Abstract
Mounting evidence across different disciplines suggests that early-life conditions can have consequences on individual outcomes throughout the lifecycle. Relative to other developed countries, the United States fares poorly on standard indicators of early-life health, and this disadvantage may have profound consequences not only for population well-being, but also for economic growth and competitiveness in a global economy. In this paper, we first discuss the research on the strength of the link between early-life health and adult outcomes, and then provide an evidence-based review of the effectiveness of existing U.S. policies targeting the early-life environment. We conclude that there is a robust and economically meaningful relationship between early-life conditions and well-being throughout the lifecycle, as measured by adult health, educational attainment, labor market attachment, and other indicators of socio-economic status. However, there is some variation in the degree to which current policies in the U.S. are effective in improving early-life conditions. Among existing programs, some of the most effective are the Special Supplemental Program for Women, Infants, and Children (WIC), home visiting with nurse practitioners, and high-quality, center-based early childhood care and education. In contrast, the evidence on other policies such as prenatal care and family leave is more mixed and limited.
INTRODUCTION
Over the last several decades, research across several disciplines has traced the origins of lifecycle well-being to the very early stages of life (see Almond & Currie, 2011, for an overview). This lasting relationship between early childhood conditions and adult well-being may be particularly consequential for the United States, which fares relatively poorly on markers of infant health compared to other developed countries. For example, the U.S. infant mortality rate was ranked 32nd among the 34 countries of the Organization for Economic Cooperation and Development (OECD) in 2010 (Centers for Disease Control and Prevention, 2013).
Recent work suggests that this U.S. infant health disadvantage is likely driven by higher inequalities across demographic groups relative to similarly wealthy countries (Chen, Oster, & Williams, 2014). For example, Figure 1 shows that relative to other races and ethnicities, non-Hispanic white mothers exhibit the lowest rates of low birth weight (defined as less than 2,500 grams) and preterm birth (defined as gestation less than 37 weeks): 7.1 and 10.5 percent, respectively. In contrast, among non-Hispanic African-American mothers, 13.3 percent of children are born with low birth weight and 16.8 percent are born preterm (90 and 70 percent higher than non-Hispanic whites, respectively). Figure 2 shows how infant health varies with other markers of socio-economic status: unmarried mothers with low education levels experience substantially higher rates of adverse birth outcomes relative to their married, more educated counterparts.
Figure 1.

Disparities in Birth Outcomes by Maternal Race/Ethnicity, 2011.
Notes: Based on authors’ own calculations using National Center for Health Statistics natality records on all 2011 births.
Figure 2.
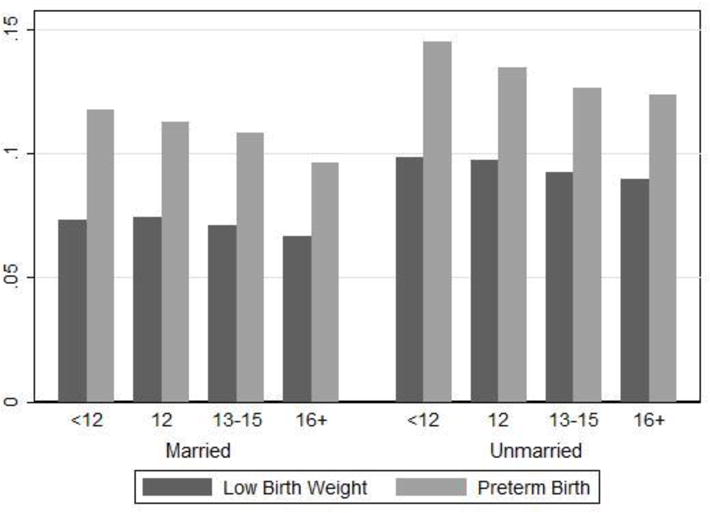
Disparities in Birth Outcomes by Maternal Years of Education and Marital Status, 2011
Notes: Based on authors’ calculations using National Center for Health Statistics natality records on all 2011 births.
The fact that the U.S. lags other advanced countries in early childhood health may have profound consequences not only for population well-being, but also for economic growth and competitiveness in a global economy. Policies that target early-life conditions, especially among vulnerable populations, may be starting to reverse this trend (Aizer & Currie, 2014). Additionally, such programs may play an important role in ameliorating intergenerational persistence of economic disadvantage and reducing inequality.i
Currently, the U.S. has a number of public policies that explicitly aim to improve the well-being of pregnant women and young children, and state and local governments are also active in this policy arena. These include prenatal care, public health insurance, the Special Supplemental Program for Women, Infants, and Children (WIC), family leave, nurse home visiting, early childhood center-based educational interventions such as Head Start, and public education campaigns such as “Back to Sleep.” These programs are varied in their structure and scope—for example, WIC targets the nutrition of pregnant women and young children by distributing vouchers to buy healthy foods, while home visiting interventions provide mothers with education in parenting skills and child development through regular sessions with trained professionals.
The substantial degree of variation in the policy landscape raises questions about how successful these programs are at improving early-life conditions and whether certain interventions work better or are more cost-effective than others. The purposes of this paper are: first, to discuss the research on the strength of the link between early-life health and adult outcomes, and second, to provide an evidence-based review of the effectiveness of existing U.S. interventions targeting the early-life environment.
Throughout this article, the terms “early life” and “early childhood” refer to conditions affecting individuals from conception to age five. The first part of the paper will make it clear that there are many policies that have the potential to affect early-life health. However, in order to keep our review manageable, the second part of the paper will focus on intervention programs that directly target pregnant women and children through age five—we do not review the many U.S. policies that do not explicitly target early-life conditions but can nevertheless affect them. These include large-scale means-tested programs such as the Supplemental Nutrition Assistance Program (SNAP, commonly known as Food Stamps) and Temporary Assistance for Needy Families (TANF), which, in addition to aiding pregnant women and young children, also cover individuals at other stages of life. Similarly, because of its broad reach in the population, we do not review the evidence on how environmental regulation impacts early-life circumstances, despite a large literature documenting a link between environmental conditions (e.g., air pollution) and infant health.ii
We also limit our review to programs and policies that have been evaluated in the academic literature using empirical designs that allow for causal inference. This is a particularly important issue for program and policy evaluation because program participants (or individuals covered by the policy under analysis) are usually not randomly selected. For example, children enrolled in Head Start tend to come from households with lower incomes and have less-educated parents than children in other early childcare programs. Garces, Thomas, and Currie (2002) show that in a large national sample, 25 percent of children who attended Head Start ever attended college, compared to 39 percent of children who did not attend Head Start. However, when they compare Head Start children to other similar children (in this case, their own siblings) they find that Head Start increases the probability of ever attending college by 9 percent. This example highlights the fact that it is challenging to isolate the causal effects of Head Start from the consequences of the other family background characteristics. Therefore, we limit ourselves to interventions that have either had randomized evaluations or been studied using empirical methods to try to control for non-random selection into program or policy treatment.
Finally, we restrict our review of the literature to articles and reports published in the last two decades (since 1994, and especially since 2000), as well as working papers that have not yet been published. When possible, we reference other review articles that summarize earlier studies.
Overall, our review of the evidence on the lasting consequences of early-life conditions throughout the life-course suggests that this relationship is quite robust. Many studies, using a variety of methods and data sets, have documented a causal link between well-being in early childhood and adult outcomes, including health, educational attainment, labor force participation, and broader measures of socio-economic status. Although the magnitudes of the effect sizes vary across studies, the relationship is economically meaningful. For instance, one of the most comprehensive studies on the topic shows that increasing a child’s birth weight from 2,500 grams (the cutoff for the low-birth-weight designation) to the U.S. national average of 3,300 grams would lead to a 3 percent increase in adult full-time earnings (Black, Devereux, & Salvanes, 2007), a magnitude that represents one third of the estimated return to an extra year of schooling (Card, 1999).
However, there is a decent amount of heterogeneity in the degree to which current programs in the U.S. can alter early-life conditions. Among existing programs, some of the most effective are WIC, home visiting with nurse practitioners, and high-quality, center-based early childhood care and education. In contrast, the evidence on other policies such as prenatal care and family leave is more mixed and limited.
This paper unfolds as follows. In the following section, we review the evidence on fetal and early childhood development and how early-life factors can influence life-long well-being. We then discuss studies on the effectiveness of some of the existing interventions specifically targeting in-utero and early childhood health and circumstances, and pay particular attention to the degree to which causal inference is credible. We conclude with a discussion and directions for future research.
LASTING IMPACTS OF EARLY-LIFE CONDITIONS
The “fetal origins hypothesis,” put forth by British physician and epidemiologist David J. Barker, brought attention to the idea that early-life conditions can have lasting consequences on life-long human well-being. Barker argued that adverse conditions during the prenatal period can “program” a fetus to have metabolic characteristics associated with future disease (Barker, 1990). He further postulated that the health consequences of fetal conditions are both persistent and possibly latent—in fact, individuals may not experience any of the insults (such as heart conditions) until middle age. The biological mechanism behind this type of “fetal programming” is relatively controversial and only beginning to be understood by scientists. One hypothesis is that the in utero period is particularly important for setting “switches” that determine whether various parts of the genome are expressed (Petronis, 2010).
This idea has been a catalyst for researchers across a variety of disciplines (including epidemiology, developmental psychology, and sociology) in adopting a “life course” approach to studying human development. The “life course” framework expands beyond the fetal period and highlights how biological, behavioral, and psychosocial processes that operate throughout an individual’s life course can influence health and disease risk at older ages (Kuh et al., 2003; Kuh & Shlomo, 2004). Physical and social exposures during gestation and in early childhood are central components of the “life course” model.
James Heckman and co-authors have formalized this perspective using the human capital model pioneered by Becker and Tomes (1979; 1986) and Mincer (1974). Their model involves several stages of childhood and dynamic complementarities between inputs at different stages (Cunha & Heckman, 2007; Heckman & Masterov, 2007; Cunha & Heckman, 2008; Cunha, Heckman, & Schennach, 2010). The key feature of this model is the idea that skills produced at one stage raise the productivity of investments in subsequent stages—i.e., skills beget skills. The model predicts that returns to investments in early childhood are higher than returns to investments in later life. Furthermore, the return to later investments may crucially depend on the critical earlier investments.
Empirical evidence documenting the link between early-life circumstances and life-long outcomes abounds. Some of the first studies on this topic followed cohorts who were exposed to the Dutch famine of 1944 in utero, and found that they on average had a higher risk of obesity, cardiovascular disease, and mental illness at ages 50 to 70 relative to unexposed cohorts (Susser et al., 1996; Neugebauer, Hoek, & Susser, 1999; McClellan, Susser, & King, 2006; Stein et al., 2007). These studies typically rely on comparisons of children born to women who were pregnant during the famine to those born to women who were pregnant during other, surrounding years. Such a design is potentially problematic in terms of identifying the causal effects of prenatal malnutrition as women who conceive and give birth during famines might have different (unobservable) characteristics from other women. As such, it may be difficult to separate out the impacts of the famine per se from the possible influences of other maternal characteristics that are associated with the ability to conceive and carry to term during a famine. Moreover, by focusing on one extreme famine, these studies cannot speak to the possible effects of less acute, more common, and more policy-relevant early-life shocks.
To study the consequences of less acute health shocks, researchers often use longitudinal data that combine information on individual markers of early-life health with adult outcomes. Much of this work focuses on the long-run consequences of birth weight, a commonly used marker of infant health that can be seen as a summary proxy for prenatal conditions. Low birth weight is strongly associated with infant mortality and subsequent morbidity for infants who survive (Paneth, 1995; Almond, Chay, & Lee, 2005). However, while birth weight captures some information about prenatal health, it is not a sufficient statistic: Children of normal birth weight may nevertheless have health problems, and vice versa. Health after birth and in early childhood (e.g., through age five) is even harder to quantify with a summary measure. A number of studies use adult height as an indicator of early childhood health post-birth, which can be affected both by nutrition and by disease. Growth until age three is more rapid than at any other stage during the life course, and therefore health and nutrition during this period are critical determinants of adult height (see Case & Paxson, 2010 and the references therein for more details). Additionally, some researchers use information on the presence of chronic health conditions in early childhood, which likely captures some of the most severe forms of health deficiencies.
In one of the first studies using this approach, Currie and Hyson (1999) analyze data from the 1958 National Child Development Survey (NCDS), which follows a cohort of British individuals from birth until middle age, and show that low-birth-weight (less than 2,500 grams) individuals are 25 to 44 percent less likely to pass English and math exams at age 16, and 9 to 16 percent less likely to be employed in their 20s and 30s, even after controlling for a large number of individual and family background characteristics. Other work, using birth weight, height, and the presence of chronic conditions as markers of early-life health, documents impacts on adult health, employment, earnings, and socio-economic status, as well as cognitive function into old age (Case, Fertig, & Paxson, 2005; Case & Paxson, 2008a,b). For example, Case and Paxson (2008a) use data on U.S. adults ages 50 and older from the Health and Retirement Study, and show that a one inch increase in height is associated with a 1 percent increase in the delayed word recall score, a 0.3 percent increase in the probability of being able to count backwards, and a 0.3 percent increase in the probability of knowing the date.
Yet while these studies are some of the first to document significant relationships between early-life health and adult economic outcomes, questions about causality remain. In particular, although these analyses control for a large number of demographic and family background characteristics, it is possible that individuals with worse health at birth and in early childhood have unobservable characteristics that generate independent insults to their life course outcomes. For instance, mothers of low-birth-weight children, who are more likely to be economically disadvantaged, may have lower parenting skills and resources than their more advantaged counterparts.
To address this issue, many studies have exploited differences in childhood health between siblings (or twins) and examined how they are correlated with differences in long-run outcomes. By comparing siblings born to the same parents, these studies control for any constant observed or unobserved components of family background that are shared by the two siblings. Black, Devereux, and Salvanes (2007) have conducted one of the largest studies in this literature, using administrative data from Norway on over 30,000 twins born between 1967 and 1997. They show that a 10 percent increase in birth weight reduces mortality in the first year of life by 13 percent, increases the probability of high school completion by 1 percent, and increases adult full-time earnings (at age 25 and above) by 1 percent. To put these magnitudes in context, consider that average birth weight in the U.S. was 3,266 grams in 2011.iii This implies that the 30 percent increase in birth weight from 2,500 grams (the cutoff for a low-birth-weight designation) to the national average is estimated to raise adult earnings by 3 percent.
In another recent study, Figlio et al. (2013) present evidence on the long-term effects of birth weight on cognitive development in the U.S., using a large sample of twin birth records linked to school records from Florida. They find that a 10 percent increase in birth weight increases math and reading test scores in grades 3 through 8 by about 0.05 standard deviations (with somewhat larger impacts on math than reading scores). Using a back-of-the-envelope calculation based on these results, the authors estimate that increases in cognitive skills in grades 3 through 8 explain approximately three-quarters of the effect of birth weight on adult earnings found by Black, Devereux, and Salvanes (2007).
Similar sibling and twin studies have been conducted in a variety of other countries (e.g., Australia, Canada, Germany, Sweden, United Kingdom, and Taiwan). Overall, these studies provide relatively robust evidence that early-life health indicators—birth weight, height, and the presence of various physical and mental health conditions in childhood—are associated with many long-run outcomes including school test scores, educational attainment, as well as adult employment, income, public assistance take-up, crime, and self-reported health.iv
There is some controversy about whether the estimated long-term effects represent a biological effect of early-life health per se, or whether they are mediated by social factors. For example, a parent might subsequently decide to invest more or less in a child with poor health at birth than in a sibling. Bharadwaj, Eberhard, and Neilson (2013) address this issue using a large sample of births from Chile, and find that parents tend to compensate for poor health at birth, suggesting that sibling comparisons may understate the true negative effects of early-life health. Still, the extent to which parents may reinforce or compensate for early health problems is likely to be sensitive to both culture and parental resources.
Additionally, there is some recent evidence suggesting that there are important differences across children with poor early-life health that translate into differences in how early-life health impacts long-term outcomes. Robinson (2013) uses insights from the medical literature to decompose low-birth-weight infants into two distinct sub-types: symmetric and asymmetric. The symmetric type exhibits proportional growth restriction in all major organs, including the brain; while the asymmetric type exhibits relatively less restriction in brain development. Robinson (2013) shows that the symmetric low-birth-weight children are more likely to have low IQ. However, despite these differences in cognitive impairment, both sub-types exhibit similar insults to physical health. This paper thus provides some insights into the biological mechanisms behind how poor early-life health indicators such as low-birth-weight translate into adverse long-term outcomes.
Another line of research has used variation in the early-life environment provided by sudden and often unexpected natural disasters and disease epidemics to identify the causal effects of early childhood health. For example, Almond (2006) studies the long-run consequences of in utero exposure to the 1918 influenza epidemic on a broad range of individual adult outcomes using U.S. Census data. Comparing cohorts who were in utero during the epidemic to those who were in utero either shortly before or after, he finds that exposed cohorts who had infected mothers were 13 to 15 percent less likely to complete high school and scored 2 to 7 percent lower on a socioeconomic status index. Additionally, prenatally exposed males had 5 to 9 percent lower adult incomes and were 3 to 6 percent more likely to have a work-limiting disability, while prenatally exposed females received 12 percent more income from welfare benefits in adulthood.v In related work, Almond and Mazumder (2005) find that prenatally exposed cohorts were more likely to have poor self-reported health, and to experience trouble hearing, speaking, lifting, and walking in adulthood.vi
Other researchers have looked beyond disease outbreaks to identify the long-term con-sequences of early-life events. For example, several studies have shown that in utero and early childhood exposure to adverse environmental conditions harms later-life measures of well-being. Almond, Edlund, and Palme (2009) show that prenatal exposure to radiation in Sweden due to fallout from the Chernobyl accident reduced the probability of qualifying for high school (based on performance in the final year of compulsory school) by about 4 percent. This paper compares areas of Sweden that were affected by the fallout to areas just adjacent, using cohorts in utero before, during, and after the crisis. Black et al. (2013) also use variations in fallout from nuclear testing and find that even low-dose exposure to radiation can have lasting consequences—using Norwegian administrative data, they estimate that a one standard deviation increase in prenatal exposure to radiation reduces educational attainment by 0.08 years for men and 0.1 years for women. For men, they further find that a one standard deviation increase in in utero radiation exposure lowers age-18 IQ scores by 0.06 standard deviations and reduces age-35 earnings by about 1 percent. Early-life air pollution exposure also has long-run effects: a 10 percent reduction in exposure to total suspended particulates (TSP) in an individual’s year of birth increases high school test scores by about 4 percent (Sanders, 2012) and raises age-30 earnings by 1 percent (Isen, Rossin-Slater, & Walker, 2014).vii
There is also evidence that economic conditions in early life can have lasting influences throughout the lifecycle. For example, using historical data from the Netherlands, Van Den Berg, Lindeboom, and Portrait (2006) compare individuals born during the economic boom of 1872 to 1876 with individuals born during the recession of 1877 to 1881. They find that people born during economically prosperous years had life expectancies that were about 1.6 years longer than those born during the economic downturn. In another study, Banerjee et al. (2010) exploit regional variation in phylloxera attacks that substantially reduced wine production in French vineyards between 1863 and 1890.viii They show that individuals from wine-growing families born during the year that their region was affected by phylloxera were 3 to 5 percent shorter at age 20 relative to their counterparts who were not exposed to these negative income shocks in early life. In addition, Page, Stevens, and Lindo (2007), Stevens and Schaller (2011), and Johnson, Kalil, and Dunifon (2012) show that parental job loss and income and employment shocks have negative impacts on children’s educational attainment and behavior.
In contrast to earlier studies in this literature that have focused on the long-term effects of rare natural disasters, disease outbreaks, and famines, the more recent work in this area has begun to examine the long-term impacts of policy-generated shocks to early-life health. For example, Hoynes, Schanzenbach, and Almond (2012) use variation in the roll-out of the Food Stamps program in the 1960s and 1970s, and find that having access to the Food Stamps program between conception and age five reduces an adult metabolic syndrome (an index that captures the presence of health conditions including obesity, diabetes, and high blood pressure) by about 0.3 standard deviations, and increases an economic self-sufficiency index (a measure that includes indicators for high school graduation, employment, not being below the poverty line, not receiving TANF, not receiving Food Stamps, as well as continuous earnings and family income in adulthood) by about 0.3 standard deviations (for women only). In contrast, simple comparisons of children on Food Stamps with those who are not often show that the former are more likely to be food insecure and to have deficient diets, a finding that is not surprising given that relative poverty is a precondition for participation in the program (Bhattacharya & Currie, 2001).ix
On the whole, the links between early-life conditions and important markers of development and well-being throughout childhood, adulthood, and into old age seem quite robust, despite the fact that researchers have used a variety of empirical methods and have studied a number of different contexts. Consequently, this evidence suggests that interventions targeting early-life conditions could be particularly influential in improving individual well-being throughout the lifecycle, and thus motivates an examination of the effectiveness of existing policies and programs targeting this age range in the U.S.
EXISTING INTERVENTIONS TARGETING EARLY-LIFE HEALTH AND WELL-BEING
In this section, we discuss the research on some of the existing U.S. programs and policies that specifically target pregnant women or children through age five. However, before doing so, we first briefly discuss the mechanisms by which these interventions might impact early-life health.
Mechanisms Behind the Potential Impacts of Programs Targeting Early-Life Health
There are a number of mechanisms by which the interventions described below might impact early-life health. First, the medical literature posits stress as a potentially important biological mechanism through which early-life health insults translate into impacts on life-long outcomes. When a fetus is exposed to excessive amounts of the stress hormone cortisol in utero, there can be a reprogramming of the hypothalamic-pituitary-adrenal axis (HPA), which can in turn lead to impaired fetal development and worse health in adult age.x Many of the interventions discussed below (such as prenatal care, access to public health insurance, WIC, family leave, home visiting programs, and public health educational campaigns) could in principle lower stress levels during pregnancy, especially among low-income women who experience disproportionate amounts of chronic stress (Thompson, 2014). However, at present, this remains a hypothesis, as there is no research that we are aware of linking participation in specific programs to biological measures of stress reduction or effects on fetuses or young children.
Second, some of the interventions might improve early-life health through medical care that enables early detection and treatment of health conditions. For instance, prenatal care and access to public health insurance may be useful in diagnosing rare but serious pregnancy complications that threaten mother and child, such as eclampsia. Newborn screening and treatment for specific neonatal conditions like phenylketonuria can prevent negative health consequences such as mental retardation. Contact with social programs may also help to detect conditions such as maltreatment or maternal depression, which threaten child health and development.
Third, these interventions might affect parental behaviors during pregnancy and in the first few years of life. For example, programs like WIC teach mothers about nutrition and breastfeeding, and home visiting programs teach parents about developmentally appropriate child behavior and effective parenting strategies. Head Start includes programming aimed at parents that might help them, for example, to conduct effective job searches. Many interventions such as public education campaigns are targeted at specific negative behaviors of parents (i.e., drinking alcohol during pregnancy or smoking around children).
Fourth, interventions such as home visiting programs and early childhood care and education programs can impact child development directly through targeted curricula and materials. And some social programs such as Head Start explicitly require providers to connect children with necessary medical and dental services, as well as to provide them with nutritious meals and snacks.
Prenatal Care
When a woman first becomes pregnant, much of her contact with the healthcare system occurs through prenatal care. This is one of the most commonly used health services in the U.S.—for instance, among women giving birth in 2011, 95 percent reported having at least one prenatal care visit.xi This near-universal contact with the healthcare system during pregnancy is in part due to large expansions in the Medicaid program throughout the 1980s and 1990s, which have ensured that prenatal care is covered for low-income women (Currie & Gruber, 1996a,b). Thus, prenatal care has the potential to influence the health of nearly the entire population of mothers-to-be.
The American College of Obstetricians and Gynecologists recommends that, on average, women should have 11 prenatal care visits during pregnancy. A lot of the existing research has examined whether the number of these routine visits has any effect on infant health. For instance, researchers have conducted several randomized trials, comparing the outcomes of women who had a standard number of prenatal care visits with those of women who had a reduced schedule of visits (Sikorski et al., 1996; Fiscella, 1995). These studies find little impact of additional visits on birth outcomes or infant health. However, many of these trials were conducted on relatively small numbers of low-risk women, and thus cannot address the question of whether prenatal care might be beneficial for higher-risk women who have chronic health conditions or engage in behaviors such as drinking or smoking during pregnancy.
Some non-randomized studies present additional evidence on the impacts of prenatal care for larger and less selected populations. For example, Abrevaya and Dahl (2008) use data on all sibling births in Arizona and Washington from 1992 to 2002. They compare the outcomes of children born to the same mother, where the effects are identified by mothers who had different numbers of prenatal care visits across pregnancies. They find that an additional prenatal care visit increases birth weight by about 12–20 grams, a 0.3 to 0.5 percent effect at the sample mean. The effects are somewhat larger at the bottom of the birth weight distribution. However, the siblings approach only controls for time-invariant characteristics of the mother that might be correlated with both prenatal care receipt and birth outcomes. There may be important time-varying factors (e.g., maternal employment and marital status) that determine the amount of prenatal care a mother gets and also have independent impacts on birth outcomes, thereby biasing the estimates. Moreover, the number of prenatal care visits is strongly related to the length of gestation, which itself is a predictor of birth weight. Hence, it may be that women get more prenatal care visits because their pregnancies are longer rather than vice versa.
Another study uses a unique natural experiment to identify the impacts of prenatal care. Evans and Lien (2005a) exploit a bus strike in Pennsylvania that reduced the number of prenatal care visits that low-income women were able to attend. Women with more prenatal care reported a lower incidence of smoking during pregnancy, but saw no improvements in their birth outcomes. However, the bus strike only lasted 28 days and thus could not have had substantial impacts on the number of prenatal visits—African-American women living in the inner-city, who were most likely to be impacted, experienced a reduction of 0.45 visits on average. It is also likely that the bus strike affected other aspects of these women’s lives (e.g., ability to get to work, etc.) and these factors may confound the estimates of the effects of prenatal care.
It is possible that despite the lack of observable early-life health impacts, prenatal care might influence maternal health-related parenting behaviors and the utilization of pediatric care, which may ultimately contribute to child health and well-being later in life. Reichman et al. (2010) argue that first trimester prenatal care initiation decreases maternal post-partum smoking, increases well-baby care visits, and increases breastfeeding. To identify the effects of prenatal care, they control for a rich set of family background characteristics and use distance to the nearest hospital as an instrument. A potential limitation of this study is that the instrument may impact the outcomes of interest through channels other than the receipt of prenatal care, since the residential location of the mother (and hence her distance to a hospital) may be correlated with other factors (e.g., distance to the pediatrician).
It may also be the case that the quantity of prenatal care is not the relevant dimension to study. Instead, the quality of prenatal care may be more important. However, research on the impacts of prenatal care quality is almost non-existent, in part due to a lack of data on quality measures. Indeed, a recent Institute of Medicine report, which focuses on preterm births as markers of poor early-life health, calls for establishing a “quality agenda with the intent of maximizing outcomes with current technology for infants born preterm” (Behrman & Butler, 2007).xii Finally, prenatal care may serve as an important tool for providing mothers-to-be with medical services that are not necessarily limited to pregnant women. For instance, since exposure to the influenza virus has been linked to preterm delivery (Currie & Schwandt, 2013), prenatal care visits may be helpful in ensuring that more pregnant women receive flu vaccinations.
On the whole, the evidence suggests that the effects of the quantity of prenatal care on birth weight and other markers of early-life health have been elusive. However, high-quality care may be necessary to see impacts, and research on the quality as opposed to the quantity of care is much more limited. Moreover, prenatal care may be important for improving maternal health and related investments in their children, and serve as a conduit to support other types of medical or social interventions that are beneficial to early childhood health. Such beneficial effects would not be captured by research that focuses exclusively on measures of health at birth, such as birth weight.
Public Health Insurance
Despite the lack of evidence regarding the efficacy of prenatal care quantity, research suggests that expansions of public health insurance coverage to low-income pregnant women, infants, and young children have improved early-life health. Historically, eligibility for health insurance coverage for these groups under the Medicaid program was closely tied to receipt of welfare. Beginning in April 1987, states were first given the option and then required to cover pregnant women with much higher income levels. By April 1990, all states were required to cover pregnant women with incomes up to 133 percent of the poverty line, and states had the option of using federal funds to cover women with incomes up to 185 percent of the poverty line. The federal government also began encouraging states to cover children at higher income levels, and then mandating them to do so. The Omnibus Reconciliation Act of 1990 was an important milestone, mandating that states cover children under age 19 born after Sept. 1983—thus, the age cutoff for coverage went up one year every year until all poor children under age 19 were covered. Finally, the Children’s Health Insurance Program (CHIP), which was created in 1996, encouraged states to cover uninsured children at incomes higher than their existing cutoffs for Medicaid, either by further expanding Medicaid or by developing stand-alone programs.
Currie and Gruber (1996b) use state-level data and show that places where poverty in-creased, also tend to see increases in Medicaid enrollments, a connection that is not surprising given the structure of the program. However, they find that when these mechanical correlations are controlled for using instrumental variables methods, the above-noted expansions of public health insurance to pregnant women led to significant reductions in infant mortality.xiii They argue that these effects are largely driven by better care at the time of the birth and immediately afterwards. While some recent work has suggested that these effects may be sensitive to the inclusion of additional controls, such as state-specific linear trends (Dave et al., 2008), there is also evidence Medicaid coverage during pregnancy translates into long-term positive impacts. For example, Miller and Wherry (2014) show that early-life access to Medicaid stemming from these expansions was associated with lower rates of obesity and fewer preventable hospitalizations in adulthood. Levine and Schanzenbach (2009) find long-run effects of Medicaid on child educational attainment. They examine the performance of different cohorts of children on the National Assessment of Educational Progress (scores) and find higher scores in states and cohorts where larger numbers of children were covered at birth. Boudreaux, Golberstein, and McAlpine (2014) use variation in the staggered timing of initial adoption of the Medicaid program across states in the late 1960s, and find that access to Medicaid in early childhood is associated with long-term improvement in adult health, measured with an index that combines information on high blood pressure, diabetes, heart disease, and obesity.
Howell and Kenney (2012) provide an excellent overview of 38 studies that have tried to assess the effects of Medicaid and CHIP expansions on access to and utilization of care among children. Their review only covers studies that attempt to assess the causal effect of insurance by controlling for selection into the programs, using a variety of methods including difference-in-differences, instrumental variables, and regression discontinuity designs. They point out that there is substantial variation in the estimates, but that most studies find significant positive effects on measures of utilization of care, such as whether the child has any visits for preventive care.
A smaller number of studies examine child health outcomes including reported health status, preventable hospitalization, and child mortality. For example, Currie, Decker, and Lin (2008) use data from the National Health Interviews Survey (NHIS) and look at effects of Medicaid expansions in childhood on later child health. They argue that being covered at a young age is associated with better health in adolescence, but do not find any strong effects of contemporaneous changes in coverage. Dafny and Gruber (2005) examine the effects of the expansions on child hospitalizations. They find reductions in preventable hospitalizations, consistent with better access to preventive care. However, they find increases in overall levels of hospitalization, suggesting that more generous insurance coverage may also increase the number of unnecessary hospitalizations in some cases. Meyer and Wherry (2012) examine the effects of the Medicaid expansions (specifically, the fraction of a child’s life that he or she would have been eligible for public health insurance) on child mortality and find effects among blacks but not among whites. An important limitation of these studies is that since most data sources do not track children over time, and do not include the child’s state of birth, researchers wishing to infer the long-term effects of insurance must assume that the child has always lived in the state where he or she is currently observed. Still, although controversy remains about the size of the effects, and about the extent to which increases in public health insurance have been offset by reductions in private health insurance, most analysts believe that the programs have significantly improved access to care and children’s health.xiv
The Special Supplemental Program for Women, Infants, and Children (WIC)
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is one of the largest U.S. initiatives explicitly targeting early childhood health and nutritional well-being in the low-income population. The program was originally established in 1974 and covers low-income pregnant and post-partum women, infants, and young children through age five. Eligibility rules require participants to live in households with incomes below 185 percent of the poverty line and to be “at nutritional risk” (most individuals who satisfy the income requirement are assessed to be “at nutritional risk”). Participating pregnant and post-partum women, as well as parents and guardians of eligible young children, receive monthly benefits from WIC that can be taken to grocery stores and used to buy nutritious foods. WIC foods include iron-fortified infant formula and infant cereal, iron-fortified adult cereal, vitamin C-rich fruit and vegetable juice, milk, eggs, cheese, beans, and peanut butter. Additionally, WIC participants receive education about nutrition, health, and breastfeeding, and referrals to other social service agencies.
Research on how WIC affects infant health dates back several decades (see Currie, 2003 for a comprehensive review of the early work on this topic). Almost all of the existing work has focused on the effects of WIC among pregnant women and infants—there is very little evidence on how WIC impacts toddlers and children through age five. As such, we focus our review in this section on the impacts of WIC on measures of health at birth and some immediate post-birth behaviors such as breastfeeding.
Early WIC studies found a positive association between WIC food receipt and birth weight, as well as favorable relationships with other health outcomes like the probability of an infant being small-for-gestational-age (see, e.g., Ahluwalia et al., 1998). The magnitudes of the estimated effects are quite substantial—for example, the early WIC literature finds that participation in the program is associated with a 10 to 43 percent reduction in the likelihood of a low-birth-weight birth (Currie, 2003). By comparing WIC participants to non-participants, however, these studies may not have adequately addressed the issue of non-random selection into WIC. In particular, if WIC participants tend to have characteristics associated with better birth outcomes relative to the comparison groups (for example, perhaps WIC participants have healthier behaviors, better knowledge about public programs, or greater family support networks relative to non-participants), then the benefits of WIC could be overstated.
To address this criticism, some researchers have tried to choose comparison groups that are more similar to WIC participants. Bitler and Currie (2005) compare women who received WIC benefits to other women on Medicaid (who are also eligible for WIC), and find that the children of WIC participants have 64 to 78 gram higher birth weights, are 30 percent less likely to be born low-birth-weight or premature, and are 10 percent less likely to be admitted to the Intensive Care Unit. Importantly, Bitler and Currie (2005) show that WIC participants on average have observable characteristics that are actually associated with worse birth outcomes, suggesting that at least some of the earlier studies on WIC may have in fact been underestimating the program’s benefits. It is nonetheless still possible that the unobservable characteristics of WIC participants may be biasing the estimated effects.
As noted earlier, sibling comparisons can in part deal with this issue by controlling for all time-invariant family background characteristics that could be correlated with both WIC take-up and child health. For example, one study comparing children born to women who participated in WIC during one pregnancy and not during another shows that WIC-exposed children have lower incidence of anemia, failure-to-thrive, and nutritional deficiencies (Lee & Mackey-Bilaver, 2007). However, as with all sibling studies, the possibility of omitted variables bias still remains due to unobservable time-varying factors that determine why a mother receives WIC during one pregnancy and not during another. For example, mothers who did not know about WIC during their first pregnancy and learned about the program during their subsequent pregnancy may have also gotten access to other resources that could affect the younger sibling’s health. Currie and Rajani (2014) examine this question in a large sample of women in New York City and find that mothers are more likely to participate in WIC when they are young, unmarried, and unemployed, and more likely to participate if they have chronic conditions, such as diabetes. Like Bitler and Currie (2005), their analysis suggests that the effects of WIC may actually be under-estimated in sibling comparisons.
An additional concern in the WIC literature is “gestational-age bias,” i.e., the mechanical correlation between the length of gestation (which is associated with other measures of infant health such as birth weight) and the likelihood of enrolling in WIC. After accounting for gestation length, Joyce, Gibson, and Colman (2005) and Joyce, Racine, and Yunzal-Butler (2008) find somewhat smaller effects on birth weight—7 to 40 gram increases in average birth weight (depending on the subsample considered), and a 9 percent reduction in low-birth-weight births.
Three more recent papers on WIC have introduced novel empirical strategies to address the issues raised in earlier studies, and all point to notable benefits of WIC for infant health. Figlio, Hammersma, and Roth (2009) use data linking Florida birth records to information on these children’s older siblings who are enrolled in elementary school. Since the household income eligibility threshold for reduced-price lunches is the same as for WIC, the analysis compares outcomes of infants whose older siblings received reduced-price lunches in the same year to those of infants whose older siblings did not but received them in either the previous or following years. The results suggest that WIC participation reduces the likelihood of low birth weight by nearly 160 percent when evaluated at the sample mean. The authors acknowledge that this effect is quite large, but that it also has a wide confidence interval, so that the actual effect may not be dissimilar from other studies.
In a subsequent study, Hoynes, Page, and Stevens (2011) examine the period of the initial roll-out of WIC in the 1970s, and use county-year variation in access to the program to identify its effects. The authors provide evidence that program roll-out was uncorrelated with other observable determinants of birth outcomes (such as local labor market conditions, etc.). Results show that initial access to the WIC program led to 18 to 29 gram increases in average birth weight and an 8 percent reduction in the likelihood of a low-birth-weight birth among participating women. It is important to note that these estimates may not be applicable to more current times though—relative to when it was first implemented in the 1970s, the WIC program operates on a much larger scale and provides a wider range of services today. As a result of its wider reach, WIC also serves a population that is on average less needy than the population served in the 1970s.
To examine the impacts of WIC in more recent years, Rossin-Slater (2013) uses within-zip-code variation in WIC clinic openings and closings in Texas and compares siblings born to the same mother from 2005 to 2009. The idea behind this empirical design is to compare women who had a WIC clinic in their zip code of residence during one pregnancy and not during another. Note that in this sibling study, the within-mother variation in WIC access comes only from WIC clinic openings and closings, rather than from other (likely unobservable) factors that may influence whether a woman receives WIC services during one pregnancy and not during another. Rossin-Slater (2013) further shows that these WIC clinic openings and closings are uncorrelated with other factors that might influence birth outcomes. The results suggest that access to WIC increases food benefit take-up, pregnancy weight gain, birth weight, and the probability of breastfeeding initiation at the time of hospital discharge. The magnitudes of these effects are larger than those reported in Hoynes, Page, and Stevens (2011), suggesting that the WIC program may be a more consequential early childhood intervention today than it was at the time of its inception—among mothers with a high school education or less (who are most likely to be eligible for WIC), WIC access is found to be associated with a 32 gram increase in average birth weight and a 14 percent decrease in the likelihood of a low-birth-weight birth.
Overall, the vast literature on WIC presents a wide range of estimates of the relationship between WIC participation (or access) and health at birth. Although some of the earlier studies may be subject to biases that could overstate the benefits of WIC, more recent work that carefully attempts to identify the causal effects of WIC nevertheless points to positive and relatively large effects of the program, especially in recent years. However, the program serves children up to age five, and there are very few studies that attempt to measure causal effects of the program on infants and young children after birth. While there are some studies showing that WIC participation is associated with a higher likelihood of breastfeeding initiation and with more well-child visits post-birth (e.g., Chatterji & Brooks-Gunn, 2004), strong causal evidence on the relationship between WIC and breastfeeding, as well as on the program’s impacts on other measures of child well-being through age five is limited. This is an area that could definitely use further research.
Family Leave
According to the Bureau of Labor Statistics, over 60 percent of mothers with children under age three are currently in the labor force.xv Family leave programs are designed to provide time off from work so that new mothers can prepare for and recover from childbirth and parents can stay home to care for their newborns. As such, they could have important consequences not only for women’s employment and career trajectories, but also for early childhood health.
In particular, the guarantee of leave (especially if it is job-protected) may reduce maternal stress during and immediately after pregnancy, which has been shown to have an adverse effect on infant and child health (Mulder et al., 2002; Aizer, Stroud, & Buka, 2009; Currie & Rossin-Slater, 2013; Persson & Rossin-Slater, 2014). After birth, as family leave availability can influence the quantity and quality of time that a newborn child spends with his parents, there may be further health impacts. For example, a mother may have more time to take care of an ill child, to breastfeed, or to seek prompt medical care if she is on leave instead of working. Leave policies that provide health insurance coverage can also increase access to regular medical care. Additionally, leave policies may exert effects on family income depending on whether they are paid or unpaid, and therefore influence the family’s material resources available for child rearing.
In the U.S., before 1993, twenty-five states and the District of Columbia had enacted some type of family leave provisions, which were mostly unpaid and did not offer job protection, and varied in length between six and sixteen weeks (Trzcinski & Alpert, 1994). The Family and Medical Leave Act (FMLA), enacted at the federal level in 1993, mandated twelve weeks of unpaid job-protected family leave with continued coverage by the employer’s health insurance (if such coverage was already offered at the job). However, due to firm size and work history requirements, only slightly more than half of U.S. workers in the private sector were eligible. Currently, as only five states (California, Hawaii, New Jersey, New York, and Rhode Island) provide paid family leave either through the Temporary Disability Insurance (TDI) system or through explicit paid leave legislation, the vast majority of working parents in the U.S. are only covered by a relatively short and unpaid leave policy, if at all (Ruhm, 2011). In contrast, most other countries in the world have a national paid family leave policy. In fact, the U.S. is the only OECD country that does not provide some type of paid family leave on the national level.xvi
Yet although most developed countries have paid family leave policies, the existing research shows limited impacts of these policies on early childhood health. Cross-country analyses correlating the length of available parental leave with child mortality rates show that longer leaves are associated with lower post-neonatal and age one to five mortality rates in European countries (Ruhm, 2000; Tanaka, 2005). Yet it is difficult to draw causal conclusions from cross-country comparisons as other country-specific factors may be correlated with both leave provision and infant health. For example, Scandinavian countries, which tend to have some of the longest family leaves, also have a variety of other social safety net supports such as low-cost public childcare.
Other work has focused on one country at a time and examined the impacts of changes in leave availability due to expansions of existing leave policies and introductions of new ones. Such research designs can more credibly identify causal effects of family leave by comparing the outcomes of children who were born under more generous family leave regimes to those of similar children born during times of (or in areas with) less generous leave availability. Several such studies find that expansions in family leave have little effect on child well-being. Baker and Milligan (2010) study an expansion in paid maternity leave from six months to a year in Canada and show no statistically significant impacts on early childhood development indicators for children up to 29 months old. Dustmann and Schönberg (2012) consider three family leave reforms in Germany: an increase from two to six months of paid leave in 1979, an increase from six to ten months of paid leave in 1986, and an increase from 18 to 36 months of unpaid leave in 1986. None of these reforms exerted detectable effects on any long-run child outcomes, including grade retention, selective high school attendance, adult wages, and employment. Similarly, a Swedish expansion in paid leave from 12 to 15 months in 1988 had no significant impacts on a variety of child health measures or on children’s academic performance at age 16 (Liu & Skäns, 2010).
However, while these studies offer fairly credible evidence that extensions in paid family leaves longer than two months may not play a large role in influencing child well-being in Canada and Europe, they provide little guidance on what to expect from the introduction of (paid or unpaid) leave for the first time. Moreover, the institutional setting where a family leave policy is enacted likely matters. A reform that expands paid leave from 12 to 15 months in a setting with subsidized child care and universal health insurance (as is the case in Sweden, for example) is quite different from one that provides national family leave for the first time in a setting where neither child care nor health insurance is guaranteed (as would be the case if the United States implemented a national paid family leave policy). In fact, a recent study of the 1977 introduction of a four month paid leave in Norway, where the preceding policy only provided three months of unpaid leave, offers evidence that contrasts with the findings from the other studies in Europe and Canada. The implementation of the Norwegian policy had lasting beneficial impacts on children’s educational attainment, and especially helped children from disadvantaged backgrounds whose mothers were least likely to have had the means to take advantage of the former unpaid leave provisions (Carneiro, Løken, & Salvanes, 2011).
In the United States, a country with very limited leave provisions relative to the rest of the world, recent evidence suggests that even the 12 weeks of unpaid leave guaranteed by the FMLA can affect early-life health. Using variation in pre-FMLA maternity leave policies across states and in which firms are covered by FMLA provisions, Rossin (2011) finds that FMLA leads to small increases in birth weight of about 6 grams and fairly large reductions in infant mortality of about 10 percent. This effect would not be evident if one just simply compared child health in states with and without pre-FMLA leave policies in a descriptive analysis; in fact, states that had pre-FMLA leave provisions, like California, New York, and Washington, also had some of the highest infant mortality rates in the country in 1990.xvii This study thus highlights the importance of using an empirical design that can control for state-level characteristics associated with both family leave existence and child health in order to isolate the causal impact of family leave. The larger impact on infant mortality than birth weight in Rossin (2011) is also consistent with the fact that most women take leave after childbirth rather than during pregnancy. Moreover, these health benefits only accrue to children born to highly educated and married women, who are most likely to be eligible for FMLA and able to afford to take unpaid time off.
To date, there is very limited evidence on the consequences of the few state-level paid leave policies in the United States. Rossin-Slater, Ruhm, and Waldfogel (2013) show that California’s paid family leave program, which was introduced in 2004 and has very few eligibility restrictions, increased leave-taking among low-education, unmarried, and minority mothers who were previously taking an average of less than two weeks of leave. These findings point to the possibility that paid leave programs might provide less advantaged children with early-life health benefits in the U.S., although thorough research on this question has not yet been conducted.
In sum, the existing evidence is inconclusive on the role family leave may play in early childhood health. Although expansions in already generous paid leave programs around the world have had little effect on children’s early-life health or on measures of welfare throughout childhood and early adulthood, these analyses are not particularly informative for the U.S. context, which offers much shorter leaves to new parents. There is some evidence that the implementation of relatively short unpaid leave measures can benefit the children of mothers who are able to make use of them, implying that a paid leave program may have more far-reaching effects, especially in the disadvantaged population. However, more research is necessary to extract definitive conclusions on the benefits of family leave on early-life health in the U.S. Additionally, the existing research has primarily focused on how maternal leave-taking affects children’s outcomes—evidence about the effects of policies that some countries have adopted to encourage fathers to take paternity leave would be especially interesting.
Home Visiting
In the preceding sections, we have reviewed policies that can impact early-life health through altering the choices and constraints faced by pregnant women and new mothers. In contrast, a variety of initiatives target early-childhood circumstances with a broader approach by serving both parents and children at the same time. These programs seek to develop children’s cognitive and non-cognitive skills in early life and to provide low-income new parents with education about parenting skills, health, nutrition, and resource availability through regular home visits by program-trained paraprofessionals, nurses, or other child development professionals. Many such interventions have been implemented as randomized experiments, allowing for a thorough causal evaluation of their effects on child outcomes.
One of the first and largest such programs in the U.S. was the Comprehensive Child Development Program (CCDP). The Administration on Children, Youth, and Families within the U.S. Department of Health and Human Services made competitive grants available for local agencies to implement CCDP. Between 1989 and 1990, 24 sites in 22 states received these grants. The CCDP guidelines specified that families eligible for the program must meet the following criteria: a) they must have incomes below the federal poverty line, b) they must include a pregnant woman or a child under age one, and c) they must agree to participate in CCDP activities for five years. The eligible families were to be randomly assigned to one of three groups: program treatment group, control group, and replacement group. The replacement group provided a pool of families to be used by the CCDP projects to replace program drop-outs to maintain service levels and keep per-family costs under control and was not used in the evaluation. The grantees were asked to recruit eligible families (360 families in urban areas and 180 families in rural areas), which had to be proportionately representative of the low-income population in the grantee’s recruitment area in terms of ethnicity and maternal age. The intervention involved biweekly home visits by paraprofessionals, who were local community members with limited post-high school education, but who underwent program-specific training. The responsibilities of the home visitors included working with families to assess their goals and service needs, developing a service plan that referred families to services offered by the community, monitoring and recording the family’s receipt of services, and providing psychological counseling and support to both mothers and children.
An evaluation of CCDP was first conducted in 1990 at 21 of the original 24 sites, comparing outcomes of treatment and control groups over five years. On average, CCDP had little effect on the health and development of children in the treatment group across the 21 evaluation sites, except for some positive effects on some measures of child cognitive development and mothers’ parenting attitudes at one site in Vermont (St. Pierre & Layzer, 1999).
A similar home visiting program, called Healthy Families America (HFA), was first implemented in 1992. Although the primary goal of HFA is to reduce rates of child abuse and child maltreatment among at-risk populations, the program’s services (which include case management, service referrals, and parental education) can also impact other markers of early-life health. Like CCDP, HFA is administered through local agencies and thus the ex-act program details differ across sites. In general, the program recruits low-income pregnant women and mothers of newborns through a screening and assessment protocol. Participants can stay in the program for up to five years and receive weekly home visits. Unlike the CCDP, which employed home visitors with little formal training in child development, most of HFA’s home visitors have at least some college education with specializations in child development, social work, education, and nursing.
The evidence, based on at least 33 evaluation studies, suggests mixed effects of HFA on family outcomes. Some sites show positive effects on infant health and development, while others report reductions in rates of intimate partner violence and child abuse (see Harding et al., 2007 for a review). The variation in effects across sites in part stems from differences in program implementation and management. For instance, Harding et al. (2007) report that while all of the evaluated sites offered weekly visits, the actual duration of these services varied greatly. To produce a standardized measure of site quality, HFA has been applying a credentialing process—which delivers a rigorous assessment of program quality using trained peer reviewers—to all sites since 1997. These quality measures can in principle be used to determine whether heterogeneity in site quality plays an important role in explaining the variability in site effectiveness. However, only two of the evaluated HFA sites had completed the credentialing process prior to their evaluations. Additionally, the variation in site success is likely also driven by the substantial differences in participant risk factors across sites. Risk factors include: a history of domestic violence, maternal depression, child maltreatment, and maternal characteristics such as age, education, and income. For example, Harding et al. (2004) find that median family risk level was twice as high at some sites as in others.
While broad large-scale home visiting programs like the CCDP and HFA have had limited or mixed impacts on early-life circumstances, a more targeted intervention called the Nurse Home Visiting Partnership (NHVP) has had greater success. The program enrolls pregnant women with no prior births at less than 29 weeks of gestation who satisfy at least two of the following three criteria: they are unemployed, unmarried, or have less than 12 years of education. The women receive weekly home visits (which are gradually decreased in frequency to monthly) until their children are two years old. A key distinction of the NHVP is that all of the home visitors are certified nurses with formal training in women’s and children’s health. During the visits, the nurses are required to follow detailed guidelines that are specific to different stages of pregnancy and periods of child development. In particular, during pregnancy, the nurses help women complete 24-hour diet histories on a regular basis and plot weight gains at every visit. They assess their behaviors such as cigarette smoking and the use of alcohol and illegal drugs, and facilitate cessation through behavioral-change methods. The nurses teach women to identify signs of common pregnancy complications, encourage them to inform program staff about such complications, and promote compliance with recommended treatments. The pregnancy visits also include referrals to office-based prenatal care with physicians. Following childbirth, the nurses teach parents to take their newborns’ temperatures, detect signs of child illness, and communicate with program staff about any illnesses before seeking further care. The nurses follow specific program-developed curricula that promote parent-child interaction and instruct parents on how to understand infants’ and toddlers’ communicative signals. Finally, they teach parents how to play with their children in ways that promote emotional and cognitive development and how to develop safer households.
The NHVP has undergone randomized evaluations at three sites: Elmira, NY; Memphis, TN; and Denver, CO. These sites differed in their program participant racial and ethnic composition: Elmira participants were mostly non-Hispanic white, Memphis participants were mostly non-Hispanic black, while Denver participants were mostly Hispanic. Across the three sites, NHVP has been found to exert positive effects on a wide range of early childhood outcomes. Relative to children in control groups, treatment children experienced fewer health problems throughout childhood—for example, they had 23 percent fewer health encounters for injuries and ingestions as measured by hospitalizations and outpatient visits. Mothers in the treatment groups were 63 percent more likely to breastfeed. In the longer-term, treated children had 10 percent higher GPAs and scored 26 percent higher on math and reading achievement tests at age nine than their control group counterparts (Olds, 2006).
The positive impacts of NHVP are in line with randomized evaluations of very similar interventions in other contexts outside the U.S. For example, the Preparing for Life (PFL) program in Ireland, which was implemented between 2008 and 2010 and targeted disadvantaged pregnant women and new mothers, also exhibited consistent positive effects on a range of early childhood development indicators. PFL is somewhat more resource-intensive than NHVP as it incorporates weekly visits for families with children through age five (whereas the NHVP has less frequent visits through age two). Like NHVP, PFL also employs professionals as home visitors, although they include individuals with various educational backgrounds including social care, youth studies, psychology, and early childhood education (Doyle et al., 2013).
On the whole, the existing evidence suggests that home visiting interventions can be effective at improving early-life health and circumstances. However, the success of these programs likely depends on the level of program intensity (i.e., frequency of visits, curriculum breadth, etc.) and on the professional qualifications of the home visitors. The existing randomized evaluations suggest that large-scale interventions with low-education paraprofessional home visitors are generally ineffective, while more targeted programs with highly-trained nurse and early childhood professionals produce large positive impacts.
Early Childhood Care and Education
Head Start
We also review a group of interventions that consists of center-based programs providing care and education to children at young ages. We begin with Head Start, a federal program designed to promote school readiness of preschool-age children, which is one of the largest and oldest such programs in the U.S. The program was first implemented in 1965 as part of the War on Poverty with a goal of enhancing low-income children’s “cognitive, social, and emotional development.”xviii Head Start provides comprehensive services that include preschool education, medical, dental, and mental health care, nutrition services, and efforts to promote healthy relationships between parents and children. All Head Start programs serve preschool-age children and their families. Many programs also offer Early Head Start which expands the services to cover infants, toddlers, and pregnant women. Families are eligible if they have incomes below the federal poverty level, if they are homeless, or if they are receiving either TANF or Social Security Income (SSI) benefits. Additionally, foster children are eligible regardless of the foster family’s income level, and programs are required to set aside 10 percent of places for children with disabilities. Head Start is funded through federal grants awarded by the Office of Head Start within the Administration of Children and Families of the Department of Health and Human Services. Local public and private agencies compete for these grants to provide Head Start services.
A large body of research has examined the effectiveness of Head Start. When analyzing the program’s effects on children’s cognitive test scores, most of the evidence shows temporary improvements, followed by “fade-out” at later ages. For example, the federally mandated Head Start Impact Study, in which children on Head Start waitlists were either randomly assigned to one of 383 selected Head Start centers across 23 different states or to the control group with no Head Start exposure, analyzed the effects of Head Start using a sample of nearly 5,000 children. The results show that treatment children had higher cognitive test scores at the end of their time in Head Start. Yet these positive effects generally did not last after the children left the program—there were few statistically significant differences between the treatment and control groups in outcomes measured at the end of first grade (Office of Planning, Research, and Evaluation, 2010).
However, two important caveats should be noted with regard to the findings of the Head Start Impact Study. First, control-group children were allowed to attend other center-based care programs. As such, the experiment measured the effect of Head Start relative to other preschool programs, and cannot speak to whether Head Start might improve outcomes if the alternative were “no program at all.” Second, the study is silent on the possible longer-term effects on non-cognitive skill development, which may be especially important for long-term human capital accumulation and economic success (Heckman & Rubinstein, 2001; Heckman, Stixrud, & Urzua, 2006).
In fact, research using sibling comparisons (i.e., comparing siblings where one child at-tended Head Start while the other child did not) shows that despite the evidence of test score “fade-out,” long-term benefits persist. Children who attended Head Start are less likely to be placed in special education or retained in grade, and are more likely to graduate high school and attend college, have higher earnings in their 20s; they are also less likely to be booked or charged with a crime than their non-Head-Start-exposed siblings (Currie & Thomas, 1995; Garces, Thomas, & Currie, 2002). One study, Deming (2009), shows a gain of 0.23 standard deviations in a summary index of adult outcomes consisting of high school graduation, college attendance, “idleness” (an indicator for having no job and not being in school), crime, teen parenthood, and health status.
Several studies have examined the effects of Head Start on additional outcomes using other empirical designs. Ludwig and Miller (2007) exploit the fact that federal funding for Head Start was initially allocated to the 300 poorest counties and examine the effects of Head Start in a regression discontinuity design, essentially comparing the 300 poorest counties to the next 300 counties (i.e., the 301 to 600 poorest counties). If anything, outcomes in the poorest counties would be expected to be worse, but Ludwig and Miller (2007) instead find that Head Start counties had 35 to 80 percent lower child mortality rates. Frisvold and Lumeng (2011) use variation across states in the 1990s stemming from the elimination of a state-provided full-day expansion grant that decreased the supply of full-day Head Start classes. They show that early childhood access to full-day Head Start reduces the incidence of childhood obesity by over 100 percent among black children aged five to ten. However, the reductions in obesity do not last past age ten.
Finally, two more recent studies using experimental data from the Head Start Impact study show effects on new dimensions. Gelber and Isen (2013) find that Head Start participation is associated with greater parental involvement as measured by time spent reading, practicing math, and days spent with fathers who do not live with their children. Bitler, Domina, and Hoynes (2012) show that although earlier evaluations based on the Head Start Impact Study documented test score “fade-out” when examining average test scores, the data also point to important distributional effects on cognitive outcomes—initial test score gains are concentrated in the bottom of the baseline score distribution, and the impacts persist through first grade for some disadvantaged groups including Spanish speakers and children with low baseline scores.
In sum, despite some findings of cognitive test score “fade-out,” there is substantial evidence pointing to long-term benefits of Head Start for individual socio-economic well-being and health. It is possible that this discrepancy highlights the importance of non-cognitive skills in shaping adult well-being. For example, children who have an initially more positive experience of school, and who learn skills such as completing tasks and resolving conflicts may be more likely to ultimately succeed in life. Although Head Start curricula are often evaluated solely on the basis of their approach to academic skills (such as number and letter recognition), popular curricula such as High Scope have always emphasized a holistic approach to preschool education that emphasizes such “soft” skills.
Randomized Early Childhood Education Interventions
In addition to the federally-funded Head Start program, there have been a number of other much smaller-scale early childhood education interventions, which were often implemented as randomized experiments. The HighScope Perry Preschool study is one of the first such experiments. The intervention identified 123 low-income African-American children ages three and four in Ypsilanti, Michigan in the early 1960s, and randomly assigned 58 of these children to the treatment group. Treatment lasted for two years and consisted of a 2.5 hour preschool program on weekdays during the school year as well as weekly home visits by teachers. The program curriculum was centered on “active learning,” where children were encouraged to plan, carry out, and reflect on their own activities through a “plan-do-review” process. The children were also urged to make choices and solve problems. The program emphasized reflective and open-ended questions asked by teachers instead of strictly organized lesson plans. After the intervention ended, the treatment and control groups were followed through age 40.
The existing evidence on the Perry program shows remarkable lasting effects on a wide range of outcomes throughout the lifecycle. Treatment children performed better on school achievement tests and were more likely to graduate high school. Treatment individuals were also more likely to be employed, less likely to be receiving social assistance, and less likely to be involved in criminal activities or interacting with the criminal justice system throughout adulthood. Overall, treatment individuals had 11 to 36 percent higher lifetime earnings than the control group (Belfield et al., 2006). Even when accounting for issues with the randomization protocol, researchers estimate that the Perry program had meaningful social rates of return (7 to 10 percent), implying a benefit-cost ratio of between 2.2 and 3.2 (Heckman et al., 2010).
A similar but longer early childhood intervention, called the Abecedarian Project, was conducted in the 1970s. The program selected 112 children of mostly African-American descent who were evaluated to be at risk for delayed cognitive development based on a variety of factors such as household income, parental education, and parental IQ. The children were randomly assigned into treatment and control groups. The treatment children entered the program when they were between 6 and 12 weeks old and stayed through age five.xix The program was entirely center-based with teacher/child ratios that ranged from 1:3 for infants and toddlers to 1:6 for older children. The center operated from 7:30 a.m. to 5:30 p.m. on weekdays for 50 weeks out of the year and provided free transportation. The curriculum was based on language development and tailored to the individual needs of the children. The experiment participants have been followed through their mid-30s.
Like the Perry program, the Abecedarian intervention also had important long-term benefits. Relative to the control group, treatment group children had 48 percent less grade retention, were 37 percent less likely to be in special education, were 33 percent less likely to drop out of high school, and were more than 170 percent more likely to attend college. Researchers focusing on wage and employment gains estimate that the program benefits far outweighed the costs: per participant, the program cost $34,599, and led to an average $72,591 benefit in 2002 dollars (Masse & Barnett, 2002). Using recently collected biomedical data, researchers have found important gains in terms of health as well. They find that the treatment group had significantly lower prevalence of risk factors for cardiovascular and metabolic diseases in their mid-30s and that the gains are particularly strong for males. Treatment males had significantly lower blood pressure, and were less likely to suffer from metabolic syndrome, which predisposes individuals to heart disease and diabetes (Campbell et al., 2014).
Another important randomized intervention, the Infant Health and Development Project (IHDP), was conducted at eight sites throughout the U.S. from 1985 to 1988. Unlike Perry Preschool and the Abecedarian Project, IHDP did not restrict eligibility based on family income or demographics, but instead targeted low-birth-weight (<2,500 grams) and preterm-born (<37 weeks gestation) children. The IHDP treatment group was offered home visits and Abecedarian-type center-based care. Home visits began shortly after birth, while center-based care was initiated at age one and lasted through age three. The 377 treatment and 608 control group children were then followed through age 18. The program had large positive effects on children’s cognitive ability both in childhood (ages three to eight) and in young adulthood (age 18), with larger impacts for children from lower-income backgrounds (McCormick et al., 2006). Duncan and Sojourner (2013) estimate that if such a program were scaled up and offered to low-income children throughout the U.S., it would entirely eliminate the income-based gap in cognitive ability at age three, and close between one third and three quarters of the gap at ages five and eight.
In sum, targeted intensive early childhood center-based education programs have been shown to be very effective at improving both cognitive and non-cognitive outcomes throughout life.
Universal Pre-Kindergarten Programs
We have thus far described programs that target low-income or otherwise disadvantaged children. However, some government-funded early childhood programs might instead be offered universally in the belief that they can benefit all children and to generate more political support. The evidence on existing universal pre-kindergarten (pre-K) programs can help inform whether such programs might be effective.
As of 2012, 40 U.S. states and Washington D.C. had some kind of pre-K program in place.xx These states vary substantially in terms of access—for example, only 1 percent of Rhode Island’s four-year old children are enrolled in a pre-K program, while nearly 80 percent of Florida’s four-year-olds are enrolled. These programs are funded, directed, and controlled by the state, and must serve preschool-age children (younger children can be served as well, but programs serving only infants and toddlers are not considered pre-K). The initiatives focus on center-based early childhood education and must offer a group learning experience to children at least two days per week.
As the programs are meant to be nearly universal, they do not contain a randomized implementation design like those described in the previous section. Thus, most of the evidence on pre-K programs comes from regression discontinuity analyses that compare children with birthdays surrounding the state eligibility cut-off date. More specifically, most states require that children must turn a certain age (three or four years old) by a particular date (e.g., September 1) in order to enroll in pre-K. Thus, around that date in any given year, children who were born just before that date will have completed a year of pre-K, while slightly younger children born just after that date will have not yet begun the program. A comparison of these children’s outcomes can shed light on the effects of the program. The results from such analyses show that pre-K programs in Michigan, New Jersey, New Mexico, Oklahoma, and South Carolina have had positive effects on a variety of measures of children’s cognitive ability (Gormley & Gayer, 2005; Hustedt et al., 2008; Wong et al., 2008).
However, despite the apparent benefits of pre-K programs in some U.S. states, evidence from other countries suggests some caution. For example, Baker, Gruber, and Milligan (2008) examine the introduction of universal, highly-subsidized childcare in Quebec for pre-school children and show that this program led to adverse effects on children’s behavioral and health outcomes. These results point out that program quality and the availability and quality of alternative options for childcare are likely important determinants of program success.
In sum, many early childhood care and education programs have been shown to have positive impacts on both short- and long-run outcomes of children. Some of the most promising evidence comes from small intensive randomized interventions such as the Perry Preschool, the Abecedarian Project, and the IHDP. However, even larger-scale programs like Head Start and universal pre-K can have important although at times smaller benefits.
Public Health Educational Campaigns
In addition to the relatively well-defined public programs and policies discussed above, the government has periodically conducted public education campaigns aimed at promoting healthy behaviors among pregnant women and new parents. These programs tend to be diffuse, episodic, and often involve partners at many levels (such as federal, state, and local governments and private entities such as the American Academy of Pediatrics or the March of Dimes), making it challenging to obtain information about program elements. Moreover, often there is scant information available about the prevalence of the targeted behavior so that it is difficult to judge the effectiveness of the campaigns using standard policy evaluation tools.
Efforts to reduce Sudden Infant Death Syndrome (SIDS) by educating the public about the safest ways for infants to sleep are an excellent example of this type of campaign.xxi SIDS is the sudden death of an infant under one year of age from an unexplained cause. The majority of these deaths occur before the infant reaches six months of age. SIDS usually occurs when a baby is sleeping, and is therefore also commonly known as a “crib death.”
In 1992, following years of research into the causes of SIDS and public health initiatives in other countries such as the United Kingdom, the American Academy of Pediatrics (AAP) recommended that infants be placed on their backs to sleep. In 1994, the U.S. Surgeon General issued a policy statement that infants should be placed on their backs to sleep, and the National Institutes of Health (NIH) launched the “Back to Sleep” campaign in collaboration with the AAP, the Public Health Service, and other organizations. The initial campaign included mailings to members of the AAP, the American College of Obstetricians and Gynecologists, WIC providers, and all hospitals with newborn nurseries. In addition, public service announcements were sent to thousands of radio and television stations.
Over the years, the campaign enlisted private partners such as Gerbers, Pampers, and Johnson & Johnson, who included messages with their products; periodically updated its messages to target other problems such as soft bedding and bed-sharing; and crafted specific campaigns for child care centers, nurses who care for newborns, and African-Americans and Native Americans (both groups who have higher rates of SIDS). In addition, the federal government has periodically partnered with states, such as Mississippi, and with large cities, such as Chicago, which have relatively high rates of SIDS deaths. In 2011, the AAP updated its recommendations to include a wider array of safe sleeping measures, and in 2012, the NIH launched an updated campaign called “Safe to Sleep” that incorporated these recommendations. Because little data was available about infant sleeping practices, the government also conducted the National Infant Sleep Position study from 1992 to 2010, which collected data through telephone surveys of 1,000 mothers per year. Questions about infant sleeping positions were also included in the Pregnancy Risk Assessment Monitoring study, which samples birth certificates and surveys large samples of new mothers in participating states.
Given the length and scope of the campaign, it is perhaps surprising that we know relatively little about the effectiveness of its key elements. Between 1992 and 2001, SIDS rates fell from 120 to 56 deaths per 100,000 live births; over the same period, the incidence of supine (back) sleeping increased from 13 to 72 percent. Since 2001, both rates have been relatively flat (American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome, 2011). Clearly, the two series are correlated; however in social science it has become almost a cliché to point out that correlation does not necessarily imply causation.
Evaluations of more targeted parts of the intervention have produced somewhat mixed results. For example, Rasinski et al. (2003) evaluate an education campaign in African-American neighborhoods in Chicago. They find that the campaign resulted in some reductions in the numbers of mothers reporting that they put their infants to sleep on adult beds or sofas, though the declines were not statistically significant. The researchers do observe that mothers who had been instructed about sleep position in the hospital were more likely to use the supine position for their babies. Moon et al. (2004) evaluate a parent education program conducted at a WIC clinic in Washington, D.C. and report that after a 15-minute small-group training session, parents increased the probability that infants were placed on their backs six months after the intervention from 45 to 75 percent. In a study that goes beyond simple before and after comparisons, Moon et al. (2008) evaluate a training program for workers in child care centers. The trainers conducted an initial evaluation of sleep practices, and then randomized some centers to a training program and others to be a control group. Three months after the intervention, they found that the placement of infants on their backs to sleep increased from 51 to 57 percent in the control centers and from 51 to 62 percent in the treatment centers. As a group, these studies suggest that public health interventions like the “Back to Sleep” campaign may be effective, but do not provide strong causal evidence of effectiveness, and do not give the policymaker much advice about how best to structure such programs.
Another important example of a public health intervention targeting pregnant women is the federal requirement that all containers of alcoholic beverages sold or distributed in the United States carry the following warning label: “GOVERNMENT WARNING: (1) ACCORDING TO THE SURGEON GENERAL, WOMEN SHOULD NOT DRINK ALCOHOLIC BEVERAGES DURING PREGNANCY BECAUSE OF THE RISK OF BIRTH DEFECTS.” The rule became mandatory on November 14, 1990. This warning was aimed at preventing fetal alcohol syndrome, a leading preventable cause of mental retardation that was first identified as a syndrome in 1973 (U.S. Department of Health and Human Services, 2009). Evaluation of this intervention is hampered by the fact that it was a national intervention (hence, making it challenging to find a suitable comparison group), and by the absence of reliable time-series data either about drinking during pregnancy or about the prevalence of fetal alcohol syndrome. For example, while birth records have routinely included information about drinking during pregnancy and fetal alcohol syndrome, this information does not appear to be reliable (Druschel & Fox, 2007; Vinikoor et al., 2010). The result is that there actually have been few evaluations of the effect of the warning label on drinking among pregnant women. One evaluation of the effect of the warning label in a sample of African-American women found that after the introduction of the warning label, alcohol drinking fell among light drinkers, but not among heavy drinkers (Hankin, Sloan, & Sokon, 1998).
There is relatively more research on anti-smoking public health interventions, however. The 1964 Surgeon General Report on smoking and health was the first widely publicized report to highlight the adverse link between maternal smoking during pregnancy and infant health (specifically, birth weight). Following the release of the report, additional information on smoking and health became available, and all cigarette packages were required to have warning labels starting in 1966. Using a historical data set that includes information on the smoking habits of pregnant women from 1959 to1966, Aizer and Stroud (2010) find that immediately following the release of the report, highly educated mothers reduced their smoking levels, while less educated mothers did not. As a result, the birth outcomes of more educated mothers improved, and infant health disparities between these groups widened. Unfortunately, data on smoking during pregnancy during the 1970s and 1980s—when many states implemented anti-smoking campaigns—is not available because states only began including information on maternal smoking on birth certificates in 1989 (Mathews, 2001). Studies of more recent anti-smoking campaigns, which typically use large cigarette tax hikes as their primary policy levers, have shown reductions in smoking during pregnancy and associated decreases in low-birth-weight rates (Evans & Ringel, 2001; Evans & Lien, 2005b).
A third type of public health policy involves mandates pertaining to many different specific products. For example, the addition of folic acid to grain and cereal products (which became mandatory in the United States in 1998) in order to prevent neural tube defects is estimated to have reduced the incidence of such defects by 25 to 30 percent (Pitkin, 2007). Other mandates which have demonstrably improved children’s health include infant car seats, window bars in New York City, and safety caps on prescription drugs, among many others (Committee on Injury, Violence and Poison, Prevention and Durbin, DR, 2011; Bijur & Spiegel, 1996; Rodgers, 1996). This regulatory function of government should not be overlooked when considering policies to promote early childhood health. Although it is difficult to draw sweeping conclusions about the factors most likely to contribute to success in a public health campaign, the examples discussed above highlight either national campaigns that were of broad scope and sustained over many years, or very local and specific campaigns which resulted in specific product mandates. It seems likely that diffuse and episodic campaigns may be less likely to be effective.
CONCLUSION
The U.S. disadvantage in infant health relative to countries with similar GDP levels could have far-reaching implications for future economic growth—mounting evidence across several disciplines suggests that early-life conditions can have lasting effects on human capital formation and adult economic outcomes. This paper has provided a review of the evidence on the link between early childhood health and well-being and outcomes throughout the life course, drawing on research from epidemiology and economics. The studies on this topic exhibit substantial variation in empirical methodology, data, and context. However, despite this variation, the research points to robust and lasting consequences of early-life conditions. Additionally, recent theoretical contributions posit important complementarities between investments at different stages of child development, providing a plausible explanation for why early childhood factors might play such a significant role in life-long well-being. The evidence also suggests a close connection between children’s physical and cognitive outcomes. Thus, the traditional siloing of programs according to what aspect of child development they target may not be the most productive approach.
We also have reviewed the evidence on the effectiveness of a variety of existing interventions targeting the early-life environment. We highlight several examples in which simple comparisons of program participants with non-participants yield misleading conclusions. Often this is a result of the way that people are selected to participate in the programs—most programs we consider aim to help the disadvantaged, who, other things being equal, would be expected to have the worst outcomes.
Some of the most promising proven policies include WIC, home visiting initiatives employing nurse practitioners, and center-based early childhood care and education intervention programs that use intensive “active-learning” curricula. This research thus points to an important window of opportunity for improving children’s life chances through evidence-based early-life interventions. It is worth noting that these successful programs all take a relatively holistic view of child well-being and address it in multiple ways. There is less information to support the idea that further expansions of access to traditional medical care will have a major impact. This is perhaps good news, as it reflects the substantial improvements in child health and increases in access to care that have already been achieved.
Arguably, however, the evidence base does not yet answer the question policymakers most want to know, which is what programs they should invest in if they wish to get the highest return on their investments in early childhood. This type of comparison across programs is hampered by a lack of consistency in cost-benefit analyses (or in many cases the absence of cost-benefit analysis). Common problems include: a lack of cost information; lack of specifics about the program elements; disagreement about the most important childhood benefits to be measured; and disagreement about how to monetize benefits. As a recent National Academy workshop suggested, standards for cost-benefit analyses might help to address this important gap in the literature (Institute of Medicine and National Research Council, 2014). Moreover, the fact that programs exist at all levels of government, from the federal to the very local, may be a further impediment to collection of data and comparison across programs.
One helpful frame for future policymaking might come from reflecting on the fact that social factors, injuries, and mental health conditions are the major threats to today’s children, rather than exposure to infectious disease. Thus, programs that address these threats are most likely to be successful.
Acknowledgments
We are grateful to Ken Couch as well as three anonymous referees for their helpful comments. We also thank Jenna Stearns for excellent research assistance.
The grant number is P2C HD047879
Footnotes
JEL Codes: H40, H43, H75, I10, I12, I14, I18, I30, J1
See Currie, 2011, for a discussion of the causes and consequences of inequalities at birth.
For a review of the evidence on the link between pollution and early-life health, see Currie et al., 2014.
This information is based on data from the National Center for Health Statistics natality records on all 2011 births.
See, for example: Conley & Bennett (2001); Behrman & Rosenzweig (2004); Conley, Pfeiffer, & Velez (2007); Currie & Moretti (2007); Oreopoulos et al. (2008); Salm & Schunk (2008); Royer (2009); Lin & Liu (2009); Currie et al.. (2010); Johnson & Schoeni (2011); Webbink et al. (2012); Bharadwaj, Lundborg, & Rooth (2013). For a review of studies in developing countries, see Currie & Vogl (2013).
This paper has been criticized on the grounds that due to the effects of World War I on fertility, the affected cohorts may have been different in other respects than the preceding cohorts (Brown & Thomas, 2011). However, several other papers have also found negative long-term impacts of in utero flu exposure (Kelly, 2011; Lin & Liu, 2014), and the Almond (2006) study also exploited variation in the timing of the flu outbreak across the country to identify its effects.
See Barreca (2010) for evidence of adverse effects of in utero exposure to other disease outbreaks, such as malaria.
See, also Reyes (2007), Nilsson (2014), and Rau, Reyes, & Urzua (2013) for evidence of the relationship between early-life exposure to lead and adult outcomes.
Phylloxera are very small insects who feed on the roots and leaves of grapevines.
Other studies looking at the long-run effects of policies (not necessarily targeting the early childhood period only) include: Bharadwaj, Løken, & Neilson (2013); Isen, Rossin-Slater, & Walker (2014); Nilsson, 2014; Simon, 2014; and Miller & Wherry, 2014.
See Dunkel-Schetter (2011) as well as a review of the literature in Jaddoe (2006).
This information comes from our own calculations using National Center for Health Statistics natality records on all 2011 births.
Please see http://www.ncbi.nlm.nih.gov/books/NBK11359/ for more details.
As an instrument, they use a measure of the number of women who would be eligible for Medicaid in a fixed population of women given changes in the state’s Medicaid rules. This measure captures changes in the generosity of insurance without being contaminated by the effects of changes in economic conditions.
See Gruber and Simon (2008) for a recent discussion on whether public health insurance expansions crowd-out private health insurance use.
See http://www.bls.gov/cps/wlf-databook-2012.pdf for more information.
See http://www.mcgill.ca/files/ihsp/WFEI2007.pdf for more information on family leave policies around the world.
xviii: See: http://www.acf.hhs.gov/programs/ohs/about.
The children were further randomized at school entry to receive additional services, but these services have not been shown to have been effective (Barnett, 1995).
See http://nieer.org/sites/nieer/files/yearbook2012.pdf for more information.
Further information about the history of this campaign can be found at: http://www.nichd.nih.gov/sts/campaign/moments/Pages/default.aspx.
Contributor Information
Janet Currie, Email: jcurrie@princeton.edu, Henry Putnam Professor of Economics and Public Affairs and the Director of the Center for Health and Well-Being for the Woodrow Wilson School of Public and International Affairs at Princeton University, 316 Wallace Hall, Princeton, NJ 08544. Tel: 609-258-7393.
Maya Rossin-Slater, Email: maya.rossin-slater@ucsb.edu, Assistant Professor of Economics at the University of California at Santa Barbara, 2127 North Hall, UC Santa Barbara, CA 93106. Tel: 805-893-4823.
References
- Abrevaya J, Dahl CM. The effects of birth inputs on birthweight: Evidence from quantile estimation on panel data. Journal of Business & Economic Statistics. 2008;26:379–397. [Google Scholar]
- Ahluwalia IB, Hogan VK, Grummer-Strawn L, Colville W, Peterson A. The effect of WIC participation on small-for-gestational-age births: Michigan, 1992. American Journal of Public Health. 1998;88:1374–1377. doi: 10.2105/ajph.88.9.1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizer A, Currie J. The intergenerational transmission of inequality: Maternal disadvantage and health at birth. Science. 2014;344:856–861. doi: 10.1126/science.1251872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aizer A, Stroud L. Education, knowledge, and the evolution of disparities in health. Brown University; 2010. unpublished manuscript. [Google Scholar]
- Aizer A, Stroud L, Buka S. Maternal stress and child well-being: Evidence from siblings, Brown University working paper. 2009. [Google Scholar]
- Almond D. Is the 1918 influenza pandemic over? Long-term effects of in utero influenza exposure in the post-1940 US population. Journal of Political Economy. 2006;114:672–712. [Google Scholar]
- Almond D, Chay KY, Lee DS. The costs of low birth weight. The Quarterly Journal of Economics. 2005;120:1031–1083. [Google Scholar]
- Almond D, Currie J. Human capital development before age five. In: Ashenfleter O, Card D, editors. Handbook of Labor Economics. Vol. 4. Elsevier; 2011. pp. 1315–1486. [Google Scholar]
- Almond D, Edlund L, Palme M. Chernobyl’s subclinical legacy: Prenatal exposure to radioactive fallout and school outcomes in Sweden. The Quarterly Journal of Economics. 2009;124:1729–1772. [Google Scholar]
- Almond D, Mazumder B. The 1918 influenza pandemic and subsequent health out-comes: an analysis of SIPP data. American Economic Review Papers & Proceedings. 2005;95:258–262. doi: 10.1257/000282805774669943. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: Expansion of recommendations for a safe infant sleeping environment. Pediatrics. 2011;128:1341–1467. doi: 10.1542/peds.2011-2284. [DOI] [PubMed] [Google Scholar]
- Baker M, Gruber J, Milligan K. Universal child care, maternal labor supply, and family well-being. Journal of Political Economy. 2008;116:709–745. [Google Scholar]
- Baker M, Milligan K. Evidence from maternity leave expansions of the impact of maternal care on early child development. Journal of Human Resources. 2010;45:1–32. [Google Scholar]
- Banerjee A, Duflo E, Postel-Vinay G, Watts T. Long-run health impacts of income shocks: Wine and phylloxera in nineteenth-century France. The Review of Economics and Statistics. 2010;92:714–728. [Google Scholar]
- Barker DJ. The fetal and infant origins of adult disease. BMJ: British Medical Journal. 1990;301:1111. doi: 10.1136/bmj.301.6761.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett SW. Long-term effects of early childhood programs on cognitive and school outcomes. The Future of Children. 1995;5:25–50. [PubMed] [Google Scholar]
- Barreca AI. The long-term economic impact of in utero and postnatal exposure to malaria. Journal of Human Resources. 2010;45:865–892. [Google Scholar]
- Becker GS, Tomes N. An equilibrium theory of the distribution of income and intergenerational mobility. The Journal of Political Economy. 1979;87:1153–1189. [Google Scholar]
- Becker GS, Tomes N. Human capital and the rise and fall of families. Journal of Labor Economics. 1986;4:S1–S39. doi: 10.1086/298118. [DOI] [PubMed] [Google Scholar]
- Behrman JR, Rosenzweig MR. Returns to birthweight. Review of Economics and Statistics. 2004;86:586–601. [Google Scholar]
- Behrman RE, Butler AS. Institute of medicine (US). Committee on understanding premature birth and assuring healthy outcomes. Preterm birth: causes, consequences, and prevention. 2007 [PubMed] [Google Scholar]
- Belfield CR, Nores M, Barnett S, Schweinhart L. The HighScope Perry Preschool Program cost–benefit analysis using data from the age-40 followup. Journal of Human Resources. 2006;41:162–190. [Google Scholar]
- Bharadwaj P, Eberhard J, Neilson C. Health at birth, parental investments and academic outcomes. UC; San Diego: 2013. unpublished manuscript. [Google Scholar]
- Bharadwaj P, Løken KV, Neilson C. Early life health interventions and academic achievement. American Economic Review. 2013;103(5):1862–91. [PubMed] [Google Scholar]
- Bharadwaj P, Lundborg P, Rooth DO. The effects of birth weight over the life cycle. UC; San Diego: 2013. unpublished manuscript. [Google Scholar]
- Bhattacharya J, Currie J. Youths at nutrition risk: Malnourished or misnourished? In: Gruber J, editor. Risky behavior among youths: An economic analysis. University of Chicago Press; 2001. pp. 483–522. [Google Scholar]
- Bijur P, Spiegel C. Pediatric Research. Vol. 39. Baltimore, MD: Williams & Wilkins; 1996. Window fall prevention and fire safety: 20 years of experience in New York City; pp. 599–599. [Google Scholar]
- Bitler M, Domina T, Hoynes HW. Experimental evidence on distributional effects of Head Start. UC; Irvine: 2012. unpublished manuscript. [Google Scholar]
- Bitler MP, Currie J. Does WIC work? The effects of WIC on pregnancy and birth outcomes. Journal of Policy Analysis and Management. 2005;24:73–91. doi: 10.1002/pam.20070. [DOI] [PubMed] [Google Scholar]
- Black SE, Butikofer A, Devereux PJ, Salvanes KG. This is only a test? (NBER Working Paper 18987).Long-run impacts of prenatal exposure to radioactive downfall. 2013 [Google Scholar]
- Black SE, Devereux PJ, Salvanes KG. From the cradle to the labor market? The effect of birth weight on adult outcomes. The Quarterly Journal of Economics. 2007;122:409–439. [Google Scholar]
- Boudreaux M, Golberstein E, McAlpine D. The long-term impacts of Medicaid in early childhood. University of Minnesota, School of Public Health; 2014. unpublished manuscript. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown R, Thomas D. On the long term effects of the 1918 US influenza pandemic. Duke University; 2011. unpublished manuscript. [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, Pan Y. Early childhood investments substantially boost adult health. Science. 2014;343:1478–1485. doi: 10.1126/science.1248429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card D. The causal effect of education on earnings. Handbook of Labor Economics. 1999;3:1801–1863. [Google Scholar]
- Carneiro P, Løken KV, Salvanes KG. A flying start? Maternity leave benefits and long run outcomes of children. Institute for the Study of Labor (IZA); 2011. (Discussion Paper 5793). [Google Scholar]
- Case A, Fertig A, Paxson C. The lasting impact of childhood health and circumstance. Journal of Health Economics. 2005;24:365–389. doi: 10.1016/j.jhealeco.2004.09.008. [DOI] [PubMed] [Google Scholar]
- Case A, Paxson C. Height, health, and cognitive function at older ages. The American Economic Review Papers & Proceedings. 2008a;98:463–467. doi: 10.1257/aer.98.2.463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Paxson C. Stature and status: Height, ability, and labor market outcomes. Journal of Political Economy. 2008b;116 doi: 10.1086/589524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case A, Paxson C. Causes and consequences of early-life health. Demography. 2010;47:S65–S85. doi: 10.1353/dem.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. CDC grand rounds: Public health approaches to reducing US infant mortality. Morbidity and Mortality Weekly Report. 2013;62(31):625. [PMC free article] [PubMed] [Google Scholar]
- Chatterji P, Brooks-Gunn J. WIC participation, breastfeeding practices, and well-child care among unmarried, low-income mothers. American Journal of Public Health. 2004;94:1324. doi: 10.2105/ajph.94.8.1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen A, Oster E, Williams H. Why is infant mortality in the US higher than in Europe? University of Chicago; 2014. unpublished manuscript. [Google Scholar]
- Committee on Injury, Violence and Poison, Prevention. Durbin DR. Child passenger safety. Pediatrics. 2011;127:788. doi: 10.1542/peds.2011-0213. [DOI] [PubMed] [Google Scholar]
- Conley D, Bennett NG. Birth weight and income: interactions across generations. Journal of Health and Social Behavior. 2001;42:450–465. [PubMed] [Google Scholar]
- Conley D, Pfeiffer KM, Velez M. Explaining sibling differences in achievement and behavioral outcomes: The importance of within-and between-family factors. Social Science Research. 2007;36:1087–1104. [Google Scholar]
- Cunha F, Heckman J. The technology of skill formation. American Economic Review. 2007;97:31–47. [Google Scholar]
- Cunha F, Heckman JJ. Formulating, identifying and estimating the technology of cognitive and noncognitive skill formation. Journal of Human Resources. 2008;43:738–782. doi: 10.3982/ECTA6551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunha F, Heckman J, Schennach SM. Estimating the technology of cognitive and noncognitive skill formation. Econometrica. 2010;78:883–931. doi: 10.3982/ECTA6551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J. U.S. food and nutrition programs. In: Moffitt RA, editor. Means-tested transfer programs in the US. The University of Chicago Press; 2003. [Google Scholar]
- Currie J. Inequality at birth: Some causes and consequences. The American Economic Review. 2011;101:1–22. [Google Scholar]
- Currie J, Decker S, Lin W. Has public health insurance for older children reduced disparities in access to care and health outcomes? Journal of Health Economics. 2008;27:1567–1581. doi: 10.1016/j.jhealeco.2008.07.002. [DOI] [PubMed] [Google Scholar]
- Currie J, Gruber J. Health insurance eligibility, utilization of medical care, and child health. The Quarterly Journal of Economics. 1996a;111:431–466. [Google Scholar]
- Currie J, Gruber J. Saving babies: The efficacy and cost of recent changes in the Medicaid eligibility of pregnant women. Journal of Political Economy. 1996b;104:1263–1296. [Google Scholar]
- Currie J, Hyson R. Is the impact of health shocks cushioned by socioeconomic status? The case of low birthweight. American Economic Review. 1999;89:245–250. [Google Scholar]
- Currie J, Moretti E. Biology as destiny? Short- and long-run determinants of inter-generational transmission of birth weight. Journal of Labor Economics. 2007;25 [Google Scholar]
- Currie J, Rajani I. Within-Mother Estimates of the Effects of WIC on Birth Outcomes in New York City. National Bureau of Economic Research; 2014. (Working Paper 20400). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Rossin-Slater M. Weathering the storm: Hurricanes and birth outcomes. Journal of Health Economics. 2013;32:487–503. doi: 10.1016/j.jhealeco.2013.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Schwandt H. Within-mother analysis of seasonal patterns in health at birth. Proceedings of the National Academy of Sciences. 2013;110:12265–12270. doi: 10.1073/pnas.1307582110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J, Stabile M, Manivong P, Roos LL. Child health and young adult outcomes. Journal of Human Resources. 2010;45:517–548. [Google Scholar]
- Currie J, Thomas D. Does head start make a difference? American Economic Review. 1995;85:341–364. [Google Scholar]
- Currie J, Vogl T. Early-life health and adult circumstance in developing countries. Annual Review of Economics. 2013;5:1–36. [Google Scholar]
- Currie J, Zivin JG, Mullins J, Neidell M. What do we know about short- and long-term effects of early-life exposure to pollution? Annual Review of Resource Economics. 2014;6 [Google Scholar]
- Dafny L, Gruber J. Public insurance and child hospitalizations: Access and efficiency effects. Journal of Public Economics. 2005;89:109–129. [Google Scholar]
- Dave DM, Decker S, Kaestner R, Simon KI. Re-examining the Effects of Medicaid Expansions for Pregnant Women. National Bureau of Economic Research; 2008. (Working Paper 14591). [Google Scholar]
- Deming D. Early childhood intervention and life-cycle skill development: Evidence from head start. American Economic Journal: Applied Economics. 2009:111–134. [Google Scholar]
- Doyle O, Harmon C, Heckman JJ, Logue C, Moon S. Measuring Investment in Human Capital Formation: An Experimental Analysis of Early Life Outcomes. National Bureau of Economic Research; 2013. (@Working Paper 19316). [Google Scholar]
- Druschel CM, Fox DJ. Issues in estimating the prevalence of fetal alcohol syndrome: Examination of 2 counties in New York State. Pediatrics. 2007;119:e384–e390. doi: 10.1542/peds.2006-0610. [DOI] [PubMed] [Google Scholar]
- Duncan GJ, Sojourner AJ. Can intensive early childhood intervention programs eliminate income-based cognitive and achievement gaps? Journal of Human Resources. 2013;48:945–968. doi: 10.3368/jhr.48.4.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel-Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dustmann C, Schönberg U. Expansions in maternity leave coverage and children’s long-term outcomes. American Economic Journal: Applied Economics. 2012;4:190–224. [Google Scholar]
- Evans WN, Lien DS. The benefits of prenatal care: Evidence from the PAT bus strike. Journal of Econometrics. 2005a;125:207–239. [Google Scholar]
- Evans WN, Lien DS. Estimating the impact of large cigarette tax hikes: The case of maternal smoking and infant birth weight. Journal of Human Resources. 2005b;40:373–392. [Google Scholar]
- Evans WN, Ringel JS. Cigarette taxes and smoking during pregnancy. American Journal of Public Health. 2001;91:1851–1856. doi: 10.2105/ajph.91.11.1851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figlio D, Hamersma S, Roth J. Does prenatal WIC participation improve birth outcomes? New evidence from Florida. Journal of Public Economics. 2009;93:235–245. [Google Scholar]
- Figlio DN, Guryan J, Karbownik K, Roth J. The effects of poor neonatal health on children’s cognitive development. National Bureau of Economic Research; 2013. (Working Paper 18846). [DOI] [PubMed] [Google Scholar]
- Fiscella K. Does prenatal care improve birth outcomes? A critical review. Obstetrics & Gynecology. 1995;85:468–479. doi: 10.1016/0029-7844(94)00408-6. [DOI] [PubMed] [Google Scholar]
- Frisvold DE, Lumeng JC. Expanding exposure: Can increasing the daily duration of head start reduce childhood obesity? Journal of Human Resources. 2011;46:373–402. [Google Scholar]
- Garces E, Thomas D, Currie J. Longer-term effects of Head Start. The American Economic Review. 2002;92:999–1012. [Google Scholar]
- Gelber A, Isen A. Children’s schooling and parents’ behavior: Evidence from the Head Start impact study. Journal of Public Economics. 2013;101:25–38. [Google Scholar]
- Gormley WT, Gayer T. Promoting school readiness in Oklahoma: An evaluation of Tulsa’s pre-k program. Journal of Human Resources. 2005;40:533–558. [Google Scholar]
- Gruber J, Simon K. Crowd-out 10 years later: Have recent public insurance expansions crowded out private health insurance? Journal of Health Economics. 2008;27:201–217. doi: 10.1016/j.jhealeco.2007.11.004. [DOI] [PubMed] [Google Scholar]
- Hankin JR, Sloan JJ, Sokol RJ. The modest impact of the alcohol beverage warning label on drinking during pregnancy among a sample of African-American women. Journal of Public Policy & Marketing. 1998:61–69. [Google Scholar]
- Harding K, Galano J, Martin J, Huntington L, Schellenbach CJ. Healthy Families America effectiveness: A comprehensive review of outcomes. Journal of Prevention & Intervention in the Community. 2007;34:149–179. doi: 10.1300/J005v34n01_08. [DOI] [PubMed] [Google Scholar]
- Harding K, Reid R, Oshana D, Holton J. Report to the David and Lucile Packard Foundation. Prevent Child Abuse America; Chicago: 2004. Initial Results of the HFA Implementation Study. [Google Scholar]
- Heckman J, Masterov D. The productivity argument for investing in young children. Applied Economic Perspectives and Policy. 2007;29 [Google Scholar]
- Heckman JJ, Moon SH, Pinto R, Savelyev PA, Yavitz A. The rate of return to the HighScope Perry Preschool program. Journal of Public Economics. 2010;94:114–128. doi: 10.1016/j.jpubeco.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman J, Rubinstein Y. The importance of noncognitive skills: Lessons from the GED testing program. American Economic Review. 2001:145–149. [Google Scholar]
- Heckman J, Stixrud J, Urzua S. The effects of cognitive and noncognitive abilities on labor market outcomes and social behavior. Journal of Labor Economics. 2006;24:411–482. [Google Scholar]
- Howell EM, Kenney GM. The impact of the Medicaid/CHIP expansions on children a synthesis of the evidence. Medical Care Research and Review. 2012;69:372–396. doi: 10.1177/1077558712437245. [DOI] [PubMed] [Google Scholar]
- Hoynes H, Page M, Stevens AH. Can targeted transfers improve birth outcomes? Evidence from the introduction of the WIC program. Journal of Public Economics. 2011;95:813–827. [Google Scholar]
- Hoynes H, Schanzenbach D, Almond D. Long Run Impacts of Childhood Access to the Safety Net. National Bureau of Economic Research; 2012. (Working Paper 18535). [Google Scholar]
- Hustedt JT, Barnett WS, Jung K, Figueras A. Report. National Institute for Early Education Research, Rutgers University; 2008. Impacts of New Mexico pre-k on children’s school readiness at kindergarten entry: Results from the second year of a growing initiative. [Google Scholar]
- Institute of Medicine and National Research Council. Tech rep. 2014. Considerations in applying benefit-cost analysis to preventive interventions for children, youth, and families. [PubMed] [Google Scholar]
- Isen A, Rossin-Slater M, Walker R. Every breath you take—every dollar you’ll make: The long-term consequences of the clean air act of 1970. National Bureau of Economic Research; 2014. (Working Paper 19858). [Google Scholar]
- Jaddoe W. Hypotheses on the fetal origins of adult diseases: Contributions of epidemiological studies. European Journal of Epidemiology. 2006;21:91–102. doi: 10.1007/s10654-005-5924-5. [DOI] [PubMed] [Google Scholar]
- Johnson RC, Kalil A, Dunifon RE. Employment patterns of less-skilled workers: Links to children’s behavior and academic progress. Demography. 2012;49:747–772. doi: 10.1007/s13524-011-0086-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson R, Schoeni RF. The influence of early-life events on human capital, health status, and labor market outcomes over the life course. The BE Journal of Economic Analysis & Policy. 2011;11 doi: 10.2202/1935-1682.2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joyce T, Gibson D, Colman S. The changing association between prenatal participation in WIC and birth outcomes in New York City. Journal of Policy Analysis and Management. 2005;24:661–685. doi: 10.1002/pam.20131. [DOI] [PubMed] [Google Scholar]
- Joyce T, Racine A, Yunzal-Butler C. Reassessing the WIC effect: Evidence from the pregnancy nutrition surveillance system. Journal of Policy Analysis and Management. 2008;27:277–303. doi: 10.1002/pam.20325. [DOI] [PubMed] [Google Scholar]
- Kelly E. The scourge of Asian flu: in utero exposure to pandemic influenza and the development of a cohort of British children. Journal of Human Resources. 2011;46:669–694. [Google Scholar]
- Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life course epidemiology. Journal of Epidemiology and Community Health. 2003;57:778. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuh D, Shlomo YB. A life course approach to chronic disease epidemiology. Vol. 2. Oxford University Press; 2004. [Google Scholar]
- Lee BJ, Mackey-Bilaver L. Effects of WIC and Food Stamp program participation on child outcomes. Children and Youth Services Review. 2007;29:501–517. [Google Scholar]
- Levine PB, Schanzenbach D. The impact of children’s public health insurance expansions on educational outcomes. Forum for Health Economics and Policy. 2009;12:1. [Google Scholar]
- Lin MJ, Liu E. Does in utero exposure to illness matter? The 1918 influenza epidemic in Taiwan as a natural experiment. Journal of Health Economics. 2014;37:152–163. doi: 10.1016/j.jhealeco.2014.05.004. [DOI] [PubMed] [Google Scholar]
- Lin MJ, Liu JT. Do lower birth weight babies have lower grades? Twin fixed effect and instrumental variable method evidence from Taiwan. Social Science & Medicine. 2009;68(10):1780–1787. doi: 10.1016/j.socscimed.2009.02.031. [DOI] [PubMed] [Google Scholar]
- Liu Q, Skäns ON. The duration of paid parental leave and children’s scholastic performance. The BE Journal of Economic Analysis & Policy. 2010;10 [Google Scholar]
- Ludwig J, Miller D. Does Head Start improve children’s life chances? Evidence from a regression discontinuity design. The Quarterly Journal of Economics. 2007;122:159–208. [Google Scholar]
- Masse LN, Barnett WS. Cost-Effectiveness and Educational Policy. Larchmont, NY: Eye on Education, Inc.; 2002. A benefit-cost analysis of the Abecedarian early childhood intervention; pp. 157–173. [Google Scholar]
- Mathews T. Smoking during pregnancy in the 1990s. Report 7, Division of Vital Statistics. 2001 [PubMed] [Google Scholar]
- McClellan JM, Susser E, King MC. Maternal famine, de novo mutations, and schizophrenia. JAMA. 2006;296:582–584. doi: 10.1001/jama.296.5.582. [DOI] [PubMed] [Google Scholar]
- McCormick MC, Brooks-Gunn J, Buka SL, Goldman J, Yu J, Salganik M, Scott DT, Bennett FC, Kay LL, Bernbaum JC, et al. Early intervention in low birth weight premature infants: Results at 18 years of age for the infant health and development program. Pediatrics. 2006;117:771–780. doi: 10.1542/peds.2005-1316. [DOI] [PubMed] [Google Scholar]
- Meyer BD, Wherry LR. Saving teens: Using a policy discontinuity to estimate the effects of Medicaid eligibility. National Bureau of Economic Research; 2012. (Working Paper 18309). [Google Scholar]
- Miller S, Wherry L. The long-term health effects of early life Medicaid coverage. University of Michigan; 2014. unpublished manuscript. [Google Scholar]
- Mincer J. Schooling, experience, and earnings. National Bureau of Economic Research; 1974. [Google Scholar]
- Moon RY, Calabrese T, Aird L. Reducing the risk of sudden infant death syndrome in child care and changing provider practices: Lessons learned from a demonstration project. Pediatrics. 2008;122:788–798. doi: 10.1542/peds.2007-3010. [DOI] [PubMed] [Google Scholar]
- Moon R, Oden RP, Grady KC. Back to Sleep: An educational intervention with women, infants, and children program clients. Pediatrics. 2004;113:542–547. doi: 10.1542/peds.113.3.542. [DOI] [PubMed] [Google Scholar]
- Mulder E, Robles de Medina P, Huizink A, Van den Bergh B, Buitelaar J, Visser G. Prenatal maternal stress: Effects on pregnancy and the (unborn) child. Early Human Development. 2002;70:3–14. doi: 10.1016/s0378-3782(02)00075-0. [DOI] [PubMed] [Google Scholar]
- Neugebauer R, Hoek HW, Susser E. Prenatal exposure to wartime famine and development of antisocial personality disorder in early adulthood. JAMA. 1999;282:455–462. doi: 10.1001/jama.282.5.455. [DOI] [PubMed] [Google Scholar]
- Nilsson P. Alcohol availability, prenatal conditions, long-term economic out-comes, Institute for International Economic Studies. Stockholm University; 2014. unpublished manuscript. [Google Scholar]
- Office of Planning, Research, and Evaluation. Head Start Impact Study Final Report 2010 [Google Scholar]
- Olds DL. The nurse–family partnership: An evidence-based preventive intervention. Infant Mental Health Journal. 2006;27:5–25. doi: 10.1002/imhj.20077. [DOI] [PubMed] [Google Scholar]
- Oreopoulos P, Stabile M, Walld R, Roos LL. Short-, medium-, and long-term consequences of poor infant health: An analysis using siblings and twins. Journal of Human Resources. 2008;43:88–138. [Google Scholar]
- Page M, Stevens AH, Lindo J. Parental income shocks and outcomes of disadvantaged youth in the United States. In: Gruber J, editor. The Problems of Disadvantaged Youth: An Economic Perspective. University of Chicago Press; 2007. pp. 213–235. [Google Scholar]
- Paneth NS. The problem of low birth weight. The Future of Children. 1995;5:19–34. [PubMed] [Google Scholar]
- Persson P, Rossin-Slater M. Family ruptures and intergenerational tran-mission of stress. Stanford University; 2014. Unpublished Manuscript. [Google Scholar]
- Petronis A. Epigenetics as a unifying principle in the aetiology of complex traits and diseases. Nature. 2010;465:721–727. doi: 10.1038/nature09230. [DOI] [PubMed] [Google Scholar]
- Pitkin RM. Folate and neural tube defects. The American Journal of Clinical Nutrition. 2007;85:285S–288S. doi: 10.1093/ajcn/85.1.285S. [DOI] [PubMed] [Google Scholar]
- Rasinski KA, Kuby A, Bzdusek SA, Silvestri JM, Weese-Mayer DE. Effect of a sudden infant death syndrome risk reduction education program on risk factor compliance and information sources in primarily black urban communities. Pediatrics. 2003;111:e347–e354. doi: 10.1542/peds.111.4.e347. [DOI] [PubMed] [Google Scholar]
- Rau T, Reyes L, Urzua S. The long-term effects of early lead exposure: Evidence from a case of environmental negligence. University of Maryland; 2013. unpublished manuscript. [Google Scholar]
- Reichman NE, Corman H, Noonan K, Schwartz-Soicher O. Effects of prenatal care on maternal postpartum behaviors. Review of Economics of the Household. 2010;8:171–197. doi: 10.1007/s11150-009-9074-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes JW. Environmental policy as social policy? The impact of childhood lead exposure on crime. The BE Journal of Economic Analysis & Policy. 2007;7 [Google Scholar]
- Robinson JJ. Sound body, sound mind? Asymmetric and symmetric fetal growth restriction and human capital development. University of Alabama at Birmingham; 2013. unpublished manuscript. [Google Scholar]
- Rodgers GB. The safety effects of child-resistant packaging for oral prescription drugs: Two decades of experience. JAMA. 1996;275:1661–1665. [PubMed] [Google Scholar]
- Rossin M. The effects of maternity leave on children’s birth and infant health outcomes in the United States. Journal of Health Economics. 2011;30:221–239. doi: 10.1016/j.jhealeco.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossin-Slater M. WIC in your neighborhood: New evidence on the impacts of geographic access to clinics. Journal of Public Economics. 2013;102:51–69. doi: 10.1016/j.jpubeco.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rossin-Slater M, Ruhm CJ, Waldfogel J. The effects of California’s paid family leave program on mothers’ leave-taking and subsequent labor market outcomes. Journal of Policy Analysis and Management. 2013;32:224–245. doi: 10.1002/pam.21676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Royer H. Separated at girth: US twin estimates of the effects of birth weight. American Economic Journal: Applied Economics. 2009;1:49–85. [Google Scholar]
- Ruhm CJ. Parental leave and child health. Journal of Health Economics. 2000;19:931–960. doi: 10.1016/s0167-6296(00)00047-3. [DOI] [PubMed] [Google Scholar]
- Ruhm CJ. Policies to assist parents with young children. The Future of Children. 2011;21:37. doi: 10.1353/foc.2011.0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salm M, Schunk D. The role of childhood health for the intergenerational transmission of human capital: Evidence from administrative data. Institute for the Study of Labor (IZA); 2008. (Discussion Paper 3646). [Google Scholar]
- Sanders NJ. What doesn’t kill you makes you weaker: Prenatal pollution exposure and educational outcomes. Journal of Human Resources. 2012;47:826–850. [Google Scholar]
- Sikorski J, Wilson J, Clement S, Das S, Smeeton N. A randomised controlled trial comparing two schedules of antenatal visits: The antenatal care project. BMJ: British Medical Journal. 1996;312:54. doi: 10.1136/bmj.312.7030.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simon D. Does early life exposure to cigarette smoke permanently harm childhood welfare? Evidence from cigarette tax hikes. University of Connecticut; 2014. unpublished manuscript. [Google Scholar]
- St Pierre RG, Layzer JI. Using home visits for multiple purposes: The Comprehensive Child Development Program. Future of Children. 1999;9:134–151. [PubMed] [Google Scholar]
- Stein AD, Kahn HS, Rundle A, Zybert PA, van der Pal-de Bruin K, Lumey L. Anthropometric measures in middle age after exposure to famine during gestation: Evidence from the Dutch famine. The American Journal of Clinical Nutrition. 2007;85:869–876. doi: 10.1093/ajcn/85.3.869. [DOI] [PubMed] [Google Scholar]
- Stevens AH, Schaller J. Short-run effects of parental job loss on children’s academic achievement. Economics of Education Review. 2011;30:289–299. [Google Scholar]
- Susser E, Neugebauer R, Hoek HW, Brown AS, Lin S, Labovitz D, Gorman JM. Schizophrenia after prenatal famine: Further evidence. Archives of General Psychiatry. 1996;53:25. doi: 10.1001/archpsyc.1996.01830010027005. [DOI] [PubMed] [Google Scholar]
- Tanaka S. Parental leave and child health across OECD countries. The Economic Journal. 2005;115:F7–F28. [Google Scholar]
- Thompson R. Stress and child development. The Future of Children. 2014;24:41–59. doi: 10.1353/foc.2014.0004. [DOI] [PubMed] [Google Scholar]
- Trzcinski E, Alpert WT. Pregnancy and parental leave benefits in the United States and Canada: Judicial decisions and legislation. Journal of Human Resources. 1994;29 [Google Scholar]
- U.S. Department of Health and Human Services. Reducing alcohol-exposed pregnancies, A report of the National Task Force on Fetal Alcohol Syndrome and Fetal Alcohol Effect 2009 [Google Scholar]
- Van Den Berg GJ, Lindeboom M, Portrait F. Economic conditions early in life and individual mortality. The American Economic Review. 2006;96:290–302. doi: 10.1257/000282806776157740. [DOI] [PubMed] [Google Scholar]
- Vinikoor LC, Messer LC, Laraia BA, Kaufman JS. Reliability of variables on the North Carolina birth certificate: A comparison with directly queried values from a cohort study. Paediatric and Perinatal Epidemiology. 2010;24:102–112. doi: 10.1111/j.1365-3016.2009.01087.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webbink D, Vujić S, Koning P, Martin NG. The effect of childhood conduct disorder on human capital. Health Economics. 2012;21:928–945. doi: 10.1002/hec.1767. [DOI] [PubMed] [Google Scholar]
- Wong VC, Cook TD, Barnett WS, Jung K. An effectiveness-based evaluation of five state pre-kindergarten programs. Journal of Policy Analysis and Management. 2008;27:122–154. [Google Scholar]


