Abstract
Purpose
Given the clinical relevance of ESR1 mutations as potential drivers of resistance to endocrine therapy, this study used sensitive detection methods to determine the frequency of ESR1 mutations in primary and metastatic breast cancer, and in cell free DNA (cfDNA).
Patients and Methods
Six ESR1 mutations (K303R, S463P, Y537C, Y537N, Y537S, D538G) were assessed by digital droplet PCR (ddPCR), with lower limits of detection of 0.05% to 0.16%, in primary tumors (n=43), bone (n=12) and brain metastases (n=38), and cfDNA (n=29). Correlations between ESR1 mutations in metastatic lesions and single (1 patient) or serial blood draws (4 patients) were assessed.
Results
ESR1 mutations were detected for D538G (n=13), Y537S (n=3) and Y537C (n=1), and not for K303R, S463P or Y537N. Mutation rates were 7.0% (3/43 primary tumors), 9.1% (1/11 bone metastases), 12.5% (3/24 brain metastases), and 24.1% (7/29 cfDNA). Two patients showed polyclonal disease with more than one ESR1 mutation. Mutation allele frequencies were 0.07% to 0.2% in primary tumors, 1.4% in bone metastases, 34.3 to 44.9% in brain metastases, and 0.2% to 13.7% in cfDNA. In cases with both cfDNA and metastatic samples (n=5), mutations were detected in both (n=3) or in cfDNA only (n=2). Treatment was associated with changes in ESR1 mutation detection and allele frequency.
Conclusions
ESR1 mutations were detected at very low allele frequencies in some primary breast cancers, and at high allele frequency in metastases, suggesting that in some tumors rare ESR1 mutant clones are enriched by endocrine therapy. Further studies should address if sensitive detection of ESR1 mutations in primary breast cancer and in serial blood draws may be predictive for development of resistant disease.
Introduction
Estrogen receptor alpha (ERα, ESR1) is expressed in the majority of breast cancers and is a major regulator of breast cancer development and progression (1). Endocrine therapy is one of the most efficacious and least toxic treatments in ER-positive (+) breast cancers. Current strategies target ER action either by ligand deprivation (aromatase inhibitors (AIs) or ovarian function suppression) or ER blockade through selective estrogen receptor modulators (SERMs) and degraders (SERDs). All these therapies may improve survival in early stage breast cancer (2, 3). However, de novo or acquired resistance is a major clinical problem, especially in metastatic breast cancer. Multiple molecular mechanisms of resistance include down-regulation of ER expression, dysregulation of ER co-regulators, post-translational modifications of ER, and crosstalk with growth factor signaling pathways (4–11).
The concept that somatic base-pair missense mutations in ESR1 may confer hormone independence has been speculated for many years. However, studies of primary breast cancer have reported few or no ESR1 mutations (12–16). For example, ESR1 base-pair missense mutations are present at 0.2% (1/482) in breast cancers in The Cancer Genome Atlas (TCGA) (17), and 0.3% (5/1430) in the Catalog of Somatic Mutations in Cancer. However, recent studies have documented ESR1 as being highly mutated in metastatic breast cancer. Li et al first reported ESR1 ligand binding domain mutations in two patient-derived xenografts from hormone-resistant advanced disease (18). Subsequently, high rates of ESR1 mutation (15–50%) in metastatic breast cancer have been reported (19–22). Furthermore, recent studies have implicated that the emergence of ESR1 fusions can also be a mechanism of endocrine therapy resistance (18, 23). Preliminary functional studies indicate that some somatic mutations in ESR1 results in ER ligand-independent activity that is partially resistant to current endocrine therapies, suggesting that these mutations may undergo selection under the pressure of endocrine therapy (18–22).
One goal of precision cancer medicine is to make clinical decisions based upon genomic data, which can identify a target for therapy, and/or predict therapeutic resistance. It is hypothesized that ESR1 gene mutations may be a predictive biomarker of resistance to endocrine therapy. As longitudinal biopsy and genetic analysis of metastatic disease is often not feasible, the concept of measuring mutations in tumor DNA circulating in plasma, termed circulating cell-free DNA (cfDNA), has recently gained much attention. The feasibility of using cfDNA to noninvasively identify molecular alterations within metastatic tumors has been shown in several studies (24–26) and preliminary data suggest that cfDNA can be used to monitor breast cancer burden and treatment response (27). A recent proof-of-principle study detected an ESR1 mutation (E380Q) in cfDNA from a single patient with advanced hormone refractory breast cancer (25, 28). However, the detection of rare mutations has been challenged by several limiting factors, including low cfDNA yields and low tumor cellularity in metastatic lesions. Digital droplet PCR (ddPCR) is a highly sensitive and robust technology for detection of rare mutations compared to the available sequencing techniques (29–31). Here, we report the use of ddPCR to study the incidence of ESR1 mutation in primary breast cancer, metastatic biopsies with a focus on bone and brain metastases since they have been understudied due to difficulties in accessing such tissue, and finally cfDNA from breast cancer patients with recurrent disease.
Method
Sample acquisition
Samples used in this study were obtained from the University of Pittsburgh Health Sciences Tissue Bank (HSTB) (primary breast cancer, brain metastases), or were prospectively collected (bone metastases, blood). There were no special criteria for selection of samples for the study other than those described here. Frozen primary ER-positive breast cancers (n=43) (>60% tumor cellularity) from patients subsequently treated with endocrine therapy were obtained from HSTB. Metastatic tumor biopsies from brain (n=38) and bone (n=12) were collected through HSTB over the last three years. For collection of cfDNA (n=29), blood was drawn (1–4 × 10ml Streck tubes) between 01/14 and 08/14 from patients with advanced disease seen within the UPMC health system. There were a total of 122 samples, from 121 patients, since one patient (CF28) donated both cfDNA and a bone metastases sample. In addition, we had access to skin (CF4), liver (CF16), ovarian (CF23), and soft tissue neck metastases (CF14) from patients who donated blood for cfDNA isolation, thus totaling n=126 analyzed samples. ER status was detected by immunohistochemistry, using ASCO-CAP 2010 guidelines for tumors diagnosed in or after 2010 (32). All patients signed informed consent, and the studies were approved by the University of Pittsburgh IRB.
DNA isolation, preparation, and quantification
30–50 mg of frozen primary tumor tissue and 50–150 mg frozen bone metastases were crushed under liquid nitrogen, and DNA was isolated using Qiagen DNeasy Blood & Tissue Kit. Brain metastases were obtained as FFPE sections and Qiagen Allprep DNA/RNA FFPE Kit was used to isolate DNA from four to six 10 μm slides. cfDNA was isolated as previously described (29). Briefly, plasma was separated by double centrifugation within 7 days of blood collection, and DNA was isolated from 1–4 ml plasma using QIAamp Circulating Nucleic Acid kit. Targeted high-fidelity pre-amplification (15 cycles) was performed on cfDNA and DNA isolated from FFPE brain metastases using primers listed in Table S1. Pre-amplification products were purified using QiaQuick PCR purification kit and diluted before ddPCR at 1:100 and 1:20 for brain metastases and cfDNA, respectively. The pre-amplification does not affect linearity of detection of the mutant allele, as we have shown for ESR1 and PIK3CA mutations (Supplementary Figure S1). All DNA samples were quantified by Qubit dsDNA HS/BR assay kits (Life Technologies).
Mutation detection by droplet digital PCR (ddPCR)
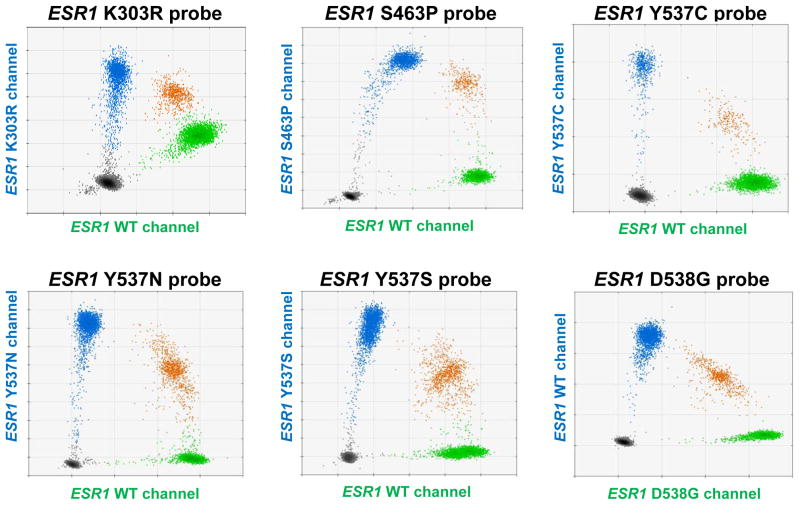
Primers and probes were designed and ordered through Life Technologies for S463P, Y537C/N/S, K303R and Integrated DNA Technologies for D538G ESR1 mutations (Table S2). Bio-Rad QX100 Droplet Digital PCR system was used. Briefly, 1 μl template from diluted pre-amplified products or 50–60 ng of non-amplified DNA was mixed with ddPCR supermix for probes (no dUTPs) (Bio-Rad laboratories, Inc.) and primer/probe set. Droplets were generated using 20 μl of the reaction mixture and 70 μl of droplet generation oil. Positive and negative controls were included in each run to exclude potential contamination artifacts, and to control for proper gating of alleles. All mutation-positive samples were run in at least 3 replicates, assaying at least 10,000 genome equivalents. For positive controls, we utilized oligonucleotides containing the mutation (463P, Y537C/N, K303R), DNA from a cell line with a D538G knock-in mutation (unpublished data), or DNA from a liver biopsy with an ESR1 mutation at Y537S confirmed by Sanger sequencing (Figure 1). Specificity of the probes was demonstrated for Y537C/N/S and D538G mutations (Figure S2). No detectable cross-reactivity of mutant probes and WT probes was observed for D538G or Y537C mutation (Figure S3A). We did find that an increase in the presence of Y537S caused a slight downshift in the fluorescent signal for D538G (Figure S3B) causing a double population, however this didn’t affect the calculated D538G allele frequency. The reason for the decrease in D538G fluorescence is unclear. Mutations with high allele frequencies were confirmed with Sanger sequencing using primers listed in Table S1.
Figure 1. Positive controls for mutation probes utilized in ddPCR technology.
ESR1 K303R, S463P, Y537C, Y537N oligos, or ESR1 D538G and Y537S gDNA were mixed with ESR1 WT gDNA to serve as positive controls for the assay. Scatter plots of ddPCR results showing fluorescent detection of individual droplets. Blue and green dots represent droplets with ESR1 genotypes indicated on Y-axis and X-axis, respectively. Orange dots represent droplets containing both WT and mutant ESR1 DNA. Black dots represent droplets that did not contain DNA.
Quantitative analysis
Data were analyzed using QuantaSoft software (Biorad), calculating a fractional abundance (“mutant allele frequency”). The background noise, which was higher in pre-amplified DNA from cfDNA and FFPE brain metastases compared to DNA from frozen tissues (primary tumors and bone metastases), was defined as the average of allele frequency plus half (for cfDNA) or full (for FFPE DNA) 95% confidence intervals (CIs) of negative controls (ESR1 wildtype DNA) across all ddPCR assays. The noise was subtracted from the allele frequencies. The background-noise-adjusted lower limits of detection (LLoD) of the assay were 0.05% for frozen tissues, 0.10% for cfDNA, and 0.16% for FFPE tissues (Fig S4). Samples were called “positive” for the ESR1 mutation if a) the allele frequencies were >0 after subtraction of background noise, AND b) >2 mutant droplets were repeatedly detected, AND c) allele frequency was > noise adjusted LLoD for at least 3 independent assays.
Results
ESR1 mutations in primary tumors
We screened 43 primary ER-positive tumors to detect ESR1 mutations (S463P, Y537C, Y537N, Y537S, and D538G) recently described in recurrent endocrine-resistant breast cancer. We also included the analysis of the K303R mutation, which has been previously described to be present in primary and metastatic disease, while it wasn’t detected in other studies (33–37). Three primary tumors (PR3, PR21, PR28) were positive for D538G, with very low mutant allele frequencies between 0.07 to 0.2% (Fig 2, and Table 1). Another sample (PR44) was positive in multiple repetitive assays, but the mutant allele frequency (0.012%) was below our LLoD. No other mutations were detected in any of the remaining primary tumors. We thus detected ESR1 mutations in 7.0% (3/43, 95% Wilson binomial confidence interval (CI) 2%–19%) of primary ER+ breast cancers.
Figure 2. ESR1 mutation allele frequency of ESR1 mutation-positive samples.
Average mutant allele frequency ± SEM were calculated using data from at least 3 replicates (after subtraction of respective background noise). Grey lines indicate the adjusted LLoD of respective tissue. PR, BM, BR, and CF represented primary tumors, bone metastases, brain metastases, and cfDNA respectively. Each mark on x-axis represents a sample, and names are indicated for ESR1 mutation-positive samples.
Table 1.
The rates of ESR1 mutations in primary tumors, cfDNA, brain and bone metastases from breast cancer patients.
| Samples | N | ER+ Primary |
ESR1 mutations
|
Pts with ESR1 mutation | Rates of ESR1 mutation | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| K303R | S463P | Y537C | Y537N | Y537S | D538G | |||||
| Primary tumor | 43 | 43 | 0 | 0 | 0 | 0 | 0 | 3 | 3 | 7.0% (3/43) |
| Bone metastases | 12 | 11‡ | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 8.3% (1/12) (9.1% in ER+)** |
| Brain metastases | 38 | 24‡ | 0 | 0 | 0 | 0 | 1 | 3 | 3* | 7.9% (3/38) (12.5% in ER+)** |
| cfDNA | 29 | 29‡ | 0 | 0 | 1 | 0 | 2 | 6 | 7* | 24.1% (7/29) |
Number with known ER+ primary tumor at time of diagnosis (ER status of primary tumor unknown for remaining samples)
One patient with a brain metastasis, and one with cfDNA analysis had multiple distinct ESR1 mutations within a single sample (polyclonal ESR1 mutations).
Frequency of mutations in metastases from a known ER+ primary tumor
ESR1 mutations in bone metastases
Since decalcification of bone metastases can impact downstream analyses, we restricted our analysis of bone metastases to fresh frozen tissue. We obtained 12 frozen bone metastases, 11 of which were from primary tumors known to be ER+. One sample (BM14) was positive for the D538G mutation, with an allele frequency of 1.4% (Fig 2), for an overall ESR1 mutation rate in bone metastases of 8.3% (1/12, 95% CI 0.4%–35%). Of note, the pathologist’s estimate of tumor cellularity in this sample was about 1–5% (Table S3), suggesting that the allele frequency of this mutation within tumor cells in this sample is likely much higher. To confirm our ability to detect mutations across all samples, we performed an additional control by assaying for a frequent PIK3CA mutation (H1047R). Three samples (BM01, BM08, and BM11) (Table S3) tested positive for PIK3CA mutation at high allele frequencies (27.0%, 29.7%, and 37.8%), supporting suitability of our metastatic samples for mutation detection by ddPCR (Fig S5).
ESR1 mutations in brain metastases
We analyzed 38 brain metastases, 24 of which originated from ER+ primary tumors, and 14 from which the ER status of the primary tumors were unknown. All brain metastases with the exception of BR55 (30–40%), BR56 (40–60%), BR60 (40%) and BR68 (30–50%) had at least 60% tumor cellularity. Three brain metastases (BR11, BR17, BR19) contained D538G mutations at high allele frequencies (34.3–44.9%) (Fig 2 for an overall mutation rate of 7.9% (3/38, 95% CI 3%–21%): all were recovered from patients with ER+ primary breast cancer giving a 12.5% frequency in disease with known ER-positivity (3/24, 95% CI 4%–31%). The presence of the D538G mutation was confirmed by Sanger sequencing in the three brain metastases (Figure S6). Interestingly, sample BR17 had an additional Y537S mutation at a lower allele frequency (0.24%). Furthermore, using a dual-mutation specific probe, the mutations were found to be on separate alleles, indicative of polyclonal ESR1 mutations within a single metastatic tumor (Figure S7).
ESR1 mutations in cfDNA
We next interrogated ESR1 mutations in cfDNA collected from 29 patients with metastatic breast cancer, all arising from ER+ primary disease. ESR1 D538G (n=6), Y537S (n=2), and Y537C (n=1) mutations were detected in a total of 7 patients, with one patient (CF4) having polyclonal ESR1-mutations consisting of Y537C, Y537S and D538G with allele frequencies of 2.7%, 1.2% and 5.1% respectively (Table 1). cfDNA allele frequency were overall higher compared to primary tumors (Fig 2). The ESR1 mutation rate in cfDNA was 24.1% (7/29, 95% CI 12%–42%).
Table 2 summarizes clinical characteristics and endocrine treatment history of patients with an ESR1 mutation identified in cfDNA. Typical of patients with ER+ metastatic breast cancer, most had an extensive history of endocrine therapy as measured by both number of agents and months of exposure. There were not sufficient number of samples to formally analyze a predicted association between ESR1 mutations and shorter survival.
Table 2.
Clinical characteristics and endocrine treatment history in patients with confirmed ESR1 mutant cfDNA, brain or bone metastases.
| Clinical Characteristics | Endocrine Therapy before to Mutation Analysis |
Endocrine Therapy after Mutation Analysis |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| ID | Speci- men |
Detected ESR1 mutations |
Stage at Dx |
ER Status |
ADJ Hormonal therapy |
ADJ Hormonal Therapy Duration (months) |
Number of therapies |
Cumulative Exposure (months) |
Endo- crine therapy |
Number of therapies |
Cumu- lative Exposure (months) |
Endo- crine therapy |
| CF4† | cfDNA | Y537C/S, D538G | IIB | + | SERM | 5 | 3 | 23 | AI, SERM | No | No | No |
| CF8† | cfDNA | D538G | IIB | + | AI | 13 | 1 | 47 | SERD | 2 | 5 | AI, SERM |
| CF14† | cfDNA/Soft tissue | Y537S | IV | + | No | 0 | 4 | 25 | AI, SERM, SERD | 1 | 2 | AI, SERM, SERD |
| CF16 | cfDNA/Liver | D538G | 0 | + | No | 0 | 4 | 35 | AI, SERM, SERD | 1 | 4 | AI |
| CF23 | cfDNA | D538G | IV | + | No | 0 | 3 | 42 | AI, SERD | 1 | 7 | SERM |
| CF27† | cfDNA | D538G | IV | + | No | 0 | 7 | 37 | AI, SERM, SERD | No | No | No |
| BR11 | Brain | D538G | 0 | + | No | 0 | 4 | 47 | AI, SERM, SERD | 1 | 7 | SERM |
| BM14/CF28 | cfDNA/Bone | D538G | IIA | + | AI | 72 | 2 | 9 | AI, SERD | 1 | 4 | AI |
| BR19 | Brain | D538G | NK | NK | NK | NK | NK | NK | NK | NK | NK | NK |
| BR17 | Brain | Y537S, D538G | NK | NK | NK | NK | NK | NK | NK | NK | NK | NK |
Patient is deceased.
AI, aromatase inhibitor; SERM, selective estrogen receptor modulator; SERD, selective estrogen receptor down-regulator; ADJ, adjuvant; NK, not known; Dx, diagnosis
Analysis of ESR1 mutations in serial blood samples, and matched metastatic tumors
Serial blood draws from four patients were available for longitudinal examination of ESR1 mutation status. Patient CF4 (Fig 3A) was originally diagnosed with ER+ lymph-node positive disease, underwent mastectomy, and was then treated with SERMs. Over the next year, she developed metastases to brain, liver, bone and skin. A metastatic skin lesion biopsy was negative for ESR1 mutation. A blood draw 6 months later showed three ESR1 mutations with different allele frequencies (Y537C – 2.7%, Y537S – 1.2%, D538G – 5.1%). The patient received an aromatase inhibitor, everolimus, and chemotherapy for six months. A subsequent blood draw (6 months after the first one) revealed an enrichment of Y537C and D538G mutations, but a loss of the Y537S mutant clone (Y537C – 7.4%, Y537S < LLoD, D538G – 10.1%). The increase in the allele frequencies of D538G and Y537C co-occurred with an increase in the tumor marker CA 27–29.
Figure 3. Clinical timelines and allele frequency of ESR1 mutations in serial blood draws and matched metastatic lesions.
A) Sample CF4 and B) Sample CF16. Top: 2D blots showing ESR1 mutant allele frequency as measured by ddPCR. Bottom: The timeline starts with diagnosis of metastatic disease and shows treatments received, disease progression (indicated with orange/red vertical arrows), tumor marker assessments (CA 27–29 antigen line graph), blood draws (indicated with syringe), and ESR1 mutant allele frequency (bar graphs). Treatment abbreviations: Chemo (chemotherapy), PARPi (PARP inhibitor), LU (Leuprolide), SERM (Selective Estrogen Receptor Modulator), SERD (Selective Estrogen Receptor Degrader), AI (Aromatase Inhibitor) and mTORi (mTOR inhibitor). *The matched metastatic lesion was positive for ESR1 mutation.
For patient CF16, DNA from five serial blood draws and from a biopsy of a liver metastasis was analyzed (Figure 2B). The patient originally developed ER+ chest wall metastases twelve years after excision of DCIS. She received serial endocrine therapy including tamoxifen, fulvestrant, and multiple AIs, followed by mTOR inhibitor and chemotherapy, but metastases progressed to other sites, including liver and bone. The ESR1 D538G mutation was detected in both the liver metastasis (23.0%) and the first blood draw (1.0%). The allele frequency was similar in the 2nd blood draw (0.9%), peaked around the time of the 3rd draw (13.7%), decreased in the 4th blood draw (4.9%), and was below LLoD in the 5th draw taken after ~ 6 months of chemotherapy (0.2% before noise subtraction, which did not pass the cut-off for “positive” mutation calling). The decreased frequency of the mutant allele corresponded to lower CA 27–29 levels after chemotherapy.
Two additional patients (CF23, CF28) had two blood draws each (Fig S8). Patient CF23 presented with Stage IV disease, with multiple bone lesions, and an ovarian metastasis that was negative for ESR1 mutation. Blood was drawn at two time points throughout disease progression, as indicated in Fig S8A, which was approximately 1 month after surgical removal of the ovarian metastasis. D538G mutation was detected at low allele frequency (0.2%) in the 1st draw, and was below LLoD in the 2nd draw. Patient CF28 developed lung, bone, and brain metastases 3 years after completion of 5 years of AI treatment for an ER+ breast tumor (Fig S8B). She was treated with AI, and fulvestrant, and cfDNA from 1st blood draw was negative for ESR1 mutations. The disease progressed, and a subsequent bone biopsy revealed an ESR1 D538G mutation (1.4% allele frequency) (BM14, described above), and cfDNA showed the D538G mutation at 7.8% allele frequency. The increase in allele frequency of D538G co-occurred with an increase in CA 27–29 tumor marker. Finally, in one additional patient (CF14) with a single blood draw, the Y537S mutation was detected in both a posterior neck soft tissue nodule (40.5% allele frequency), and in cfDNA, although at lower frequency (0.8%). Thus, in summary, mutations were either detected in both metastatic biopsy and cfDNA (n=3) or in cfDNA only (n=2), suggesting cfDNA as a source for disease phenotyping (e.g. detecting types of mutations), and potentially monitoring burden. This is supported by the observation that changes in ESR1 mutation frequency correlated with changes in CF27–29 levels.
Discussion
ESR1 mutations are present at very low allele frequency in primary ER-positive breast cancer
Previous studies have shown low or undetectable rates of ESR1 mutation in primary breast cancer using Sanger sequencing or massively parallel sequencing (MPS). This is the first study to examine ESR1 mutations (S463P, Y537C, Y537N, Y537S, and D538G, K303R) in primary breast cancer using ddPCR. We found that 7.0% (3/43) of primary breast cancers have an ESR1 D538G mutation, but the allele frequency is very low (0.07 to 0.2%). A recent NGS study of primary tumors from BOLERO trial identified ESR1 mutation in 6/183 tumors (3.3%) (22). TCGA did not detect ESR1 D538G mutation (or K303R, S463P, Y537C, Y537N, Y537S) in 482 primary breast cancers, and COSMIC contains only one ESR1 D538G mutation from 1430 primary breast cancers. The very low allele frequency suggests that in some primary tumors ESR1 mutations pre-exist as rare clones, which are then selected for during metastatic progression. This is consistent with a previous study from a single patient, which used deep-targeted MPS and identified an ESR1 mutation (E380Q) at 2% allele frequency in primary disease and 68% in synchronous liver metastasis (25, 28). Detection of rare ESR1 mutations in primary tumors (0–7%) may be clinically relevant for predicting resistance to hormone therapy; however, additional studies using sensitive detection technologies are necessary to develop this area of investigation.
ESR1 is mutated in both brain and bone metastases
Our analysis of 38 brain and 12 bone metastases showed ESR1 mutations with higher allele frequency compared to primary tumors. To our knowledge, this is the largest study of ESR1 mutations in these specific metastatic sites and the only one to use ddPCR. The most frequently identified ESR1 mutation was D538G, which is consistent with five prior studies that detected a total of fourteen D538G mutations, eleven Y537S mutations, four Y537N mutations, three Y537C mutations, two S463P mutations and eight other ESR1 mutations in a total of 329 samples (18–22). The slightly increased rate of D538G mutations compared to other mutations may be a result of the small sample size in our study. We did not detect the K303R mutation in any of our 126 analyzed samples. The prevalence of K303R has been controversial with one group reporting high frequencies of up to 34% (34) and 50% (38) in premalignant and invasive breast cancer respectively, while others have identified it at low frequency (33, 39), or not at all (18–22, 35–37, 40). The sensitivity of our detection methods suggests that the occurrence of the K303R mutation is likely to be rare.
We detected very high allele frequency (34.3–44.9%) in brain metastases, indicating that the ESR1 mutant-clones are likely dominant clones, and suggesting that the ESR1 mutation is a driver event in metastatic progression to this site. Only one bone metastasis had an ESR1 mutation of relatively low allele frequency (1.4%); however this low frequency is likely due to the very low tumor cellularity in this sample (1–5%). In the future, it might be of interest to test whether different ESR1 mutations preferentially seed at different metastatic sites.
ESR1 exhibits polyclonal mutations
Previous studies have shown convergent evolution of polyclonal mutations in cancer, with different mutations in the same gene ultimately targeting the same phenotype (41). We observed cases with multiple ESR1 mutations in the same tumor, and demonstrated that mutations (Y537S and D538G) were on different alleles, indicating polyclonal disease. Patient CF4 is unique in that cfDNA contained three different ESR1 mutations. It is possible that the cfDNA integrates ESR1 mutations from distinct populations of cells, potentially arising from different metastases. The presence of three different mutations in the ligand-binding domain of ESR1 highlights the substantial selection pressure for these types of mutations during endocrine therapy. Interestingly, longitudinal analysis of cfDNA in this patient indicated increased mutant allele frequency of two clones, and loss of the third clone, possibly reflecting differential response of individual ESR1 mutations to treatments. There is some prior evidence for different biologies of the different mutants. Toy et al show that ligand-independent activity of Y537S is stronger than that of D538G, and weak for S463P (22). It will be important to investigate if this polyclonality is important in treatment response and tumor progression, e.g. if different clones support each other, or if this simply represents a snapshot of a high rate of genomic instability.
Longitudinal monitoring of ESR1 mutations in cfDNA
We detected ESR1 mutations at high mutant allele frequency in cfDNA from patients with advanced breast cancer. The ease of obtaining cfDNA and the high sensitivity suggest that this may be a valuable tool for detecting ESR1 mutation in patients with advanced breast cancer. However, larger studies directly comparing ESR1 mutation in paired cfDNA and metastatic tumor biopsies are required to confirm this possibility.
Additionally, cfDNA analysis potentially affords an invaluable approach for longitudinal measurement of mutations that is simply not possible with solid biopsies. This is shown for example in patient CF4 where an initial skin biopsy was negative for ESR1 mutation, but subsequent cfDNA assays were positive during her course of advanced disease. A study by Mattros-Arruda et al. showed a similar concept in a proof-of-principle study of one patient with advanced disease (25, 28). Association between ESR1 mutation status and response to endocrine therapy is an important question, but our study was not designed to address this. As the numbers were small, retrospective assessment of endocrine therapy history was not examined. Larger studies, and methods to determine the ratio of cfDNA from tumor vs normal cells are required to determine the concordance between primary and metastatic disease, and effects of mutations upon response to hormone therapy. Thus, ultrasensitive detection of rare ESR1 mutations may represent an important biomarker for development of endocrine resistant disease. Note: While this manuscript was under review, two other studies reported detection of ESR1 mutations in cfDNA (42, 43).
Supplementary Material
Statement of Translational Relevance.
Recent studies have identified somatic mutations in the estrogen receptor (ERalpha, ESR1) in endocrine resistant metastatic breast cancer, but rarely or not at all in primary disease, suggesting that such mutations may undergo selection during endocrine therapy. Here we report the use of highly sensitive digital droplet (ddPCR) to study the incidence of ESR1 mutation in primary breast cancer, metastatic biopsies from brain and bone, and circulating cell-free DNA (cfDNA) from breast cancer patients with advanced disease. Our results show that mutations can indeed be identified in primary disease, although at very low mutant allele fraction. In cfDNA we find that 25% of patients with advanced breast cancer harbor mutations in ESR1. Collectively, our data suggest that sensitive detection of ESR1 mutations in primary breast cancer and in serial blood draws may be predictive for development of resistant disease, a hypothesis to be tested in prospective trials.
Acknowledgments
Research Support: The study was funded in part by Fashion Footwear of New York (FFANY), Breast Cancer Research Foundation (BCRF) to AVL, SO and NED, and National Cancer Institute of the National Institutes of Health award number P30CA047904. AVL is a recipient of a Scientific Advisory Council award from Susan G. Komen for the Cure, and is a Hillman Foundation Fellow. PW is supported by a China Scholarship Council award through Tsinghua Medical School, Beijing, China.
This project used the University of Pittsburgh Cancer Institute (UPCI) Biostatistics facility and Tissue and Research Pathology Services that are supported in part by award P30CA047904. The authors acknowledge support of the Health Sciences Tissue Bank staff especially Christina Kline, Louise Mazur, and Christine Thomas. We thank Clinical Research Supervisor Brenda E Steele and nurses in Magee-Womens Hospital of UPMC for collection of patient blood, Priscilla McAuliffe MD, PhD for assistance with IRB, and many other clinicians and staff, as well as patients at UPMC, for making the study possible. The authors wish to acknowledge the thoughtful input of Dr Daniel M Zuckerman, and the support of Dr Ben Park and David Chu for their invaluable scientific and technical advice.
Footnotes
The work is original – it has not been submitted or published elsewhere. It was recently presented in an open scientific meeting (8th International Charite-Mayo Conference, April 2015, Berlin, Germany), and was presented as a poster at ASCO 2015.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies or the University of Pittsburgh.
References
- 1.Yager JD, Davidson NE. Estrogen carcinogenesis in breast cancer. N Engl J Med. 2006;354(3):270–82. doi: 10.1056/NEJMra050776. [DOI] [PubMed] [Google Scholar]
- 2.Tamoxifen for early breast cancer: an overview of the randomised trials. Early Breast Cancer Trialists’ Collaborative Group. Lancet. 1998;351(9114):1451–67. [PubMed] [Google Scholar]
- 3.Jaiyesimi IA, Buzdar AU, Decker DA, Hortobagyi GN. Use of tamoxifen for breast cancer: twenty-eight years later. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 1995;13(2):513–29. doi: 10.1200/JCO.1995.13.2.513. [DOI] [PubMed] [Google Scholar]
- 4.Musgrove EA, Sutherland RL. Biological determinants of endocrine resistance in breast cancer. Nat Rev Cancer. 2009;9(9):631–43. doi: 10.1038/nrc2713. [DOI] [PubMed] [Google Scholar]
- 5.Osborne CK, Bardou V, Hopp TA, Chamness GC, Hilsenbeck SG, Fuqua SA, et al. Role of the estrogen receptor coactivator AIB1 (SRC-3) and HER-2/neu in tamoxifen resistance in breast cancer. J Natl Cancer Inst. 2003;95(5):353–61. doi: 10.1093/jnci/95.5.353. [DOI] [PubMed] [Google Scholar]
- 6.deGraffenried LA, Friedrichs WE, Russell DH, Donzis EJ, Middleton AK, Silva JM, et al. Inhibition of mTOR activity restores tamoxifen response in breast cancer cells with aberrant Akt Activity. Clin Cancer Res. 2004;10(23):8059–67. doi: 10.1158/1078-0432.CCR-04-0035. [DOI] [PubMed] [Google Scholar]
- 7.Hutcheson IR, Knowlden JM, Madden TA, Barrow D, Gee JM, Wakeling AE, et al. Oestrogen receptor-mediated modulation of the EGFR/MAPK pathway in tamoxifen-resistant MCF-7 cells. Breast Cancer Res Treat. 2003;81(1):81–93. doi: 10.1023/A:1025484908380. [DOI] [PubMed] [Google Scholar]
- 8.Britton DJ, Hutcheson IR, Knowlden JM, Barrow D, Giles M, McClelland RA, et al. Bidirectional cross talk between ERalpha and EGFR signalling pathways regulates tamoxifen-resistant growth. Breast Cancer Res Treat. 2006;96(2):131–46. doi: 10.1007/s10549-005-9070-2. [DOI] [PubMed] [Google Scholar]
- 9.Drury SC, Detre S, Leary A, Salter J, Reis-Filho J, Barbashina V, et al. Changes in breast cancer biomarkers in the IGF1R/PI3K pathway in recurrent breast cancer after tamoxifen treatment. Endocr Relat Cancer. 2011;18(5):565–77. doi: 10.1530/ERC-10-0046. [DOI] [PubMed] [Google Scholar]
- 10.Parisot JP, Hu XF, DeLuise M, Zalcberg JR. Altered expression of the IGF-1 receptor in a tamoxifen-resistant human breast cancer cell line. Br J Cancer. 1999;79(5–6):693–700. doi: 10.1038/sj.bjc.6690112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Martz CA, Ottina KA, Singleton KR, Jasper JS, Wardell SE, Peraza-Penton A, et al. Systematic identification of signaling pathways with potential to confer anticancer drug resistance. Science signaling. 2014;7(357):ra121. doi: 10.1126/scisignal.aaa1877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Garcia T, Sanchez M, Cox JL, Shaw PA, Ross JB, Lehrer S, et al. Identification of a variant form of the human estrogen receptor with an amino acid replacement. Nucleic acids research. 1989;17(20):8364. doi: 10.1093/nar/17.20.8364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karnik PS, Kulkarni S, Liu XP, Budd GT, Bukowski RM. Estrogen receptor mutations in tamoxifen-resistant breast cancer. Cancer Res. 1994;54(2):349–53. [PubMed] [Google Scholar]
- 14.McGuire WL, Chamness GC, Fuqua SA. Abnormal estrogen receptor in clinical breast cancer. The Journal of steroid biochemistry and molecular biology. 1992;43(1–3):243–7. doi: 10.1016/0960-0760(92)90214-4. [DOI] [PubMed] [Google Scholar]
- 15.Roodi N, Bailey LR, Kao WY, Verrier CS, Yee CJ, Dupont WD, et al. Estrogen receptor gene analysis in estrogen receptor-positive and receptor-negative primary breast cancer. J Natl Cancer Inst. 1995;87(6):446–51. doi: 10.1093/jnci/87.6.446. [DOI] [PubMed] [Google Scholar]
- 16.Zhang QX, Borg A, Wolf DM, Oesterreich S, Fuqua SA. An estrogen receptor mutant with strong hormone-independent activity from a metastatic breast cancer. Cancer Res. 1997;57(7):1244–9. [PubMed] [Google Scholar]
- 17.Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Science signaling. 2013;6(269):pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li S, Shen D, Shao J, Crowder R, Liu W, Prat A, et al. Endocrine-therapy-resistant ESR1 variants revealed by genomic characterization of breast-cancer-derived xenografts. Cell Rep. 2013;4(6):1116–30. doi: 10.1016/j.celrep.2013.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jeselsohn R, Yelensky R, Buchwalter G, Frampton G, Meric-Bernstam F, Gonzalez-Angulo AM, et al. Emergence of constitutively active estrogen receptor-alpha mutations in pretreated advanced estrogen receptor-positive breast cancer. Clin Cancer Res. 2014;20(7):1757–67. doi: 10.1158/1078-0432.CCR-13-2332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Merenbakh-Lamin K, Ben-Baruch N, Yeheskel A, Dvir A, Soussan-Gutman L, Jeselsohn R, et al. D538G mutation in estrogen receptor-alpha: A novel mechanism for acquired endocrine resistance in breast cancer. Cancer Res. 2013;73(23):6856–64. doi: 10.1158/0008-5472.CAN-13-1197. [DOI] [PubMed] [Google Scholar]
- 21.Robinson DR, Wu YM, Vats P, Su F, Lonigro RJ, Cao X, et al. Activating ESR1 mutations in hormone-resistant metastatic breast cancer. Nat Genet. 2013;45(12):1446–51. doi: 10.1038/ng.2823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Toy W, Shen Y, Won H, Green B, Sakr RA, Will M, et al. ESR1 ligand-binding domain mutations in hormone-resistant breast cancer. Nat Genet. 2013;45(12):1439–45. doi: 10.1038/ng.2822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Veeraraghavan J, Tan Y, Cao XX, Kim JA, Wang X, Chamness GC, et al. Recurrent ESR1-CCDC170 rearrangements in an aggressive subset of oestrogen receptor-positive breast cancers. Nature communications. 2014;5:4577. doi: 10.1038/ncomms5577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rothe F, Laes JF, Lambrechts D, Smeets D, Vincent D, Maetens M, et al. Plasma circulating tumor DNA as an alternative to metastatic biopsies for mutational analysis in breast cancer. Ann Oncol. 2014;25(10):1959–65. doi: 10.1093/annonc/mdu288. [DOI] [PubMed] [Google Scholar]
- 25.De Mattos-Arruda L, Weigelt B, Cortes J, Won HH, Ng CK, Nuciforo P, et al. Capturing intra-tumor genetic heterogeneity by de novo mutation profiling of circulating cell-free tumor DNA: a proof-of-principle. Ann Oncol. 2014;25(9):1729–35. doi: 10.1093/annonc/mdu239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bettegowda C, Sausen M, Leary RJ, Kinde I, Wang Y, Agrawal N, et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci Transl Med. 2014;6(224):224ra24. doi: 10.1126/scitranslmed.3007094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dawson SJ, Tsui DW, Murtaza M, Biggs H, Rueda OM, Chin SF, et al. Analysis of circulating tumor DNA to monitor metastatic breast cancer. N Engl J Med. 2013;368(13):1199–209. doi: 10.1056/NEJMoa1213261. [DOI] [PubMed] [Google Scholar]
- 28.Yu M, Bardia A, Aceto N, Bersani F, Madden MW, Donaldson MC, et al. Cancer therapy. Ex vivo culture of circulating breast tumor cells for individualized testing of drug susceptibility. Science. 2014;345(6193):216–20. doi: 10.1126/science.1253533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Beaver JA, Jelovac D, Balukrishna S, Cochran RL, Croessmann S, Zabransky DJ, et al. Detection of cancer DNA in plasma of patients with early-stage breast cancer. Clin Cancer Res. 2014;20(10):2643–50. doi: 10.1158/1078-0432.CCR-13-2933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Day E, Dear PH, McCaughan F. Digital PCR strategies in the development and analysis of molecular biomarkers for personalized medicine. Methods. 2013;59(1):101–7. doi: 10.1016/j.ymeth.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 31.Diaz LA, Jr, Bardelli A. Liquid biopsies: genotyping circulating tumor DNA. J Clin Oncol. 2014;32(6):579–86. doi: 10.1200/JCO.2012.45.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010;28(16):2784–95. doi: 10.1200/JCO.2009.25.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conway K, Parrish E, Edmiston SN, Tolbert D, Tse CK, Geradts J, et al. The estrogen receptor-alpha A908G (K303R) mutation occurs at a low frequency in invasive breast tumors: results from a population-based study. Breast Cancer Res. 2005;7(6):R871–80. doi: 10.1186/bcr1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuqua SA, Wiltschke C, Zhang QX, Borg A, Castles CG, Friedrichs WE, et al. A hypersensitive estrogen receptor-alpha mutation in premalignant breast lesions. Cancer Res. 2000;60(15):4026–9. [PubMed] [Google Scholar]
- 35.Davies MP, O’Neill PA, Innes H, Sibson DR. Hypersensitive K303R oestrogen receptor-alpha variant not found in invasive carcinomas. Breast Cancer Res. 2005;7(1):R113–8. doi: 10.1186/bcr965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ghimenti C, Mello-Grand M, Regolo L, Zambelli A, Chiorino G. Absence of the K303R estrogen receptor alpha mutation in breast cancer patients exhibiting different responses to aromatase inhibitor anastrozole neoadjuvant treatment. Exp Ther Med. 2010;1(6):939–42. doi: 10.3892/etm.2010.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tokunaga E, Kimura Y, Maehara Y. No hypersensitive estrogen receptor-alpha mutation (K303R) in Japanese breast carcinomas. Breast Cancer Res Treat. 2004;84(3):289–92. doi: 10.1023/B:BREA.0000019963.67754.93. [DOI] [PubMed] [Google Scholar]
- 38.Herynk MH, Parra I, Cui Y, Beyer A, Wu MF, Hilsenbeck SG, et al. Association between the estrogen receptor alpha A908G mutation and outcomes in invasive breast cancer. Clin Cancer Res. 2007;13(11):3235–43. doi: 10.1158/1078-0432.CCR-06-2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Abbasi S, Rasouli M, Nouri M, Kalbasi S. Association of estrogen receptor-alpha A908G (K303R) mutation with breast cancer risk. Int J Clin Exp Med. 2013;6(1):39–49. [PMC free article] [PubMed] [Google Scholar]
- 40.Cancer Genome Atlas N. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70. doi: 10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. The New England journal of medicine. 2012;366(10):883–92. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chu D, Paoletti C, Gersch C, VanDenBerg D, Zabransky D, Cochran R, et al. ESR1 mutations in circulating plasma tumor DNA from metastatic breast cancer patients. Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-15-0943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia-Murillas I, Schiavon G, Weigelt B, Ng C, Hrebien S, Cutts RJ, et al. Mutation tracking in circulating tumor DNA predicts relapse in early breast cancer. Sci Transl Med. 2015;7(302):302ra133. doi: 10.1126/scitranslmed.aab0021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.