Abstract
Appendicitis is a common surgical abdominal disease with various presentations. Its diagnosis may be obscured by asymptomatic congenital anatomical anomalies like midgut malrotation. Midgut malrotation is a rare fetal anomaly resulting from incomplete or failure of midgut rotation and fixation. It is mostly presented with bowel obstruction or volvulus in early life. Presentation in adult is rare. Here, we report an elderly patient presented with left lower abdominal pain and urinary tract infection. Abdominal computed tomography revealed left-sided appendicitis with non-rotational-type midgut malrotation. Clinicians should bear in mind the possibility of underlying midgut malrotation, as appendicitis could be the first presentation of this rare congenital condition.
Keywords: Acute appendicitis, Left-sided appendicitis, Midgut malrotation, Intestinal malrotation
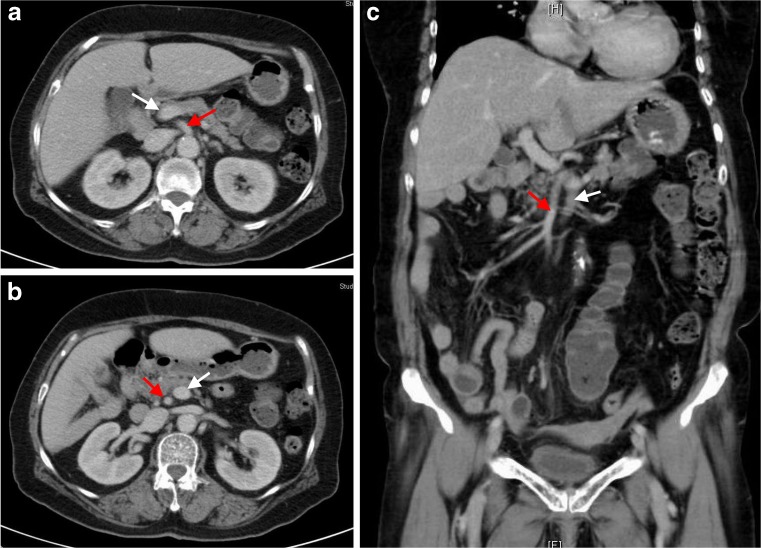
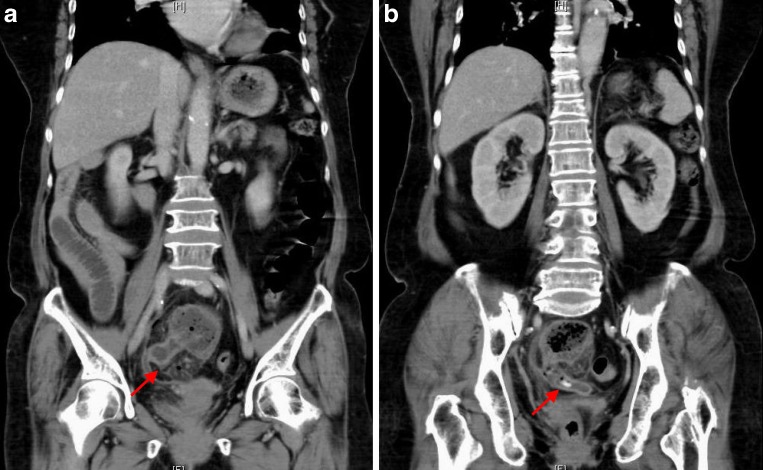
A 77-year-old female with diabetes presented to our emergency department with poor appetite, lower abdominal pain, and dysuria for 3 days. Physical examination revealed whole abdominal tenderness with mild rebounding pain, especially in the left lower abdomen. Laboratory examination showed no leukocytosis, but hyperglycemia, elevated C-reactive protein (32 mg/dl), and pyuria (urine WBC > 100/HPF). An abdominal plain film only showed some large bowel gas in the left hemi-abdomen. Because of the progression of abdominal pain, a computed tomography (CT) was done and incidentally found a congenital midgut malrotation with characteristics of transposition of the superior mesenteric artery (Fig. 1a–c, red arrows) and vein (Fig. 1a–c, white arrows), left-sided lying colon, and right-sided lying small intestine (Fig. 1c). A swollen appendix with fecalith and periappendiceal fat stranding were also found (Fig. 2a, b, red arrows). Emergency operation revealed ruptured acute appendicitis with peritonitis. The histopathologic finding of the resected appendix revealed a suppurative stage of acute appendicitis (Fig. 3). After appendectomy with drainage and antibiotics treatment, the patient was discharged uneventfully 8 days later.
Fig. 1.
The contrast-enhanced abdominal computed tomography demonstrated transposition of the superior mesenteric artery (red arrows, a–c) and vein (white arrows, a–c), left-sided lying colon, and right-sided lying small intestine (c)
Fig. 2.
The reconstructed computed tomography revealed a swollen appendix with fecalith formation and periappendiceal fat stranding (a and b, red arrows)
Fig. 3.
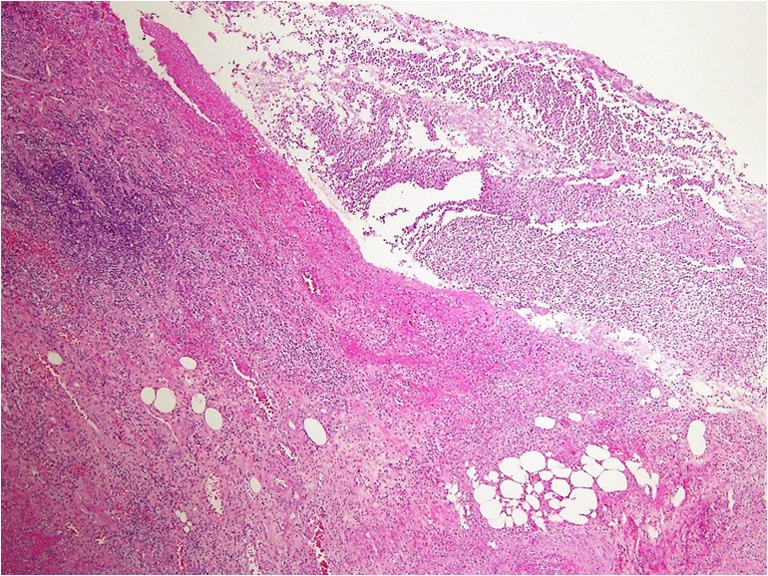
The hematoxylin and eosin-stained appendix sections (×40) revealed a suppurative stage of acute appendicitis with mucosal destruction, abscess formation, dense neutrophils infiltration, and inflammatory exudate coating on the serosal surface
Midgut malrotation is a rare fetal anomaly resulting from incomplete or failure of midgut rotation and fixation during embryonic development [1]. Most cases have been estimated to present in their early life, and less than 0.5 % of cases are identified in adulthood [2]. It has been classified into three major types, including non-rotation (type I), duodenal malrotation (type II), and combined duodenal and cecal malrotation (type III), according to the stage at which the embryologic error occurs [3, 4]. This present patient is in the non-rotation type (type I), which is characterized by right-sided duodenojejunal junction, left-sided lying cecum, and transposition of the superior mesenteric artery and vein [5]. In type II malrotation, patients may manifest as duodenal obstruction due to non-rotation of the duodenum (type IIA), or transverse colon obstruction by superior mesenteric vessels due to reverse rotation of the duodenum and colon (IIB), and paraduodenal hernia due to reverse rotation of duodenum (IIC). In type III malrotation, patients may manifest midgut volvulus due to non-rotation of colon (IIIA), duodenal obstruction by Ladd’s bands (IIIB), cecal volvulus due to incomplete attachment of cecum (IIIC), or internal hernia near the Treitz ligament (IIID) [4]. The CT scan can be used preoperatively to classify the midgut malrotation accordingly.
Although a few cases with congenital midgut malrotation presented with left-sided appendicitis were reported previously, this is the oldest patient presented with urological symptoms based on the literature. Acute appendicitis is a common surgical abdominal disease with a well-known managing protocol. However, delayed diagnosis of this disease still can increase morbidity and mortality. Clinicians must bear in mind the possibility of left-sided appendicitis, which can be presented in patients of all age groups with congenital midgut malrotation.
Acknowledgments
Conflict of Interest
All authors (Pei Wen Chuang, Bo-Ming Huang, Chung Hsien Liu, Chien-Chin Chen and Ming-Jen Tsai) declare that they have no conflict of interest.
References
- 1.Israelit S, Brook OR, Nira BR, Guralnik L, Hershko D. Left-sided perforated acute appendicitis in an adult with midgut malrotation: the role of computed tomography. Emerg Radiol. 2009;16:217–218. doi: 10.1007/s10140-008-0746-x. [DOI] [PubMed] [Google Scholar]
- 2.Gohl ML, DeMeester TR. Midgut nonrotation in adults. An aggressive approach. Am J Surg. 1975;129:319–323. doi: 10.1016/0002-9610(75)90249-4. [DOI] [PubMed] [Google Scholar]
- 3.Wang CA, Welch CE. Anomalies of intestinal rotation in adolescents and adults. Surgery. 1963;54:839–855. [PubMed] [Google Scholar]
- 4.Kanazawa T, Kasugai K, Miyata M, et al. Midgut malrotation in adulthood. Intern Med. 2000;39:626–631. doi: 10.2169/internalmedicine.39.626. [DOI] [PubMed] [Google Scholar]
- 5.Sonomura T, Koyama T, Ishii S, et al. Acute appendicitis with intestinal malrotation: the usefulness of coronal computed tomography. Intern Med. 2014;53:1511–1513. doi: 10.2169/internalmedicine.53.1755. [DOI] [PubMed] [Google Scholar]