Abstract
Catastrophizing is associated with negative outcomes in chronic pain and illness. The Communal Coping Model (CCM) and cognitive-behavioral (CB) formulations provide differing accounts of the function of catastrophizing in these contexts. The present study examined predictions from CCM and CB theoretical models in a sample of 116 patients with chronic fatigue to test: (1) whether patient-reported solicitous responses from significant others mediate the relationship of catastrophizing with patient-reported pain and fatigue behaviors, as predicted by the CCM, and (2) whether pain and fatigue behaviors mediate the relationship of catastrophizing with solicitous responses, consistent with a CB model. This work is a secondary data analysis that examined the strength of the indirect (i.e., mediating) effects among study variables. Consistent with CB models, pain and fatigue behaviors were associated with both catastrophizing and solicitous responses, and there was a significant indirect effect of catastrophizing on solicitous responses through pain and fatigue behaviors. Results were inconsistent with the CCM; catastrophizing was not significantly associated with solicitous responses, nor did solicitous responses mediate the relationship between catastrophizing and pain/fatigue behaviors. Findings highlight the importance of behavioral expressions of pain and fatigue in understanding the relationship of catastrophizing to solicitous responses in chronic fatigue.
Keywords: Catastrophizing, chronic fatigue, solicitousness, partner responses, pain and fatigue behavior
Introduction
Catastrophizing, defined as an exaggerated negative mental set,[44](p. 53) has been consistently associated with negative outcomes in chronic pain and illness.[12; 34; 40; 44] However, an understanding of why people catastrophize has proven elusive, despite the apparent negative effects of this cognitive style. The Communal Coping Model (CCM)[42] and cognitive-behavioral (CB) formulations provide differing accounts of the potential function of catastrophizing in the context of chronic pain and illness.
The CCM proposes that patients who prefer to deal with stress in an interpersonal manner will catastrophize as a strategy to elicit social support.[42] In this theoretical model, catastrophizing would be associated with perceived support, and associations between catastrophizing and pain behavior would be mediated by perceptions of available support, such as solicitousness by significant others (SO). Consistent with the CCM, a number of studies have reported positive associations between catastrophizing and solicitous SO responses.[7; 17; 32] However, this association is not always found,[5] and some research indicates that the role of catastrophizing in SO responses might depend on factors such as belief in entitlement to support.[8] To our knowledge, no study to date has directly examined whether SO responses perceived as solicitous mediate the association between catastrophizing and pain behavior.
Instead of positing that catastrophizing stems from a preference for interpersonal approaches to coping, CB models posit that people catastrophize when they appraise a stressor as posing a threat that exceeds their coping capacity. Catastrophizing, in turn, may lead to greater distress and higher levels of pain or illness behaviors, which then elicit support (such as solicitous responses) from others.[22; 23; 42–44] CB theory would also posit that higher levels of pain and illness behaviors would be elicited in the presence of reinforcing social responses to pain and illness behaviors.[14; 37; 39] Nonetheless, the hypothesis that pain behavior mediates the association between catastrophizing and solicitous responses requires further examination.
The social context of pain and illness behaviors has also been investigated in patients with cancer[17] and chronic fatigue (CF).[35; 38] There appear to be important parallels and overlaps between CF and chronic pain, and psychosocial factors may play an important role in adjustment and functioning in both conditions.[1; 6; 9; 13] Lukkahatai and Saligan[26] noted that a significant association between catastrophizing and fatigue was found in patients with cancer, chronic fatigue syndrome (CFS), multiple sclerosis, and fibromyalgia. Catastrophizing has also been related to worse functional disability in patients with CF.[33] Despite these parallels and findings, the extent to which the CCM and CB models can elucidate the role of catastrophizing in the context of chronic fatigue has not yet been examined.
Given these considerations, we tested predictions derived from two theoretical models, (CCM and CB) in a sample of patients with CF. We assessed two study questions: (1) whether perceived solicitous responses mediate the relationship of catastrophizing to self-reported pain and fatigue behaviors, as predicted by the CCM; and (2) whether self-reported pain and fatigue behaviors mediate the relationship of catastrophizing to perceived solicitous responses, as predicted by a CB model.
Methods
Participants
Participants in the current study were originally recruited for an investigation of illness behaviors and their relationship to partner responses.[35] The current study represents a secondary data analysis of this sample. Readers are referred to Romano and colleagues [35] for a detailed description of the original recruitment procedures. Briefly, in that study 117 participants were recruited from patients aged 18–70 years who were evaluated at a referral clinic for CF and met the case definition for CFS (n=111) or idiopathic CF (n=6) established by the Centers for Disease Control and Prevention.[16] For CFS, the case definition includes new, persistent, or relapsing fatigue lasting six months or more; significant fatigue-related functional impairment; body mass index (BMI) of 45 or less; and endorsement of four out of eight minor criteria (cognitive problems, sore throat, lymphadenopathy, myalgia, arthralgia, new headaches, unrefreshing sleep, and prolonged post-exertional fatigue).[16] For idiopathic CF, the case definition includes new, persistent, or relapsing fatigue lasting six months or more; significant functional impairment; body mass index (BMI) of 45 or less; and fewer than four of the eight minor criteria listed above. As previously described,[35] participants were asked to identify the SO who knew them best (the spouse or partner if in a coupled relationship, or the person closest to them if not) and to answer questions regarding SO responses with that person in mind. One participant was eliminated from the current study for non-completion of one measure used in the data analyses, leaving a final sample of 116 (111 CFS; 5 CF),
The final sample was predominantly female (108 of 116 participants; 93%). Racial identity was self-described as American Indian/Alaska Native (2%); Black/African American (1%); multiracial (1%); and White (96%). The average age was 44.34 years (SD = 10.56). Most participants were married or living with a partner (71%). Slightly more than one-third were currently employed (17% full time, 21% part time) and 21% were receiving disability payments.
Questionnaire Measures
Pain intensity
Average pain intensity over the previous two weeks, ranging from 0 (no pain) to 10 (pain as intense as it could be), was assessed by using an 11-point scale. Such numeric ratings of pain intensity have shown good validity relative to other pain intensity measures and sensitivity to changes in pain after treatment.[21]
Fatigue severity
Fatigue at the time of evaluation was measured by using the fatigue severity rating from the Multidimensional Assessment of Fatigue,[4; 55] which is elicited by a single item: “How severe is the fatigue you are experiencing right now?” Responses range from 1 (mild) to 10 (severe).
Pain and fatigue behaviors
A modified form of the Pain Behavior Checklist (PBC)[24; 50] was used to assess pain and fatigue behaviors. The PBC consists of 17 items that assess pain behavior in four categories: distorted ambulation, facial or audible expressions, affective distress, and help-seeking, and has demonstrated good reliability and validity.[24; 36; 50] We modified the PBC by adding the word “fatigue” to items that mentioned pain. For example, an item that asked about taking medication for pain was altered to include medication “for fatigue or pain.” This modification affected three items: taking medication, asking for help when in fatigue or pain, and talking about fatigue or pain. Participants were directed to complete the measure with regard to pain and fatigue.
Significant other responses
The Multidimensional Pain Inventory (MPI)[25] Spouse Response scale measures common SO responses (solicitous, punishing, and distracting) to patient pain behaviors. As in a previous study,[38] the instructions for the original version were modified to ask participants to describe the reactions of their SOs in response to the participants’ “CFS-related symptoms (pain, fatigue, weakness).” Participants reported the responses of their SOs, and SOs rated their own responses to participants’ pain and fatigue behaviors.
Catastrophizing
The Pain Catastrophizing Scale (PCS)[45] measures dimensions of catastrophic thinking, including rumination, magnification, and helplessness. For study purposes, participants were directed to complete the measure with regard to their symptoms of CFS or CF, including pain, fatigue, and weakness.
Data Analyses
Two three-variable path models were identified to evaluate the two study questions (see Figures 1 and 2), and were tested via path analysis. Path analysis is a special application of structural equation modeling (SEM) that explores the magnitude and significance of hypothesized causal paths in a defined network of observed variables. Path analysis may be seen as an extension of multiple regression, in that it provides standardized estimates of the strength of hypothesized relationships. SEM approaches such as path analysis provide several advantages over traditional regression for testing mediational models.[20] Perhaps most importantly, path analysis allows for simultaneous testing of all direct and indirect paths in the model, as opposed to testing these in a series of separate regression equations.[18; 28] Mediation using traditional multiple regression approaches (e.g.,[3]) may also be underpowered in certain circumstances.[15] In the present study, path analysis was conducted using MPlus 6 software[31], which relies on full information maximum likelihood estimation. Because any model containing three observed variables and three identified pathways has zero degrees of freedom (often described as a “saturated” model), traditional goodness-of-fit statistics could not be generated. However, the conceptual adequacy of each model was established by examining the direct and indirect (i.e., mediating) effects among key variables. Significance of indirect (mediated) effects was established using the multivariate delta method,[28; 30] a test of product coefficients that is the default in the MPlus software package[31] and which in our model is mathematically similar to the Sobel test.[41]
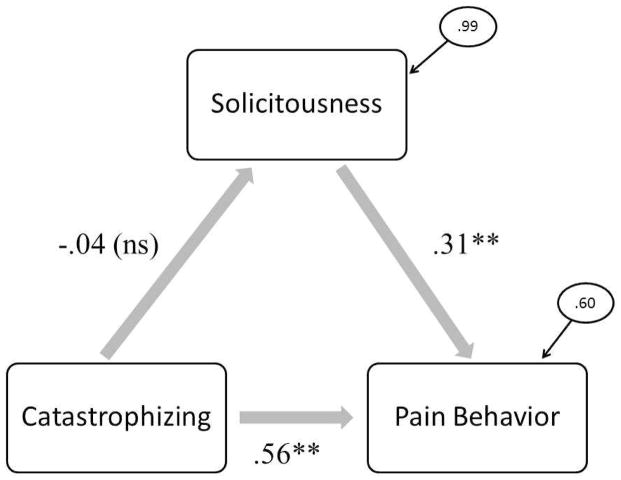
Figure 1.
Communal Coping Model of pain and fatigue behavior, solicitousness, and catastrophizing.
Indirect effect of catastrophizing on pain/fatigue behavior through solicitousness = −.02 (ns).
Standardized residual variances are shown in ovals.
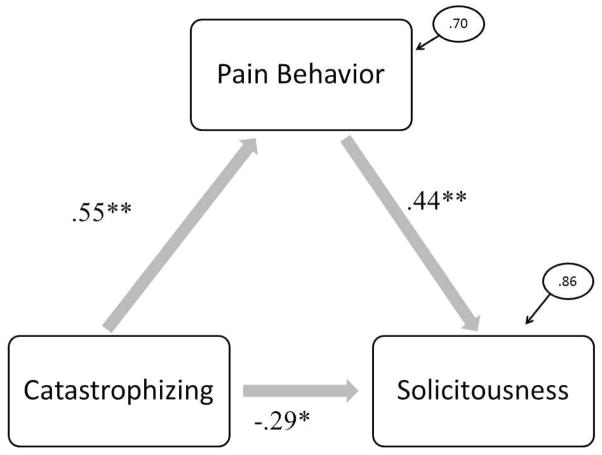
Figure 2.
Cognitive-behavioral model of pain and fatigue behavior, solicitousness, and catastrophizing
Indirect effect of catastrophizing on solicitousness through pain/fatigue behavior = .24 (p<.001)
Standardized residual variances are shown in ovals.
Results
Missing Data and Sample Selection
Before analyses, key variables were tested for the presence of missing data. We identified a small number of missing responses: on the PCS, 6 participants omitted 1 item and 1 participant omitted 2 items; on the PBCL, 4 participants omitted 1 item and 1 participant omitted 3 items; and on the MPI, 4 participants omitted 1 item. For these individuals, a mean score based on their responses to other items in the relevant scale was imputed. As noted previously, one individual from the original study [35] did not answer any items for a single scale (the MPI Solicitous subscale), and thus was not included in the current study sample or analyses.
Psychometric Qualities of Study Variables
The total PCS score, the MPI solicitousness scale, and the total PBC score were all normally distributed, showing kurtosis values below 0.16 and skew below 1.00. No single score on any scale was more than three standard deviations from the mean All three adapted scales demonstrated adequate to excellent internal consistency in the present sample (Cronbach’s α: PCS = .86, MPI = .81, PCS = .94; n = 116).
Descriptive Statistics
Mean scores, standard deviations, and correlations of the primary study measures are presented in Table 1. Pain and fatigue severity are included for descriptive purposes. Of note, the average pain score over the past two weeks was 5.2 (on a 0–10 scale); only one individual indicated no pain in the past two weeks, and an additional 16 individuals (14%) reported only mild pain (i.e., a pain level averaging below 3 in the past 2 weeks), with 86% of the sample reporting average pain levels of 3 or above. As shown in Table 1, all study variables are correlated at statistically significant levels, except for the relationship of solicitous responses with pain intensity, fatigue severity, and catastrophizing.
Table 1.
Correlations, means (M), and standard deviations (SD) of key study variables.
| 1. | 2. | 3. | 4. | 5. | M (SD) | |
|---|---|---|---|---|---|---|
| 1. Pain Intensity | -- | .31** | .40** | .12 | .26** | 5.2 (2.2) |
| 2. Fatigue Severity | -- | .33** | .14 | .21* | 6.8 (2.0) | |
| 3. Pain/Fatigue Behavior (PBCL) | -- | .30** | .55** | 36.2 (17.0) | ||
| 4. Solicitousness (MPI) | -- | −.04 | 2.9 (1.4) | |||
| 5. Catastrophizing (PCS) | -- | 18.6 (11.6) |
p < .05;
p < .01
PBCL= Pain Behavior Checklist; MPI= Multidimensional Pain Inventory; PCS=Pain Catastrophizing Scale
Path Analysis
To evaluate study hypotheses regarding mediation, we tested the significance of the indirect effect in two models. Table 2 lists path coefficients, standard errors, and significance testing values for all parameters in the models.
Table 2.
Standardized parameter estimates for path analytic models.
| Model 1 (CCM) n = 116 | Standardized Coefficient | Standard Error (S.E.) | Est./S.E. | p |
|---|---|---|---|---|
| Catastrophizing → Solicitousness | −.04 | .09 | −.48 | .63 |
| Solicitousness → Pain/Fatigue Behavior | .31 | .07 | 4.4 | <.001 |
| Catastrophizing → Pain/Fatigue Behavior | .56 | .06 | 9.2 | <.001 |
| Catastrophizing → Solicitousness → Pain/Fatigue Behavior (indirect effect) | −.01 | .03 | −.47 | .64 |
| Model 2 (CB) n = 116 | Standardized Coefficient | Standard Error (S.E.) | Est./S.E. | p |
|---|---|---|---|---|
| Catastrophizing → Pain/Fatigue Behavior | .55 | .06 | 8.5 | <.001 |
| Pain/Fatigue Behavior → Solicitousness | .44 | .10 | 4.6 | <.001 |
| Catastrophizing → Solicitousness | −.29 | .10 | −2.8 | <.01 |
| Catastrophizing → Pain/Fatigue Behavior → Solicitousness (indirect effect) | .24 | .06 | 3.8 | <.001 |
First, we tested the path model derived from the CCM in which there would be a hypothesized indirect effect from catastrophizing and pain and fatigue behaviors, through perceived solicitousness. Results showed a significant direct effect of catastrophizing on pain and fatigue behaviors (.56; p <.01), as well as a significant effect of perceived solicitousness on these behaviors (.31; p <.01). However, we found no significant relationship between catastrophizing and perceived solicitousness, and therefore no significant indirect effect of catastrophizing on pain and fatigue behavior through mediation by solicitousness (−0.02), which was inconsistent with predictions based on the CCM. The analytical model for the CCM and relevant data appear in Figure 1.
Next, we evaluated the CB model in which catastrophizing was related to perceived solicitousness through its effects on pain and fatigue behaviors. Results showed direct effects of catastrophizing on solicitousness (−.29; p <.01), of catastrophizing on pain and fatigue behaviors (.55; p <.01), and of pain and fatigue behaviors on solicitousness (.44; p <.01). The indirect effect of catastrophizing on solicitousness through pain and fatigue behaviors was significant (.24; p < .01). These findings are consistent with CB predictions that catastrophizing would be associated with solicitous responding through its effects on pain and fatigue behavior. The CB analytical model appears in Figure 2.
Discussion
This study examined a sample of patients with CFS or CF to evaluate predictions based on the CCM and CB models regarding the interrelationships of catastrophizing, reported pain and fatigue behaviors, and patient perceptions of solicitous SO responses. Consistent with the CB model, we found significant associations of pain and fatigue behaviors with catastrophizing, as well as between these behaviors and patient-reported solicitous responses. However, we did not find significant relationships between solicitous responses and catastrophizing, contrary to expectations based on the CCM. Path analyses further explored these interrelationships, revealing a significant path from catastrophizing to solicitous responses through pain and fatigue behaviors, again consistent with a CB model. However, the hypothesis that there would be an indirect effect of catastrophizing on pain and fatigue behaviors through solicitous responses – as expected in the CCM – was not supported.
These findings underscore the importance of the role of behavioral expressions of pain, illness or distress in understanding the relationships of within-person processes (e.g., catastrophizing) to social contextual factors (e.g., significant others’ responses). Recent research [49] suggested a refinement to the CCM that would include a direct path from pain intensity to pain behavior. Findings from the current study underscore the need for a more explicit differentiation of catastrophizing, understood as a patient’s “mental set” or appraisal process, from overt behavior. Thorn and colleagues[47; 48] noted this distinction and proposed a model that differentiates catastrophizing thoughts from catastrophizing behaviors.[48] However, not all studies of the relationship between catastrophizing and social processes have explicitly incorporated this distinction or included measures of pain, illness, or distress behaviors. Future studies should investigate whether there are specific behavioral indicators associated with catastrophizing that are distinct from behavioral indicators of pain, illness, or distress.
This study could not address the central hypothesis of the CCM that a preference for communal coping drives the catastrophizing process. Both CCM and CB models predict that the presence of solicitous others can cue expressions of pain or distress, and that catastrophizing can mediate the relationship between pain and pain behaviors. However, in the absence of unambiguous evidence that catastrophizing represents a preference for communal coping, further work should assess whether the CCM offers unique explanatory power, or whether existing theoretical models, such as CB approaches, can provide a more parsimonious explanation for these relationships.[39] Future studies are also needed to establish whether subgroups of patients exhibit patterns of catastrophizing, appraisal, or social contextual factors that are more consistent with CCM, CB, or other theoretical models.
Findings from the CB model also suggest the complexity of the relationships among these variables. The relationship between catastrophizing and solicitousness was not significant until pain/fatigue behavior was included in the model. This suggests that pain/fatigue behavior may function as a “suppressor” variable in this context. Suppressors (i.e., variables that, by their inclusion, increase the strength of a relationship between other variables) can be present in the mediational context.[29] Suppression was also suggested by the fact that the indirect and direct effects in the CB model were of opposite signs,[51] in a phenomenon sometimes referred to as “inconsistent mediation”.[11] In this situation the total effect (sum of the direct and indirect effects) may be attenuated despite the significance of the direct and indirect paths, because these effects mathematically cancel one another out. This was true in our CB path analytic model, where we saw significant direct negative (−.29; p < .01) effects of catastrophizing on solicitousness and significant indirect positive (.24; p <.01) effects of catastrophizing on solicitousness through pain/fatigue behavior, but as a result of their opposite signs, the total effect was close to zero.
The findings highlight the interdependence of social contextual factors, behavior, and catastrophizing. Overt behavioral indicators of pain or fatigue may be a necessary pathway for catastrophizing to have social consequences. In the absence of such behaviors, significant others may not respond solicitously or may respond negatively to dysfunction. For example, if patient catastrophizing is associated with withdrawal from others, there may be fewer opportunities for patients to elicit or significant others to provide support. Further research is needed to replicate our finding of a possible suppression effect, as well as to explore conditions under which catastrophizing might function to reduce rather than increase support or solicitousness. It will also be important to determine if solicitous responding can be elicited by patient behaviors not captured by measures such as the PBCL, and whether other overt behavioral cues may be associated with catastrophizing.
Another issue is the extent to which findings from patients with chronic fatigue may generalize to those with chronic pain and vice versa. As noted previously, chronic fatigue and pain are highly comorbid. [1; 2; 10; 56] Pain symptoms of myalgia, arthralgia and headaches are among the minor criteria that are used to diagnose CFS,[16] and thus are highly prevalent in patients with CFS/CF. Consistent with this, in the current study, 86% of the sample reported average pain over 3 on a 0–10 point scale, with a mean score of 5, suggesting that both pain and fatigue were significant problems. Moreover, studies of patients with fibromyalgia (in which pain and fatigue are likely to co-occur) suggest that, like pain, fatigue is multidimensional and impacts functioning across a wide variety of contexts.[52] Thus it is highly plausible that CB and CCM models developed in the context of chronic pain may be applicable to CFS/CF. The extent to which these concepts generalize across related health conditions and symptoms may provide an important evaluation of their overall utility.
Another related issue is how the overt behavioral communication of fatigue and pain may differ. One study found that spouses tended to underestimate fatigue more than pain.[27] Some studies of overt cues of fatigue have been based on acute sleep deprivation[46] and may not generalize to more complex and pervasive problems such as CFS/CF. However, overlap between fatigue and pain behaviors is also likely. In a study examining observable chronic pain behaviors, Vlaeyen et al.[54] found fatigue to be a component of pain behavior. In addition, behaviors that can indicate pain, such as sighing or stopping activity to rest, may also signal fatigue. More research is needed on similarities and differences between behavioral indicators of chronic fatigue and pain, and whether they have similar relationships to social responses.
This study has several limitations. First, participants were predominantly female specialty center patients with CFS or CF, and there may be important differences (including sex distribution) from patients with chronic pain, or from patients with CFS or CF not seen in specialty settings that may limit generalizability of findings. Second, although validated measures of pain and fatigue behaviors, catastrophizing, and partner responses were adapted for use with patients with CFS or CF, and demonstrated strong psychometric properties in our sample, these adapted measures have not been formally validated. Third, data were based on patient self-report, and thus suffer the limitations of all self-reported data. Ideally, direct observational data would be available to test these path models in a sample of this size. However, patient report may also have advantages in that it can capture a larger time window and potentially more naturalistic situations than a direct observational protocol conducted in an analogue setting. Patient perception of the availability and frequency of social responses may be important in understanding the relationship of a cognitive process such as catastrophizing to social contextual factors. Ideally, in future research both direct observation and self-report would be used to test these models.
Finally, data were cross-sectional, so analyses cannot provide a causal or longitudinal analysis of the models. We also acknowledge that this study is not a definitive or comprehensive test of these models given the circumscribed nature of the data, and that further research will be needed. A comprehensive model of pain communication such as that proposed by Hadjistavropoulos and colleagues[19] may provide a template for a heuristic framework for such research. Notably, both pain and fatigue communications involve a complex internal experience which is encoded, communicated via behavior, and decoded by others in the social environment. Moreover, this process is embedded in a context of cultural, social, intrapersonal and environmental factors, as outlined in this model. Development and use of a similar model of fatigue communication would further the conduct of theory- guided and hypothesis- driven research.
In summary, while findings from this study of patients with CFS/CF were more consistent with a CB model than with the CCM, the role of catastrophizing in the context of chronic fatigue and pain requires further study and model development. Vlaeyen and colleagues[53] noted that neither the CCM nor a cognitive appraisal model were fully able to account for the findings of the lack of an interaction between pain catastrophizing and the presence of others, as predicted by the CCM, or between pain catastrophizing and threat information, as predicted by a threat appraisal model. Future research on catastrophizing should address questions about behavioral linkages between cognitive appraisals and social responses to illness and pain behaviors, while exploring potential roles for catastrophizing that go beyond social coping.
Perspective.
This study of chronic fatigue patients tested cognitive-behavioral and communal coping models of catastrophizing, pain and fatigue behaviors, and solicitous responses by significant others. Results were more consistent with CB formulations, highlighting the importance of behavioral expressions of pain and fatigue in understanding the relationship of catastrophizing to solicitous responses.
Highlights.
Communal coping and behavioral models of catastrophizing make different predictions
This study tested mediational paths from these models in chronic fatigue patients
Catastrophizing’s effects on solicitousness occurred through pain/fatigue behavior
Solicitousness did not mediate the path of catastrophizing to pain/fatigue behavior
Results were more consistent with a cognitive behavioral than communal coping model
Footnotes
Disclosures: Funding for this study was provided through NIH U19 A138429 (Joan M. Romano, PhD, Project Principal Investigator) as part of the NIH Chronic Fatigue Syndrome Research Center at the University of Washington (Dedra Buchwald, MD, Principal Investigator). There are no conflicts of interest on the part of the authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Aaron LA, Burke MM, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med. 2000;160:221–227. doi: 10.1001/archinte.160.2.221. [DOI] [PubMed] [Google Scholar]
- 2.Aaron LA, Herrell R, Ashton S, Belcourt M, Schmaling K, Goldberg J, Buchwald D. Comorbid clinical conditions in chronic fatigue: a co-twin control study. J Gen Intern Med. 2001;16:24–31. doi: 10.1111/j.1525-1497.2001.03419.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baron RM, Kenny DA. The moderator mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 4.Belza BL. Comparison of self-reported fatigue in rheumatoid arthritis and controls. J Rheumatol. 1995;22:639–643. [PubMed] [Google Scholar]
- 5.Boothby JL, Thorn BE, Overduin LY, Ward LC. Catastrophizing and perceived partner responses to pain. Pain. 2004;109:500–506. doi: 10.1016/j.pain.2004.02.030. [DOI] [PubMed] [Google Scholar]
- 6.Buchwald D, Pearlman T, Umali J, Schmaling K, Katon W. Functional status in patients with chronic fatigue syndrome, other fatiguing illnesses, and healthy individuals. Am J Med. 1996;101:364–370. doi: 10.1016/S0002-9343(96)00234-3. [DOI] [PubMed] [Google Scholar]
- 7.Buenaver LF, Edwards RR, Haythornthwaite JA. Pain-related catastrophizing and perceived social responses: Inter-relationships in the context of chronic pain. Pain. 2007;127:234–242. doi: 10.1016/j.pain.2006.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cano A, Leong L, Heller JB, Lutz JR. Perceived entitlement to pain-related support and pain catastrophizing: associations with perceived and observed support. Pain. 2009;147:249–254. doi: 10.1016/j.pain.2009.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ciccone DS, Natelson BH. Comorbid illness in women with chronic fatigue syndrome: a test of the single syndrome hypothesis. Psychosom Med. 2003;65:268–275. doi: 10.1097/01.psy.0000033125.08272.a9. [DOI] [PubMed] [Google Scholar]
- 10.Dansie EJ, Furberg H, Afari N, Buchwald D, Edwards K, Goldberg J, Schur E, Sullivan PF. Conditions comorbid with chronic fatigue in a population-based sample. Psychosomatics. 2012;53:44–50. doi: 10.1016/j.psym.2011.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davis MD. The logic of causal order. In: Sullivan JL, Niemi RG, editors. Sage University Paper Series on Quantitative Applications in the Social Sciences. Beverly Hills, CA: Sage Publications; 1985. [Google Scholar]
- 12.Edwards RR, Bingham CO, Bathon J, Haythornthwaite JA. Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006;55:325–332. doi: 10.1002/art.21865. [DOI] [PubMed] [Google Scholar]
- 13.Epstein SA, Kay G, Clauw D, Heaton R, Klein D, Krupp L, Kuck J, Leslie V, Masur D, Wagner M, Waid R, Zisook S. Psychiatric disorders in patients with fibromyalgia. A multicenter investigation. Psychosomatics. 1999;40:57–63. doi: 10.1016/S0033-3182(99)71272-7. [DOI] [PubMed] [Google Scholar]
- 14.Fordyce WE. Behavioral methods for chronic pain and illness. St. Louis, MO: Mosby; 1976. [Google Scholar]
- 15.Fritz MS, Mackinnon DP. Required sample size to detect the mediated effect. Psychol Sci. 2007;18:233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med. 1994;121:953–959. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 17.Gauthier LR, Rodin G, Zimmermann C, Warr D, Librach SL, Moore M, Shepherd FA, Gagliese L. The communal coping model and cancer pain: the roles of catastrophizing and attachment style. J Pain. 2012;13:1258–1268. doi: 10.1016/j.jpain.2012.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Gunzler D, Chen T, Wu P, Zhang H. Introduction to mediation analysis with structural equation modeling. Shanghai Arch Psychiatry. 2013;25:390–394. doi: 10.3969/j.issn.1002-0829.2013.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hadjistavropoulos T, Craig KD, Duck S, Cano A, Goubert L, Jackson PL, Mogil J, Rainville P, Sullivan MJ, de C Williams AC, Vervoort T, Fitzgerald TD. A biopsychosocial formulation of pain communication. Psychol Bull. 2011;137:910–939. doi: 10.1037/a0023876. [DOI] [PubMed] [Google Scholar]
- 20.Iacobucci D, Saldanha N, Deng Z. A meditation on mediation: Evidence that structural equations models perform better than regressions. Journal of Consumer Psychology. 2007;17:140–154. [Google Scholar]
- 21.Jensen MP, Karoly P. Self-report scales and procedures for assessing pain in adults. In: Turk DC, Melzack R, editors. Handbook of pain assessment. 2. New York, NY: Guilford Press; 2001. pp. 15–34. [Google Scholar]
- 22.Keefe FJ, Caldwell DS, Queen KT, Gil KM, Martinez S, Crisson JE, Ogden W, Nunley J. Pain coping strategies in osteoarthritis patients. J Consult Clin Psychol. 1987;55:208–212. doi: 10.1037//0022-006x.55.2.208. [DOI] [PubMed] [Google Scholar]
- 23.Keefe FJ, Lefebvre JC, Egert JR, Affleck G, Sullivan MJ, Caldwell DS. The relationship of gender to pain, pain behavior, and disability in osteoarthritis patients: the role of catastrophizing. Pain. 2000;87:325–334. doi: 10.1016/S0304-3959(00)00296-7. [DOI] [PubMed] [Google Scholar]
- 24.Kerns RD, Haythornthwaite J, Rosenberg R, Southwick S, Giller EL, Jacob MC. The Pain Behavior Check List (PBCL): factor structure and psychometric properties. J Behav Med. 1991;14:155–167. doi: 10.1007/BF00846177. [DOI] [PubMed] [Google Scholar]
- 25.Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- 26.Lukkahatai N, Saligan LN. Association of catastrophizing and fatigue: a systematic review. J Psychosom Res. 2013;74:100–109. doi: 10.1016/j.jpsychores.2012.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyons KS, Jones KD, Bennett RM, Hiatt SO, Sayer AG. Couple perceptions of fibromyalgia symptoms: the role of communication. Pain. 2013;154:2417–2426. doi: 10.1016/j.pain.2013.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.MacKinnon D. Introduction to Statistical Mediation Analysis. New York, NY: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- 29.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1:173–181. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus User’s Guide. 6. Los Angeles, CA: Muthén & Muthén; 2011. [Google Scholar]
- 32.Pence L, Cano A, Thorn B, Ward LC. Perceived spouse responses to pain: the level of agreement in couple dyads and the role of catastrophizing, marital satisfaction, and depression. J Behav Med. 2006;29:511–522. doi: 10.1007/s10865-006-9073-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Petrie K, Moss-Morris R, Weinman J. The impact of catastrophic beliefs on functioning in chronic fatigue syndrome. J Psychosom Res. 1995;39:31–37. doi: 10.1016/0022-3999(94)00071-c. [DOI] [PubMed] [Google Scholar]
- 34.Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9:745–758. doi: 10.1586/ERN.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romano JM, Jensen MP, Schmaling KB, Hops H, Buchwald DS. Illness behaviors in patients with unexplained chronic fatigue are associated with significant other responses. J Behav Med. 2009;32:558–569. doi: 10.1007/s10865-009-9234-3. [DOI] [PubMed] [Google Scholar]
- 36.Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H. Observational assessment of chronic pain patient-spouse behavioral interactions. Behavior Therapy. 1991;22:549–567. [Google Scholar]
- 37.Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H, Wright SF. Sequential analysis of chronic pain behaviors and spouse responses. J Consult Clin Psychol. 1992;60:777–782. doi: 10.1037//0022-006x.60.5.777. [DOI] [PubMed] [Google Scholar]
- 38.Schmaling KB, Smith WR, Buchwald DS. Significant other responses are associated with fatigue and functional status among patients with chronic fatigue syndrome. Psychosom Med. 2000;62:444–450. doi: 10.1097/00006842-200005000-00018. [DOI] [PubMed] [Google Scholar]
- 39.Severeijns R, Vlaeyen JW, van den Hout MA. Do we need a communal coping model of pain catastrophizing? An alternative explanation. Pain. 2004;111:226–229. doi: 10.1016/j.pain.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 40.Severeijns R, Vlaeyen JW, van den Hout MA, Weber WE. Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clin J Pain. 2001;17:165–172. doi: 10.1097/00002508-200106000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological methodology. Washington, DC: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- 42.Sullivan M, Tripp D, Santor D. Gender differences in pain and pain behavior: The role of catastrophizing. Cognitive Therapy and Research. 2000;24:121–134. [Google Scholar]
- 43.Sullivan MJ, Martel MO, Tripp D, Savard A, Crombez G. The relation between catastrophizing and the communication of pain experience. Pain. 2006;122:282–288. doi: 10.1016/j.pain.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 44.Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 45.Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychological Assessment. 1995;7:524–532. [Google Scholar]
- 46.Sundelin T, Lekander M, Kecklund G, Van Someren EJ, Olsson A, Axelsson J. Cues of fatigue: effects of sleep deprivation on facial appearance. Sleep. 2013;36:1355–1360. doi: 10.5665/sleep.2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thorn BE, Keefe FJ, Anderson T. The communal coping model and interpersonal context: problems or process? Pain. 2004;110:505–507. doi: 10.1016/j.pain.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 48.Thorn BE, Ward LC, Sullivan MJ, Boothby JL. Communal coping model of catastrophizing: conceptual model building. Pain. 2003;106:1–2. doi: 10.1016/s0304-3959(03)00228-8. [DOI] [PubMed] [Google Scholar]
- 49.Tsui P, Day M, Thorn B, Rubin N, Alexander C, Jones R. The communal coping model of catastrophizing: patient-health provider interactions. Pain Med. 2012;13:66–79. doi: 10.1111/j.1526-4637.2011.01288.x. [DOI] [PubMed] [Google Scholar]
- 50.Turk DC, Wack JT, Kerns RD. An empirical examination of the “pain-behavior” construct. J Behav Med. 1985;8:119–130. doi: 10.1007/BF00845516. [DOI] [PubMed] [Google Scholar]
- 51.Tzelgov J, Henik A. Suppression situations in psychological research: definitions, implications, and applications. Psychological Bulletin. 1991;109:524–536. [Google Scholar]
- 52.Vincent A, Benzo RP, Whipple MO, McAllister SJ, Erwin PJ, Saligan LN. Beyond pain in fibromyalgia: insights into the symptom of fatigue. Arthritis Res Ther. 2013;15:221. doi: 10.1186/ar4395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vlaeyen JW, Hanssen M, Goubert L, Vervoort T, Peters M, van Breukelen G, Sullivan MJ, Morley S. Threat of pain influences social context effects on verbal pain report and facial expression. Behav Res Ther. 2009;47:774–782. doi: 10.1016/j.brat.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 54.Vlaeyen JW, Van Eek H, Groenman NH, Schuerman JA. Dimensions and components of observed chronic pain behavior. Pain. 1987;31:65–75. doi: 10.1016/0304-3959(87)90007-8. [DOI] [PubMed] [Google Scholar]
- 55.Whitehead L. The measurement of fatigue in chronic illness: a systematic review of unidimensional and multidimensional fatigue measures. J Pain Symptom Manage. 2009;37:107–128. doi: 10.1016/j.jpainsymman.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 56.Wong WS, Fielding R. The co-morbidity of chronic pain, insomnia, and fatigue in the general adult population of Hong Kong: Prevalence and associated factors. J Psychosom Res. 2012;73:28–34. doi: 10.1016/j.jpsychores.2012.04.011. [DOI] [PubMed] [Google Scholar]