females or non-cardia GC [36,54]. Lu et al. (2010) also showed a significant association of this SNP with GC risk [37] while other studies showed no association [41,44,47]. Moreover, previous meta-analysis also demonstrated that the rs2976392 SNP conferred increased risk of GC [59,61,62,63,65,68]. This discrepancy may be due to the inclusion of GWAS studies which is the largest number of association studies dominating the result of pooled analysis in all previous meta-analysis. The rs2976392G > A positioned in intron 2 is in strong linkage disequilibrium with rs2294008C > T, and its function is unclear till yet [61]. Hence, the positive association observed in various case-control studies may be due to the linkage effect of rs2294008 polymorphism.
Our study is the most up-to-date study, including all the published case-control studies in English language until September 2015. However, like other studies, we also have some flaws such as; possibility of selection biases due to study selection based on English language only and different genotyping methods. Likewise, the number of available studies were not sufficient in subgroup analysis, such as for other cancers, Cacuasians and mixed populations to perform a comprehensive analysis. Thus, our study is not a complete cancer analysis but is limited to the Asian population and specific cancer (BC and GC) for rs714 and rs2294008 polymorphism, respectively. Furthermore, our association analysis was based on unadjusted or crude estimates and the roles of gene-gene, gene-environment interactions, as well as linkage disequilibrium was not considered. Further analysis considering all these is required to make a more appropriate association of DCC and PSCA gene variants in modulation of cancer risk.
Study Advantage
Since we pooled large number of cases and controls from various studies, our study has improved statistical power of the analysis. In addition, we adopted a stringent inclusion/exclusion touchstone to include the well-defined case-control studies in the present meta-analysis. We have excluded GWAS thus preventing the likely bias. We also performed sensitivity analysis confirming the stability of our meta-analysis results in all models.
5. Conclusions
Our meta-analysis results showed that DCC rs714 polymorphism was associated with increased risk of cancer in Asian populations. Further, we confirmed a firm association between the PSCA rs2294008 C > T polymorphism with increased susceptibility of gastric and bladder cancers, signifying PSCA rs2294008 polymorphism as potential biomarker for these cancers. However, since our study is limited for ethnicity (DCC rs714) and cancer types (PSCA rs2294008), further larger studies involving other cancers and other population are needed to perform a more rigorous comparative analysis to corroborate this conclusion and to assess the more accurate association between these polymorphisms and overall cancer risk.
Abbreviation
| PSCA | Prostate stem cell antigen |
| DCC | Deleted in Colorectal Carcinoma |
| SNP | Single nucleotide polymorphism |
| GBC | Gallbladder cancer |
| GC | Gastric cancer |
| EC | Esophageal cancer |
| BC | Bladder cancer |
| PC | Prostate cancer |
| CRC | Colorectal cancer |
| BrC | Breast cancer |
| OR | Odds ration |
| CI | Class interval |
| HWE | Hardy Weinberg Equilibrium |
| GWAS | Genome wide association study |
| PCR-RFLP | Polymerase chain reaction-restriction fragment length polymorphism |
| LDR | Ligation detection reaction |
| HRM | High-resolution melting (HRM) |
Author Contributions
R.R.: Collection and analysis of data, writing the manuscript. U.G., V.C., B.M.: Collection and analysis of data. J.J.K.: Editing the manuscript.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- 1.Sharma K.L., Rai R., Srivastava A., Sharma A., Misra S., Kumar A., Mittal B. A multigenic approach to evaluate genetic variants of PLCE1, LXRs, MMPs, TIMP, and CYP genes in gallbladder cancer predisposition. Tumour Biol. 2014;35:8597–8606. doi: 10.1007/s13277-014-2094-7. [DOI] [PubMed] [Google Scholar]
- 2.Umar M., Upadhyay R., Mittal B. PLCE1 rs2274223 A > G polymorphism and cancer risk: A meta-analysis. Tumour Biol. 2013;34:3537–3544. doi: 10.1007/s13277-013-0932-7. [DOI] [PubMed] [Google Scholar]
- 3.Savas S., Liu G. Genetic variations as cancer prognostic markers: Review and update. Hum. Mutat. 2009;30:1369–1377. doi: 10.1002/humu.21078. [DOI] [PubMed] [Google Scholar]
- 4.Guo X., Chen C., Liu B., Wu Y., Chen Y., Zhou X., Huang X., Li X., Yang H., Chen Z., et al. Genetic variations in monocarboxylate transporter genes as predictor of clinical outcomes in non-small cell lung cancer. Tumour Biol. 2015;36:3931–3939. doi: 10.1007/s13277-014-3036-0. [DOI] [PubMed] [Google Scholar]
- 5.Chen Y.Q., Hsieh J.T., Yao F., Fang B., Pong R.C., Cipriano S.C., Krepulat F. Induction of apoptosis and G2/M cell cycle arrest by DCC. Oncogene. 1999;18:2747–2754. doi: 10.1038/sj.onc.1202629. [DOI] [PubMed] [Google Scholar]
- 6.Castets M., Broutier L., Molin Y., Brevet M., Chazot G., Gadot N., Paquet A., Mazelin L., Jarrosson-Wuilleme L., Scoazec J.Y., et al. DCC constrains tumour progression via its dependence receptor activity. Nature. 2011;482:534–537. doi: 10.1038/nature10708. [DOI] [PubMed] [Google Scholar]
- 7.Krimpenfort P., Song J.Y., Proost N., Zevenhoven J., Jonkers J., Berns A. Deleted in colorectal carcinoma suppresses metastasis in p53-deficient mammary tumours. Nature. 2012;482:538–541. doi: 10.1038/nature10790. [DOI] [PubMed] [Google Scholar]
- 8.Khan N.P., Pandith A.A., Hussain M.U., Yousuf A., Khan M.S., Siddiqi M.A., Khrusheed A.W., Mudassar S. Loss of heterozygosity (LOH) of deleted in colorectal cancer (DCC) gene and predisposition to colorectal cancer: Significant association in colorectal cancer patients of Kashmir. J. Cancer Res. Exp. Oncol. 2011;3:88–94. [Google Scholar]
- 9.Bamias A.T., Bai M.C., Agnantis N.J., Michael M.C., Alamanos Y.P., Stefanaki S.V., Razi E.D., Skarlos D.V., Kappas A.M., Pavlidis N.A. Prognostic significance of the deleted in colorectal cancer gene protein expression in high-risk resected gastric carcinoma. Cancer Investig. 2003;21:333–340. doi: 10.1081/CNV-120018219. [DOI] [PubMed] [Google Scholar]
- 10.Rai R., Sharma K.L., Tiwari S., Misra S., Kumar A., Mittal B. DCC (deleted in colorectal carcinoma) gene variants confer increased susceptibility to gallbladder cancer (Ref. No.: Gene-D-12-01446) Gene. 2013;518:303–309. doi: 10.1016/j.gene.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 11.Cha P.C., Zembutsu H., Takahashi A., Kubo M., Kamatani N., Nakamura Y.J. A genome-wide association study identifies SNP in DCC is associated with gallbladder cancer in the Japanese population. Hum. Genet. 2012;57:235–237. doi: 10.1038/jhg.2012.9. [DOI] [PubMed] [Google Scholar]
- 12.Malik M.A., Gupta A., Zargar S.A., Mittal B. Role of genetic variants of deleted in colorectal carcinoma (DCC) polymorphisms and esophageal and gastric cancers risk in Kashmir Valley and meta-analysis. Tumour Biol. 2013;34:3049–3057. doi: 10.1007/s13277-013-0870-4. [DOI] [PubMed] [Google Scholar]
- 13.Djansugurova L., Zhunussova G., Khussainova E., Iksan O., Afonin G., Kaidarova D., Parker M.I. Association of DCC, MLH1, GSTT1, GSTM1, and TP53 gene polymorphisms with colorectal cancer in Kazakhstan. Tumour Biol. 2015;36:279–289. doi: 10.1007/s13277-014-2641-2. [DOI] [PubMed] [Google Scholar]
- 14.Raff A.B., Gray A., Kast W.M. Prostate stem cell antigen: Prospective therapeutic and diagnostic target. Cancer Lett. 2009;277:126–132. doi: 10.1016/j.canlet.2008.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Han K.R., Seligson D.B., Liu X., Horvath S., Shintaku P.I., Thomas G.V., Said J.W., Reiter R.E. Prostate stem cell antigen expression is associated with gleason score, seminal vesicle invasion and capsular invasion in prostate cancer. J. Urol. 2004;171:1117–1121. doi: 10.1097/01.ju.0000109982.60619.93. [DOI] [PubMed] [Google Scholar]
- 16.Amara N., Palapattu G.S., Schrage M., Gu Z., Thomas G.V., Dorey F., Said J., Reiter R.E. Prostate stem cell antigen is overexpressed in human transtitional cell carcinoma. Cancer Res. 2001;61:4660–4665. [PubMed] [Google Scholar]
- 17.Ono H., Hiraoka N., Lee Y.S., Woo S.M., Lee W.J., Choi I.J., Saito A., Yanagihara K., Kanai Y., Ohnami S., et al. Prostate stem cell antigen, a presumable organ-dependent tumor suppressor gene, is down-regulated in gallbladder carcinogenesis. Genes Chromosome Cancer. 2012;51:30–41. doi: 10.1002/gcc.20928. [DOI] [PubMed] [Google Scholar]
- 18.Zou Q., Yang L., Yang Z., Huang J., Fu X. PSCA and Oct-4 expression in the benign and malignant lesions of gallbladder: Implication for carcinogenesis, progression, and prognosis of gallbladder adenocarcinoma. Biomed. Res. Int. 2013;2013 doi: 10.1155/2013/648420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wente M.N., Jain A., Kono E., Berberat P.O., Giese T., Reber H.A., Friess H., Büchler M.W., Reiter R.E., Hines O.J. Prostate stem cell antigen is a putative target for immunotherapy in pancreatic cancer. Pancreas. 2005;31:119–125. doi: 10.1097/01.mpa.0000173459.81193.4d. [DOI] [PubMed] [Google Scholar]
- 20.Ramírez M.L., Nelson E.C., Evans C.P. Beyond prostate-specific antigen: Alternate serum markers. Prostate Cancer Prostatic Dis. 2008;11:216–229. doi: 10.1038/pcan.2008.2. [DOI] [PubMed] [Google Scholar]
- 21.Madu C.O., Lu Y. Novel diagnostic biomarkers for prostate cancer. J. Cancer. 2010;1:150–177. doi: 10.7150/jca.1.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sakamoto H., Yoshimura K., Saeki N., Katai H., Shimoda T., Matsuno Y., Saito D., Sugimura H., Tanioka F., Kato S., et al. Genetic variation in PSCA is associated with susceptibility to diffuse-type gastric cancer. Nat. Genet. 2008;40:730–740. doi: 10.1038/ng.152. [DOI] [PubMed] [Google Scholar]
- 23.Fu Y.P., Kohaar I., Rothman N., Earl J., Figueroa J.D., Ye Y., Malats N., Tang W., Liu L., Garcia-Closas M., et al. Common genetic variants in the PSCA gene influence gene expression and bladder cancer risk. Proc. Natl. Acad. Sci. USA. 2012;109:4974–4979. doi: 10.1073/pnas.1202189109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rai R., Sharma K.L., Misra S., Kumar A., Mittal B. PSCA gene variants (rs2294008 and rs2978974) confer increased susceptibility of gallbladder carcinoma in females. Gene. 2013;530:172–177. doi: 10.1016/j.gene.2013.08.058. [DOI] [PubMed] [Google Scholar]
- 25.Saeki N., Gu J., Yoshida T., Wu X. Prostate stem cell antigen: A Jekyll and Hyde molecule? Clin. Cancer Res. 2010;16:3533–3538. doi: 10.1158/1078-0432.CCR-09-3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang M., Wang X.J., Ma Y.F., Ma X.B., Dai Z.M., Lv Y., Lin S., Liu X.H., Yang P.T., Dai Z.J. PSCA rs2294008 C > T contributed to gastric and bladder cancer risk. J. Ther. Clin. Risk Manag. 2015;11:237–245. doi: 10.2147/TCRM.S77089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Matsuo K., Tajima K., Suzuki T., Kawase T., Watanabe M., Shitara K., Misawa K., Ito S., Sawaki A., Muro K., et al. Association of prostate stem cell antigen gene polymorphisms with the risk of stomach cancer in Japanese. Int. J. Cancer. 2009;125:1961–1964. doi: 10.1002/ijc.24519. [DOI] [PubMed] [Google Scholar]
- 28.Wang S., Tang J., Wang M., Yuan L., Zhang Z. Genetic variation in PSCA and bladder cancer susceptibility in a Chinese population. Carcinogenesis. 2010;31:621–624. doi: 10.1093/carcin/bgp323. [DOI] [PubMed] [Google Scholar]
- 29.Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4 doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mantel N., Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 32.DerSimonian R., Laird N. Meta-analysis in clinical trials. Control. Clin. Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 33.Egger M., Smith D.G., Schneider M., Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toma M., Stavarachi M., Cimponeriu D., Apostol P., Cojocaru M., Belusica L., Panduru N., Radu I., Gavrila L. P53 And DCC Polymorphisms and the risk for colorectal cancer in Romanian Patients—A preliminary study. J. Anal. Univ. Oradea Fasc. Biol. 2009;16:162–165. [Google Scholar]
- 35.Zhao J., Geng P., Li Z., Cui S., Zhao J., Wang L., Li J., Ji F., Li G., Shen G., et al. Prostate stem cell antigen rs2294008 polymorphism differentially contributes to Helicobacter pylori-negative gastric cancer among various populations in China. Mol. Clin. Oncol. 2013;1:493–498. doi: 10.3892/mco.2013.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wu C., Wang G., Yang M., Huang L., Yu D., Tan W., Lin D. Two genetic variants in prostate stem cell antigen and gastric cancer susceptibility in a Chinese population. Mol. Carcinog. 2009;48:1131–1138. doi: 10.1002/mc.20565. [DOI] [PubMed] [Google Scholar]
- 37.Lu Y., Chen J., Ding Y., Jin G., Wu J., Huang H., Deng B., Hua Z., Zhou Y., Shu Y., et al. Genetic variation of PSCA gene is associated with the risk of both diffuse- and intestinal-type gastric cancer in a Chinese population. Int. J. Cancer. 2010;127:2183–2189. doi: 10.1002/ijc.25228. [DOI] [PubMed] [Google Scholar]
- 38.Ou J., Li K., Ren H., Bai H., Zeng D., Zhang C. Association and haplotype analysis of prostate stem cell antigen with gastric cancer in Tibetans. DNA Cell Biol. 2010;29:319–323. doi: 10.1089/dna.2009.0960. [DOI] [PubMed] [Google Scholar]
- 39.Zeng Z., Wu X., Chen F., Yu J., Xue L., Hao Y., Wang Y., Chen M., Sung J.J., Hu P. Polymorphisms in prostate stem cell antigen gene rs2294008 increase gastric cancer risk in Chinese. Mol. Carcinog. 2011;50:353–358. doi: 10.1002/mc.20718. [DOI] [PubMed] [Google Scholar]
- 40.Song H.R., Kim H.N., Piao J.M., Kweon S.S., Choi J.S., Bae W.K. Association of a common genetic variant in prostate stem-cell antigen with gastric cancer susceptibility in a Korean population. Mol. Carcinog. 2011;50:871–875. doi: 10.1002/mc.20796. [DOI] [PubMed] [Google Scholar]
- 41.Joung J.Y., Lee Y.S., Park S., Yoon H., Lee S.J., Park W.S., Chung J., Kim S.Y., Hong S.H., Kim J.S., et al. Haplotype analysis of prostate stem cell antigen and association with prostate cancer risk. J. Urol. 2011;185:2112–2118. doi: 10.1016/j.juro.2011.01.083. [DOI] [PubMed] [Google Scholar]
- 42.Lochhead P., Frank B., Hold G.L., Rabkin C.S., Ng M.T., Vaughan T.L., Risch H.A., Gammon M.D., Lissowska J., Weck M.N., et al. Genetic variation in the prostate stem cell antigen gene and upper gastrointestinal cancer in white individuals. Gastroenterology. 2011;140:435–441. doi: 10.1053/j.gastro.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sala N., Muñoz X., Travier N., Agudo A., Duell E.J., Moreno V., Overvad K., Tjonneland A., Boutron-Ruault M.C., Clavel-Chapelon F., et al. Prostate stem-cell antigen gene is associated with diffuse and intestinal gastric cancer in Caucasians: Results from the EPIC-EURGAST study. Int. J. Cancer. 2012;130:2417–2427. doi: 10.1002/ijc.26243. [DOI] [PubMed] [Google Scholar]
- 44.Kim S.Y., Yoo J.Y., Shin A., Kim Y., Lee E.S., Lee Y.S. Prostate stem cell antigen single nucleotide polymorphisms influence risk of estrogen receptor negative breast cancer in Korean females. Asian Pac. J. Cancer Prev. 2012;13:41–48. doi: 10.7314/APJCP.2012.13.1.041. [DOI] [PubMed] [Google Scholar]
- 45.Smith C., Lochhead P., Basavaraju U., Hold G.L., Fyfe N., Murray G.I., El-Omar E.M. Lack of association between the rs2294008 polymorphism in the prostate stem cell antigen gene and colorectal neoplasia: A case-control and immunohistochemical study. BMC Res. Notes. 2012;5 doi: 10.1186/1756-0500-5-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Li F., Zhong M.Z., Li J.H., Liu W., Li B. Case-control study of single nucleotide polymorphisms of PSCA and MUC1 genes with gastriccancer in a Chinese. Asian Pac. J. Cancer Prev. 2012;13:2593–2596. doi: 10.7314/APJCP.2012.13.6.2593. [DOI] [PubMed] [Google Scholar]
- 47.Ono H., Chihara D., Chiwaki F., Yanagihara K., Sasaki H., Sakamoto H., Tanaka H., Yoshida T., Saeki N., Matsuo K. Missense allele of a single nucleotide polymorphism rs2294008 attenuated antitumor effects of prostate stem cell antigen in gallbladder cancer cells. J. Carcinog. 2013;12 doi: 10.4103/1477-3163.109030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ma Z., Hu Q., Chen Z., Tao S., Macnamara L., Kim S.T., Tian L., Xu K., Ding Q., Zheng S.L., et al. Systematic evaluation of bladder cancer risk-associated single-nucleotide polymorphisms in a Chinese population. Mol. Carcinog. 2013;52:916–921. doi: 10.1002/mc.21932. [DOI] [PubMed] [Google Scholar]
- 49.Dai N., Zheng M., Wang C., Ji Y., Du J., Zhu C., He Y., Zhu M., Zhu X., Sun M., et al. Genetic variants at 8q24 are associated with risk of esophageal squamous cell carcinoma in a Chinese population. Cancer Sci. 2014;105:731–735. doi: 10.1111/cas.12399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sun Y., Gu J., Ajani J.A., Chang D.W., Wu X., Stroehlein J.R. Genetic and intermediate phenotypic susceptibility markers of gastric cancer in Hispanic Americans: A case-control study. Cancer. 2014;120:3040–3048. doi: 10.1002/cncr.28792. [DOI] [PubMed] [Google Scholar]
- 51.Wang P., Ye D., Guo J., Liu F., Jiang H., Gong J., Gu C., Shao Q., Sun J., Zheng S.L., et al. Genetic score of multiple risk-associated single nucleotide polymorphisms is a marker for genetic susceptibility to bladder cancer. Genes Chromosomes Cancer. 2014;53:98–105. doi: 10.1002/gcc.22121. [DOI] [PubMed] [Google Scholar]
- 52.Lee J.H., Song H.R., Kim H.N., Kweon S.S., Yun Y.W., Choi J.S., Jung S.I., Kwon D.D., Kim S.H., Choi Y.D., et al. Genetic variation in PSCA is associated with bladder cancer susceptibility in a Korean population. Asian Pac. J. Cancer Prev. 2014;15:8901–8904. doi: 10.7314/APJCP.2014.15.20.8901. [DOI] [PubMed] [Google Scholar]
- 53.Kupcinskas J., Wex T., Link A., Bartuseviciute R., Dedelaite M., Kevalaite G., Leja M., Skieceviciene J., Kiudelis G., Jonaitis L., et al. PSCA and MUC1 gene polymorphisms are linked with gastric cancer and pre-malignant gastric conditions. Anticancer Res. 2014;34:7167–7175. [PubMed] [Google Scholar]
- 54.Sun H., Wu X., Wu F., Li Y., Yu Z., Chen X., Chen Y., Yang W. Associations of genetic variants in the PSCA, MUC1 and PLCE1 genes with stomach cancer susceptibility in a Chinese population. PLoS ONE. 2015;10:9. doi: 10.1371/journal.pone.0117576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.García-González M.A., Bujanda L., Quintero E., Santolaria S., Benito R., Strunk M., Sopeña F., Thomson C., Pérez-Aisa A., Nicolás-Pérez D., et al. Association of PSCA rs2294008 gene variants with poor prognosis and increased susceptibility to gastric cancer and decreased risk of duodenal ulcer disease. Int. J. Cancer. 2015;15:1362–13736. doi: 10.1002/ijc.29500. [DOI] [PubMed] [Google Scholar]
- 56.Ichikawa H., Sugimoto M., Uotani T., Sahara S., Yamade M., Iwaizumi M., Yamada T., Osawa S., Sugimoto K., Miyajima H., et al. Influence of prostate stem cell antigen gene polymorphisms on susceptibility to Helicobacter pylori-associated diseases: A case-control study. Helicobacter. 2015;20:106–113. doi: 10.1111/hel.12183. [DOI] [PubMed] [Google Scholar]
- 57.Zhang W., Liang P., Wang W., Dai P., Wang Q., Yan W., Zhao J., Sun J., Peng Y., Cui D., et al. The Influence of PSCA Gene Variation on Its Expression and Gastric Adenocarcinoma Susceptibility in the Northwest Chinese Population. Int. J. Mol. Sci. 2015;16:11648–11658. doi: 10.3390/ijms160511648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kupcinskas J., Gyvyte U., Bruzaite I., Leja M., Kupcinskaite-Noreikiene R., Pauzas H., Tamelis A., Jonaitis L., Skieceviciene J., Kiudelis G. Common Genetic Variants of PSCA, MUC1 and PLCE1 Genes are not associated with Colorectal Cancer. Asian Pac. J. Cancer Prev. 2015;16:6027–6032. doi: 10.7314/APJCP.2015.16.14.6027. [DOI] [PubMed] [Google Scholar]
- 59.Qiao L., Feng Y. Genetic variations of prostate stem cell antigen (PSCA) contribute to the risk of gastric cancer for EasternAsians: A meta-analysis based on 16792 individuals. Gene. 2012;493:83–91. doi: 10.1016/j.gene.2011.11.017. [DOI] [PubMed] [Google Scholar]
- 60.Wu X., Ye Y., Kiemeney L.A., Sulem P., Rafnar T., Matullo G., Seminara D., Yoshida T., Saeki N., Andrew A.S., et al. Genetic variation in the prostate stem cell antigen gene PSCA confers susceptibility to urinary bladder cancer. Nat. Genet. 2009;41:991–995. doi: 10.1038/ng.421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang T., Chen Y.N., Wang Z., Chen J.Q., Huang S. Effect of PSCA gene polymorphisms on gastric cancer risk and survival prediction: A meta-analysis. Exp. Ther. Med. 2012;4:158–164. doi: 10.3892/etm.2012.563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi D., Wang S., Gu D., Wu D., Wang M., Chu H., Tong N., Ma L., Zhong D., Zhang Z. The PSCA polymorphisms derived from genome-wide association study are associated with risk of gastric cancer: A meta-analysis. J. Cancer Res. Clin. Oncol. 2012;138:1339–1345. doi: 10.1007/s00432-012-1210-6. [DOI] [PubMed] [Google Scholar]
- 63.Wang T., Zhang L., Li H., Wang B., Chen K. Prostate stem cell antigen polymorphisms and susceptibility to gastric cancer: A systematic review and meta-analysis. Cancer Epidemiol. Biomark. Prev. 2012;21:843–850. doi: 10.1158/1055-9965.EPI-11-1176. [DOI] [PubMed] [Google Scholar]
- 64.Zhang Q.H., Yao Y.L., Gu T., Gu J.H., Chen L., Liu Y. Association of the PSCA rs2294008 C > T polymorphism with gastric cancer risk: Evidence from a meta-analysis. Asian Pac. J. Cancer Prev. 2012;13:2867–2871. doi: 10.7314/APJCP.2012.13.6.2867. [DOI] [PubMed] [Google Scholar]
- 65.Gu X., Zhang W., Xu L., Cai D. Quantitative assessment of the influence of prostate stem cell antigen polymorphisms on gastric cancer risk. Tumour Biol. 2014;35:2167–2174. doi: 10.1007/s13277-013-1287-9. [DOI] [PubMed] [Google Scholar]
- 66.Gao J., Yang P.T., Diao Y., Kang H.F., Zhao Y., Lin S., Wang Z.M., Wang M., Wang X.J., Dai Z.J. Effects of PSCA rs2294008 (C/T) and c-MYC rs9642880 (G/T) polymorphisms on bladder cancer: Evidence from a meta-analysis. Int. J. Clin. Exp. Med. 2015;8:2156–2164. [PMC free article] [PubMed] [Google Scholar]
- 67.Zhao Y., Gui Z.L., Liao S., Gao F., Ge Y.Z., Jia R.P. Prostate stem cell antigen rs2294008 (C > T) polymorphism and bladder cancer risk: A meta-analysis based oncases and controls. Genet. Mol. Res. 2014;13:5534–5540. doi: 10.4238/2014.July.25.7. [DOI] [PubMed] [Google Scholar]
- 68.1. Gu Y., Dai Q.S., Hua R.X., Zhang B., Zhu J.H., Huang J.W., Xie B.H., Xiong S.Q., Tan G.S., Li H.P. PSCA rs2294008 C > T and rs2976392 G > A polymorphism contribute to cancer susceptibility: Evidence from published studies. Genet. Cancer. 2015;6:254–264. doi: 10.18632/genesandcancer.63. [DOI] [PMC free article] [PubMed] [Google Scholar]