Abstract
Laparoscopic surgery is a minimally invasive surgery, and the incidence of postoperative small bowel obstruction (SBO) is not high. However, SBO is a disease that detracts from the benefits of laparoscopic surgery due to the need for additional therapies or prolongation of hospital stay. Seprafilm is effective in reducing adhesions and preventing the occurrence of SBO. However, it is very difficult to place the Seprafilm during laparoscopic surgery compared to open surgery. Herein, we report a simple and easy method. The Seprafilm including the holder paper is divided into six pieces; each piece is wound around the end of the forceps and the reduction sleeve is slid over it. The forceps with the reduction sleeve is inserted through a 12-mm trocar and moved closer to the target place. Then, the reduction sleeve is slid down the forceps to expose the Seprafilm. This method does not require any special preparation or training. Based on our experience, this method can easily overcome the problems that the Seprafilm is vulnerable to tear and is difficult to spread out in the abdominal cavity.
Keywords: Adhesion, Seprafilm, Laparoscopic surgery, Ileus
Introduction
The rate of postoperative adhesion after digestive surgery is reported to be 66 to 93 % [1]. The rate of SBO caused by formation of adhesions seems to be decreasing because of the prevalence of laparoscopic surgery, which could minimize injury of the abdominal wall and shorten the postoperative recovery time. The incidence of SBO after laparoscopic surgery was reported to be 5 % in the COLOR II trial [2] and 2.5 % in the 11th Nationwide Survey of Endoscopic Surgery in Japan [3]. As seen above, the incidence of SBO is not very high, but SBO is a disease that detracts from the merits of laparoscopic surgery due to the need for additional therapies or prolongation of hospital stay. Seprafilm (Sanofi, Paris, France), which is comprised of sodium hyaluronate-carboxymethylcellulose, is an adhesion barrier and helps to prevent adhesion formation by becoming a hydrated gel and remaining in place for approximately 7 days. It is easy to place the Seprafilm during open surgery, but in laparoscopic surgery, it is difficult without some ingenuities due to the structure of the material. Although there have been some reports on techniques of using the Seprafilm in laparoscopic surgery, each method has some drawbacks. Therefore, Seprafilm is not widely used during laparoscopic surgery. The method of applying Seprafilm during laparoscopic surgery described herein is much easier than methods reported previously based on our experience.
Materials and Surgical Technique
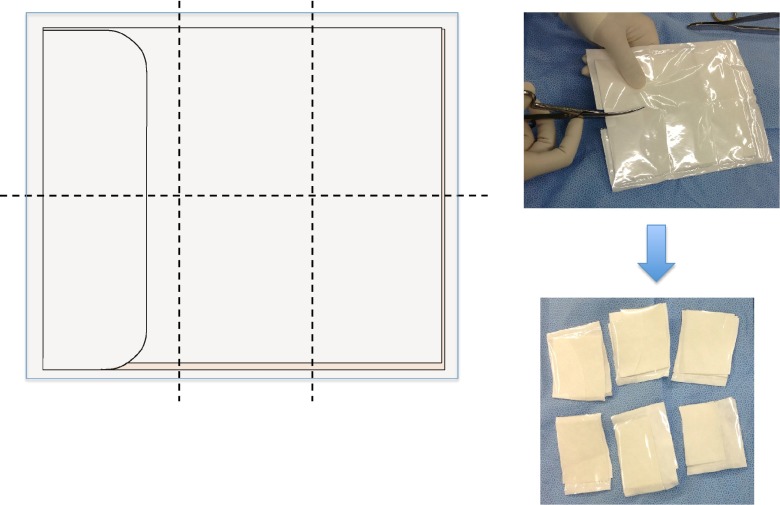
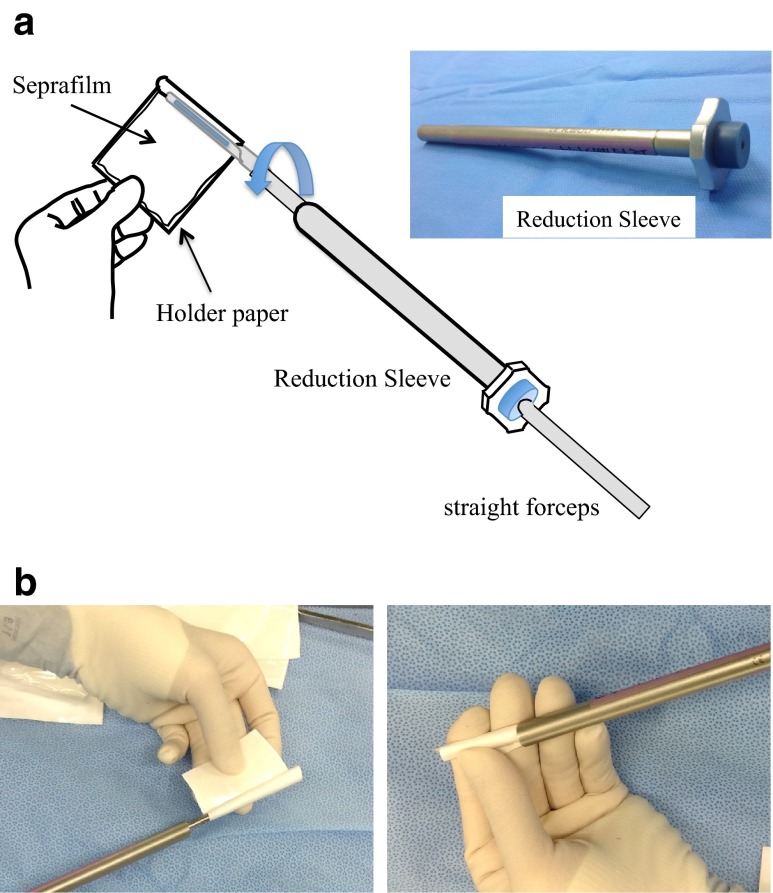
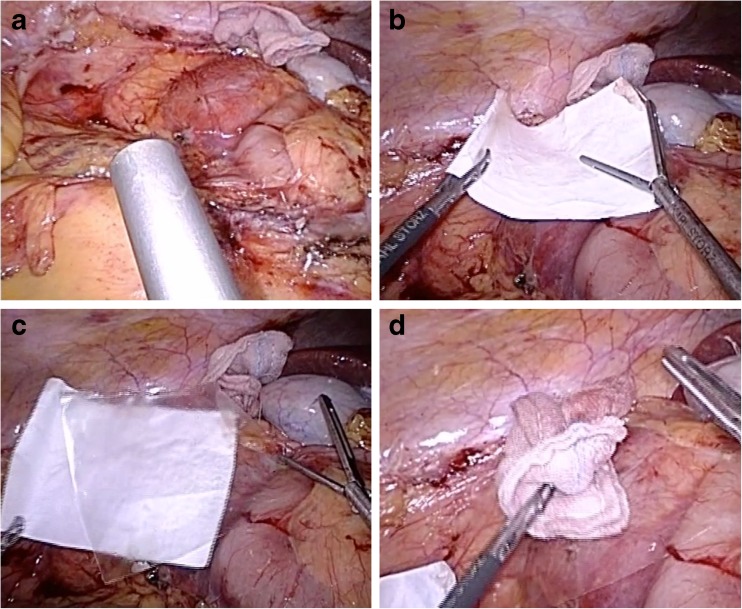
The Seprafilm including the holder paper is divided into six pieces by cutting it once longitudinally and twice along the minor axis (Fig. 1). A straight and long forceps is inserted into a reduction sleeve (KARL STORZ GMBH & CO, Tuttlingen, Germany), and then one of the six pieces of Seprafilm with holder paper is grasped by the forceps, as shown in Fig. 2a. The Seprafilm is wound around the end of the forceps, and then the reduction sleeve is slipped over the Seprafilm (Fig. 2b). The Seprafilm is wound around the forceps inward so that the adhesive side is not exposed. The forceps with the reduction sleeve is inserted through a 12-mm trocar and moved closer to the target place in the surgical field. Then, the reduction sleeve is slid down the forceps to expose the Seprafilm. The Seprafilm is unwound from the forceps and spread out while being grasped by a second forceps and applied to the target location (Fig. 3a–c). Finally, the Seprafilm is pressed by a small wet gauze and fit on the target place (Fig. 3d). This procedure is repeated with as many pieces of the Seprafilm as needed.
Fig. 1.
The Seprafilm including the holder paper is cut into six pieces
Fig. 2.
a The piece of Seprafilm with holder paper is grasped with the forceps, and the Seprafilm is wound around the end of the forceps. b The Seprafilm is wound around the end of the forceps (left panel), and then the reduction sleeve is slipped over the Seprafilm (right panel)
Fig. 3.
a The forceps is moved close to the target area. b, c After the reduction sleeve is slipped off the Seprafilm, the Seprafilm is unwound from the forceps and applied to the target location while using a second forceps. d The Seprafilm is pressed by a small wet gauze and fit on the target location
Results
A total of 18 patients laparoscopically underwent the placement of Seprafilm by two surgeons (Y.S. and K.Y.) using this method at Kobe University Hospital between January 2013 and April 2014. Eight patients underwent laparoscopic right hemicolectomy, two patients underwent laparoscopic ileocecal resection, six patients underwent laparoscopic abdominoperineal resection including lateral lymph node dissection, one patient underwent laparoscopic cholecystectomy, and one patient underwent laparoscopic lymphadenectomy. During the laparoscopic surgeries, there were no cases in which the piece of Seprafilm could not be used due to becoming wet nor incomplete application. The Seprafilm was able to be applied to the intended target in all cases perfectly. It took only 1 to 2 min to apply each piece of Seprafilm. None of the patients showed skin rash or any adverse effects after surgery. There have been no cases of postoperative ileus or any other postoperative complication.
Discussion
It is easy to overlook the importance of preventing postoperative adhesion because laparoscopic surgery is a minimally invasive surgery. However, in colorectal surgery, the possibility of SBO caused by adhesions is considered sufficiently high in terms of the extent of dissection. We have experienced a case of SBO caused by adhesion to the pelvic wall after laparoscopic surgery. To prevent SBO after laparoscopic surgery, it is necessary to take measures to prevent adhesions of the short bowel to organs in the widely dissected area such as the back of the liver or pelvic wall.
Several techniques for laparoscopic placement of Seprafilm have been reported [4, 5]. However, those methods are not easy-to-use approaches and, in reality, are not widely used. Factors that make laparoscopic placement of Seprafilm difficult include its vulnerability to tear when inserting into a trocar and the difficulty in spreading out the Seprafilm in the abdominal cavity due to the structural feature of Seprafilm. Herein, we report an excellent method that overcomes the difficulty easily. This method has two important points. The first is to grasp the Seprafilm with holder paper with a straight forceps and wind the Seprafilm around the end of the forceps. This can provide protection against tearing of the Seprafilm before it is applied. Also, with this method, the Seprafilm with holder paper can be applied to the target area surely without adhering to other tissues before reaching the target location. The second important point is to use the reduction sleeve. In addition to protecting the Seprafilm, the use of the reduction sleeve can keep the Seprafilm dry for as long as possible because it is not necessary to expose the Seprafilm before the target area is reached. When the Seprafilm was inserted into a trocar directly without using the reduction sleeve, the Seprafilm often tore even with the holder paper. Due to the condition in the trocar toward the end of the operation, it is possible that not only the holder paper but also the Seprafilm will become wet. These two points, i.e., winding the Seprafilm with a holder paper at the end of the forceps and using the reduction sleeve, are the important points of this method.
The method described herein is simple and helpful for surgeons. This method does not require any special preparation or training. Based on our experience, this method can easily overcome the problems that the Seprafilm is vulnerable to tear and is difficult to spread out in the abdominal cavity.
The original purpose of the reduction sleeve was to prevent air leakage when inserting a 5-mm forceps into a 12-mm trocar. However, recently, trocars have become much improved and there is only a little air leakage. Therefore, this reduction sleeve is rarely used now. In our division, we do not use it for the original purpose, but use it to prevent port-site recurrence after laparoscopically sampling lymph nodes. Therefore, the reduction sleeve can be used for purposes other than the method described herein and is a very versatile device. Also, the reduction sleeve is reusable, costs approximately $200, and is deemed to be acceptable.
A limitation of this technique is that it is necessary to use a 10–12 mm trocar. Therefore, it is not possible to use this technique in surgeries in which the trocars are all 5-mm trocars.
In conclusion, the Seprafilm is vulnerable to tear and it is difficult to spread out the Seprafilm in the abdominal cavity during laparoscopic surgery. The method described herein is effective for overcoming these problems.
Acknowledgments
Conflict of interest
The authors have no conflicts of interest.
References
- 1.Fazio VW, Cohen Z, Fleshman JW, et al. Reduction in adhesive small-bowel obstruction by Seprafilm adhesion barrier after intestinal resection. Dis Colon Rectum. 2006;49:1–11. doi: 10.1007/s10350-005-0268-5. [DOI] [PubMed] [Google Scholar]
- 2.van der Pas MH, Haglind E, Cuesta MA, et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. Lancet Oncol. 2013;14:210–18. doi: 10.1016/S1470-2045(13)70016-0. [DOI] [PubMed] [Google Scholar]
- 3.11th Nationwide Survey of Endoscopic Surgery in Japan. (2012) JSES 17: 571-694 (in Japanese)
- 4.Shinohara T, Kashiwagi H, Yanagisawa S. A simple and novel technique for the placement of antiadhesive membrane in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech. 2008;18:188–191. doi: 10.1097/SLE.0b013e318166192f. [DOI] [PubMed] [Google Scholar]
- 5.Chuang YC, Fan CN, Cho FN. A novel technique to apply a Seprafilm (hyaluronate–carboxymethylcellulose) barrier following laparoscopic surgeries. Fertil Steril. 2008;90:1959–1963. doi: 10.1016/j.fertnstert.2007.10.003. [DOI] [PubMed] [Google Scholar]