Abstract
Congenital epulis, a benign tumor of the oral cavity, is an extremely rare condition in newborn. It may lead to mechanical obstruction, therefore resulting in respiratory distress and difficulty in feeding. Addressing the problem may need a multidisciplinary team approach at the time of birth. Antenatal ultrasonography and perinatal magnetic resonance imaging are an adjunct to treatment planning. Prenatal diagnosis remains difficult as the findings are nonspecific due to the late development of the tumor. Surgical excision is, therefore, the treatment of choice. Our report discusses this condition and the treatment thereafter on a newborn, with an epulis originating from the upper alveolar ridge discovered at birth. Histological examination confirmed the diagnosis of large polygonal granular cells. The mass was excised under general anesthesia, and the outcome was good after surgery allowing regular feeds on the second postoperative day.
Keywords: Congenital epulis, granular cells, new born
INTRODUCTION
Congenital oral tumors in the mouth of the newborn are rare.[1] They are also referred as congenital granular cell tumor, congenital granular epulis, congenital granular cell myoblastoma and congenital granular cell fibroblastoma.[2,3] Although these lesions are benign, they need immediate surgical intervention because they cause interference in feeding and have the potential to cause the death of the child from asphyxia during the perinatal and postnatal period.[3] The most common site is the alveolar ridges of maxilla and mandible with a marked predilection of occurrence in females. The lesion is 3 times more frequently seen in maxilla than in mandible and the female: male ratio is 10:1.[4] The incidence rates were found to be 0.0006% at a center in wales[5] and epulis accounted for 10.8% of all the oral lesions in a center in India.[6] Mostly, they are solitary but, in some cases, large and multiple tumors are shown. Addressing the problem may need a multidisciplinary team approach at the time of birth; herein, we report a case of bilobed congenital epulis of the newborn arising from the maxillary alveolar ridge.
CASE REPORT
A 3-day-old female full-term infant weighing 2.45 kg at birth was admitted with complaints of a mass in the oral cavity measuring about 4.3 cm × 3.2 cm. Clinical examination of the newborn revealed the presence of a pink, bilobed, pedunculated, nontender smooth surfaced mass with a firm consistency arising from the right side of the maxillary alveolar ridge [Figure 1]. Respiratory distress was not evident, but the child had sucking problems. In discussion with the pediatrician and anesthetist, surgical excision was planned under general anesthesia. After preoperative evaluation, surgical excision of the mass was done by the use of cautery after orotracheal intubation under general anesthesia [Figure 2] on the 5th day of life without any complications. The examination of the resected specimen showed a bilobular, encapsulated, smooth mass which was pedunculated. On histological examination, the tissue was seen to be composed of sheets of large polygonal granular cells with distinct borders, having abundant granular eosinophilic cytoplasm and predominantly eccentrically located vesicular nuclei with conspicuous nucleoli [Figures 3 and 4]. Infant was able to commence feeding on the second postoperative day and was discharged on his 8th day of life with normal closure of the mouth and was able to suck normally. The postoperative period was uneventful with infant not showing any signs of recurrence after 4 months of follow-up.
Figure 1.

Tumor mass attached to the alveolar ridge of maxilla
Figure 2.

Postoperative clinical image demonstrating the site of the wound.
Figure 3.
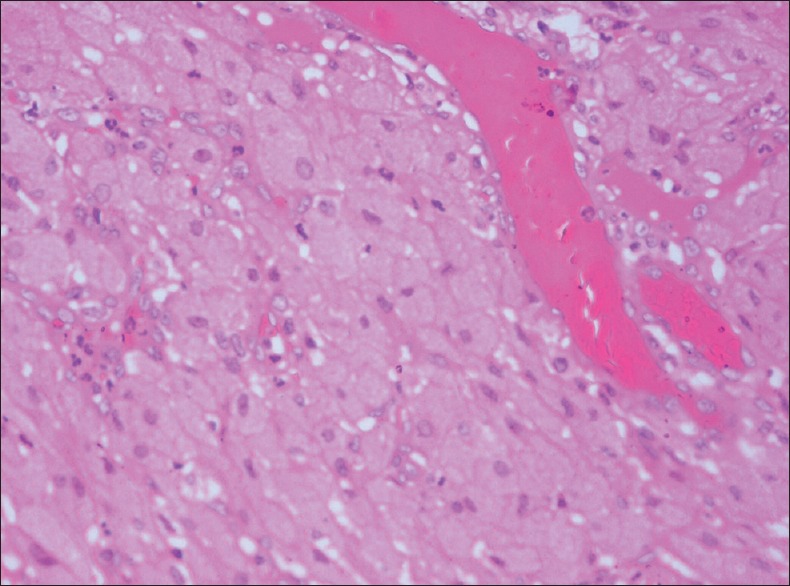
Microscopic examination of excised specimen revealing polygonal cells with granular cytoplasm (H&E stain, x100)
Figure 4.
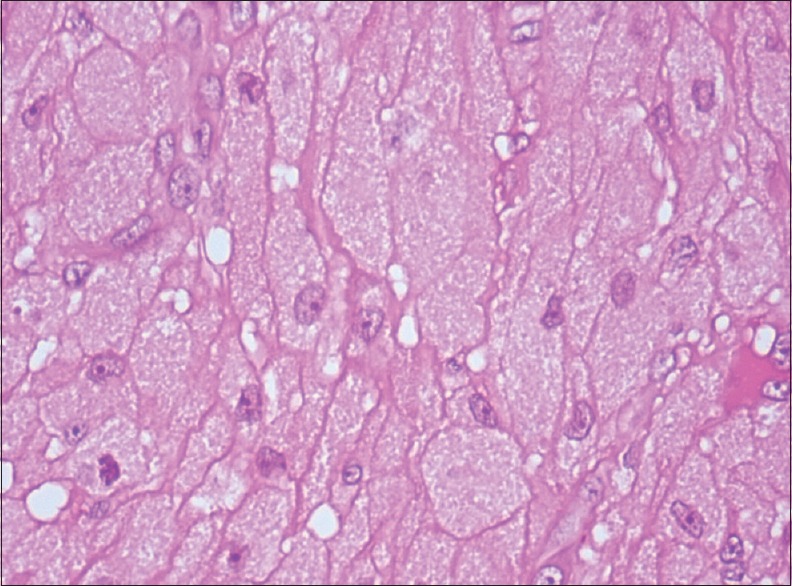
Microscopic examination of excised specimen demonstrating polygonal cells with granular cytoplasm and vesiculated nuclei (H&E stain, x400)
DISCUSSION
Congenital epulis also known as congenital granular cell tumor, congenital granular epulis, congenital granular cell myoblastoma and congenital granular cell fibroblastoma is a very rare condition among newborn and is predominant in females.[3,7,8] The tumor is benign with no clear etiology but is reported to be hormone-related although other theories do exist.[9] The female predominance argues in favor of the endocrine theory.[10] Histological and electron microscope studies suggest a reactive theory in which the tumor results from stromal gingival cells such as fibroblasts or histiocytes. The cases of spontaneous regression in the literature and the absence of recurrence after incomplete tumor resection support this theory.[11]
They are mostly recognized at birth or just after birth except in cases where the size is very small and, therefore, absence of symptoms. Prenatal diagnosis remains difficult because of the absence of specific signs and also as the tumor generally develops beyond the 22nd week of gestation.[12] Fetal three-dimensional ultrasound and magnetic resonance imaging (MRI) can provide the diagnosis by the 36th week of gestation, thereby helping to decide and plan in advance an early multidisciplinary management of the newborn with participation from the neonatologist, the maxillofacial or head and neck surgeon or the pediatric surgeon and the anesthesiologist.[12]
Classically, there is a single firm tumor with a quite regular surface, sometimes multilobed, sessile or pedenculated, pink or red in color and nonpainful on palpation. The tumor size varies from a few millimeters to around 10 cm at its widest diameter.[13] The maxillary location opposite the future canines or incisors is the most frequent, but the mandibular region can also be involved. Multiple lesions or maxillary and mandibular locations have been described in 5–16% of the cases.[12,14]
Although benign, immediate surgical intervention is required because of risk to patient's life due to asphyxia. Some other common clinical manifestations include dyspnea, cyanosis, cough, difficulty in sucking and swallowing and occasionally, vomiting.[15]
Perinatal MRI of the oral cavity helps in differentiating congenital epulis from other masses of oral cavity and in determining characteristics of the mass. It is, therefore, a recommended procedure for surgical planning.[16,17] Literature shows no evidence of surgical excision affecting the growth of the bone or the eruption of teeth.[18] Surgery can be performed under local or general anesthesia and the choice between the two depends on the size, number and location. Authors have shown preference for general anesthesia when tumor size is large or is present at multiple locations.[10,11] With single and sessile tumor local anesthesia is preferred.[13]
In our case, we performed the excision under general anesthesia because of large and pedunculated size of tumor. Histological examination confirmed the lesion to be consistent with a congenital granular cell tumor. Histological examination of the tumor specimen demonstrated large polygonal granular cells with distinct borders, having abundant granular eosinophilic cytoplasm and predominantly eccentrically located vesicular nuclei with conspicuous nucleoli.
CONCLUSION
Congenital epulis may regress spontaneously but requires surgical removal due to problems in feeding and respiration. It often recurs after surgical removal. It is important that General Dentists and Pediatricians recognize this lesion and give relevant information regarding the treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chattopadhyay A, Patra R, Kumar V. Oral tumors in newborn. Indian J Pediatr. 2003;70:587–8. doi: 10.1007/BF02723164. [DOI] [PubMed] [Google Scholar]
- 2.Costas JB, Di Piramo S. Congenital epulis (congenital granular-cell myoblastoma). Report of two cases. Oral Surg Oral Med Oral Pathol. 1968;26:497–504. doi: 10.1016/0030-4220(68)90330-7. [DOI] [PubMed] [Google Scholar]
- 3.Bhaskar SN, Akamine R. Congenital epulis (congenital granular cell fibroblastoma); report of a case. Oral Surg Oral Med Oral Pathol. 1955;8:517–23. doi: 10.1016/0030-4220(55)90083-9. [DOI] [PubMed] [Google Scholar]
- 4.Tatli U, Abayli C, Kisa HI, Uguz HA. Congenital granular cell epulis: A case report of an unexpected feature with histopathological and immunohistochemical examination. J Cranio Maxillary Dis. 2014;3:51–5. [Google Scholar]
- 5.Bosanquet D, Roblin G. Congenital epulis: A case report and estimation of incidence. Int J Otolaryngol 2009. 2009 doi: 10.1155/2009/508780. 508780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Modi D, Laishram RS, Sharma LD, Debnath K. Pattern of oral cavity lesions in a tertiary care hospital in Manipur, India. J Med Soc. 2013;27:199–202. [Google Scholar]
- 7.Lapid O, Shaco-Levy R, Krieger Y, Kachko L, Sagi A. Congenital epulis. Pediatrics. 2001;107:E22. doi: 10.1542/peds.107.2.e22. [DOI] [PubMed] [Google Scholar]
- 8.Zuker RM, Buenechea R. Congenital epulis: Review of the literature and case report. J Oral Maxillofac Surg. 1993;51:1040–3. doi: 10.1016/s0278-2391(10)80053-9. [DOI] [PubMed] [Google Scholar]
- 9.Lack EE, Perez-Atayde AR, McGill TJ, Vawter GF. Gingival granular cell tumor of the newborn (congenital “epulis”): Ultrastructural observations relating to histogenesis. Hum Pathol. 1982;13:686–9. doi: 10.1016/s0046-8177(82)80018-x. [DOI] [PubMed] [Google Scholar]
- 10.Bilen BT, Alaybeyoglu N, Arslan A, Türkmen E, Aslan S, Celik M. Obstructive congenital gingival granular cell tumour. Int J Pediatr Otorhinolaryngol. 2004;68:1567–71. doi: 10.1016/j.ijporl.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 11.Williams RW, Grave B, Stewart M, Heggie AA. Prenatal and postnatal management of congenital granular cell tumours: A case report. Br J Oral Maxillofac Surg. 2009;47:56–8. doi: 10.1016/j.bjoms.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 12.Messina M, Severi FM, Buonocore G, Molinaro F, Amato G, Petraglia F. Prenatal diagnosis and multidisciplinary approach to the congenital gingival granular cell tumor. J Pediatr Surg. 2006;41:E35–8. doi: 10.1016/j.jpedsurg.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 13.Song WS, Kim JW, Kim YG, Ryu DM. A case report of congenital epulis in the fetus. J Oral Maxillofac Surg. 2005;63:135–7. doi: 10.1016/j.joms.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 14.Charrier JB, Droullé P, Vignaud JM, Chassagne JF, Stricker M. Obstructive congenital gingival granular cell tumor. Ann Otol Rhinol Laryngol. 2003;112:388–91. doi: 10.1177/000348940311200417. [DOI] [PubMed] [Google Scholar]
- 15.Maeda K, Yamamoto T, Yoshimura H, Itoh H. Epignathus: A report of two neonatal cases. J Pediatr Surg. 1989;24:395–7. doi: 10.1016/s0022-3468(89)80279-9. [DOI] [PubMed] [Google Scholar]
- 16.Roy S, Sinsky A, Williams B, Desilets V, Patenaude YG. Congenital epulis: Prenatal imaging with MRI and ultrasound. Pediatr Radiol. 2003;33:800–3. doi: 10.1007/s00247-003-1024-4. [DOI] [PubMed] [Google Scholar]
- 17.Kim YD, Kim HJ, Lee NK, Ha WH, Lee CH, Park SE. Congenital epulis: Prenatal ultrasonographic and postnatal MR features with pathologic correlation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:743–8. doi: 10.1016/j.tripleo.2007.12.018. [DOI] [PubMed] [Google Scholar]
- 18.Loyola AM, Gatti AF, Pinto DS, Jr, Mesquita RA. Alveolar and extra-alveolar granular cell lesions of the newborn: Report of case and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:668–71. doi: 10.1016/s1079-2104(97)90370-x. [DOI] [PubMed] [Google Scholar]


