Abstract
The aim of this study was to evaluate the morbidity and survival outcome following radical hysterectomy after chemoradiotherapy in the International Federation of Gynecology and Obstetrics (FIGO) stages IB–IIB cervical cancer patients in whom intracavitory brachytherapy was not feasible. We retrospectively reviewed the medical records of our patients who underwent adjuvant radical hysterectomy between January 2005 and December 2012. Post-operative complications were graded according to the grading system of Chassagne et al. (Radiother Oncol 26:195–202, 1993). Survival analysis was done using Kaplan-Meir method. Between January 2005 and December 2012, 43 patients underwent type 2 radical hysterectomy after external beam radiotherapy and concurrent chemotherapy. The median age of the study group was 44 years (range 28–63 years). There were no perioperative deaths. In the early post-operative period, there were 45 complications in 29 patients of which three were of grade 3 severity. The most common post operative complications were urinary tract infections and lymphoedema. The median follow-up time was 29 months (range 9–68 months). The 5-year overall survival was 85.5 % and disease-free survival 82.1 %. This study shows that radical hysterectomy is feasible with good survival outcome and acceptable morbidity after chemoradiotherapy in cervical cancer patients.
Keywords: Cervical cancer, Adjuvant hysterectomy, Radical hysterectomy, Morbidity
Introduction
Cervical cancer continues to be the major tumour burden in India. Most patients with cervical cancer present in advanced stages due to poor organized screening and early detection facilities and are treated with chemoradiation. There is paucity of literature regarding the role of radical hysterectomy in patients with stages IB–IIB disease after chemoradiotherapy. Such a procedure is controversial and not routinely performed because of difficulties in obtaining tumour-free margins and high rate of associated morbidity. However, treatment remains suboptimal in patients in whom intracavitary brachytherapy is not feasible due to difficulty in insertion of intrauterine applicators. Such patients sometimes undergo adjuvant hysterectomy. In this study, we evaluated the morbidity and survival outcome following radical hysterectomy in our patients with the International Federation of Gynecology and Obstetrics (FIGO) stages IB–IIB cervical cancer who were referred for adjuvant hysterectomy after external radiation and concurrent chemotherapy.
Methods
We performed a retrospective study of 43 consecutive patients with FIGO stages IB, IIA and IIB disease who underwent adjuvant hysterectomy after concurrent chemoradiation at our institution from January 2005 to December 2012. Treatment prior to surgery consisted of external beam pelvic radiotherapy in doses ranging from 40 to 46 Gy in 20 to 23 fractions and concurrent weekly low-dose cisplatin in a dose of 40 mg/m2. Patients were referred for surgery after unsuccessful brachytherapy. The most common cause for failed brachytherapy insertion was cervical stenosis in 35 patients; five patients had fibroids distorting the uterine cavity, and three had pyometra.
Radical hysterectomy (Piver type 2) was performed 4 to 6 weeks after completion of radiotherapy. Following surgery, patients underwent brachytherapy to the vaginal vault using vaginal ovoids in a dose of 8 Gy at 0.5 cm from the applicator surface in two sittings. Surgical morbidity was classified according to the grading system of Chassagne et al. [1] (Table 1). Early post-operative complication was defined as any adverse event occurring within 30 days from surgery.
Table 1.
Chassagne et al. grading system [1]
| Morbidity | ||
|---|---|---|
| Grade 1 | Mild complication | Mildly disabling and may cause some functional impairment |
| Grade 2 | Moderate complication | With obvious signs and symptoms and interference with normal activity |
| Grade 3 | Severe complication | Symptoms are life threatening per se or because of treatment and with permanent organ damage |
| Grade 4 | Death | Death occurred as a consequence of a complication of cancer treatment |
Patients were followed up until death or until May 2013. Follow-up information included the date of last follow-up or death and disease status at last follow-up. Survival analysis was done using Kaplan-Meier method.
Results
Forty-three patients underwent type 2 radical hysterectomy after external beam radiotherapy and concurrent chemotherapy from January 2005 to December 2012 (Table 2). Their median age was 44 years (range 28–63 years). Thirty-two patients had squamous cell carcinoma, ten had adenocarcinoma, and one had small cell carcinoma. Twenty-two patients (51.2 %) had FIGO stage IB, 15 (34.9 %) had stage IIA, and 6 (13.9 %) had stage IIB disease. There was no post-surgery mortality.
Table 2.
Patient characteristics
| No. of patients | 43 |
| Age (years) | Median 44 |
| Range 28–63 | |
| Histology, n (%) | |
| Squamous cell carcinoma | 32 (74.4) |
| Adenocarcinoma | 10 (23.3) |
| Small cell carcinoma | 1 (2.3) |
| FIGO stage, n (%) | |
| IB | 22 (51.2) |
| IIA | 15 (34.9) |
| IIB | 6 (13.9) |
| Residual tumour, n (%) | |
| Absent | 17 (39.5) |
| Present | 26 (60.5) |
The mean length of hospital stay was 12.6 days (range 7–18 days). There was no residual tumour in 17 (39.5 %) pathology specimens, indicating complete pathological response.
The medium follow-up period was 29 months (range 9–68 months).
Complications
In the early post-operative period, there were 45 complications in 29 patients of which three were of grade 3 severity (Table 3). The most common complication was related to the urinary tract. Thirteen patients needed prolonged catheterization for more than 14 days. There were five patients with recurrent urinary tract infection. One patient developed vesicovaginal fistula for which she underwent fistula repair 4 weeks after surgery.
Table 3.
Complications
| Number | Total | |
|---|---|---|
| Immediate complications | ||
| Grade 1 | ||
| Wound infection | 5 | 16 |
| Urinary tract infection | 10 | |
| Paralytic ileus | 1 | |
| Grade 2 | ||
| Recurrent urinary infection | 5 | 26 |
| Lymph cyst | 7 | |
| Bladder atony | 13 | |
| Cellulites | 1 | |
| Grade 3 | ||
| Sepsis | 1 | 3 |
| Vesicovaginal fistula | 1 | |
| Intestinal obstruction | 1 | |
| Total | 45 | |
| Late complications | ||
| Grade 1 | ||
| Lymph edema | 6 | 6 |
| Grade 2 | ||
| Urinary infection | 3 | 7 |
| Ureteric stenosis | 2 | |
| Incisional hernia | 1 | |
| Deep vein thrombosis | 1 | |
| Total | 13 | |
Thirteen patients developed long-term complications. Lymphoedema was the most common problem which was managed conservatively. Two patients had bilateral ureteric stenosis requiring stenting, and one patient developed deep vein thrombosis needing prolonged anticoagulation.
Post-operative complications were seen in all stages of disease, and the incidence was not more in advanced stage disease. Of the three grade 3 complications, one was in stage IIB disease, and two were in stage IIA disease. Of the 26 grade 2 complications, 15 were in stage IB disease, 8 were in stage IIA disease, and 3 were in stage IIB disease. Late complications were also uniformly distributed in all stages of disease.
Survival Analysis
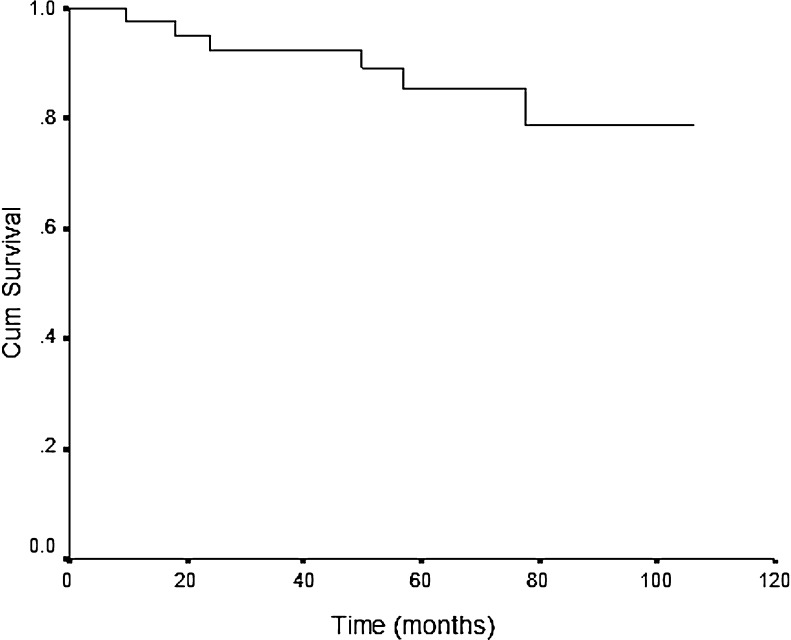
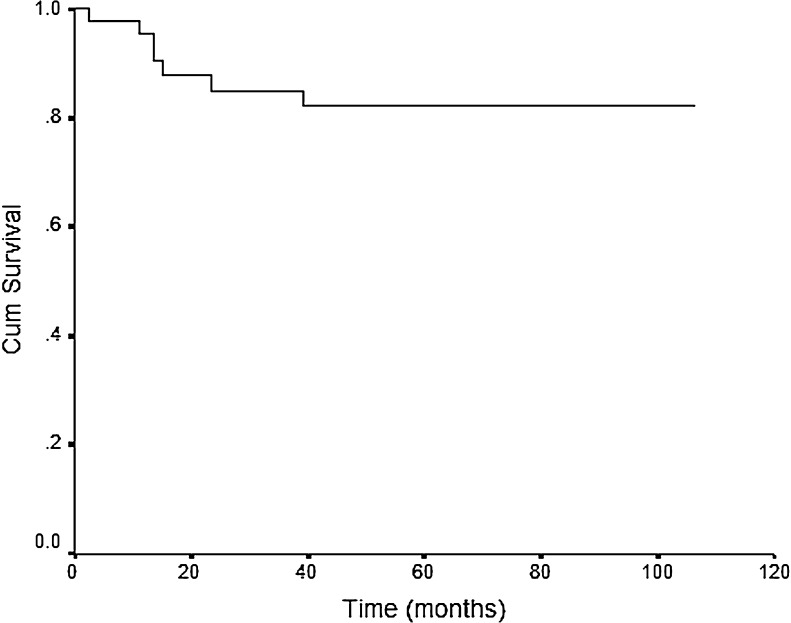
The median duration of follow-up was 29 months. Local recurrence was seen in seven patients and metastasis in three. Two patients had para-aortic nodal metastasis, and another had supra-clavicular nodal metastasis. Six patients died due to disease. Six patients received chemotherapy, and one was referred to palliative care. The 5-year overall survival was 85.5 %, and 5-year disease-free survival was 82.1 % (Figs. 1 and 2). The 5-year survival for stage IB was 94 %, stage IIA 80 %, and stage IIB 50 %.
Fig. 1.
Five-year overall survival of 85.5 %
Fig. 2.
Five-year disease-free survival of 82.1 %
Discussion
The standard treatment of cervical cancer with radiation generally requires the use of external beam radiation combined with intracavitory brachytherapy. External beam radiation is used to treat the pelvic nodes and parametria, whereas the central disease is primarily treated by the intracavitory brachytherapy. Adjuvant hysterectomy after radical chemoradiotherapy has not been shown to be associated with survival benefit [2, 3]. However, in patients in whom brachytherapy is not feasible due to various reasons, the total radiation dose is compromised. In such situations adjuvant hysterectomy may have to be resorted to. Walji et al. [4] published a study assessing the role of adjuvant hysterectomy in the treatment of cervical carcinoma after unsuccessful intracavitary brachytherapy insertion. Recurrence-free survival was improved in their series of five patients who underwent adjuvant hysterectomy in comparison to those who received external beam radiotherapy alone.
Local recurrence is the major cause of treatment failure in bulky cervical cancer. Residual tumour is associated with a higher rate of local recurrence and shorter disease-free survival [5–8]. It has been suggested recently that radical surgery could lower the rate of local recurrence in patients with bulky cervical cancer, by removing potential radio- and chemo-resistant foci of disease. In the trial by Keys et al. [9], rates of complete pathological response after concurrent chemoradiation in stage IB2 cervical cancer ranged from 41 to 52 %. The 5-year disease-free survival was 62 % in those who underwent adjuvant hysterectomy and 53 % in the absence of hysterectomy. This benefit was mainly due to the reduced rate of local recurrence after hysterectomy. In our series the pathological specimen showed no residual tumour in 17 of 43 patients (47.2 %). However, this cannot be compared to the series of Keys et al. because our patients had not received intracavitary brachytherapy. The overall survival of 85.5 % at 5 years in our cohort could be due to the contribution of surgery in reducing local recurrence.
The argument against performing radical hysterectomy in previously irradiated patients is because of the potential for a higher risk of complications. In our series, patients underwent type 2 radical hysterectomy after external beam radiation therapy and concurrent chemotherapy. There were only three grade 3 complications and 28 grade 2 complications which are comparable to the data previously reported [10–12]. The most common complications were related to the urinary tract and grade 2 severity. Only three patients needed surgical intervention: two required ureteric stenting and one underwent laparotomy for vesicovaginal fistula repair. There were no treatment-related deaths.
Post-operative complications were seen in all stages of disease, and the incidence was not high in advanced disease. The complications were not life threatening and were managed conservatively. The risk benefit ratio was favourable even in the advanced stages, indicating a benefit from salvage hysterectomy in patients not receiving intracavitory brachytherapy.
Conclusion
Radical hysterectomy can be safely performed in patients with cervical cancer after external beam radiotherapy and concurrent chemotherapy in situations where intracavitary brachytherapy is not feasible. The morbidity is acceptable, and survival outcomes are on par with reported literature. However, prospective randomized studies are needed to determine the potential role of surgery in cervical cancer patients, when offered as part of combined treatment.
References
- 1.Chassagne D, Sismondi P, Horiot JC, et al. A glossary for reporting complications of treatment in gynecological cancers. Radiother Oncol. 1993;26:195–202. doi: 10.1016/0167-8140(93)90260-F. [DOI] [PubMed] [Google Scholar]
- 2.Spensley S, Hunter RD, Livsey JE, Swindell R, Davidson SE. Clinical outcome for chemoradiotherapy in carcinoma of the cervix. R Coll Radiol. 2009;21:49–55. doi: 10.1016/j.clon.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 3.Tan LT, Zahra M. Long-term survival and late toxicity after chemoradiotherapy for cervical cancer—the Addenbrooke’s experience. R Coll Radiol. 2008;20:358–364. doi: 10.1016/j.clon.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 4.Walji N, Chue AL, Yap C, et al. Is there a role for adjuvant hysterectomy after suboptimal concurrent chemoradiation in cervical carcinoma? R Coll Radiol. 2010;22:140–146. doi: 10.1016/j.clon.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 5.Classe JM, Morice P, Rodier J. Pathological evaluation of pelvic radiotherapy with concurrent cisplatin-based chemotherapy followed by surgery in treatment of locally advanced cervical cancer: a retrospective multicentric experience of French Federation of Cancer Centers. Eur J Surg Oncol. 2002;28(3):61. [Google Scholar]
- 6.Perez CA, Kuske RR, Camel HM, Galakatos AE, Hederman MA, Kao MS, et al. Analysis of pelvic tumour control and impact on survival in carcinoma of the uterine cervix treated with radiation therapy alone. Int J Radiat Oncol Biol Phys. 1988;14(4):613–621. doi: 10.1016/0360-3016(88)90081-8. [DOI] [PubMed] [Google Scholar]
- 7.Paley PJ. The prognostic significance of radiation dose and residual tumor in the treatment of barrel-shaped endophytic cervical carcinoma. Gynecol Oncol. 2000;76:373–379. doi: 10.1006/gyno.1999.5691. [DOI] [PubMed] [Google Scholar]
- 8.Motton S, Houvenaeghel G, Delannes M, et al. Results of surgery after concurrent chemotherapy in advanced cervical cancer: comparison of extended hysterectomy and extrafascial hysterectomy. Int J Gynecol Cancer. 2010;20:268–275. doi: 10.1111/IGC.0b013e3181c9e385. [DOI] [PubMed] [Google Scholar]
- 9.Keys HM, Bundy BN, Stehman FB, Okagaki T, Gallupo DG, Burnett AF, et al. Radiation therapy with and without extrafascial hysterectomy for bulky stage IB cervical carcinoma: a randomized trial of the Gynecologic Oncology Group. Gynecol Oncol. 2003;89(3):343–353. doi: 10.1016/S0090-8258(03)00173-2. [DOI] [PubMed] [Google Scholar]
- 10.Touboul C, Uzan C, Mauguen A, et al. Prognostic factors and morbidities after completion surgery in patients undergoing initial chemoradiation therapy for locally advanced cervical cancer. Oncologist. 2010;15:405–415. doi: 10.1634/theoncologist.2009-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen D, de la Rochefordiere A, Chauvenie L, et al. Chemoradiotherapy in locally advanced cancers of the uterine neck. Retrospective study of 92 patients treated at the Institute Curie between 1986 and 1998. Cancer Radiother. 2002;6:201–208. doi: 10.1016/S1278-3218(02)00196-8. [DOI] [PubMed] [Google Scholar]
- 12.Ferrandina G, Legge F, Fagotti A, et al. Preoperative concomitant chemoradiotherapy in locally advanced cervical cancer: safety, outcome, and prognostic measures. Gynecol Oncol. 2007;107:S127–S132. doi: 10.1016/j.ygyno.2007.07.006. [DOI] [PubMed] [Google Scholar]