Abstract
Pilonidal sinus surgery has evolved with the novel flap techniques, and off-midline closure became a preferred surgical procedure due to shorter recovery time and low recurrence rates. To obtain a better off-midline closure without maceration and a possible wound problem, we modified a novel excision technique. We aimed to present this novel flag modification of rhomboid excision and flap reconstruction experience. From December 2007 to June 2009, 100 patients were treated with flag excision and flap reconstruction under regional anesthesia and followed with a mean of 42 (range 35–55) months. Competent closure results were obtained successfully in all patients without an overlap between incision line and midline. None of the patients had seroma. Two patients (2 %) had partial wound detachment superiorly. None of the patients had recurrence during follow-up. The flag excision and flap reconstruction procedure is an effective and comfortable technique both for the surgeon and the patient with a quick healing period and low complication rates without maceration.
Keywords: Pilonidal sinus, Flag excision, Flap, Off-midline closure
Introduction
Pilonidal disease continues to be a significant health problem. The disease itself and many of its treatment modalities often result in time lost from work or school due to the frequent admissions to the surgeon.
Pilonidal disease is thought to be an acquired condition, which is related to the presence of hair in the midline at the depth of the natal cleft [1]. This hair causes a foreign body reaction, which leads to pit formation [2]. Pilonidal disease may present as a simple cyst, an acute abscess, or a chronic discharging sinus [3]. Hence, treatment of pilonidal disease is variable and may change from observation and simple hair removal, to incision and drainage, or even to wide excision with complex surgical reconstruction.
In the surgical treatment of pilonidal sinus, there is no single operative intervention that has been proven superior to another in overall healing, time away from work, or recurrence [4]. On the other hand, extensive disease with numerous pilonidal openings, branching tracts, and overt symptoms usually require wide excision. When excisional surgery is needed, management of the resultant defect on the tense sacral region appears to be the most important issue, because this step is closely related to postoperative morbidity and recurrence [5]. It was confirmed that asymmetric-oblique closure techniques or flap techniques were much more beneficial than simple closure in the midline in a recent meta-analysis [6]. When the midline is lateralized or flattened, recurrences are less likely to occur than after primary closure or other methods that fail to reconstruct the intergluteal sulcus.
The Limberg flap is a very efficient method of flattening the natal cleft, and therefore, low recurrence rates have been reported [5, 7–9]. In spite of the recently accepted superiority of the flap reconstructions to the non-flap techniques, morbidity related to infection and recurrence has not been completely eliminated [10–12]. The only weak point with the Limberg flap procedure is that the lower pole of the flap stays within the intergluteal sulcus, which may promote wound problems. Postoperatively, the cases of infection, non-healing, and/or recurrence usually occur on the inferior midline, which is close to the anal region and most inclined to invert [12, 13]. This technique was modified by some authors by tailoring the rhomboid excision asymmetrically to place the lower pole of the flap lateral to the intergluteal sulcus in order to lower wound problems and recurrence [5, 14, 15].
In this prospective study, we modified the rhomboid excision technique by a flag style incision with the aim of lifting the inferior midline more upward on the midline to prevent wound problems and recurrence.
Methods
From December 2007 to June 2009, 100 consecutive patients (all males, median age 21 ± 2; range 19–35 years) with pilonidal disease were primarily operated with flag excision and flap (FEF) technique. All the patients had more than one opening within the natal cleft, and 24 patients had laterally situated sinus formation. The length of symptoms ranged from 5 months to 4 years (median 21 ± 6 months). The data were recorded prospectively and included age, gender, healing time, complications, and recurrence. The patients had a regular follow-up every 2 months for the first 6 months and every 6 months thereafter for possible recurrence. The average follow-up was 42 (range 35–55) months.
Surgical Technique
All patients had a rectal enema an hour before the operation. Operative region was shaved in the operating room. The patient is placed in prone position and is requested to squeeze his/her buttocks. The gluteal skin contacting during the squeezing is pointed out with permanent pencil. Later, the patient is requested to ease the buttocks and the marked points are connected with pencil and the contacting gluteal skin during resting is pointed out again with pencil. Then, the marked points are connected. Thereby, the inner and outer drawings are completed. The base of this field is the fold formed by counterattraction of the buttocks (Fig. 1). This fold is regarded as the lowest point of the intergluteal sulcus.
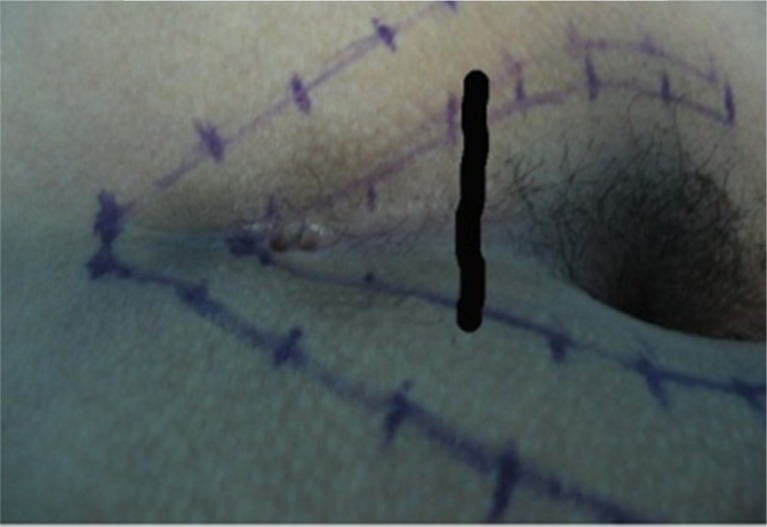
Fig. 1.
Marking of the fold as the base of the field formed by counter attraction of the buttocks
After the first part of the drawings is completed, flag excision area is prepared. The lower end of the flag should be placed both a little bit lower to the base line (fold) and outer line of the inner area, which should contain all the sinus orifices (Fig. 2). The lower oblique line of the flag lies from the inner line of one side to the outer line of the counter side as upper curved. The upper oblique line is projection of the lower line, but straight. The lower side line is curved to the outer side, and the upper side line is drawn straight. Then, the flap lines are prepared at the course of oblique alignment (Fig. 2). Both the size of the excision area and the size of the flag depend on the depth of intergluteal sulcus. The length of the oblique course depends on the distance from the inner line to midline. This configuration states the lines of incision previously at rest, the flap fills the excised intergluteal sulcus, and the incisions and suture lines stay out of contacting gluteal areas.
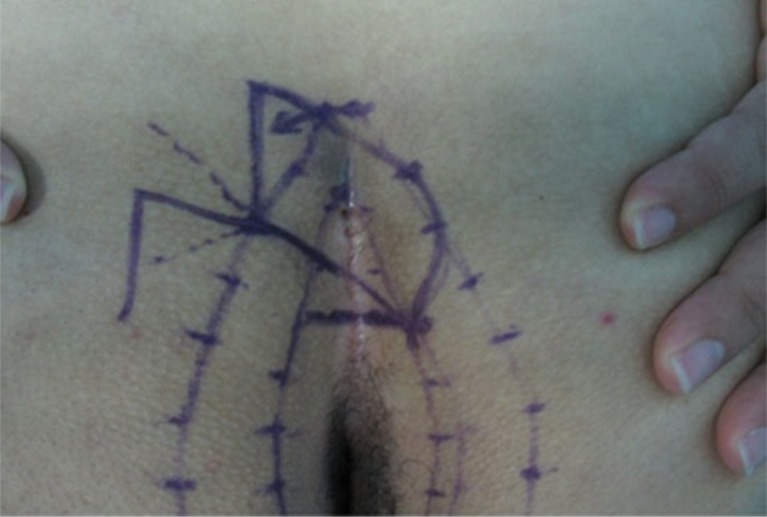
Fig. 2.
Preparation of the flag excision area. The lower end of the flag is placed lower to the fold and outer line of the inner area. The lower oblique line of the flag lies down from the inner line of one side to the outer line of the counter side as upper curved. The upper oblique line is projection of the lower line, but straight. The lower side line is curved to the outer side and the upper side line is drawn straight. The flap lines are prepared at the course of oblique alignment
All the operations were performed under regional anesthesia (spinal and epidural). The operations were performed by two surgeons. Patients were placed in the prone jackknife position on the operating table. The antibiotic prophylaxis was done by a single dose of the first-generation cephalosporin, intravenously. The buttocks were retracted laterally by adhesive tapes. Povidone–iodine solution was used for a proper cleaning. All sinus vestibules were injected with methylene blue in order to visualize exact sinus tract spread. The flag-shaped excision was done through the pencil marks previously drawn, and the excision was deepened down to the presacral fascia (Fig. 3). The fasciocutaneous flap was prepared from the left buttock. After bleeding control, the adhesive tapes are removed from the buttocks and the flap was rotated to the excised area and fixed by 2/0 polyglycolic acid sutures subcutaneously. The skin was closed subcutaneously by 3/0 polypropylene sutures (Fig. 4).
Fig. 3.
Flag-shaped excision through the previously drawn pencil marks deepened down under to the presacral fascia
Fig. 4.
Transposition and fixation of the fasciocutaneous flap prepared from the left buttock
Results
All the patients were male. There was no major anesthetic and surgical complication. Satisfactory flap rotation was achieved in all patients. Good closure results were obtained successfully in all patients without an overlap between incision line and midline. Off-midline closure was achieved in all the patients. No patient had a seroma. The average suture removal time was 10.8 days. Only two patients (2 %) had partial wound detachments. Both complications occurred after discharge following the removal of the skin sutures. In the first case, a partial wound dehiscence at the lower end of the flap line close to the midline occurred and healed secondarily. In the second case, a superficial wound dehiscence occurred at the left upper edge due to maceration, which healed secondarily in a very short time. None of the patients had recurrence during follow-up. Patients returned to full activity on the fourth to seventh postoperative days.
Discussion
The options for the surgical treatment of chronic pilonidal disease vary widely and range from simple excision with or without primary closure to complex flap reconstruction. On the other hand, still there is no consensus as to the correct operation.
The radical treatment modality is wide excision of the chronic tracts. Pilonidal sinus excision can be performed in many different ways. The main problem is the reconstruction of the excised area. In case of sinus removal through a midline incision, the wound can be closed primarily, marsupialized, or left open to heal by secondary intention. Edwards [16] reported their local excision results after a 5-year appraisal. Their overall recurrence rate was as high as 43 % in patients who failed to complete treatment in the dressing clinic. They have a median healing time of 39 days with a range up to 1 year. This causes great discomfort for the patients, and cost/effect rates are very high. Primary closure of the defect under tension also leads to ischemia at the wound edges. Patients complain of tension, especially on sitting, even years after the operation [17]. For primary closure, faster healing [18–20] and more rapid return to work rates have been shown [19]. On the other hand, they were associated with higher recurrence rates when compared to healing by secondary intention [21, 22].
The fundamental objective in treatment and prevention of pilonidal sinus is the stopping of hair insertion, thus neutralizing the causative mechanism. The natural depth of the natal cleft is the target point of hair for mechanical reasons and is also very vulnerable to hair insertion due to a number of congenital or acquired characteristics [23, 24]. Many methods used for treatment of pilonidal sinus have increased this vulnerability, making the natal depth an open portal for entry of hair, for example, by leaving an open wound, defects in a sutured mid-line wound, or holes in the scar from sutures. This was the cause of the very high recurrence rate with the older methods of treatment of pilonidal sinus [1]. Some attempts were made to increase local defenses by decreasing or neutralizing the vulnerability of the target point of hair in the depth of the natal cleft by flattening it and avoiding of any wound scar in the depth of the fold. Although new pits can form in the new midline after skin has been brought across, a new sinus is less likely to form if the cleft is flatter [25].
Lots of flap-based options for the treatment of chronic pilonidal disease were proposed [3, 14, 24–26]. The theory behind flap-based reconstruction is to cover the resultant defect with healthy, rich blood supply without tension. In spite of the recently accepted superiority of the flap reconstructions to the non-flap techniques, morbidity related to infection and recurrence has not been completely eliminated [10–12]. None of these techniques were able to completely flatten the natal cleft to lower the pressure on the midline, especially in the lower part, which is thought to be one of the main causes of the wound separation and recurrence [3]. Postoperatively, the cases of infection, non-healing, and/or recurrence usually occur on the inferior midline, which is close to the anal region and most inclined to invert [12–14]. In this respect, procedures which flatten the depth of intergluteal sulcus and bring the suture line away from the midline appear to be advantageous. In two different systemic reviews, including 10,090 and 1687 patients [6, 27], it was shown that off-midline close had lower recurrence rates when compared with midline closure in the former [6] while off-midline closure was concluded as the best choice if the sinus was to be excised and sutured and was associated with short hospital stay and the lowest recurrence rate in the latter study [27]. Besides, off-midline closure had lower infection rate (6.3 %) when compared with midline closure (10.4 %) [27]. In the studies with follow-up lasting more than a year, off-midline closure had a lower recurrence rate (1.4 %) than midline closure (10.3 %) [6, 27].
The rhomboid or Limberg flap involves midline excision of the pilonidal disease to the presacral fascia with fasciocutaneous coverage [7, 28–30]. It is a rotational flap and results in flattening of the gluteal cleft. The potential problems of this technique include a large tissue mobilization, the increased risk of hematoma/seroma, and wound dehiscence, although they are rare [4]. Additionally, the modification in tailoring the rhomboid excision and the Limberg flap appears to further refine the technique by eliminating the weakest point after reconstruction, namely the inferior midline. In the study of Mentes et al., following a median follow-up period of 4.2 years, the recurrences were 17.9, 7.5, and 0 % in the primary closure, Limberg flap (midline), and modified Limberg flap (off-midline) groups, respectively [14]. The authors eventually realized that the inferior midline was frequently macerated, healed slowly, and might even be a source of recurrences. All of the recurrences, which were eventually noted in the Limberg flap group, developed on the inferior midline. On the other hand, the modified Limberg flap technique itself is able to solve the wound problem in the upper pole, but it is unable to create a good off-midline closure. Studies about the classical Limberg flap and the modified Limberg flaps showed us that these techniques have problems in the lower part of the incision and there are trap and danger points of wound problems like maceration that causes recurrences [5, 14, 30].
In the present study, in order to improve the outcomes with tissue breakdown and recurrence, we applied a novel modification of rhomboid excision named “flag excision and flap” (FEF) reconstruction, which enables off-midline closure with higher suture line and lower tissue tension. Flag excision and flap transposition has some advantages. The midline and incision neighborhood is quite far from the other off-midline techniques (Fig. 5). The sufficient off-midline closure results in lower wound problems in the inferior pole, and in our series, we did not note any maceration and wound problem in the inferior pole except two partial wound detachments in the upper pole. The technique also seems to provide an efficient flattening of the natal cleft in addition to the upper positioning of the inferior suture line.
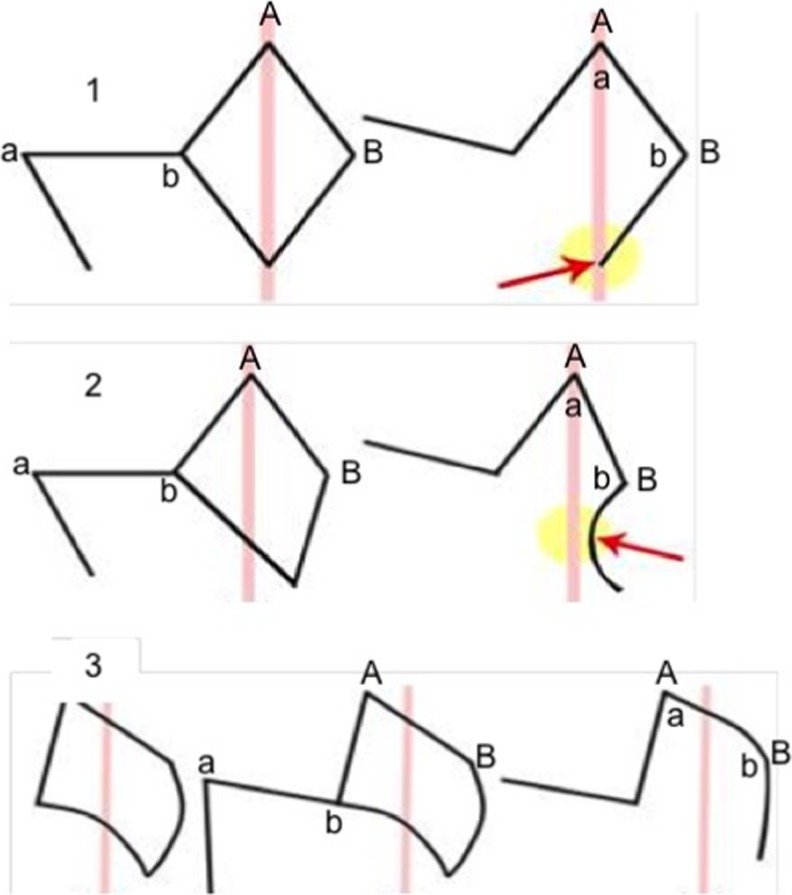
Fig. 5.
Graphical demonstration of relationship between flap margins and midline in different flap techniques; (1) Limberg flap, (2) modified Limberg flap, and (3) flag excision and flap. Red arrows show the relationship between the flap margins and intergluteal sulcus
In conclusion, the results of this series provided further evidence that flag excision and flap reconstruction is an effective operative procedure for primary pilonidal sinus, associated with low complication and recurrence rates. Further clinical studies, including case cohort or randomized studies on a larger patient population with longer follow-up, are needed to prove the efficacy of this technique in the surgical treatment of pilonidal sinus disease.
Acknowledgments
Conflict of Interest
None.
References
- 1.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62:385–389. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 2.Hull TL, Wu J. Pilonidal disease. Surg Clin North Am. 2002;82:1169–1185. doi: 10.1016/S0039-6109(02)00062-2. [DOI] [PubMed] [Google Scholar]
- 3.Chintapatla S, Safarani N, Kumar S, Haboubi N. Sacrococcygeal pilonidal sinus: historical review, pathological insight and surgical options. Tech Coloproctol. 2003;7:3–8. doi: 10.1007/s101510300001. [DOI] [PubMed] [Google Scholar]
- 4.Humphries AE, Duncan JE. Evaluation and management of pilonidal disease. Surg Clin N Am. 2010;90:113–124. doi: 10.1016/j.suc.2009.09.006. [DOI] [PubMed] [Google Scholar]
- 5.Mentes BB, Leventoglu S, Cihan A, Tatlicioglu E, Akin M, Oguz M. Modified Limberg transposition flap for sacrococcygeal pilonidal sinus. Surg Today. 2004;34:419–423. doi: 10.1007/s00595-003-2725-x. [DOI] [PubMed] [Google Scholar]
- 6.Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002;45:1458–1467. doi: 10.1007/s10350-004-6451-2. [DOI] [PubMed] [Google Scholar]
- 7.Urhan MK, Kucukel F, Topgul K, Ozer I, Sari S. Rhomboid excision and Limberg flap for managing pilonidal sinus: results of 102 cases. Dis Colon Rectum. 2002;45:656–659. doi: 10.1007/s10350-004-6263-4. [DOI] [PubMed] [Google Scholar]
- 8.Kapan M, Kapan S, Pekmezci S, Durgun V. Sacrococcygeal pilonidal sinus disease with Limberg flap repair. Tech Coloproctol. 2002;6:27–32. doi: 10.1007/s101510200005. [DOI] [PubMed] [Google Scholar]
- 9.Bozkurt MK, Tezel E. Management of pilonidal sinus with the Limberg flap. Dis Colon Rectum. 1998;41:775–777. doi: 10.1007/BF02236268. [DOI] [PubMed] [Google Scholar]
- 10.Arumugam PJ, Chandrasekaran TV, Morgan AR, Beynon J, Carr ND. The rhomboid flap for pilonidal disease. Colorectal Dis. 2003;5:218–221. doi: 10.1046/j.1463-1318.2003.00435.x. [DOI] [PubMed] [Google Scholar]
- 11.Yilmaz S, Kirimlioglu V, Katz D. Role of simple V-Y advancement flap in the treatment of complicated pilonidal sinus. Eur J Surg. 2000;166:269. doi: 10.1080/110241500750009410. [DOI] [PubMed] [Google Scholar]
- 12.Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996;83:1452–1455. doi: 10.1002/bjs.1800831040. [DOI] [PubMed] [Google Scholar]
- 13.Hurst DW. The evolution of management of pilonidal sinus disease. Can J Surg. 1984;27:603–605. [PubMed] [Google Scholar]
- 14.Cihan A, Mentes BB, Tatlicioglu E, Ozmen S, Leventoglu S, Ucan BH. Modified Limberg flap reconstruction compares favourably with primary repair for pilonidal sinus surgery. ANZ J Surg. 2004;74:238–242. doi: 10.1111/j.1445-2197.2004.02951.x. [DOI] [PubMed] [Google Scholar]
- 15.Can MF, Sevinç MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010;200:318–327. doi: 10.1016/j.amjsurg.2009.08.042. [DOI] [PubMed] [Google Scholar]
- 16.Edwards MH. Pilonidal sinus. a 5-year appraisal of the Millar-Lord treatment. Br J Surg. 1977;64:867–868. doi: 10.1002/bjs.1800641209. [DOI] [PubMed] [Google Scholar]
- 17.Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Am J Surg. 1978;136:640–642. doi: 10.1016/0002-9610(78)90326-4. [DOI] [PubMed] [Google Scholar]
- 18.Rao M, Zawislak W, Kennedy R, Gilliland R. A prospective randomized trial comparing two treatment modalities for chronic pilonidal sinus. Int J Colorectal Dis. 2010;25:395–400. doi: 10.1007/s00384-009-0804-1. [DOI] [PubMed] [Google Scholar]
- 19.Khawaja HT, Bryan S, Weaver PC. Treatment of natal cleft sinus: a prospective clinical and economical evaluation. BMJ. 1992;304:1282–1283. doi: 10.1136/bmj.304.6837.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sondenaa K, Nesvik E, Soreide J. Recurrent pilonidal sinus after excision with closed or open treatment: final result of a randomized trial. Eur J Surg. 1996;162:237–240. [PubMed] [Google Scholar]
- 21.Mohamed HA, Kadry I, Adly S. Comparison between three therapeutic modalities for non-complicated pilonidal sinus disease. Surgeon. 2005;3:73–77. doi: 10.1016/S1479-666X(05)80065-4. [DOI] [PubMed] [Google Scholar]
- 22.Oncel M, Kurt N, Kement M, Colak E, Eser M, Uzun H. Excision and marsupialization versus sinus excision for the treatment of limited chronic pilonidal disease: a prospective randomized trial. Tech Coloproctol. 2002;6:165–169. doi: 10.1007/s101510200037. [DOI] [PubMed] [Google Scholar]
- 23.Bascom J. Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum. 1983;26:800–807. doi: 10.1007/BF02554755. [DOI] [PubMed] [Google Scholar]
- 24.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980;87:567–572. [PubMed] [Google Scholar]
- 25.Armstrong JH, Barcia PJ. Pilonidal disease. The conservative approach. Arch Surg. 1994;129:914–917. doi: 10.1001/archsurg.1994.01420330028006. [DOI] [PubMed] [Google Scholar]
- 26.Kitchen P. Pilonidal sinus: has off-midline closure become the gold standard? ANZ J Surg. 2009;79:4–9. doi: 10.1111/j.1445-2197.2008.04783.x. [DOI] [PubMed] [Google Scholar]
- 27.Karydakis GE (1973) New approach to the problem of pilonidal sinus. The Lancet. 302(7843):1414–1415 [DOI] [PubMed]
- 28.Abu Galala KH, Salam IM, Abu Samaan KR, El Ashaal YI, Chandran VP, Sabastian M, et al. Treatment of pilonidal sinus by primary closure with a transposed rhomboid flap compared with deep suturing: a prospective randomized clinical trial. Eur J Surg. 1999;165:468–472. doi: 10.1080/110241599750006721. [DOI] [PubMed] [Google Scholar]
- 29.Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005;92:1081–1084. doi: 10.1002/bjs.5074. [DOI] [PubMed] [Google Scholar]
- 30.Topgul K, Ozdemir E, Kilic K, Gokbayir H, Ferahkose Z. Long-term results of Limberg flap procedure for treatment of pilonidal sinus: a report of 200 cases. Dis Colon Rectum. 2003;46:1545–1548. doi: 10.1007/s10350-004-6811-y. [DOI] [PubMed] [Google Scholar]