Abstract
The term ossifying fibroma (OF) has recently been included under fibro-osseous lesions. Cemento-OF (COF) is a benign neoplasm that arises from the periodontal membrane which contains multipotential cells that are capable of forming cementum, lamellar bone and fibrous tissue. These tumors occur in the third and fourth decades of life with a predilection for women. The mandible is more commonly involved than the maxilla. This lesion has caused considerable controversy regarding the use of terminology, origin and diagnostic criteria. This article describes an unusual case of COF presenting as unilocular lytic lesion of mandible in a 38-year-old male patient with review of literature.
Keywords: Fibro-osseous lesions, mandible, ossifying fibroma
INTRODUCTION
Cemento-ossifying fibromas (COFs) are rare benign, nonodontogenic tumors of the jaw, a subdivision of fibro-osseous lesions characterized by massive deposition of cementum, cementoid substance or calcified material admixed with predominantly fibrous tissue.[1] Branon and Fowler were the first to use the term “OF” in place of COF, and the recent WHO (2005) edition of the classification of odontogenic neoplasms has replaced the term COF with OF.[2,3] As early as 1872, Menzel gave the first description of a variant of OF, calling it a COF, in a 35-year-old woman with long-standing large tumor of the mandible.[4] Radiographically, COF presents as a well-defined unilocular or multilocular lesion with smooth contours. The maturity of the lesion will determine the degree of radiopacity. The immature lesions may present as a complete radiolucent lesion whereas the mature lesion may appear completely radiopaque. However, they can present with varying degrees of radiolucency. Histologically, COFs are well-circumscribed, occasionally encapsulated, consisting of cellular fibrous tissues and thin isolated trabeculae of bones. The bone may show osteoblastic rimming and spherical deposits of calcified material, which are relatively acellular resembling cementum.[5] Fibro-osseous lesions are a heterogeneous group of benign lesions of unknown etiology, affecting the jaws and other craniofacial bones. Lesions in this category include fibrous dysplasia (FD), focal cemento-osseous dysplasia (FCOD) and COF.[2] The group often exhibits resemblance in clinical presentation, radiographic appearance and histological criteria, therefore, poses difficulties in classification, diagnosis and management.[6]
CASE REPORT
A 42-year-old male patient was referred to our hospital with a painless swelling in the right mandible of 6 months duration. Clinically lingual expansion was evident. Skin over the lesion was normal and no regional lymph node enlargement was noted. Intraorally, there was marked bone expansion. Both lingual and buccal cortical plate expansion extending from right lower first premolar to retro-molar region was noticed. On palpation, swelling was smooth, nontender and bony hard in consistency. Mucosa over the lesion was normal. Orthopantomogram [Figure 1] showed expansile lytic lesion in the body of mandible involving the roots of premolars, first and second molars. The lateral aspect of the lesion shows faint sclerosis. Computed tomography (CT) [Figures 2 and 3] showed expansile lytic lesion with patchy sclerosis measuring about 4.2 cm × 3.5 cm (Tr × AP). No unerupted teeth were noted within the lesion. There were no loculations or fluid-levels within the lesion. The central densities within the lesion were of soft tissue density, suggesting solid or fibrous lesion rather than a cystic lesion. The CT diagnosis was that of OF due to patchy sclerosis. No cortical breach was noted in three-dimensional surface shaded display images. The margins of the lesion blended smoothly with rest of the body of mandible.
Figure 1.

Orthopantomogram showing expansile lytic lesion in the body of mandible involving the roots of premolars, first and second molars. The lateral aspect of the lesion shows faint radiopacity
Figure 2.
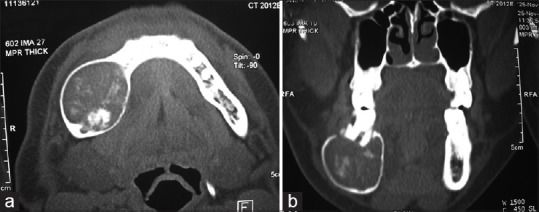
Computed tomography scan (in bone window) axial section (a) and coronal reformation (b) showing the expansile lytic lesion with patchy sclerosis. There are no loculations/fluid- levels or an embedded tooth noted
Figure 3.
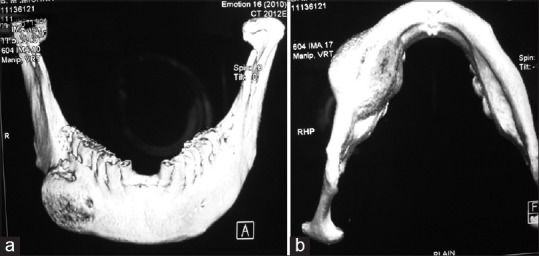
Computed tomography three-dimensional surface shaded display images from frontal (a) and basal (b) view showing the expansile lesion with smooth outlines without any cortical break
The incisional biopsy and surgical enucleation with curettage of lesion [Figure 4] that were done under local anesthesia and sent for histopathological examination, revealed similar findings. Grossly, specimen consisted of multiple irregular mass of pinkish-white tissue largest measuring 3 cm × 2.5 cm. Mass was gritty on cut section with grey-white solid area. Histopathologically, [Figure 5] a mass of highly cellular stroma with calcified areas was evident. The stroma composed of proliferating fibroblasts arranged in various patterns such as storiform and whorls was noted. Calcified areas appeared to be composed of cementum-like substance. No cellular atypia or atypical mitotic activity was noted. The lesion was diagnosed as COF. The patient was reviewed after 2 months of surgery; complete healing had taken place and was asymptomatic on follow-up after 6 months.
Figure 4.
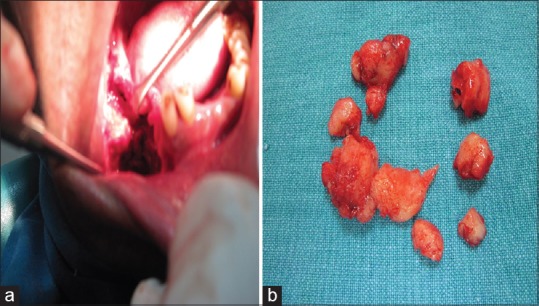
(a) Surgical enucleation with curettage of the lesion of the patient. (b) Enucleated lesion of the patient mentioned in the case report
Figure 5.
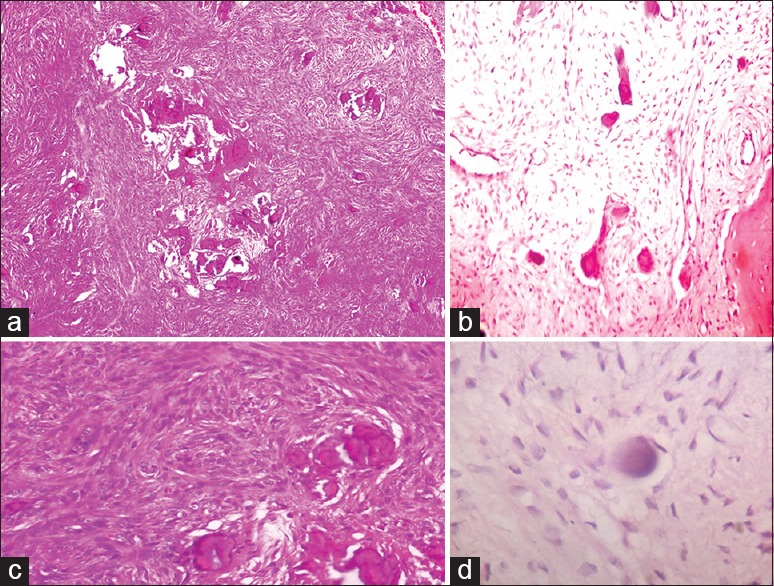
Photomicrograph (a) Showing highly cellular fields with spheroidal cementum-like material (H&E stain, ×40). (b) Photomicrograph showing bony trabeculae rimmed by osteoblast with surrounding loose fibrous tissue (H&E stain, ×100). (c) Photomicrograph showing proliferating fibroblasts arranged in whorls and short fascicles with cementum-like material (H&E stain, ×100). (d) Photomicrograph Showing concentric cementum-like material (H&E stain, ×400)
DISCUSSION
Endless list of terms has been used to describe these benign fibro-osseous neoplasms. Earlier, many investigators classified cementifying fibromas separately from OFs because the former were considered to be of odontogenic origin and the latter osteogenic. It is now agreed that both types fall under the same classification as osteogenic neoplasms based on Eversole et al. classification. Analysis of 64 cases classified as ossifying and/or cementifying fibroma concluded that a distinction between these two variants would be academic as no behavioral or histological differences exist. They suggested that nomenclature could be simplified by referring to all lesions in this group as OF.[7] This entity under WHO classification has undergone revision from time to time. According to 1971 classification, complex group of lesions with cementum-like tissue, neoplastic (benign cementoblastomas, COF) and nonneoplastic lesions (periapical cemental dysplasias, gigantiformcementomas) formed single group. In 1992 WHO modification, benign fibro-osseous lesions in the oral and maxillofacial regions were divided into two categories, osteogenic neoplasm and nonneoplastic bone lesions, thus clearly separating neoplastic from nonneoplastic lesions containing cementum-like tissue. Cementifying OF belonged to the former category. During the 2003 consensus conference held in conjunction with the preparation of new WHO volume Tumors of the Head and Neck, some changes were made. Osseous neoplasm and nonneoplastic lesions were categorized under the section “Neoplasms and other lesions occurring in the maxillofacial skeleton”. Under this section, COF was included in neoplastic lesions and was designated as OF. Nonneoplastic lesions comprised FD, osseous dysplasias, central giant cell lesion/granuloma, cherubism, aneurysmal bone cyst and simple bone cyst.[8] These lesions are slow-growing and are most often seen in women between the third and fourth decades of life and more common in mandible than maxilla, typically inferior to the premolars and molars.[7,9] MacDonald-Jankowski did a systematic review of 64 reports and found that 84% of cases displayed bucco-lingual expansion. Half of the mandibular cases exhibited downward displacement of the lower border of the mandible and 90% of maxillary cases involved the maxillary antrum.[2] In the present case also, the growth was slow and was located in mandible, occurred in fourth decade but in a male patient and showed bucco-lingual expansion as well as downward displacement of the lower border of the mandible. The central OF is used when there is spectrum of lesions that arise from the periodontal ligament, ranging from those with only deposition of cementum to those with only deposition of bone. When this tumor arises in children, it is called as the aggressive COF which is more aggressive clinically and more vascular at pathologic examination.[10] The lesions arising from periodontal ligament and located in the gingiva are termed peripheral COF.[11] The recommended treatment of the central COF is excision. Due to the good delimitation of the tumor, surgical removal and curettage is also a treatment of choice.[12] Liu et al. observed that the time of recurrence was always unpredictable, ranging from 6 months to 7 years after the operation. Hence, long-term follow-up of such cases is advisable.[13] However, recurrent peripheral COF has been reported in literature 15 months after surgery.[14]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.White SC, Pharoah MJ. Oral Radiology. 6th ed. China: Mosby Co; 2009. pp. 440–1. [Google Scholar]
- 2.MacDonald-Jankowski DS. Ossifying fibroma: A systematic review. Dentomaxillofac Radiol. 2009;38:495–513. doi: 10.1259/dmfr/70933621. [DOI] [PubMed] [Google Scholar]
- 3.Reichart PA, Philipsen HP, Sciubba JJ. The new classification of head and neck tumours (WHO) – Any changes? Oral Oncol. 2006;42:757–8. doi: 10.1016/j.oraloncology.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 4.Hamner JE, 3rd, Scofield HH, Cornyn J. Benign fibro-osseous jaw lesions of periodontal membrane origin. An analysis of 249 cases. Cancer. 1968;22:861–78. doi: 10.1002/1097-0142(196810)22:4<861::aid-cncr2820220425>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 5.Soames JV, Southam JC. Oral Pathology. 4th ed. New Delhi: Oxford University Press; 2005. Disorders of bone; pp. 241–61. [Google Scholar]
- 6.Ong AH, Siar CH. Cemento-ossifying fibroma with mandibular fracture. Case report in a young patient. Aust Dent J. 1998;43:229–33. doi: 10.1111/j.1834-7819.1998.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 7.Eversole LR, Leider AS, Nelson K. Ossifying fibroma: A clinico pathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985;60:505–11. doi: 10.1016/0030-4220(85)90239-7. [DOI] [PubMed] [Google Scholar]
- 8.Khan SA, Sharma NK, Raj V, Sethi T. Ossifying fibroma of maxilla in a male child: Report of a case and review of the literature. Natl J Maxillofac Surg. 2011;2:73–9. doi: 10.4103/0975-5950.85859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ram R, Singhal A, Singhal P. Cemento-ossifying fibroma. Contemp Clin Dent. 2012;3:83–5. doi: 10.4103/0976-237X.94553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tamiolakis DE, Thomaidis VA, Tsamis IO. Cemento-ossifying fibroma of the maxilla: A case report. Acta Stomatol Croat. 2005;39:319–21. [Google Scholar]
- 11.Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H. Peripheral cemento-ossifying fibroma: A case report with review of literature. World J Clin Cases. 2013;1:128–33. doi: 10.12998/wjcc.v1.i3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rangil JS, Silvestre FJ, Bernal JR. Cemento-ossifying fibroma of the mandible: Presentation of a case and review of the literature. J Clin Exp Dent. 2011;3:66–9. [Google Scholar]
- 13.Liu Y, Wang H, You M, Yang Z, Miao J, Shimizutani K, et al. Ossifying fibromas of the jaw bone: 20 cases. Dentomaxillofac Radiol. 2010;39:57–63. doi: 10.1259/dmfr/96330046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pereira T, Shetty S, Shetty A, Pereira S. Recurrent peripheral cemento-ossifying fibroma. J Indian Soc Periodontol. 2015;19:333–5. doi: 10.4103/0972-124X.152410. [DOI] [PMC free article] [PubMed] [Google Scholar]


